Abstract
Introduction and hypothesis
Pregnancy and delivery are well-established risk factors for pelvic floor dysfunction (PFD), but the physiopathology, such as the delivery route, is not well understood. This study evaluated the impact of delivery route on the pelvic floor muscles via 3D ultrasound.
Methods
This review is registered in the PROSPERO database. The criteria for inclusion were prospective studies with 3D translabial ultrasound assessment in primigravida women during pregnancy and postpartum published in English, Spanish or Portuguese between 1980 and 2016. We excluded studies that did not include the topic of urogenital hiatus measurement and literature reviews. The MeSH terms were obstetric delivery, postpartum period, labor, parturition, three-dimensional images, ultrasonography, pelvic floor, and pelvic floor disorders.
Results
The search retrieved 155 articles. After analysis, 6 articles were included. Four studies showed that vaginal delivery (VD) was associated with a larger hiatal area. One study associated the hiatal area with levator ani muscle (LAM) defects in VD. Four articles evaluated the bladder neck, 3 of which showed a significant increase in bladder neck mobility associated with VD and 1 showed decreased bladder neck elevation, not associated with the delivery mode; the first 3 articles all evaluated LAM injuries and showed an association between VD and LAM injury. Women who underwent VD presented defects of the puborectalis muscle.
Conclusions
Vaginal delivery was associated with a higher number of LAM injuries, puborectalis defects, increased bladder neck mobility, and enlargement of the hiatal area.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pelvic floor dysfunction (PFD) comprises disorders that include stress urinary incontinence (SUI), overactive bladder, pelvic organ prolapse (POP), and fecal incontinence [1]. These disorders are prevalent among women, affecting approximately 24% of American women, of which 16% present with SUI, 3% present with POP, and 9% present with fecal incontinence [2]. An increase from 28 million affected American women in 2010 to 43.8 million in 2050 is estimated [3].
The physiopathology of PFD is complex and has many factors, such as obesity, menopause, aging, and a chronic increase in intra-abdominal pressure [4, 5], but some factors, such as pregnancy and delivery, play an important role in the etiology of these dysfunctions [6]. During the gestational period, there is a maternal weight gain and uterine weight increase, leading to an increase in intra-abdominal pressure and therefore an overload of the ligamentous structures, fascias, and pelvic floor muscles [7,8,9]. Furthermore, the pregnant uterus necessitates an increase in the urethrovesical angle, which in turn leads to an increase in the mobility of the vesical neck and can contribute to the onset of urinary symptoms [10]. Some authors have shown that an increase in the size of the hiatal area could occur in the antepartum period [11, 12], and an increase in the hiatal area may be a risk factor for POP.
However, pregnancy is not the only factor that can lead to PFD. Several authors identify vaginal delievery (VD) as a risk factor for PFD, as it causes changes in shape and damage to the levator ani muscle (LAM). LAM defects, particularly its avulsion, are associated with enlargement of the genital hiatus after delivery. In the case of levator defects, the genital hiatus may increase 20–30% in size [13]. Maternal expulsive efforts during delivery and the force uterine contractions exert on the fetal head can induce stretching and compression of the pelvic floor nerves, which may lead to ischemia, neurapraxia or compromised nerve function [14]. It is believed that nerve lesion during delivery can entail muscle atrophy, altering its function and morphology [15].
Many recent studies have tried to establish PFD through imaging methods, such as ultrasound, because of its ease of use, lack of ionizing radiation, minimal discomfort, the relatively short period required for its use, and low price [16,17,18,19,20].
Studies that used 3D ultrasound demonstrated that the pelvic floor muscles undergo considerable distension in VD during crowning [17]. The degree of muscular distension may lead to either a lesion or avulsion [18], especially of the puborectalis muscle, the latter being important to the physiopathology of the POP [19, 20].
Despite PFDs being very prevalent and causing great suffering to women and costs to health services, the physiopathology is not very clear [21]. Many articles associate VD with PFD, but there is no consensus on the protective role of cesarean section (CS).
The purpose of this systematic review was to evaluate the impact of delivery route on the pelvic floor muscles, as evaluated by 3D ultrasound.
