Abstract
Introduction and hypothesis
Urinary incontinence (UI) is frequent among women worldwide, but embarrassment and shame can prevent them from discussing symptoms with others. This study aimed to identify personal and professional relations involved by Danish women with UI. It further aimed to investigate whether age, persistence of symptoms, number of symptoms, influence on daily activities and concern about the symptoms are associated with involving personal and professional relations.
Methods
A sample of 51,090 Danish women, aged ≥ 20 years, were invited to participate in a web-based cross-sectional survey in 2012. We identified individuals with self-reported symptoms of stress incontinence, urge incontinence and UI without stress/urge and explored the involvement of personal and professional relations. Descriptive statistics and multivariate logistic regression were used for analyses.
Results
In total, 26,466 women completed the questionnaire. Of the 5861 (22.1%) women who had experienced a minimum of one UI symptom within the preceding 4 weeks, 71.4% did not involve any professional relations and 45.0% did not involve any personal relations. Further, 38.8% involved neither personal nor professional relations. Personal relations were most often involved, mainly those with the spouse/partner, friends and children. Involving a personal relation was associated with three to five times increased odds of involving health care professionals for all UI types.
Conclusions
UI is highly prevalent, but the condition is infrequently discussed in personal and professional relations. Future research should address the quality of the contacts made and barriers to involving other people.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urinary incontinence (UI) is frequent among women worldwide; a review of several national population-based studies found a median prevalence of UI among women of 27.6% (range 4.8–58.4%) [1]. Lack of treatment can cause reduced quality of life [2], but simple treatment options provided by primary health care, i.e. by general practitioners (GPs) and/or physiotherapists, can improve the condition for many women [3, 4].
Despite available treatment options [3, 4] and a national guideline recommending training of pelvic floor muscles as first-line treatment [5], few women seek treatment for their symptoms [6]. Severity and influence on daily activities are factors found to enhance the decision to involve the GP/physician regarding UI [7,8,9], while embarrassment prevents women from seeking treatment [7, 10]. How these factors influence the decision to involve personal relations is, however, unknown.
Age also seems to be a factor worth exploring, because many studies suggest that older women are more likely than younger women to seek medical help for UI [7, 11,12,13,14], while some studies suggest the contrary [9, 15].
The sociologist Pescosolido has investigated decision-making in medical sociology and argues that it is a “dynamic, interactive process fundamentally intertwined with the structured rhythms of social life” [16]. Consequently, seeking help and deciding with whom symptoms should be discussed could well be based on a complicated decision-making process. Pescosolido found that two patterns in particular were frequent when seeking help: seeking help from both the family and the physician and seeking help only from the physician [16]. Whether the general patterns of help-seeking behaviour suggested by Pescosolido are representative for women experiencing UI is unknown.
Hence, the primary aim of the present study was to identify the personal and professional relations involved by Danish women experiencing UI. The secondary aim was to investigate whether age, persistence of symptoms, number of symptoms, influence on daily activities and concern about the symptoms are associated with involving family and friends and professionals.
Materials and methods
This study is based on data from the Danish Symptom Cohort, which contains data from a nationwide web-based cross-sectional survey. Data collection was conducted from June to December 2012, and the methodological framework has been thoroughly described by Rasmussen et al. [17].
All Danish inhabitants are registered with a unique personal identification number in the Danish Civil Registration System (CRS), which contains information on any Danish resident’s date of birth, gender, emigration, etc. [18]. The individuals invited to participate in the survey were randomly selected using the CRS. Overall, 100,000 adults (51,090 women) aged ≥ 20 years were invited to participate in the survey. The survey was mainly conducted using a secure website, but to prevent the exclusion of people with no access to a computer, tablet or smartphone, the participants were offered the opportunity to respond to the survey in a telephone interview conducted by trained interviewers. Subjects were excluded if they had died, could not be reached because of an unknown address, were suffering from a severe illness (including dementia), had language problems or had moved abroad.
