Abstract
Introduction and hypothesis
Our objective was to assess episiotomy technique used in Israeli hospitals, to determine factors influencing incision parameters, and to review relevant up-to-date professional literature.
Methods
Using anonymous questionnaires, a survey was conducted among obstetricians and midwives in the four public hospitals in northern Israel over a 1-year period commencing in October 2013. In addition to demographic and professional data, the accoucheurs were asked to describe the technique they usually use to perform an episiotomy (length, angle, and distance of initiation point from midperineum).
Results
Overall, 84 obstetricians and 32 midwives participated in the survey. Only 37.6 % reported performing a mediolateral episiotomy, while the rest described the lateral type, placing the initiation point at an average distance of 2.45 ± 0.88 cm from the fourchette. Compared with midwives, obstetricians reported performing a significantly longer episiotomy (3.53 ± 1.01 vs. 2.73 ± 0.81 cm, p = 0.0002).
Conclusions
According to our study and relevant literature review, the technique of episiotomy varies significantly between health professionals and is not uniformly congruent with international practice guidelines. In part, this is derived from unclear literature evidence and lack of consensus definition for proper technique of this procedure by the national guidelines. Thus, further higher-quality research, uniform protocols, and educational programs are needed to guide episiotomy practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
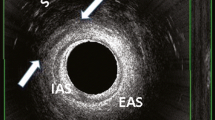
Episiotomy is one of the most prevalent surgical interventions in the delivery room, ranging in frequency from about 10 % and up to 75 % [1–3]. The three main parameters can be used to characterize this incision are length, angle to the vertical axis, and distance of initiation point from midperineum. Since median episiotomy commences at midperineum and continues downwards at 90°, the incision can vary only by its length. Mediolateral episiotomy incision, beginning at midperineum and directed laterally and downward, may also vary by its angle. Lateral episiotomy, commencing laterally to midline, can differ between obstetricians in the definition of its length, angle, and incision initiation point [4].
Despite the commonness of this procedure, the accepted national guidelines provide no flawless definition for technique. The American College of Obstetricians and Gynecologists (ACOG) notes that mediolateral episiotomy is an incision at least 45° from the midline [5]. Similarly, the Royal College of Obstetricians and Gynecologists (RCOG) recommends mediolateral episiotomy performance originating at the vaginal fourchette with a 45–60° angle [6]. The guidelines do not mention the length of mediolateral or median incisions or refer to lateral type. These inconsistencies lead to differences in episiotomy performance between personal obstetrical members. For instance, it has been shown that physicians perform longer and higher-angled episiotomies compared with midwives [7, 8]. These differences are important not only for statistical description purposes but mainly because of their potential effect on delivery outcomes. Decreased angle of mediolateral episiotomy has been linked to a higher risk of obstetric anal sphincter injuries (OASIS) [9], while longer and deeper episiotomies located further from the midperineum have been shown to reduce this risk in spontaneous vaginal deliveries [10] as well as in vacuum-assisted extraction [11].
Episiotomy type reported in Israel is mainly mediolateral, but no assessment of this procedure’s performance has yet been done in our country. Thus, the objectives of our study were to describe the technique of episiotomy performance in four Israeli hospitals, to evaluate possible factors influencing the incision parameters, and to review the relevant professional literature regarding this important issue.
Methods
This cross-sectional survey of midwives and obstetricians attending birth was conducted using an anonymous questionnaire at the obstetrics and gynecology departments of four public northern Israeli medical centers from October 2013 to September 2014. These hospitals contribute to approximately 14,000 deliveries annually (Carmel Medical Center, about 3,000 deliveries per year; Rambam Health Care Campus, 5,000 deliveries; Bnai Zion Medical Center, 3,000 deliveries; Baruch Padeh Medical Center, Poriya, 3,000 deliveries). Average [± standard deviation (SD)] episiotomy rates in these medical centers are 13.8 ± 5.4 %, with a 7.7 ± 3.0 % operative vaginal delivery rate, 19.8 ± 3.3 % cesarean delivery rate, and 0.6 ± 0.3 % OASIS rate. In Israel, the majority of normal vaginal deliveries are managed by midwives only, while obstetricians usually intervene in cases of complicated labor, such as fetal distress or operative vaginal deliveries. There are no formal guidelines for episiotomy performance, and the procedure is used according to the clinical judgment of the accoucheur attending the delivery.