Materials and methods
A systematic review was conducted to evaluate pelvic floor disorders during pregnancy and during the postpartum period using 3D ultrasound images according to the type of delivery. This study was recorded in the PROSPERO database under the number CRD42016041313.
For a complete literature search regarding the original articles, the following steps were followed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flowchart [22]. Criteria for inclusion: prospective studies with 3D ultrasound assessment of the pelvic floor muscles in primigravida women during pregnancy and postpartum, with at least one 3D ultrasound examination to identify the pelvic floor muscles during pregnancy and at least one examination in the postpartum period, with the identification of the method of childbirth. We included studies published in English, Portuguese, and Spanish. The criteria for exclusion were studies that did not include the topic, literature reviews and studies that did not include a urogenital hiatus measurement. The variables evaluated were hiatal area, bladder neck mobility, LAM injury, and pelvic floor muscle strength.
The database used for the search was PubMed®, and the following search strategy was elaborated after Medical Subject Headings (MeSH) terms: “delivery, obstetric” OR “postpartum period” OR “labor, obstetric” OR “parturition” AND “three-dimensional images” OR “ultrasonography” AND “pelvic floor” OR “pelvic floor disorders.” The search was conducted on 28 June 2016.
The inclusion process for studies was performed by two independent reviewers (CCA/SC). Initially, the articles were selected by analyzing their titles and summaries. Then, full-text articles that potentially addressed the topic were accessed. Whenever the two reviewers were not in consensus, a third reviewer (CRTJ) was consulted to solve the disagreement. The risk of bias in the studies was evaluated by the Risk Of Bias In Non-randomized Studies of Interventions (ROBINS-I) [23].
Results
The search strategy cross-referenced the descriptors “delivery, obstetric” OR “postpartum period” OR “labor, obstetric” OR “parturition” AND “three-dimensional images” OR “ultrasonography” AND “pelvic floor” OR “pelvic floor disorders” beginning in the PubMed database. A total of 155 articles were found in the PubMed database. A filter tool was used to filter the results by species (“human”), gender (“female”), and language (“English,” “Portuguese,” and “Spanish”).
Of 155 articles, 117 were excluded by title or summary because they did not meet the inclusion criteria (Fig. 1). After evaluating 38 full articles, 32 studies were excluded because they did not have the proper methodology or did not include a urogenital hiatus measurement. After a final analysis, 6 articles were included (Table 1). The risk of bias was evaluated using the tool ROBINS-I. All studies showed a low-risk bias overall (Table 2).
The six articles included in this review were prospective studies, with primigravida women, evaluated both before and after delivery. A total of 1,153 women were included in this review, of which 926 underwent VD and 227 underwent a CS. All studies had at least one ultrasound analysis in the third trimester of pregnancy and one ultrasound analysis in the postpartum period, which varied between 6 weeks and 12 months. The ultrasound devices used were the GE Voluson and Kretz Combison. With regard to the 3D evaluation, all studies evaluated the hiatal area, 4 evaluated bladder neck mobility, and 3 evaluated levator defects (Table 1). The principal results are summarized in Table 3.
Hiatal area
Six studies evaluated the hiatal area [17, 24,25,26,27,28]. Four studies [17, 24, 27, 28] showed that VD was associated with a larger hiatal area in the postpartum period. Toozs-Hobson et al. showed that VD was associated with a significant increase in the levator hiatus area at rest, and during the Valsalva maneuver and pelvic floor contraction. Six weeks postpartum, the differences in the hiatal area between the VD and CS groups were +5.43 cm2 (Valsalva), +3.68 cm2 (rest), and 2.95 cm2 (squeeze; all p < 0.001). Six months postpartum, the differences in the hiatal area between the VD and CS groups were +3.76 cm2 (Valsalva), +1.83 cm2 (rest), and 1.50 cm2 (squeeze; p < 0.001, 0.002, and 0.002, respectively) [28].
