Abstract
Introduction and hypothesis
There is a lack of epidemiological studies evaluating female pelvic organ prolapse in developing countries. Current studies have largely focused on women of white ethnicity. This study was designed to determine interethnic variation in pelvic floor functional anatomy, namely, levator hiatal distensibility and pelvic organ descent, in women with symptomatic pelvic organ prolapse in a multi-ethnic South African population.
Methods
This prospective observational study included 258 consecutive women referred for pelvic organ prolapse assessment and management at a tertiary urogynaecological clinic. After a detailed history and clinical examination, including POPQ assessment, patients underwent a 4D transperineal ultrasound. Offline analysis was performed using 4D View software. Main outcome measures included levator muscle distensibility, pelvic organ descent, and levator ani defects (avulsion).
Results
Mean age was 60.6 (range, 25–91) years, mean BMI 29.83 (range, 18–53). Points Ba and C were lower and the genital hiatus more distensible in black women (all p < 0.05). They were found to have greater hiatal area (p = 0.017 at rest, p = 0.006 on Valsalva) compared with South Asians and whites and showed greater pelvic organ mobility (all p < 0.05) than Caucasians on ultrasound. Levator defects were found in 32.2% (n = 83) of patients and most were bilateral (48.2%, n = 40), with significant interethnic differences (p = 0.014).
Conclusion
There was significant variation in clinical prolapse stage, levator distensibility, and pelvic organ descent in this racially diverse population presenting with pelvic organ prolapse, with South Asians having a lower avulsion rate than the other two ethnic groups (p = 0.014).
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Interethnic differences are well documented for the bony anatomy of Homo sapiens. The bony skull, and more recently the pelvis, are most commonly used to determine biological affinity, i.e. gender and ethnicity in forensic anthropology and archaeology. Measurements of bony pelvic dimensions suggest that ethnicity might be determined with high accuracy (88%) [1,2,3]. Patriquin et al. studied consistent bony landmarks in os coxae of 100 white and black South African women of known age, sex, and ethnicity, and found statistically significant differences in 12 out of 13 measurements, i.e. white women had greater pelvic dimensions than black women, suggesting that ethnic differences in the bony pelvis might be highly significant [4].
Recently, there has been interest in studying the potential impact of ethnicity on the development of pelvic floor dysfunction (PFD) and variations in obstetric outcomes. Magnetic resonance imaging (MRI) and four-dimensional transperineal ultrasound (4D TPUS) studies have shown that there are significant ethnic differences in the female pelvic architecture as regards bony and soft-tissue pelvic dimensions and pelvic floor function [5,6,7].
Handa et al. compared soft-tissue dimensions between 178 Caucasian and 56 African–American primiparous women using MRI at 6–12 month postpartum. Apart from finding significant differences in both the pelvic inlet and outlet measurements (greater in Caucasian women), African–American women had statistically significantly greater pelvic floor descent measured by calculating the difference in descent of the posterior rectal wall from the pubococcygeal line on straining [8].
In a group of 207 asymptomatic nulliparous women, we have recently shown that, compared with white and South Asian women, black nulliparous women had statistically significantly greater levator distensibility and pelvic organ descent of the anterior, middle and posterior compartments as measured on 4D TPUS [9]. Similarly, Shek et al. have shown that there are significant differences in pelvic organ support and levator hiatal distensibility between black Ugandan and white nulliparous women using 4D TPUS [10]. This has not been tested in women with symptomatic pelvic organ prolapse (POP). The clinical significance of observed differences may well suggest that different pathophysiological mechanisms might exist in women with POP of different ethnicities that need further exploration.
The primary objective of this study was to prospectively analyse biometric indices of functional pelvic floor anatomy on clinical examination and pelvic floor ultrasound (hiatal distensibility and pelvic organ descent) in a multi-ethnic South African population presenting with symptomatic POP.