The questionnaires were designed following guidance by an experienced epidemiologist. They were distributed during conventional departmental meetings and filled out by all presenting medical personnel, which constituted 65 % of total obstetric personnel. The questionnaire included the following questions: caregiver’s age, gender, and profession (midwife or obstetrician), duration (in years) of delivery room experience, and the main source of information regarding episiotomy technique (midwife/medicine studies, senior colleagues, professional literature, personal experience). The technique of episiotomy performance was evaluated by three parameters: approximate incision length in centimeters, cutting angle (by selection of one of the four categories: 0–20°, 20–40°, 40–60° or >60°), and incision initiation point (distance in centimeters from the midline of the fourchette).
Data was analyzed using SPSS software (SPSS Inc., Chicago, IL, USA). Continuous variables were presented as mean ± SD and compared using Student’s t test. Proportions were calculated for the remaining responses, as appropriate, and compared using Fisher’s exact test. To alleviate data interpretation and presentation, the cutting angle was divided into two groups (<40° vs. >40°), and the main source of information regarding episiotomy indications was presented as subjective vs. objective sources (subjective including personal experience and knowledge attained from senior colleagues, while objective was defined as midwife/medicine studies and professional literature). Subgroup analysis was performed for obstetricians vs. midwives, males vs. females, ≤15 years’ vs. >15 years’ professional experience, and subjective vs. objective main source of information regarding episiotomy indications; p < 0.05 was considered statistically significant for all comparisons.
Articles included in literature review were identified by searches of PubMed, the Cochrane Collaboration, and the Google search engine. Search terms and keywords were episiotomy AND (angle OR length OR lateral OR median OR midline OR mediolateral OR technique OR parameters). In addition, reference lists of the relevant articles were screened to ensure maximal literature coverage. No language or time restrictions were applied.
Results
A total of 117 questionnaires from the four hospitals were analyzed (72.4 % obstetricians and 27.6 % midwives). Characteristics of respondents including subgroup analysis are presented in Table 1. Of note, the main source of information regarding episiotomy technique was subjective, encompassing 26 (22.6 %) respondents basing their attitude on the experience of senior colleagues and 51 (44.3 %) on their personal experience. Only 14 (12.2 %) respondents relied on professional literature, and 24 (20.9 %) based their knowledge on midwife/medicine studies. Compared with midwives, doctors yielded a significantly higher proportion of male participants (60.5 % vs. 0 %, respectively, p < 0.0001) and of subjective rather than objective sources of education regarding episiotomy indications (73.1 % vs. 53.1 %, respectively, p = 0.047). Less experienced accoucheurs (≤15 years of professional experience) were younger (p < 0.0001) and demonstrated higher proportions of objective educational sources (41.5 % vs. 27.3 %, respectively, p = 0.027).
Table 2 shows parameters of episiotomy technique including subgroup analysis. According to the results, obstetricians reported performing significantly longer episiotomies compared with midwives (p = 0.0002). In addition, 90.9 % of accoucheurs with fewer than 15 years of professional experience performed the episiotomy >40°, compared with 64 % of their more experienced colleagues (p = 0.0005). Mediolateral episiotomy was performed in 37.6 % of cases, and in 93.5 % of cases, the incision angle was >40°, a significantly higher rate compared with lateral episiotomy (75.3 %, p = 0.023). None of the other examined factors (gender, profession, duration of professional experience, or type of experience acquisition) exhibited a significant influence on incision parameters.
Discussion and review of the literature
The first description of perineal incision was published in 1741 by Ould [12]. He suggested “an incision made towards the anus” in cases of extraordinary constriction of the external vaginal orifice, endangering the fetus by contraction of uterine cervix over the child’s neck. Presently, seven episiotomy types have been mentioned in the literature [4], the most commonly described and investigated being mediolateral and median. Lateral incision, commencing 1–2 cm from the midline and continuing toward the ischial tuberosity, is reported in several European countries. Although this type is rarely mentioned in the professional literature, its use appears to be surprisingly frequent [4]. In addition, many physicians perform incisions commencing some distance from midline and erroneously define this type as mediolateral [13]. In the first study relating to episiotomy trigonometric parameters, published in 2005 by Tincello et al., 50 physicians and 78 midwives were asked to depict on a two-dimensional drawing of the optimal mediolateral episiotomy they would make [14]. The results showed that about one third of respondents began the episiotomy laterally to the midline. Our study demonstrated that although the accepted episiotomy method in Israel is mediolateral, about two thirds of accouchers perform a lateral episiotomy. This finding by itself highlights the need for continuing education on the subject.