Chan et al. also showed that the hiatal area was significantly increased in the VD group compared with the cesarean group 8 weeks after delivery [27]. The study included 442 women, of whom 328 completed a 12-month postpartum follow-up. Hiatal areas according to VD and CS were 10.76 ± 2.28 and 8.95 ± 1.74 cm2 (<0.005), 10.04 ± 2.17 and 8.83 ± 1.86 cm 2 (p < 0.005), and 9.99 ± 2.11 and 9.22 ± 1.67 cm 2 (p = 0.002) at 8 weeks, 6 months, and 12 months postpartum respectively. One-third (34.8%) of VD women had irreversible hiatal distension, defined by more than 20% of the increase in hiatal area. The hiatal area was persistently larger after VD [27].
Staer-Jensen et al. evaluated the hiatal area using as a definition for enlarged levator hiatus (also called ballooning) an area of more than 25 cm2 during the Valsalva maneuver. They found that women who underwent VD had a significantly larger levator hiatus measurement at 6 weeks and 6 months postpartum than women who underwent CS [24]. The percentage of women with VD with an enlarged levator hiatus area increased at 6 weeks postpartum (4.9 to 26.8%) and decreased at 6 and 12 months postpartum (most during 6 months postpartum, 14.8 and 14.1% respectively). In women with cesarean delivery, the number of enlarged levator hiatus areas remained stable in the postpartum period: 2.9% (21 weeks’ gestation), 20% (37 weeks’ gestation), 11.4% (6 weeks postpartum), 5.7% (6 months postpartum), and 14.3% (12 months postpartum). The hiatal area difference and the number of women with enlarged levator hiatus areas both decreased the most during the first 6 months after VD. This study had the most evaluations included out of any in this review (5 times between before and after delivery), and it was the only study that showed a decrease in the hiatal area 12 months after delivery, suggesting recovery [24].
Two studies evaluated the hiatal area, but not before and after delivery. Van Delft et al. compared hiatal areas with and without avulsion of the LAM and showed 21% LAM avulsion in women after VD. There was no avulsion after CS. The LAM avulsion was associated with a smaller hiatal area during pregnancy in the VD group [26].
Siafarikas et al. associated the hiatal area with major and minor defects of the muscle and found 44 out of 234 women with major LAM defects with VD. Only 5 women had CS (2.1%), and none had major LAM defects. Smaller levator hiatus areas in pregnancy are associated with major levator defects. Women with a major LAM defects were more likely to have an instrumental VD than a normal VD [25].
Bladder neck
Four articles evaluated bladder neck [17, 24, 27, 28], of which 3 evaluated bladder neck mobility [17, 24, 27] and 1 evaluated bladder neck elevation [28]. The first three articles showed a significant increase in bladder neck mobility, and one showed a decrease in bladder neck elevation [17] associated with VD. According to Staer-Jensen et al., bladder neck mobility was significantly higher at 12 months postpartum than at 37 weeks’ gestation in VD women. There was no difference for CS [24]. Another author showed that there was more displacement in the VD group (0.42 ± 0.30 cm to 0.58 ± 0.64 cm) than in the cesarean group (0.39 ± 0.30 cm to 0.47 ± 0.33 cm), but there was no difference between the two groups 1 year after delivery (0.59 ± 0.64 cm in the vaginal group and 0.47 ± 0.33 cm in the cesarean group, p = 0.16) [27].
One article that evaluated the angle of the bladder neck showed that VD was associated with a change in the position of the bladder neck by 6 weeks postpartum. The bladder neck analysis was performed using an x-y coordinate system, as described by Peschers et al. [29]. The bladder neck changed from 93° to 84° in VD and appeared to recover to the antenatal position by 6 months. The differences in bladder neck mobility degrees between VD and CS were +18.38 (p < 0.001) and +8.54 (p = 0.093) [28].
Another article showed a reduction in the average bladder neck elevation from antepartum to postpartum (3.3 ± 3.2 mm to 2.3 ± 2.2 mm, p = 0.001) that was not associated with delivery mode [17].