Materials and methods
This study was conducted at the Steve Biko Academic Hospital tertiary urogynaecology clinic and included 263 women presenting with symptomatic female POP from June 2013 to March 2015. The hospital is located in an urbanised city and is the major referral centre for the province. After informed consent was obtained, clinical examination using the pelvic organ prolapse quantification system of the International Continence Society (ICS POP-Q) and completion of the International Consultation on Incontinence Modular Questionnaire Vaginal Symptoms (ICIQ-VS) questionnaire, all women had a pelvic floor assessment using 4D transperineal ultrasound using a GE Voluson i ultrasound system with a 8- to 4-MHz curved array volume transducer (GE Kretz Ultrasound, Zipf, Austria) as previously described [11, 12]. The acquisition angle was set at 85° to include the entire levator hiatus. For analysis of the central compartment, we excluded women after hysterectomy as imaging of the vault has yet to be validated. Data on ethnicity was self-reported.
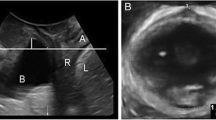
The ultrasound methodology, in addition to offline volume analysis, has been described in detail for the same cohort in a previous study evaluating the association between pelvic floor symptoms and functional pelvic floor anatomy [13]. Ultrasound volumes were de-identified and analysed 6–8 weeks later using proprietary software 4D View version 10. Figure 1 is a schematic representation illustrating descent of the pelvic organs on Valsalva relative to the inferior margin of the pubic symphysis.
Multi-slice or tomographic imaging was obtained in the axial plane, with the interslice interval set at 2.5-mm intervals from 5 mm below to 12.5 mm above the plane of minimal hiatal dimensions, as described previously. Levator avulsion was diagnosed by visualising detachment of the pubovisceral muscle form the pelvic sidewall in the rendered axial volumes obtained at maximal pelvic floor muscle contraction (PFMC), or in volumes obtained at rest in those unable to contract (n = 22) [14, 15]. Figure 2 demonstrates a bilateral levator avulsion on tomographic ultrasound.
This study was approved by the local Human Research Ethics Committee, University of Pretoria (226/2011). Statistical analysis was performed after normality testing (Kolmogorov–Smirnov testing) using IBM SPSS statistics v23 (IBM Corporation). To compare ethnic differences among the three groups, one-way analysis of variance (ANOVA) was performed and necessary adjustments for age, BMI, parity and previous prolapse surgery were controlled for in the analysis of covariance (ANCOVA). Pairwise comparison for ethnicity was performed using Bonferroni statistics. Fisher’s exact test was used for comparing the prevalence of avulsion between ethnicities. A p value <0.05 was considered statistically significant. Our null hypothesis was defined as “there is no ethnic variation in levator muscle distensibility, levator avulsion and pelvic organ descent in women presenting for symptoms of prolapse”.
Results
Two hundred and fifty-eight women were included in the analysis after excluding 5 cases because of missing data. The mean age was 60.6 (range, 25–91) years, mean vaginal parity was 3.6 (range, 0–9) and mean BMI 29.8 (range, 18–53). This study consisted of a racially diverse cohort, i.e. 12% Asian (n = 31), 41.5% black (n = 107) and 46.5% white (n = 120). Table 1 shows the demographic characteristics for the entire population and for the three ethnic groups.
Black women were significantly more vaginally parous (p = 0.001); previous prolapse procedures were more often reported by white women (p = 0.001).
Table 2 shows the results of POP-Q coordinates on clinical examination. There were significant differences between the ethnicities studied, specifically for the anterior (Ba; p = 0.048) and central compartment (C; p = 0.001), in addition to genital hiatus and perineal body measurements (p = 0.001). Post hoc test confirmed that the differences observed between blacks and whites regarding the anterior compartment, point C and genital hiatus (Gh) + perineal body (Pb) were statistically significant.
