Abstract
Introduction and hypothesis
We compared the clinician’s ability to cut episiotomies at the recommended 60° angle with traditional straight Mayo scissors compared with patented fixed-angle episiotomy scissors EPISCISSORS-60® in a simulated setting using mounted incision pads. The hypothesis was that fixed-angle episiotomies would achieve a more accurate cutting angle of 60°.
Methods
Angles were cut on episiotomy incision pads in a mounted birth model simulating crowning: 110 midwives and doctors cut an 60° episiotomy with Mayo scissors and then EPISCISSORS-60. Angles were measured with protractors. Average angles were calculated and the one-tailed paired t test was used to compare groups.
Results
Mean angle was 45° with Mayo scissors [SD = 9, 95% confidence interval (CI) = 43.3–46.7, interquartile range (IQR) 38–50] and 60° with the EPISCISSORS-60 (SD = 3, 95% CI = 59.3–60.7, IQR = 58–60). Two-thirds of cuts with Mayo scissors were below 50°.
Conclusions
In a simulated setting the majority of operators are unable to cut an episiotomy at the recommended 60° angle with Mayo scissors. The EPISCISSORS-60 cut an episiotomy a statistically significant 15° wider than regular Mayo scissors and achieved the recommended 60° in the vast majority of cases. If these findings translate into real life situations, then cutting episiotomies at 60° is expected to make a valuable contribution in reducing third- and fourth-degree tears in both spontaneous and operative vaginal deliveries. Variability in mediolateral episiotomies should be reduced by use of fixed-angle scissors or through validated health professional training programmes to improve visual accuracy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstetric anal sphincter injuries (OASIS), a serious complication of childbirth, are the leading cause of anal incontinence in women and are reported 6.1% of first vaginal births, with their incidence tripling between 2000 and 2012 [1]). OASIS has huge implications on women’s quality of life (QoL) and carries an enormous financial burden. The main consequence is faecal incontinence. In a recent study, 9% of women reported faecal incontinence at 24 weeks postpartum [2], and it may affect up to 25–30% of women in the year following delivery [3, 4]. In addition, OASIS has significant emotional and psychological consequences [5] and causes postpartum sexual dysfunction [6] and ongoing perineal pain [7]. Financial costs are associated with secondary repair, long-term care and increase caesarean section rate in future pregnancies. In addition, in their report of 10 years of claims, the National Health Service Litigation Authority (2012) cites OASIS as being the fourth largest cause of faecal incontinence in women [8]. These consequences are present when OASIS is recognised and a primary repair is performed, thus putting the onus on prevention rather than recognition and treatment.
In their guideline for managing third- and fourth-degree tears, the Royal College of Obstetricians and Gynaecologists (RCOG) lists the following risk factors for OASIS: Asian ethnicity, nulliparity, birthweight greater than 4 kg, shoulder dystocia, occipitoposterior position, prolonged second stage of labour and instrumental delivery [9]. Most of these factors are fixed and, other than limiting the duration of the second stage of labour, not amenable to change. The search for effective strategies to reduce OASIS has therefore intensified in recent years, and one possible strategy could be an increased role for episiotomies. Although their role in OASIS prevention has been controversial and is not routinely recommended, Gurol-Urganci et al. [1] found that episiotomy was protective for OASIS. The possible reasons for the existing controversy are twofold. Firstly, there are two main types of episiotomy: mediolateral, as favoured in Europe, with an OASIS risk of 2%; and the midline episiotomy, as favoured in the USA, with an OASIS risk between 12 and 20% [10, 11]. Secondly, for mediolateral episiotomies to be effective, they must be cut at an appropriate angle. Kalis et al. [12] found that an episiotomy angle <45° increases the risk of OASIS. and Stedenfeldt et al. (2012) [13] reported that >60° fails to relieve pressure on the perineum and increases OASIS risk. Eogan et al. (2006) [14] found that if the post-suturing angle was 25°, the incidence of OASIS was 10%. The incidence decreased by 50% for every 6° the episiotomy was cut away from the midline and achieved a minimum incidence of 0.5% at a postsuturing angle of 43°.