Rasmussen et al. stated that “The conceptual objective of the questionnaire was to measure the prevalence of symptom experiences in the general population and to investigate the individual’s interpretation of symptoms and healthcare seeking behavior” [17]. The questionnaire included 44 symptom categories; 3 of these related to UI were included in the present study. Self-reported symptom experiences were explored by positing the following question: “Have you experienced any of the following bodily sensations, symptoms or discomforts within the past four weeks?” Women with UI were identified as those having a positive response to at least one of the following three symptom categories: “Involuntary urination (incontinence) during exertion, e.g. coughing, sneezing, lifting and exercise”, “Urge to urinate so strong that you cannot make it to the toilet in time” and/or “Involuntary urination (incontinence) without exertion and urge (leakage)”. In this article, these symptom categories correspond to stress incontinence (SUI), urge incontinence (UUI) and incontinence without stress/urge (UI without S/U), respectively. The women had the opportunity to report more than one type of UI.
For each individual symptom category, the women were asked to provide additional information about the persistence of their symptoms, influence on daily activities and their concern about the symptoms.
Inspired by the work of Pescosolido, we explored the involvement of professional and personal contacts [16], professional relationships meaning health care professionals (GP, another doctor, physiotherapist/chiropractor, home help/district nurse, pharmacy staff, alternative therapist and “other”) and personal relations meaning those within the social network (spouse/partner, children, parents, colleagues/classmates, friends, neighbours, siblings and “other”). The items concerning relations are described in detail by Elnegaard et al. [19].
Based on Due et al., we also evaluated a subgroup of respondents without any available personal relations [20]. This subgroup is also described by Elnegaard et al. [19].
Data analysis and statistics
Basic descriptive analyses were used to explore the characteristics of the study sample and the relations involved. For this, we first analyzed the three symptoms separately and subsequently together in a group of respondents reporting at least one of the three incontinence symptoms. Moreover, we stratified the study sample into four age groups: 20–39 years, 40–59 years, 60–79 years or ≥ 80 years.
Symptom persistence was categorized into three groups, based on when the respondents first experienced the symptom: < 1 month, 1–6 months or > 6 months. Concern about the symptoms and the level of influence on daily activities were categorized on a five-point Likert scale: not at all, slightly, moderate, quite a bit and extremely.
Respondents were regarded as having no available personal relations if they had all the following responses to the items concerning personal relations: never/less than once a month being in contact with others, having no available individuals who can help in case of illness, often being alone when desiring to be with others and never/almost never having a person to talk to in case of problems or when in need of support.
We used multivariate logistic regression models to analyze possible associations between involvement of relations and specific characteristics. The characteristics included age, number of UI symptoms, persistence of symptoms, influence on daily activities, concern about the symptoms and involvement of personal relations. Subsequently, we adjusted for these characteristics as possible confounders. For the regression analyses, we categorized the relations into three groups: (1) the GP, (2) other health care professionals (HCPs) and (3) personal relations. Other HCPs encompassed all professional relations selectable apart from the GP.
In the multivariate logistic regression models, concern about the symptoms and influence on daily activities were categorized into no/mild, moderate and severe. No/mild encompassed not at all and slightly; moderate encompassed moderate only; severe encompassed quite a bit and extremely.
All data analyses were conducted using STATA statistical software 14.1 (StataCorp, College Station, TX, USA).
Ethics
The Regional Scientific Ethics Committee for Southern Denmark evaluated the project and concluded that, according to Danish law, it could be implemented without permission from their authority. The project was approved by the Danish Data Protection Agency (j.nr. 2011-41-6651). All participants consented to participate in the study.
Results
Of the 51,090 randomly selected women, 48,606 were eligible for the study (Fig. 1). The response rate was 54.5% and the majority (97.1%) completed the questionnaire online (Fig. 1). The median age of the participants and non-participants was 51 (interquartile range 39–63) and 53 (interquartile range 37–71), respectively.
A total of 5861 women had experienced at least one of the three incontinence symptoms, which corresponds to a prevalence of UI in the general population of 22.2% (Fig. 1). Of those, 4671 women experienced only one of the three symptoms, 974 women experienced two symptoms, and 216 women experienced all three incontinence symptoms. Among women aged 20–39, 12.2% experienced at least one incontinence symptom increasing to 41.5% among women over 80.