On 4D ultrasound volume data acquisition, 4 women were unable to produce a proper Valsalva manoeuvre, despite coaching, leaving 254 datasets for levator distensibility/area assessment. Black women were found to have statistically significantly greater hiatal areas at rest (p = 0.017) and on Valsalva (p = 0.006) compared with Asians and whites. Bonferroni post-hoc test revealed that this difference was mainly between blacks and South Asians for both rest (p = 0.01) and Valsalva volumes (p = 0.006). Black women showed greater pelvic organ descent on Valsalva in all three compartments (all p < 0.05) and these differences in descent seen on imaging were mainly between black and white women. Exclusion of women with previous prolapse surgery did not materially change these results.
Levator defects were found in 32.3% (n = 83) of patients and most were bilateral (48.2%, n = 40). Table 3 shows ethnic variations in levator distensibility, pelvic organ descent and avulsion, as examined by translabial ultrasound. South Asians showed a lower avulsion rate than the other two ethnic groups (P = 0.014 on Fisher’s exact test). The mean Oxford scores were significantly lower in those women with an avulsion (mean, 1.62 [right], 1.71 [left] compared with those without, i.e. 2.58 (right) and 2.57 (left; p = 0.001).
For the analysis of symptoms, we tested positive responses to “most of the time” and “all of the time” of the ICIQ-VS questionnaire. The major core symptoms reported were for questions 4a (do you feel that your vagina is too loose or lax?); 5a (are you aware of a lump or bulge coming down in your vagina?; 6a (do you feel a lump or bulge come out of your vagina, so that you can feel it on the outside or see it on the outside?); and 8a (do you have to insert a finger into your vagina to help empty your bowels?), and the results are as follows: 70.5% (n = 182), 79.8% (n = 206), 71.3% (n = 184), 21.3% (n = 55) respectively. There were no statistically significant interethnic differences in the prevalence of symptoms.
Discussion
Pelvic organ prolapse (POP) is a significant health problem in developing countries, with an estimated mean prevalence of 19.7% (range 3.4–56.4%) [16,17,18]. However, most clinical and imaging studies on morphological changes of the pelvic floor musculature focus on nulliparous and multiparous white women presenting with pelvic floor dysfunction [7, 19,20,21].
Current studies on ethnicity emphasise epidemiological findings (i.e. prevalence and risk factors), as opposed to functional anatomical assessment. To our knowledge, this is the first study evaluating clinical and pelvic floor functional anatomy in a racially diverse South African population presenting with symptomatic POP. Furthermore, it includes a large cohort of black women (41.5%, n = 107), thus illustrating that FPOP is common in this ethnic group. Although it has been shown that age, parity, menopause, assisted delivery, and levator trauma are significantly associated with pelvic floor dysfunction, it is likely that women in developing countries are exposed to other potential risk factors for pelvic floor dysfunction, such as heavy lifting, younger age at first delivery, early resumption of household duties postpartum, poor nutrition and lower annual household income. Proper identification and description of these potentially modifiable risk factors may require further study.
The epidemiological evidence for the role of ethnicity as a potential risk factor for POP has long been debated and is conflicting. Hendrix et al. and Whitcomb et al. reported that African–American women demonstrated the lowest risk for POP compared with whites and other ethnic minorities (Hispanic, Asian and American–Indian) [22, 23]. In contrast, Bump found a similar prevalence of POP for black and white women referred for a urogynaecological evaluation (24 vs 23% respectively) [24]. Graham and Mallett evaluated the effect of ethnicity on POP and UI in 183 symptomatic African–Americans and 132 Caucasians, and found no significant ethnic difference in the presence and severity of POP [25]. Although this scientific debate on the ethnic distribution of POP continues, we have noted higher POP-Q stage compared with developed countries, with more than a third of symptomatic patients (36.4%) presenting with POP-Q stage 3 prolapse [26]. In a Caucasian exclusive cohort (n = 270), 25.2% had the leading edge of the prolapse at or below the hymen, in contrast to our mixed population with the leading edge of the prolapse at almost +2 cm for the anterior compartment and +1 cm for the middle and posterior compartments [27]. This implies that patients present to our clinic with higher stages of prolapse than in developed countries, which is likely due to the nature of healthcare services in South Africa and/or other factors mentioned earlier.