Obviously, the recommended episiotomy type should be the one associated with the lowest rates of delivery complications. It is well demonstrated and agreed upon by national guidelines that median episiotomy increases the risk of obstetric anal sphincter injuries (OASIS) [5]. However, very few studies had analyzed the consequences of mediolateral vs. lateral episiotomy (in fact, exploring the issue of incision-point location). A retrospective case–control trial by Stedenfeldt et al. compared episiotomy characteristics in 37 OASIS cases to 37 control deliveries. All participants were primiparous delivered during the previous 1–8 years [15]. These authors reported that increasing the distance from the posterior fourchette to the incision point of the episiotomy by 4.5 mm decreased OASIS risk by 56 % [odds ratio (OR) 0.44, 95 % confidence interval (CI) 0.23–0.86]. Fodstad et al. prospectively evaluated episiotomy characteristics 0–3 days after delivery in 300 participating women. The authors found that lateral episiotomies were neither associated with more perineal pain the first postpartum day nor with more blood loss compared with the mediolateral episiotomy techniques. However, mean incision-point distance to midline was significantly shorter among the 12 OASIS cases compared with women without OASIS (4.5 vs. 10.5 mm, respectively, p = 0.002) [7]. In a 3-month follow-up of 179 deliveries, the authors found no difference in perineal pain perception, dyspareunia, intercourse resumption, or perineal wound infection rates between mediolateral and lateral episiotomy types [16]. The authors noted that a lateral incision point was related to higher triggering of pain when walking (p = 0.037), but there was no significant difference between incision-point location for any other perineal pain-triggering situations. Only one randomized study exploring this issue has been published: Karbanova et al. compared perineal outcomes in 390 women with mediolateral episiotomy (directed at an angle of at least 60°) and 400 women with lateral (incision beginning 1–2 cm laterally from the midline and directed toward the ischial tuberosity) [17]. The researchers failed to show any difference in the incidence or extent of vaginal and perineal trauma and reported that mediolateral episiotomy was associated with shorter repair times, less suturing material, and shorter distances from the anus.
Angle of incision has been the most investigated trigonometric episiotomy parameter. Of note, below we discuss the noticeable variation in this angle in accordance with the timing of its measurement—whether at incision, during suturing, or after delivery; readers will notice the varying definitions used by different studies. Regarding episiotomy parameters, Tincello et al. reviewed the commonly used obstetric textbooks and concluded that the recommended incision angle for mediolateral episiotomy was 40–60°. However, these standard texts provided no evidence to support this practice [14]. The incision angle is the only parameter mentioned by the accepted national guidelines, which state that mediolateral episiotomy angle should be “of at least 45°”. More recent articles, including an excellent review by Kalis and Tincello et al., elevated the recommended incision angle to “at least 60° from the midline” [4], while an angle of 40° had become the optimal postsuturing cutoff [8]. Specialized and angled episiotomy scissors were recently introduced with the aim of maintaining the supposedly optimal 60° cutting angle [18, 19].
Indeed, the majority of responders in our study who reported using mediolateral episiotomy depicted an incision angle >40°. However, as shown by Wong et al., subjective angle assessments are inaccurate and may be higher than the actual angle used. These investigators asked 100 accoucheurs to describe the angle at which they would cut a mediolateral episiotomy and to depict this on a pictorial representation of the perineum [20]. Midwives depicted episiotomies 8° closer to the midline (37.6° vs. 44.9°, p = 0.013) than they described.
According to our study, duration of obstetric experience can affect the preferred incision angle, as more than one third of senior obstetricians with professional experience >15 years perform an acute-angled episiotomy (i.e., <40°), compared with only 10 % of their less experienced colleagues. One possible explanation could be the greater reliance of senior accoucheurs on their subjective experience rather than on evidence found in professional literature. This fact highlights the need for continuing education on this subject.