LAM injury
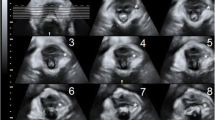
Three of the six articles included an evaluation of LAM injuries [25,26,27]. All articles used the criteria proposed by Dietz et al. [30] to define LAM injuries using tomographic imaging of the axial plane at maximal LAM contraction. Major defects in the medial part of the LAM were diagnosed when an abnormal insertion of the muscle into the pubic bone was present in all three central slices at the plane of minimal dimension and at 2.5 and 5.0 mm cranially to it. Minor defects were diagnosed when an abnormal insertion of the muscle into the pubic bone was present, but not in all three central slices. The three articles showed an association between VD and LAM injury.
Siafarikas et al. evaluated major defects of the LAM 6 weeks postpartum. Major defects were diagnosed in 44 women (18.8% of all 234 deliveries), of whom 14.4% had a VD, and there were no major LAM defects in the 5 women with second-stage CS. The most important finding of the study by Siafarikas et al. was that women who presented major defects in the postpartum period had a smaller hiatal area at rest and during the Valsalva maneuver during the gestational period, which indicates that a smaller hiatal area can be a risk factor for muscle lesions. Women with and without major defects showed a levator hiatus area of 10.84 ± 1.84 and 11.90 ± 2.25 cm2 (p = 0.005) at 21 weeks of pregnancy and 16.34 ± 5.08 and 19.18 ± 6.12 cm2 (p = 0.005) at 37 weeks’ pregnancy respectively [25].
Van Delft et al. [26] also showed that women who underwent CS did not present avulsion. Twenty-one percent of women who underwent VD presented avulsion; 4.9% presented minor avulsion, and 16.1% presented major avulsion. The study also concluded that a smaller hiatal anteroposterior diameter during the antenatal period increases the risk for postnatal LAM avulsion. The anteroposterior diameter was 5.7 ± 0.7 (no avulsion group), 5.2 ± 0.8 (minor avulsion group), and 5.3 ± 0.9 (major avulsion group). Van Delft et al. assessed pelvic floor muscle strength by digital palpation using the modified Oxford scale. Antenatal and postnatal pelvic floor muscle strength was significantly lower in women with minor and major avulsion (3.0 and 2.4 respectively) than in women without LAM avulsion (3.6 and 3.1 respectively). Women with avulsion are less sexually active before and after delivery and have more urinary incontinence symptoms, reduced vaginal sensation, and a “loose vagina.” No postnatal differences were found for fecal incontinence, prolapse symptoms or quality of life [26].
A study by Chan et al. showed that 19% of women had a LAM injury 8 weeks after VD, which decreased to 15.1% 12 months after delivery. VD and LAM injuries were factors associated with irreversible hiatal distension at rest with ORs 3.10 (1.277–7.58, p = 0.013) and 7.19 (3.45-–4.97, p < 0.005) respectively [27].
Discussion
This systematic review showed that LAM injury evaluated by 3D ultrasound was associated with VD. The LAM is the largest component of the pelvic floor, and its lesions can be implicated in some dysfunctions, such as POP, urinary incontinence, and sexual complaints [4, 31].
This systematic review concluded that VD had a close relationship with imaging defect and no one article included in this review showed imaging defect with CS, reinforcing the current state of literature knowledge. Additionally, one-third of women with lesions have decreased muscle strength [32]. The study by van Delft et al. included in this review supports these data, showing decreased muscle strength in women with major and minor lesions in the postpartum period [26].
All six studies included in this systematic review showed that there is an increase in the hiatal area after delivery, especially if associated with VD. LAM defects are associated with enlargement of the genital hiatus after delivery. In cases of levator injury, the genital hiatus may increase 20–30% in size [13]. Enlargement of the hiatal area has been associated with POP and symptoms [33]. However, this systematic review was not able to reach a consensus on the resolution of the enlargement of the hiatal area in the postpartum period. One of the studies included [24] showed that there is resolution of the genital hiatus 6–12 months after delivery and another study showed that the hiatal area was persistently larger in the VD group than in the CS group [27]. Two studies also showed resolution of the genital hiatus size in the first 6 months postpartum [34, 35].