Overall, 17.2% of the responding women had experienced SUI within the previous four weeks, 7.2% had experienced UUI, and 3.1% had experienced UI without S/U. In around two-thirds of the women, the symptoms had persisted for more than 6 months (Table 1). The proportion of women reporting that the symptom influenced their daily activities and being concerned about the symptom was higher for UUI and UI without S/U compared with SUI (Table 1).
For 37.5% of women with SUI, 30.5% of women with UUI and 30.0% of women with UI without S/U, neither personal nor professional relations were involved (Table 1).
When a relation was involved, it was usually among the personal relations, mainly the spouse/partner, friends and children for all types of UI (Table 1). Among professional relations, the GP and “another doctor” were the most frequently involved for all types of UI. Less than 5% had talked with a physiotherapist/chiropractor (Table 1).
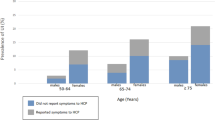
Involvement of personal and professional relations among women experiencing at least one incontinence symptom stratified according to age groups is shown in Table 2. Overall, 38.8% of women experiencing at least one UI symptom involved neither personal nor professional relations, and 71.4% involved no professional relations at all (Table 2). Women aged 20–59 years were less likely to involve both personal and professional relations compared with women over 60. Among personal relations, women > 80 years most often involved their children while women < 80 years more often involved a spouse/partner or friend (Table 2).
The odds of involving the GP, other HCPs and personal relations regarding each of the covariates are shown in Tables 3, 4 and 5. Age > 60 years increased the odds of involving the GP and other HCPs for women with SUI and UUI, but not for women with UI without S/U. In adjusted analysis, age > 60 years only significantly increased the odds of involving the GP among women with SUI (Table 3).
An increasing number of UI symptoms and symptoms persisting for > 6 months were associated with increased odds of involving the GP, other HCPs and personal relations for all three types of incontinence (Tables 3, 4 and 5). After adjustment, the odds remained statistically significant for most relations among the three types of incontinence (Tables 3, 4 and 5).
A higher level of influence on daily activities and concern about the symptom were also associated with increased odds of involving the GP, other HCPs and personal relations for all three types of incontinence in crude analyses (Tables 3, 4 and 5). After adjustment, the results overall remained statistically significant among women with SUI and UUI, but not among women with UI without S/U (Tables 3, 4 and 5).
Involvement of personal relations was associated with three to five times’ increased odds of involvement of the GP and other HCPs for all types of incontinence, and the results remained statistically significant after adjustments (Tables 3, 4 and 5).
The subgroup of women without any available personal relations (n = 87) did not differ from the study population in their involvement of professional relations when experiencing UI (data not shown).
Discussion
Among women experiencing UI, 38.8% involved neither professional nor personal relations regarding their symptoms. Involving personal relations was most frequent and was associated with three to five times’ increased odds of involving the GP and other HCPs.
Overall, odds of involving personal and professional relations were increased among women who had experienced the symptoms for more than 6 months, had more than one type of incontinence, were more concerned about their symptoms, reported a higher impact on daily activities and were older than 60 years.
The prevalence of UI in the present study was 22.2%, increasing from 12.2% for women aged 20–39 to 41.5% for women over 80 years. This is consistent with Danish findings by Rohr et al. [21], but lower than recent findings by Pedersen et al., which suggests a prevalence of 46.4% in women > 18 years [22]. Selection bias could account for this difference, because participants in the study by Pedersen et al. [22] were aware that the study concerned UI at inclusion, which was not the case in our study. It is reasonable to believe that there could have been some selection bias in our study where the weakest/oldest people living in nursing homes and hospitals were ruled out because of the complexity of completing an online questionnaire. The prevalence estimates may therefore be underestimated in the oldest group of respondents.
In the present study, 38.8% of all women experiencing UI did not involve any personal or professional relations. In comparison, only 3.3% had used no source of care in the study by Pescosolido that investigated sources of care used by individuals who had an “illness episode” [16]. The “illness episode” was included on the basis of severity and recency [16], which could have caused selection of a group with increased requests for help compared with the present study, which included all levels of concern and influence; however, UIs seldom induce concern or influence daily activities, as seen in Table 1.