Our study is by no means the first to illustrate potential differences in episiotomy angle between different health professionals. The study by Tincello et al., using a pictorial questionnaire, demonstrated that more midwives use an episiotomy angled 30° or less, compared with obstetricians (23 % vs. 2 %, a statistically significant difference) [14]. The first clinical study aimed to objectively demonstrate genuine differences in episiotomy technique between obstetricians and midwives was published at 2005 by Andrews et al. [8]. Their prospective cohort study evaluated episiotomy characteristics in 241 deliveries immediately after suturing and demonstrated that obstetricians performed episiotomies that were significantly more obtuse from the midline than did midwives [median angle 27° (range 0–73.7) vs. 20.1° (range 12.8–38.7), respectively, p = 0.047]. Using a standard obstetric textbook definition of mediolateral episiotomy as incision of at least 40° from the midline, the authors showed that none of the episiotomies performed by midwives and only 22 % performed by obstetricians were actually mediolateral.
The importance of episiotomy angle lies in its possible effect on advanced perineal tears and other delivery complications. The first study aiming to determine the impact of episiotomy angle on anal sphincter injury was published in 2006 by Eogan et al. [21]. Their case–control study involved 100 primiparous women undergoing episiotomy within the previous 3 months, including 54 deliveries with third-degree perineal tears and 46 controls. Mean angle of episiotomy measured significantly smaller in OASIS cases (30°; 95 % CI 28–32°) than in controls (38°; 95 % CI 35–41°; p <0.001), and the association of episiotomy angle with risk of OASIS remained significant after adjustment for birthweight and mode of delivery. A prospective study published during the same year by Andrews et al. [9] included 241 primiparous women, with anal sphincter injuries diagnosed in 59 (25 %) deliveries. As opposed to the study by Eogan et al., episiotomy characteristics were measured in the lithotomy position immediately after suturing. Episiotomies angled closer to the midline were associated with advanced perineal tears (26° vs 37°, p = 0.01). However, a logistic regression containing three categories (no episiotomy, episiotomy < 40° or >40°) and adjusted for delivery mode did not yield statistical significance. In their case–control trial of 74 patients, examined several years after the delivery, Stedenfeldt et al. reported a U-shaped association between scar episiotomy angle and OASIS, with increased risk conferred by an angle of either <15° or >60° [15]. A matched case–control analysis of 72 operative vaginal deliveries by Gonzalez-Díaz et al. compared trigonometric characteristics of mediolateral episiotomy (measured at 8–12 weeks postpartum) in 36 primiparous women with OASIS and 36 control cases [11]. The authors showed that the risk of third-degree tear decreased substantially from 32.82 % in women with an angle of episiotomy <20° to 3.95 % in women with episiotomies >20°. Finally, the single randomized trial compared OASIS and short-term pain rates in 165 primiparous women who had the episiotomy made at an angle of 60° to the midline and 165 women with incision angle of 40° [22]. The study found no statistically significant difference in OASIS rates; however, a mediolateral episiotomy angled at 60° was associated with significantly higher rates of moderate/severe episiotomy-related postpartum pain.
In summary, the only available prospective study involving 241 women and evaluating episiotomy characteristics immediately after suturing did not demonstrate a significant relationship between episiotomy angle and OASIS. These results are supported by results of a single randomized trial. Three smaller case–control studies (100, 74, and 72 women, respectively), assessing episiotomy angle several weeks to years after delivery, have shown a significant association between more acute incision angle and OASIS. The findings should be interpreted cautiously due to inconsistent results, relatively low number of participants, and the fact that measurement of episiotomy angle after suturing cannot adequately represent the original incision angle. Kalis et al. prospectively examined 50 nulliparous women with episiotomy performed at a 40° angle to the midline [23]. The authors demonstrated that episiotomy angle at the time of repair was significantly lower than the incision angle—a decrease of 15° in cases in which episiotomy was performed during head crowning and by 10 % when it done before crowning (i.e., in cases of fetal distress). The same first author published an additional article in 2011, prospectively describing episiotomy characteristics in 60 primiparous women [24]. This time, the cut was at 60° during crowning, and the results demonstrated that the median suturing angle of these episiotomies decreased to 45° (p < 0.001). In the 46 women attending follow-up at 6 months postpartum, median scar angle was 48°. Of note, no anal sphincter injury was detected in the study group.