With regard to avulsion, most studies in this field have reported on whites [28, 29]. The similar avulsion rates for whites (34.2%) and blacks (35.5%) is an interesting finding. The lower prevalence in South Asians is intriguing and may be due to a surprisingly low number of vaginally assisted deliveries in this group. We intend to study this issue in more detail in the future. As regards the reported symptoms, we have recently shown that there is a significant association between core prolapse symptoms, i.e. awareness, visualisation and/or feeling of a vaginal lump, levator hiatal distensibility and levator avulsion [13].
Limitations of the study include the fact that ultrasound acquisition and clinical examination were both performed by the first author (ZA). To overcome this potential bias for the analysis of imaging data, volumes were de-identified during acquisition and only analysed 6–8 weeks later, blinded against all clinical data, including ethnicity. Hence, the ultrasound data presented here should not be confounded by assessment bias, as the evaluation of imaging data was blinded against ethnicity. The congruence of imaging and clinical findings, incidentally, argues against any such bias. The impact of higher socio-economic class, educational level, employment status, and differential access to primary care are various forms of selection bias that need to be further explored.
In conclusion, we have found significant ethnic differences in clinical prolapse stage, levator distensibility and pelvic organ descent. Possible reasons include differences in bony pelvis, genetic inheritance of collagen endowment, lifestyle, nutritional factors and labour. POP is common in African–African women and to date this topic has been inadequately studied. The role of levator avulsion in the pathogenesis of prolapse is unlikely to vary greatly among the ethnicities examined, although interethnic differences deserve further study.
References
Howells WW, Hotelling H. Measurements and correlations on pelves of Indians of the South West. Am J Phys Anthropol. 1936;21:91–106.
Işcan MY. Assessment of race from the pelvis. Am J Phys Anthropol. 1983;62:205–8.
Steyn M, İşcan M. Metric sex determination from the pelvis in modern Greeks. Forensic Sci Int. 2008;179:86.e1.
Patriquin M, Loth S, Steyn M. Sexually dimorphic pelvic morphology in South African whites and blacks. Homo. 2003;53:255–62.
Derpapas A, Ahmed S, Vijaya G, Digesu GA, Regan L, Fernando R, et al. Racial differences in female urethral morphology and levator hiatal dimensions: an ultrasound study. Neurourol Urodyn. 2012;31:502–7.
Hoyte L, Schierlitz L, Zou K, Flesh G, Fielding JR. Two- and 3-dimensional MRI comparison of levator ani structure, volume, and integrity in women with stress incontinence and prolapse. Am J Obstet Gynecol. 2001;185:11–9.
Hoyte L, Thomas J, Foster RT, Shott S, Jakab M, Weidner AC. Racial differences in pelvic morphology among asymptomatic nulliparous women as seen on three-dimensional magnetic resonance images. Obstet Gynecol. 2005;193:2035–40.
Handa VL, Lockhart ME, Fielding JR, Bradley CS, Brubaker L, Cundiff GW, et al. Racial differences in pelvic anatomy by magnetic resonance imaging. Obstet Gynecol. 2008;11:914–20.
Abdool Z, Dietz HP, Lindeque GB. Are there ethnic differences in the levator hiatus and pelvic organ descent? A prospective observational study ultrasound. Obstet Gynecol. 2016; doi:10.1002/uog.17297.
Shek KL, Krause HG, Wong V, Goh J, Dietz HP. Is pelvic organ support different between young nulliparous African and Caucasian women? Ultrasound Obstet Gynecol. 2016;47:774–778. doi:10.1002/uog.15811.
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175:10–7.
Price N, Jackson SR, Avery K, Brookes ST, Abrams P. Development and psychometric evaluation of the ICIQ vaginal symptoms questionnaire: the ICIQ-VS Br. J Obstet Gynecol. 2006;113:700–12.