A high level of utilization of the GP could theoretically be expected in our study because it was conducted in a gatekeeper system with free access to the GP [23]. However, 71.4% of the women experiencing UI had not involved any professional relations at all, and consequently < 30% had talked with the GP or another HCP. In comparison, other studies on UI suggest that 15–26% of women with UI seek medical help for their symptoms [11, 24], which is lower than our findings. From previous studies, we know that generally only a minority of symptoms are revealed to the GP [6, 25]. UIs are often mild symptoms of benign origin that therefore do not necessarily need focus or treatment.
Various barriers to seeking medical help among women with UI have been suggested, for example, the assumption that UI is a normal condition related to age [26,27,28]. Discussing the symptom with others could possibly remove some of the barriers to help-seeking. This might be an explanation for the finding that women who had involved personal relations were more likely to involve professional relations too, a finding consistent with that of Kinchen et al. [7]. Another explanation could be that increased severity of the symptoms increases the willingness to discuss the problem with others. This was also the case in the present study where we saw a tendency towards a greater influence on daily activities and higher concern, reflecting a higher symptom severity and an increase in the involvement of the GP, HCPs and personal relations.
While many studies have investigated the involvement of the GP and HCPs among women with UI, only sparse literature exists regarding involvement of personal relations. A study conducted by Roe et al. investigated the involvement of different personal relations within two health authorities: one with an established continence advisory service and one without [10]. Comparable to the present findings, they found that the spouse/partner was most frequently involved, followed by family and friends [10]. However, Roe et al. found a slightly higher prevalence of involving personal relations; 47–49% had involved the spouse/partner (vs. 39.9% in our study) and 25–32% had involved a friend (vs. 22.2% in our study) [10]. The difference might be explained by the fact that Roe et al. included both men and women.
Concerning age, the descriptive analyses showed that those over the age of 60 years more frequently involved both personal and professional relations. The variations seen in the involvement of personal relations could reflect the social network available. Regarding the professional relations, several studies agree that age increases the likelihood of seeking medical help [7, 11,12,13,14]. This is, however, contradictory to Burgio et al. and Reckers et al., who found that older women were less likely to consult a physician [9, 15]. In the study by Burgio et al., the difference could be explained by restriction of the study population to subjects over age 64 years, while there is no obvious explanation for the findings by Reckers et al. A reason for more frequent involvement of the GP among elderly women could be that elderly women consult the GP more often than younger women in general, hence providing more opportunities to present the problem [29]. Moreover, younger women might be more likely to use online resources compared with elderly women, as suggested in a survey exploring internet use among women with a range of pelvic floor problems [30]. Unfortunately, it is not possible to explore this topic retrospectively; hence, it is worth investigating in future studies.
The high level of reluctance to involve other people regarding UI symptoms implies that the GP could take a more proactive approach towards his female patients during consultations for other issues. Future research should explore when case findings would be most relevant. Moreover, the low rate of involving physiotherapists/chiropractors found in this study implies that the GP could refer more women with UI to physiotherapists who provide supervised bladder and pelvic floor training, recommended as first-line treatment [5].
The main strength of this study is the large sample consisting of 26,466 women randomly selected from the general Danish population. Previous analyses of the Danish Symptom Cohort showed that the respondents were fairly representative of the initial study sample, i.e. the Danish population, although more respondents were females, were married/living together, had a high educational and income level and were attached to the labour market [6]. Moreover, this study examines a wide range of relations among women experiencing UI and such studies have not previously been conducted, to our knowledge. It should be noted that the knowledge obtained in this study is specific to the Danish setting and might be applicable to similar settings but is not necessarily generalizable to other cultural settings.
Another strength is anonymity. Data for most respondents were collected in an online survey, which possibly reduced underreporting of intimate symptoms such as UI. Finally, an effort was made to reduce the number of non-respondents by providing an alternative way to complete the survey—using a telephone interview.
The study also has some limitations. First, the questionnaire does not reveal the chronological order of relations involved or the quality or content of the contacts made. Therefore, we can only describe whether a relation was involved or not. Second, a woman was identified as having UI only if she had experienced symptoms within the preceding 4 weeks. Women who had been treated for their symptoms might not have experienced symptoms within 4 weeks, and this could underestimate the prevalence of UI and the proportion of individuals seeking help. Third, the symptoms described in this study are self-reported symptoms and therefore can be affected by recall bias. Since the recall period was only 4 weeks, this type of bias is considered minimal.