It is worth mentioning that, as opposed to mediolateral episiotomy, no studies have been published referring to the angle of a lateral incision. This lack of evidence may explain the significantly lower rates of >40° angle in respondents who reported using lateral episiotomy compared with mediolateral incision (75.3 % vs. 93.5 %). It is tempting to assume that these episiotomy methods do not differ in their effect on delivery complications and can be used interchangeably. However, as lateral episiotomy appears to be used much more frequently than previously thought, well-designed randomized trials are urgently needed to evaluate the importance of lateral incision angle.
Compared with episiotomy angle, length has been investigated far less frequently. According to our results, the accoucheur’s profession can affect this parameter as well, as obstetricians perform significantly longer incisions than do midwives (3.53 ± 1 vs. 2.73 ± 0.81, respectively). In Israel, as in many other countries, midwives generally assist uncomplicated vaginal birth, while obstetricians are responsible in cases of operative vaginal delivery. This fact may influence the accoucheur’s episiotomy method. Similar results have been reported by several other studies. For instance, Tincello et al., using a pictorial questionnaire, show that median episiotomy length drawn by obstetricians was 16 mm (8–31) compared with 14 mm (5–22) for midwives (p = 0.002) [14]. A study by van Dillen et al., prospectively evaluating 420 deliveries with episiotomy, shows that mean episiotomy length was 38.9 ± 8.4 mm, with no difference between obstetricians and midwives [25]. An interesting fact worth noting is the varying length of episiotomy between all these trials.
Several studies examined the clinical importance of episiotomy length. Fodstad et al. prospectively evaluated incision characteristics 0–3 days after delivery in 300 participating women and found no difference in perineal pain perception related to episiotomy length [7]. However, when analyzing episiotomy length as a continuous variable, the authors found a borderline significant p value of 0.06 for the relationship between this variable and postpartum blood loss. At 3 months postpartum follow-up of 179 deliveries, no association was shown between episiotomy length and perineal pain perception or intercourse resumption [16]. According to a retrospective case–control trial of 74 women by Stedenfeldt et al., a 75 % reduced risk (OR 0.25, 95 % CI 0.10–0.61) of obstetric anal injuries was found for each 5.5-mm increase in episiotomy length [15]. However, the prospective examination of 241 primiparous women by Andrews et al. and the case–control trial of 72 operative vaginal deliveries by Gonzalez-Díaz et al. demonstrated no significant association between episiotomy length and OASIS [9, 11]. No randomized controlled trials are as yet reported examining this important issue.
The value of our study is in being the first to describe in detail the episiotomy technique in several Israeli hospitals (a country with one of the lowest reported rates of OASIS worldwide) and in exploring the up-to-date literature evidence for optimal incision characteristics. The drawbacks of this study are its limited number of respondents, especially from the midwife sector, and the inability to ensure that respondents are representative of the general obstetric health providers in Israel. An additional problem, as with any survey-based research, lies in respondents’ subjective evaluation. Finally, our questionnaire did not assess additional episiotomy parameters, such as timing, incision depth, and distance from the anal orifice. These factors could also have clinical importance. For example, Stedenfeldt et al. demonstrated a 70 % decreased risk of OASIS for each 5.5-mm increase in episiotomy depth (OR 0.30; 95 % CI 0.14–0.66) [15]. Gonzalez et al. showed that mean episiotomy depth and distance between incision and anus were shorter in OASIS cases (11.96 and 13.39 mm) than in the control group (16.23 and 17.6 mm) [11]. Future randomized controlled trials should strive to examine these parameters as well.
Besides the continuing research, education of obstetric personnel and supervised episiotomy training are important. Wong et al. showed that obstetricians, after being supervised for at least ten mediolateral episiotomies, performed incisions that were in keeping with the angle they described, whereas those with less experience depicted episiotomies that were significantly more acute [20].
In conclusion, the optimal technique for performing an episiotomy varies significantly between health professionals and is not uniformly congruent with international practice guidelines. In part, this is derived from unclear literature evidence and lack of consensus definition by national guidelines regarding the most appropriate technique. Thus, further higher-quality research, uniform protocols, and educational programs are needed to guide episiotomy practice.