A further important aspect is the difference between the angle at which the episiotomy is cut during childbirth and the angle of the episiotomy after suturing. As the episiotomy is cut on a sphere when the fetal head is crowning, there will be a difference between cutting and suturing angles when the perineum recedes to a plane. When the episiotomy is cut at 40°, the resulting suturing angle is 22°. To achieve a postsuturing angle of 45°, the episiotomy at time of crowning needs to be angled at 60° [15]. This is also the recommendation in the RCOG Green Top Guideline 29 for managing third- and fourth-degree tears [15]. However, both doctors and midwives are relatively inept at estimating and cutting episiotomies at the desired angle. In model situations, only 12–15% of clinicians are able to cut at the recommended angle [16, 17] and in real life situation no midwife and 22% of doctors are able to cut a true mediolateral episiotomy [18].
It appears that true mediolateral episiotomies are protective for OASIS but that only a minority of episiotomies are actually cut at the recommended angle, thus depressing the true effect episiotomies could have on the incidence of the OASIS. To reduce the human error in cutting episiotomies, a team led by Professor Robert Freeman developed the EPISCISSORS-60® (Medinvent Ltd, Romsey, Hampshire, UK).
Materials and methods
Materials
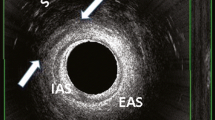
EPISCISSORS-60® are designed to achieve a true mediolateral cut of 60° and differ from regular scissors in two major ways. Firstly, they have a guide limb in the vertical angle comprising a stiff but mobile spring with a blunt end to prevent injury. When this guide limb is pointed towards the anus at crowning, the scissors will cut at a fixed 60° angle. Secondly, the scissors initiate the cut 5 mm away from the midline in the vertical plane, and as Stedenfeldt et al. [13] demonstrated, for each 4.5 mm an episiotomy is cut away from the midline, OASIS reduces relatively by a further 56%. A recent study shows that using EPICISSORS in in a real-life setting results in a significant majority of episiotomies being cut between 40 and 60° and a significant reduction in OASIS in nulliparous spontaneous vaginal deliveries [19] (Fig. 1).
To introduce these scissors into clinical practice, a practical training programme was designed to provide all clinical staff with a theoretical framework around OASIS and the practical skills necessary to use the scissors. Clinical decision to perform an episiotomy in real life remained with the operators. Two hospitals in the UK were awarded an innovation grant to introduce this programme: Poole Hospital (Poole, UK) and Hinchingbrooke Hospital (Huntington, UK). As part of this training programme, a trial was carried out in which clinicians were asked to cut a 60° episiotomy on a model mimicking a perineum with a crowning head first using regular Mayo scissors and then EPISCISSORS-60.
Methods
Two NHS consultant-led maternity units commenced implementing the training programme called Strategy for Prevention of OASIS using Practical Aids, Recording Episiotomies and Clinicians Training (SUPPORT) and introduced the EPISCISSORS-60 into clinical practice. All clinical operators using episiotomies in their practices were enrolled in the SUPPORT programme and included all midwifes, student midwifes, obstetric consultants and obstetric trainees working in the department. The training programme covered a summary of the scientific literature on perineal body length, nature of perineal distension from the first stage of labour to crowning, risk factors for OASIS, relationship of episiotomy angles with OASIS, recent advances in manual perineal protection, and comparison of OASIS rates in spontaneous tears and episiotomies. All participants were invited to measure perineal body lengths and to cut episiotomies on the training model at the conclusion of the session. The training model was adapted from Silf et al. [8] using the Keele and Staffs episiotomy trainer, Limbs and Things (UK). Incision pads were mounted using Velcro strips to the episiotomy trainer with the foetal head in situ. The mounted model was placed in the standing position. It was designed to simulate the distended perineum at crowning with 7 cm of the foetal head seen. Clinicians were encouraged to cut as per their normal practice. Most clinicians inserted one to two fingers of the nondominant hand between the foetal head and perineum while inserting the scissors blades. The were instructed to first cut an episiotomy at 60° with a straight Mayo scissors and then with EPISCISSORS-60. The model was positioned as per the individual clinician’s choice, i.e. at eye level or on a table. Angles were measured with transparent protractors and recorded. A 2° margin of error was regarded as inherent and acceptable in manual measurements. Both instructor and clinician were required to agree on recorded angles, which were noted on a paper data collection form. Means, medians, standard deviations (SD), 95% confidence intervals (CI) and interquartile ranges (IQR) were calculated. Difference in means was calculated using the one-tailed paired-sample t test. The study was approved by the local research and development department; as it involved a simulated setting, no ethical approval was required.