During VD, the levator ani is extended by approximately 25–245%, allowing the levator hiatus to widen during crowning [17, 18, 36]. This distension can result in a LAM injury and is a risk factor for levator hiatus “ballooning,” which may be associated with POP [20]. One study included in this systematic review showed that ballooning is more prevalent 6 months after VD than after CS [25].
Regarding the hiatal area, a small area during pregnancy was associated with a greater risk for LAM injury in two studies included in this review, because this requires the LAM to stretch more to allow the passage of the fetus [25, 26]. This is a topic that should be better studied in future articles. Neither of these two articles [16, 25] showed that there is a threshold for hiatus size that indicates a greater chance of a lesion.
This systematic review showed increased urethral mobility after delivery, corroborating current knowledge. Additionally, this systematic review showed that there is a recovery 6–12 months after delivery. The study by Staer-Jensen et al. showed resolution of bladder neck mobility 6 months postpartum [24], and the study by Chan et al. supported these data. There was greater bladder neck mobility 8 weeks after delivery in the VD group, but there was no difference between VD and CS at 6 and 12 months postpartum [27]. Other articles in the literature support these findings [27, 37,38,39].
With regard to CS, the literature is divergent regarding the increase in urethral mobility after this delivery route. Staer-Jensen et al. showed that there is no increase in bladder neck mobility after CS [24]. Unlike the genital hiatus, there is no consistency in the resolution of urethral hypermobility after delivery, which shows that the effect of pregnancy on urethral mobility may be persistent [40] and explains that there may also be increased mobility in women who underwent a CS.
The 3D ultrasound was chosen in this study because it is more accessible than magnetic resonance imaging (MRI). A recent systematic review showed that translabial 3D ultrasound is reproducible for diagnosing levator ani defects and a ballooning hiatus in a population with PFD [41]. Translabial 3D ultrasound is non-invasive and by far the easiest, cheapest, and most widely available imaging modality at present. One study showed that translabial ultrasound results are consistent with the MRI results [42].
The strengths of this systematic review consist in the inclusion of studies with only primigravida, as the number of deliveries is a risk factor for pelvic floor trauma. Prospective studies were included to evaluate the reversibility of the damage found. We also included studies with at least one 3D ultrasound examination to identify the PFM during pregnancy, and at least one examination in the postpartum period as pregnancy could also be a risk factor for pelvic floor trauma. For weaknesses, we found that only 3 of the 6 included studies followed women for more than 6 months postpartum. More studies with longer follow-up are required. Also, the heterogeneity of results was mitigated by inclusion of primiparous women, to avoid measurement complexity arising from multiple births. Because this article has included only primiparous women, the results could not be generalizable. Another point is the potential bias inherent in the original studies. The ratio of VD/CS births differs and this must represent a difference in patient populations and/or obstetric practices. Finally, the relevance of ultrasound findings is not clearly established. Although levator enlargement is consistent after VD and biologically plausible as a contributing factor to prolapse, the association has not yet been proven to relate to causation.
Conclusions
Vaginal delivery was associated with an increased number of LAM defects, bladder neck mobility, and enlargement of the hiatal area, posing a risk factor for prolapses and urinary incontinence. There are insufficient data to determine whether post-partum ultrasound changes may resolve over time.
References
Dietz HP. Pelvic floor trauma in childbirth. Aust N Z J Obstet Gynecol. 2013;53(3):220–30.
Nygaard I, Barber MD, Burgio KL, Kenton K, Meikle S, Schaffer J, et al. Prevalence of symptomatic pelvic floor disorders in US women. JAMA. 2008;300(11):1311–6.
Shamliyan T, Wyman J, Bliss DZ, Kane RL, Wilt TJ. Prevention of urinary and fecal incontinence in adults. Evid Rep Technol Assess (Full Rep). 2007;161:1–379.
Progetto Menopausa Italia Study Group. Risk factors for genital prolapse in non-hysterectomized women around menopause. Results from a large cross-sectional study in menopausal clinics in Italy. Eur J Obstet Gynecol Reprod Biol. 2000;93(2):135-40.
Mant J, Painter R, Vessey M. Epidemiology of genital prolapse: observations from the Oxford family planning association study. Br J Obstet Gynaecol. 1997;104(5):579–85.