References
Seijmonsbergen-Schermers AE et al (2013) The use of episiotomy in a low-risk population in the Netherlands: a secondary analysis. Birth 40(4):247–255
Chalmers B et al (2012) Rates of interventions in labor and birth across Canada: findings of the Canadian maternity experiences survey. Birth 39(3):203–210
Frass KA, Al-Harazi AH (2010) Episiotomy is still performed routinely in Yemeni women. Saudi Med J 31(7):764–767
Kalis V et al (2012) Classification of episiotomy: towards a standardisation of terminology. BJOG 119(5):522–526
(2006) ACOG Practice Bulletin. Episiotomy. Clinical Management Guidelines for Obstetrician-Gynecologists. Number 71, April 2006. Obstet Gynecol, 107(4): p. 957–62
Intrapartum Care: Care of healthy women and their babies during childbirth. National Collaborating Centre for Women’s and Children’s Health (UK), 2007
Fodstad K, Laine K, Staff AC (2013) Different episiotomy techniques, postpartum perineal pain, and blood loss: an observational study. Int Urogynecol J 24(5):865–872
Andrews V et al (2005) Are mediolateral episiotomies actually mediolateral? BJOG 112(8):1156–1158
Andrews V et al (2006) Risk factors for obstetric anal sphincter injury: a prospective study. Birth 33(2):117–122
Kalis V et al (2012) Episiotomy characteristics and risks for obstetric anal sphincter injuries: a case-control study. BJOG 119(9):1147, author reply 1148-9
Gonzalez-Diaz E, Moreno Cea L, Fernandez Corona A (2015) Trigonometric characteristics of episiotomy and risks for obstetric anal sphincter injuries in operative vaginal delivery. Int Urogynecol J 26(2):235–242
Longo LD (1976) Classic pages in obstetrics and gynecology. A treatise of midwifery. In three parts by Sir Fielding Ould, Dublin, O. Nelson & C. Connor, 1742. Am J Obstet Gynecol 124(6):656
Kalis V et al (2008) Definitions of mediolateral episiotomy in Europe. Int J Gynecol Obstet 100(2):188–189
Tincello DG et al (2003) Differences in episiotomy technique between midwives and doctors. BJOG 110(12):1041–1044
Stedenfeldt M et al (2012) Episiotomy characteristics and risks for obstetric anal sphincter injuries: a case-control study. BJOG 119(6):724–730
Fodstad K, Staff AC, Laine K (2014) Effect of different episiotomy techniques on perineal pain and sexual activity 3 months after delivery. Int Urogynecol J 25(12):1629–1637
Karbanova J et al (2014) Clinical evaluation of peripartum outcomes of mediolateral versus lateral episiotomy. Int J Gynecol Obstet 124(1):72–76
Patel RP, Ubale SM (2014) Evaluation of the angled Episcissors-60((R)) episiotomy scissors in spontaneous vaginal deliveries. Med Devices (Auckl) 7:253–256
Freeman RM et al (2014) Cutting a mediolateral episiotomy at the correct angle: evaluation of a new device, the Episcissors-60. Med Devices (Auckl) 7:23–28
Wong KW et al (2014) Mediolateral episiotomy: are trained midwives and doctors approaching it from a different angle? Eur J Obstet Gynecol Reprod Biol 174:46–50
Eogan M et al (2006) Does the angle of episiotomy affect the incidence of anal sphincter injury? BJOG 113(2):190–194
El-Din AS, Kamal MM, Amin MA (2014) Comparison between two incision angles of mediolateral episiotomy in primiparous women: a randomized controlled trial. J Obstet Gynecol Res 40(7):1877–1882
Kalis V et al (2008) The incision angle of mediolateral episiotomy before delivery and after repair. Int J Gynecol Obstet 103(1):5–8
Kalis V et al (2011) Evaluation of the incision angle of mediolateral episiotomy at 60 degrees. Int J Gynecol Obstet 112(3):220–224
van Dillen J et al (2010) A prospective multicenter audit of labor-room episiotomy and anal sphincter injury assessment in the Netherlands. Int J Gynecol Obstet 108(2):97–100
Acknowledgments
We thank all midwives and obstetricians who participated in the study.
Conflicts of interest
None.
Author’s contribution to the manuscript
L. Sagi-Dain: Project development, data collection and analysis, manuscript writing
S. Sagi: Protocol development, data collection and management, manuscript editing.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sagi-Dain, L., Sagi, S. The correct episiotomy: does it exist? A cross-sectional survey of four public Israeli hospitals and review of the literature. Int Urogynecol J 26, 1213–1219 (2015). https://doi.org/10.1007/s00192-015-2680-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-015-2680-2