Results
The training programme was addended by 110 doctors and midwives. Distribution of professional experience is given in Table 1. Clinicians achieved an average angle of 45° when asked to cut at 60° with straight scissors (SD = 9, 95% CI = 43.3–46.7, IQR 38–50): five (4.7%) were able to cut between 58 and 62° and 14% between a wider clinical range of 55–65° (inclusive). There was no statistically significant relationship between level of experience and ability to cut a true mediolateral episiotomy with Mayo scissors. The average angle achieved with the EPISCISSORS-60 was 60° (SD = 3, 95% CI = 59.3–60.7, IQR = 58–60)., demonstrating a statistically significant 15° difference where the EPISCISSORS-60 showed a consistent episiotomy angle of 60° (p = 0.0001). Detailed results are given in Table 2. responses in shown in both tables do not add up to 110, as some participants did not mention their professional status and some did not return their angle measurements as requested on the data collection forms.
Discussion
In a birth simulation model, despite being prompted to cut at 60°, two thirds of clinicians cut <50° (30–50°) using straight scissors. In real-life situations, these episiotomies would result in suture angles of 0–35° based on perineal distension data of 15–30°. This would place them at clinically significantly higher risk of OASIS. In contrast, EPISCISSORS-60 episiotomies were cut consistently around the 60° angle. In real life, these would result in a postsuturing angle of ∼45° and should in theory result in a significantly reduced OASIS rate. We did not measure the distance from posterior fourchette or episiotomy length, as these factors are influenced by the stretchiness of the foam and are therefore not reliable measurements in a model situation. In addition, we did not analyse episiotomy angle data by professions, as there is no evidence that visual accuracy is inherently superior in any one professional group.
In addition, an important aim of this study was for clinicians to discover for themselves the difference in accurately achieving the intended episiotomy angle with each type of scissors. We recognise that this is an unavoidable weakness in this study but not to the extent where it would invalidate results.
Our results are important, as there appears to be abundant emphasis on suturing episiotomies in the general training of clinicians but very little attention to cutting them at the correct angle in the first place. This study also demonstrates that clinicians, when using regular Mayo scissors and eyeballing the angle, are generally unable to cut the episiotomy at a clinically beneficial angle. The limitation of this study is that it was done in a simulated environment, and although recent studies have shown a reduction in third- and fourth-degree tears when using EPISCISSORS in real life, further research is needed.
Conclusion
EPISCISSORS-60 allow clinicians to consistently cut episiotomies at 60°, the angle at which the risk of OASIS is significantly reduced. In view of the increasing OASIS rate and all its implications for QoL, healthcare finance and litigation, this could be an important weapon in the arsenal to bring this rate down. It is, of course, vital to demonstrate that using the EPISCISSORS-60 will indeed result in a lower OASIS rate.
References
Gurol-Urganci I, Cromwell DA, Edozien LC, Mahmood TA, Adams EJ, Richmond DH. Third- and fourth-degree perineal tears among primiparous women in England between 2000 and 2012: time trends and risk factors. BJOG. 2013;120:1516–25.