Information about the obstetric history could have been relevant to include in a study about urinary incontinence among women. Unfortunately, this information was not available in the survey data.
Conclusions
This study showed a 22.2% prevalence of UI, but despite the high frequency, more than a third of women experiencing UI involved neither personal nor professional relations, and two-thirds did not involve any professional relations. The involvement of relations differed with age, but overall the spouse/partner, friends and children were most frequently involved among the personal relations, while GP and “another doctor” were preferred among the professional relations. Involving personal relations was associated with increased odds of involving both the GP and other HCPs for all types of incontinence.
Further research should investigate how relations are used whenever they are involved, including the chronological order and use of online information sources. Moreover, possible barriers to initiating and pursuing conversations about UI among HCPs should be explored.
Abbreviations
- GP:
-
General practitioner
- UI:
-
Urinary incontinence
- SUI:
-
Stress urinary incontinence
- UUI:
-
Urge urinary incontinence
- HCP:
-
Health care professional
References
Minassian VA, Drutz HP, Al-Badr A. Urinary incontinence as a worldwide problem. Int J Gynaecol Obstet. 2003;82(3):327–38.
Bartoli S, Aguzzi G, Tarricone R. Impact on quality of life of urinary incontinence and overactive bladder: a systematic literature review. Urology. 2010;75(3):491–500. https://doi.org/10.1016/j.urology.2009.07.1325.
Wood LN, Anger JT. Urinary incontinence in women. BMJ. 2014;349:g4531. https://doi.org/10.1136/bmj.g4531.
Seim A, Sivertsen B, Eriksen BC, Hunskaar S. Treatment of urinary incontinence in women in general practice: observational study. BMJ. 1996;312(7044):1459–62.
The Danish College of General Practitioners (DSAM). Klinisk vejledning for almen praksis: Udredning og behandling af nedre urinvejssymptomer hos mænd og kvinder [Clinical guideline: Investigation and Treatment of Lower Urinary symptoms among Men and Women]. 2009.
Elnegaard S, Andersen RS, Pedersen AF, Larsen PV, Sondergaard J, Rasmussen S, et al. Self-reported symptoms and healthcare seeking in the general population—exploring “the symptom iceberg”. BMC Public Health. 2015;15:685. https://doi.org/10.1186/s12889-015-2034-5.
Kinchen KS, Burgio K, Diokno AC, Fultz NH, Bump R, Obenchain R. Factors associated with women's decisions to seek treatment for urinary incontinence. J Women’s Health. 2003;12(7):687–98. https://doi.org/10.1089/154099903322404339.
Elnegaard S, Pedersen AF, Sand Andersen R, Christensen Rd-P, Jarbøl DE. What triggers healthcare-seeking behaviour when experiencing a symptom? Results from a population-based survey. BJGP Open. 2017;1(2). https://doi.org/10.3399/bjgpopen17X100761.
Burgio KL, Ives DG, Locher JL, Arena VC, Kuller LH. Treatment seeking for urinary incontinence in older adults. J Am Geriatr Soc. 1994;42(2):208–12.
Roe B, Doll H, Wilson K. Help seeking behaviour and health and social services utilisation by people suffering from urinary incontinence. Int J Nurs Stud. 1999;36(3):245–53.
Shaw C, Das Gupta R, Williams KS, Assassa RP, McGrother C. A survey of help-seeking and treatment provision in women with stress urinary incontinence. BJU Int. 2006;97(4):752–7. https://doi.org/10.1111/j.1464-410X.2006.06071.x.
Holst K, Wilson PD. The prevalence of female urinary incontinence and reasons for not seeking treatment. N Z Med J. 1988;101(857):756–8.
Hagglund D, Walker-Engstrom ML, Larsson G, Leppert J. Quality of life and seeking help in women with urinary incontinence. Acta Obstet Gynecol Scand. 2001;80(11):1051–5.
Seim A, Sandvik H, Hermstad R, Hunskaar S. Female urinary incontinence—consultation behaviour and patient experiences: an epidemiological survey in a Norwegian community. Fam Pract. 1995;12(1):18–21.