MacLennan AH, Taylor AW, Wilson DH, Wilson D. The prevalence of pelvic floor disorders and their relationship to gender, age, parity and mode of delivery. BJOG. 2000;107(12):1460–70.
Kisli E, Kisli M, Agargun H, Altinokyigit F, Kamaci M, Ozman E, et al. Impaired function of the levator ani muscle in the grand multipara and great grand multipara. Tohoku J Exp Med. 2006;210(4):365–72.
Bim CR, Perego AL, Pires-Jr H. Fisioterapia aplicada à ginecologia e obstetrícia. Cesumar. 2002;4(1):57–61.
Lukacz ES, Lawrence JM, Contreras R, Nager CW, Luber KM. Parity, mode of delivery, and pelvic floor disorders. Obstet Gynecol. 2006;107(6):1253–60.
Herbert J. Pregnancy and childbirth: the effects on pelvic floor muscles. Nurs Times. 2009;105(7):38–41.
Staer-Jensen J, Siafarikas F, Hilde G, Bø K, Engh ME. Ultrasonographic evaluation of pelvic organ support during pregnancy. Obstet Gynecol. 2013;122:329–36.
Dietz HP. Levator function before and after childbirth. Aust N Z J Obstet Gynaecol. 2004;44(1):19–23.
Otcenasek M, Krofta L, Baca V, Grill R, Kucera E, Herman H, et al. Bilateral avulsion of the puborectal muscle: magnetic resonance imaging-based three-dimensional reconstruction and comparison with a model of a healthy nulliparous woman. Ultrasound Obstet Gynecol. 2007;29(6):692–6.
Jou IM, Lai KA, Shen CL, Yamano Y. Changes in conduction, blood flow, histology, and neurological status following acute nerve-stretch injury induced by femoral lengthening. J Orthop Res. 2000;18(1):149–55.
Dietz HP, Wilson PD. Childbirth and pelvic floor trauma. Best Pract Res Clin Obstet Gynaecol. 2005;19(6):913–24.
Shek KL, Dietz HP. Pelvic floor ultrasonography: an update. Minerva Ginecol. 2013;65(1):1–20.
Dixit P, Shek KL, Dietz HP. How common is pelvic floor muscle atrophy after vaginal childbirth? Ultrasound Obstet Gynecol. 2014;43(1):83–8.
Shek KL, Dietz HP. Intrapartum risk factors for levator trauma. BJOG. 2010;117(12):1485–92.
DeLancey JO, Morgan DM, Fenner DE, Kearney R, Guire K, Miller JM, et al. Comparison of levator ani muscle defects and function in women with and without pelvic organ prolapse. Obstet Gynecol. 2007;109:295–302.
Dietz HP, Simpson JM. Levator trauma is associated with pelvic organ prolapse. BJOG. 2008;115(8):979–84.
Schwertner-Tiepelmann N, Thakar R, Sultan AH, Tunn R. Obstetric levator ani muscle injuries: current status. Ultrasound Obstet Gynecol. 2012;39(4):372–83.
Moher D, Liberati A, Tetzlaff J, Altman DG. Systematic reviews and meta-analyses: the PRISMA statement. Annu Intern Med. 2009;151(4):264–9.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomized studies of interventions. BMJ. 2016;355:i4919.
Staer-Jensen J, Siafarikas F, Hilde G, Benth JS, Bo K, Engh ME. Postpartum recovery of levator hiatus and bladder neck mobility in relation to pregnancy. Obstet Gynecol. 2015;125(3):531–9.
Siafarikas F, Staer-Jensen J, Hilde G, Bø K, Ellström Engh M. The levator ani muscle during pregnancy and major levator ani muscle defects diagnosed postpartum: a three- and four-dimensional transperineal ultrasound study. BJOG. 2015;122(8):1083–91.
Van Delft K, Sultan AH, Thakar R, Schwertner-Tiepelmann N, Kluivers K. The relationship between postpartum levator ani muscle avulsion and signs and symptoms of pelvic floor dysfunction. BJOG. 2014;121(9):1164–71. discussion 1172
Chan SSC, Cheung RYK, Yiu KW, Lee LL, Chung TKH. Pelvic floor biometry in Chinese primiparous women 1 year after delivery: a prospective observational study. Ultrasound Obstet Gynecol. 2014;43(4):466–74.