Richter HE, Nager CW, Burgio KL, et al. Incidence and predictors of anal incontinence after obstetric anal sphincter injury in primiparous women. Female Pelvic Med Reconstr Surg. 2015;21:182–9.
Fitzpatrick M, O’Herlihy C. Short-term and long-term effects of obstetric anal sphincter injury and their management. Curr Opin Obstet Gynecol. 2005;17:605–10.
Oberwalder M, Connor J, Wexner SD. Meta-analysis to determine the incidence of obstetric anal sphincter damage. Br J Surg. 2003;90:1333–7.
Keighley MR, Perston Y, Bradshaw E, Hayes J, Keighley DM, Webb S. The social, psychological, emotional morbidity and adjustment techniques for women with anal incontinence following Obstetric Anal Sphincter Injury: use of a word picture to identify a hidden syndrome. BMC Pregnancy Childbirth. 2016;16(1):275.
Signorello L, Harlow B, Chekos A, Repke J. Postpartum sexual functioning and its relationship to perineal trauma: a retrospective cohort study of primiparous women. Am J Obstet Gynecol. 2001;184:881–90.
Macarthur AJ, Macarthur C. Incidence, severity and determinants of perineal pain after vaginal delivery: a prospective cohort study. Am J Obstet Gynecol. 2004;191(4):1199–204.
National Health Service Litigation Authority. Ten years of maternity claims: an analysis of NHS litigation authority data. NHSLA, 2012.
RCOG Greentop guideline 29: the management of Third- and Fourth-Degree Perineal tears: RCOG June 2015. www.rcog.org.uk.
Coats PM, Chan KK, Wilkins M, Beard RJ. A comparison between midline and mediolateral episiotomies. Br J Obstet Gynaecol. 1980;87:408–12.
Signorello LB, Harlow BL, Chekos AK, Repke JT. Midline episiotomy and anal incontinence: retrospective cohort study. Br Med J. 2000;320(7227):86–90.
Kalis V, Karbanova J, Horak M, et al. The incision angle of mediolateral episiotomy before and after repair. Int J Gynaecol Obstet. 2008;103:5–8.
Stedenfeldt M, Pirhonen J, Blix E, Wilsqaard T, Vonen B, Qian P. Episiotomy characteristics and risks for obstetric anal sphincter injury: a case–control study. BJOG. 2012;119:724–30.
Eogan M, Daly L, O’Connell PR, O’Herlihy C. Does the angle of episiotomy affect the incidence of anal sphincter injury? BJOG. 2006;113:190–4.
Kalis V, Landsmanova J, Bednarova B, et al. Evaluation of the incision angle of mediolateral episiotomy at 60 degrees. Int J Gynaecol Obstet. 2011;112:220–4.
Silf K, Woodhead N, Kelly J, Fryer A, Kettle C, Ismail KMK. Evaluation of accuracy of mediolateral episiotomy incisions using a training model. Midwifery. 2015;31(1):197–200
Naidu M, Kapoor DS, Evans S, Vinayakarao L, Thakar R, Sultan AH. Cutting an episiotomy at 60 degrees: how good are we? Int Urogynecol J. 2015;26(6):813–6
Andrews V, Thakar R, Sultan AH, Jones PW. Are mediolateral episiotomies actually mediolateral? BJOG. 2005;112:1156–8.
Van Roon Y, Kirwin C, Rahman N, Vinayakarao L, Kester N, Pathak S, et al. Comparison of obstetric anal sphincter injuries in nulliparous women before and after introduction of the EPISCISSORS-60® at two hospitals in the United Kingdom. Int J Womens Health. 2015;7:949–55.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
van Roon, Y., Vinayakarao, L., Melson, L. et al. Comparative study of episiotomy angles achieved by cutting with straight Mayo scissors and the EPISCISSORS-60 in a birth simulation model. Int Urogynecol J 28, 1063–1066 (2017). https://doi.org/10.1007/s00192-016-3227-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-016-3227-x