Rekers H, Drogendijk AC, Valkenburg H, Riphagen F. Urinary incontinence in women from 35 to 79 years of age: prevalence and consequences. Eur J Obstet Gynecol Reprod Biol. 1992;43(3):229–34.
Pescosolido BA. Beyond rational choice: the social dynamics of how people seek help. Am J Sociol. 1992;97(4):1096–138.
Rasmussen S, Sondergaard J, Larsen PV, Balasubramaniam K, Elnegaard S, Svendsen RP, et al. The Danish symptom cohort: questionnaire and feasibility in the Nationwide study on symptom experience and healthcare-seeking among 100 000 individuals. Int J Family Med. 2014;2014:187280. https://doi.org/10.1155/2014/187280.
Pedersen CB, Gotzsche H, Moller JO, Mortensen PB. The Danish civil registration system. A cohort of eight million persons. Dan Med Bull. 2006;53(4):441–9.
Elnegaard S, Andersen RS, Pedersen AF, Jarbol DE. Activation of professional and personal network relations when experiencing a symptom: a population-based cross-sectional study. BMJ Open. 2017;7(10):e017620. https://doi.org/10.1136/bmjopen-2017-017620.
Due P, Holstein B, Lund R, Modvig J, Avlund K. Social relations: network, support and relational strain. Soc Sci Med. 1999;48(5):661–73.
Rohr G, Stovring H, Christensen K, Gaist D, Nybo H, Kragstrup J. Characteristics of middle-aged and elderly women with urinary incontinence. Scand J Prim Health Care. 2005;23(4):203–8. https://doi.org/10.1080/02813430500362803.
Schreiber Pedersen L, Lose G, Hoybye MT, Elsner S, Waldmann A, Rudnicki M. Prevalence of urinary incontinence among women and analysis of potential risk factors in Germany and Denmark. Acta Obstet Gynecol Scand. 2017. https://doi.org/10.1111/aogs.13149.
Pedersen KM, Andersen JS, Sondergaard J. General practice and primary health care in Denmark. J Am Board Fam Med. 2012;25(Suppl 1):S34–8. https://doi.org/10.3122/jabfm.2012.02.110216.
Burgio KL, Matthews KA, Engel BT. Prevalence, incidence and correlates of urinary incontinence in healthy, middle-aged women. J Urol. 1991;146(5):1255–9.
Elliott AM, McAteer A, Hannaford PC. Revisiting the symptom iceberg in today's primary care: results from a UK population survey. BMC Fam Pract. 2011;12:16. https://doi.org/10.1186/1471-2296-12-16.
Shaw C, Tansey R, Jackson C, Hyde C, Allan R. Barriers to help seeking in people with urinary symptoms. Fam Pract. 2001;18(1):48–52.
Shaw C. A review of the psychosocial predictors of help-seeking behaviour and impact on quality of life in people with urinary incontinence. J Clin Nurs. 2001;10(1):15–24.
Wojtowicz U, Plaszewska-Zywko L, Stangel-Wojcikiewicz K, Basta A. Barriers in entering treatment among women with urinary incontinence. Ginekol Pol. 2014;85(5):342–7.
Campbell SM, Roland MO. Why do people consult the doctor? Fam Pract. 1996;13(1):75–83.
Mazloomdoost D, Kanter G, Chan RC, Deveaneau N, Wyman AM, Von Bargen EC, et al. Social networking and internet use among pelvic floor patients: a multicenter survey. Am J Obstet Gynecol. 2016;215(5):654.e651–10. https://doi.org/10.1016/j.ajog.2016.06.011.
Acknowledgements
The initial survey was conducted in collaboration among the Research Unit for General Practice, University of Southern Denmark and the Research Centre for Cancer Diagnosis in Primary Care, Aarhus University.
The authors thank Sonja Wehberg and René dePont Christensen for statistical advice and calculations.
Funding
The study is financially supported by the Novo Nordisk Foundation and the Danish Cancer Society. The funding sources had no involvement in the study or in the approval of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Raasthøj, I., Elnegaard, S., Rosendal, M. et al. Urinary incontinence among women—which personal and professional relations are involved? A population-based study. Int Urogynecol J 30, 1565–1574 (2019). https://doi.org/10.1007/s00192-018-3804-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-018-3804-2