Toozs-Hobson P, Balmforth J, Cardozo L, Khullar V, Athanasiou S. The effect of mode of delivery on pelvic floor functional anatomy. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(3):407–16.
Peschers U, Schaer GN, DeLancey JO, Schussler B. Levator ani function before and after childbirth. Br J Obstet Gynaecol. 1997;104:1004–8.
Dietz HP, Bernardo MJ, Kirby A, Shek KL. Minimal criteria for the diagnosis of avulsion of the puborectalis muscle by tomographic ultrasound. Int Urogynecol J. 2011;22(6):699–704.
Jelovsek JE, Barber MD. Women seeking treatment for advanced pelvic organ prolapse have decreased body image and quality of life. Am J Obstet Gynecol. 2006;194(5):1455–61.
Braekken IH, Majida M, Ellstrøm-Engh M, Dietz HP, Umek W, Bø K. Retest and intra-observer repeatability of two-, three- and four-dimensional perineal ultrasound of pelvic floor muscle anatomy and function. Int Urogynecol Pelvic Floor Dysfunct. 2008;19(2):227–35.
Glazener C, Elders A, Macarthur C, Lancashire RJ, Herbison P, Hagen S, et al. Childbirth and prolapse: long-term associations with the symptoms and objective measurement of pelvic organ prolapse. BJOG. 2013;120(2):161–8.
Yousuf AA, DeLancey JO, Brandon CJ, Miller JM. Pelvic structure and function at 1 month compared to 7 months by dynamic magnetic resonance after vaginal birth. Am J Obstet Gynecol. 2009;201(5):514.e1–7
Tunn R, DeLancey JO, Howard D, Thorp JM, Ashton-Miller JA, Quint LE. MR imaging of levator ani muscle recovery following vaginal delivery. Int Urogynecol J Pelvic Floor Dysfunct. 1999;10(5):300–7.
Svabik K, Shek KL, Dietz HP. How much does the puborectalis muscle have to stretch in childbirth? Ultrasound Obstet Gynecol. 2008;32:395.
Shek KL, Kruger J, Dietz HP. The effect of pregnancy on hiatal dimensions and urethral mobility: an observational study. Int Urogynecol J. 2012;23(11):1561–7.
Wijma J, Potters AE, de Wolf BT, Tinga DJ, Aarnoudse JG. Anatomical and functional changes in the lower urinary tract following spontaneous vaginal delivery. BJOG. 2003;110(7):658–63.
Shek KL, Dietz HP, Kirby A. The effect of childbirth on urethral mobility: a prospective observational study. J Urol. 2010;184(2):629–34.
Dietz HP, Lanzarone V. Levator trauma after vaginal delivery. Obstet Gynecol. 2005;106(4):707–12.
Notten KJB, Vergeldt TFM, van Kuijk SMJ, Weemhoff M, Roovers JWR. Ultrasound for the assessment of levator ani defects and levator ani biometry in women with pelvic organ prolapse: a systematic review. Female Pelvic Med Reconstr Surg. 2017;23(6):420–8.
Yan Y, Dou C, Wang X, Xi Y, Hu B, Ma L, et al. Combination of tomographic ultrasound imaging and three-dimensional magnetic resonance imaging-based model to diagnose postpartum levator avulsion. Sci Rep. 2017;7(1):11235.
Funding
We are grateful to Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) for the support of this study with a post-graduate scholarship to one of the authors (CCA), and Fundação de Amparo a Pesquisa do Estado de São Paulo (FAPESP 2016/24065-2).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
de Araujo, C.C., Coelho, S.A., Stahlschmidt, P. et al. Does vaginal delivery cause more damage to the pelvic floor than cesarean section as determined by 3D ultrasound evaluation? A systematic review. Int Urogynecol J 29, 639–645 (2018). https://doi.org/10.1007/s00192-018-3609-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-018-3609-3