Abdool Z, Dietz HP, Lindeque BG. Prolapse symptoms are associated with abnormal functional anatomy of the pelvic floor. Int Urogynecol J Pelvic Floor Dysfunct. 2017; doi:10.1007/s00192-017-3280-0.
Dietz HP, Bernardo MJ, Kirby A, Shek KL. Minimal criteria for the diagnosis of avulsion of the puborectalis muscle by tomographic ultrasound. Int Urogynecol J Pelvic Floor Dysfunct. 2011;22:699–704.
Dietz HP, Pattillo Garnham A, Guzman Rojas R. Is it necessary to diagnose levator avulsion on pelvic floor muscle contraction? Ultrasound Obstet Gynaecol. 2015;49(2):252–6. doi:10.1002/uog.15832.
Bonetti TR, Erpelding A, Pathak LR. Listening to “felt needs”: investigating genital prolapse in western Nepal. Reprod Health Matters. 2004;12:166–75.
Walker GJ, Gunasekera P. Pelvic organ prolapse and incontinence in developing countries: review of prevalence and risk factors. Int Urogynecol J Pelvic Floor Dysfunct. 2011;22:127–35.
Wang J, Cao D, Zhang X. The prevalence of urinary incontinence and pelvic organ prolapse and its effects on the life quality of women in Beijing suburb. Chin J Clin Obstet Gynecol. 2007;8:5–9.
Reed H, Freeman R, Waterfield A, Adekanmi O. Prevalence of bladder neck mobility in asymptomatic non-pregnant nulliparous volunteers. Br J Obstet Gynaecol. 2004;111:172–5.
Dietz H. Do Asian women have less pelvic organ mobility than Caucasians? Int Urogynecol J Pelvic Floor Dysfunct. 2003;14:250–3.
Kruger JA, Dietz HP, Murphy BA. Pelvic floor function in elite nulliparous athletes. Ultrasound Obstet Gynecol. 2007;30:81–5.
Hendrix SL, Clark A, Nygaard I, Aragaki A, Barnabei V, McTiernan A. Pelvic organ prolapse in the women’s health initiative: gravity and gravidity. Obstet Gynecol. 2002;186:1160–6.
Whitcomb EL, Rortveit G, Brown JS, Creasman JM, Thom DH, Van Den Eeden SK, et al. Racial differences in pelvic organ prolapse. Obstet Gynecol. 2009;114:1271–7.
Bump RC. Racial comparisons and contrasts in urinary incontinence and pelvic organ prolapse. Obstet Gynecol. 1993;81:421–5.
Graham CA, Mallett VT. Race as a predictor of urinary incontinence and pelvic organ prolapse. Obstet Gynecol. 2001;185:116–20.
Abdool Z, Swart P. Symptomatic pelvic organ prolapse: experience at a tertiary urogynaecology clinic. S Afr J Obstet Gynaecol. 2016;22:18–20.
Nygaard I, Bradley C, Brandt D. Pelvic organ prolapse in older women: prevalence and risk factors. Am J Obstet Gynecol. 2004;104:489–97.
Dietz HP. The prevalence of major abnormalities of the levator ani in urogynaecological patients. BJOG. 2006;113:225–30.
Kearney R, Miller J, Ashton-Miller J, Delancey J. Obstetric factors associated with levator ani muscle injury after vaginal birth. Obstet Gynecol. 2006;107:144–9.
Acknowledgements
The authors would like to thank Professor Piet J Becker (PhD), Faculty of Health Science, University of Pretoria, for assistance with statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
HP Dietz has received unrestricted educational grants from GE Medical. The other authors declare that they have no conflicts of interest.
Previous presentation
NA
Rights and permissions
About this article
Cite this article
Abdool, Z., Dietz, H.P. & Lindeque, B.G. Interethnic variation in pelvic floor morphology in women with symptomatic pelvic organ prolapse. Int Urogynecol J 29, 745–750 (2018). https://doi.org/10.1007/s00192-017-3391-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-017-3391-7