Abstract
Introduction and hypothesis
The urethral closure mechanism in women is incompletely understood. Measuring closure function in a collapsed urethral tube without distending the tube and changing its natural shape is impossible with conventional methods. Over the last decade, studies with urethral pressure reflectometry (UPR), a method that measures pressure and the corresponding cross-sectional area along the entire length of the urethra continuously by means of acoustic reflectometry, have been performed. The studies have mainly been performed on patients with stress urinary incontinence (SUI).
Methods
Our aim was to provide an overview of the studies conducted with UPR, establishing whether the method may be used in clinical practice. We reviewed all literature published on UPR.
Results
Urethral pressure reflectometry is easily performed with limited bother for the patient. The catheter consists of a 45-cm-long PVC tube connected to a thin and highly flexible polyurethane bag, which is placed in the urethra. When inserted, the bag only occupies 0.4 mm2 of the urethra, respecting the natural shape and orientation of the urethra and, most importantly; respecting the laws of physics when measuring urethral pressure. UPR can discriminate patients with SUI from continent women and separate assessment of the sphincter function and support system is possible. Also, UPR has revealed statistically significant differences in urethral pressures after drug therapy for SUI.
Conclusions
We conclude that UPR has a place in clinical practice. The method has shown groundbreaking potential in the understanding of urethral dysfunction in SUI patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The closure mechanism of the urethra in women, not to mention the diseases and dysfunctions of the organ, is still incompletely understood. To be able to understand a disease we have to understand the normal anatomy and function of the organs involved. This is essential for the successful treatment of any disease. To obtain more insight into a condition such as stress urinary incontinence (SUI), corresponding measurements of urethral pressure and cross-sectional area have been conducted [1]. Over 40 years ago, Susset et al. [2] demonstrated how patients with SUI could be treated based on their urodynamic results and introduced sphincter incompetence as a possible explanation for urethral dysfunction. In 1971, Harris et al. [3] proposed a system for cross-sectional area measurement in the ureter. Over the years, this idea has been the subject of several studies that all have attempted to develop a technique to enable the simultaneous measurement of pressure and cross-sectional area in a biological, collapsible tube [4–8]. In 1976, Rask-Andersen and Djurhuus [4] constructed a urethral probe that could measure both parameters consecutively. Mortensen et al. [9] modified the probe a few years later and in the 1980s, Colstrup et al. [5, 10, 11] succeeded in measuring pressure and cross-sectional area simultaneously in the resting urethra. Lose et al. [6] developed the technique further, enabling dynamic measurements in the urethra [1, 12]. The techniques described are still not commercially available; however, the simultaneous measurement of pressure and cross-sectional area has been carried out by conventional urethral pressure profilometry (UPP) using catheters of increasing size [13]. Unfortunately, measuring closure function in a collapsed urethral tube without distending the tube and changing its natural shape is impossible using any of the above-mentioned methods, including UPP, because of the use of rigid catheters. Furthermore, the risk of measurement artefacts is high both because the catheter is likely to move during the examination and because UPP requires withdrawal during the examination if urethral pressures along the entire length of the urethra are to be obtained [14, 15].
Urethral pressure reflectometry (UPR), a technique that emerged in 2005, circumvents the traditional pitfalls of urethral pressure measurements by using a thin and highly flexible polyurethane bag that occupies only 0.4 mm2 when placed in the urethra. UPR measures the urethral pressure and the cross-sectional area simultaneously. The cross-sectional area, which is the area of the opened lumen of the urethra, is measured continuously along the entire length of the urethra by means of acoustic reflectometry: a sound wave, generated outside the urethra, passes into the urethra where echoes arise. The echoes are then reflected and recorded, and the cross-sectional area is calculated [16]. As a result, the air pressure required to force the urethra open is the urethral pressure, which agrees with the physical definition of pressure [17].
Interestingly, UPR has shown groundbreaking potential as a diagnostic test for SUI. It can distinguish between women with and those without SUI [18]. The purpose of this review is to provide an overview of the studies conducted using UPR, establishing whether it has a place in everyday clinical practice.
The journey of acoustic reflectometry
Originally, acoustic reflectometry was developed for the analysis of the stratification of the earth’s crust [19]. In the 1960s, it was used in the search for oil, in the 1970s, it was further developed for the theoretical assessment of vocal tract shape and, finally, in the 1980s, the first study with reflectometry in humans was conducted [19–21]. In 2005, in vitro recordings with acoustic reflectometry in a collapsed tube were performed for the very first time [22]; subsequently, the technique was applied in women and measurements in the female urethra were conducted [16]. The technique was named urethral pressure reflectometry (UPR) and has been proven to be highly reproducible and accurate [23].
UPR: how does it work and what do we measure?
Urethral pressure reflectometry allows measurements at rest, and during squeezing and straining. A digital signal processor generates wide band sound waves (100 Hz to 16 kHz) which are transmitted via a probe into a catheter placed in the urethra (Fig. 1). The catheter is a 45-cm-long polyvinyl chloride tube connected to a thin and highly flexible polyurethane bag, which is inserted into the urethra using an introducer (Ch 8 feeding tube). Essentially, this is a catheter-free technique as the bag only occupies 0.4 mm2 when placed in the urethra. The bag is fixated to the external urethral meatus with a DuoDERM® plaster (Fig. 2). The bag is 6 cm long, has a wall thickness of 0.025 mm and a diameter of 5 mm when fully dilated. A microphone in the probe records the reflections from the urethra and relays them to a computer, which in turn converts the reflections and calculates the cross-sectional area. A transducer measures the pressure in the system and the computer registers it. Originally, a pump controlled the pressure [16], however, because of noise from the pump, which interfered with the acoustic reflectometry measurements, examinations had to be carried out stepwise. The pressure was increased to a certain level, the cross-sectional area was measured, and then the pressure was increased again. This continued until the bag was completely open. The examination took at least 90 s, which is longer than most women can squeeze. Consequently, measurements during squeezing had to be adapted; the squeeze had to be repeated at each pressure level and each squeeze at each pressure level could have been of a different strength and the patient could get fatigued. The UPR technique had to be modified; thus, a syringe was introduced into the system, instead of the pump. The syringe pumps air into the polyurethane bag, increasing the pressure, distending the bag, and thereby opening the urethra. The total measurement takes 7 s and so the woman only has to hold the squeeze for 7 s. Thus, UPR allows for the simultaneous measurement of pressure and cross-sectional area in the urethra at rest, and during squeezing and straining. Each examination measures up to 20 times per second. At rest, the patient is instructed to relax, the pressure in the polyurethane bag is increased until the bag is fully dilated and then the pressure is decreased again. During squeezing, the patient is told to squeeze and to hold the squeeze until the bag is opened. During straining, simultaneous abdominal pressure recordings are performed with an air-filled balloon catheter placed in the rectum (T-dock, Wenonah, NJ, USA). The patient is asked to strain and to hold the pressure until the bag is opened. Measurements are carried out ten times at different intensities [18, 24].
The catheter is connected to a polyurethane bag as displayed in the picture. The bag is inserted into the urethra using an introducer and fixates to the external urethral meatus with a DuoDERM plaster, also displayed. Finally, the introducer is removed and the catheter is loosely fixated to the patient’s inner thigh. The patient in this figure has given her written consent to the use of these photos in publications
Urethral pressure reflectometry enables continuous measurements (20 measurements per second) of the cross-sectional area along the entire length of the urethra (Fig. 3). However, only measurements from the high-pressure zone (HPZ) are used for further analyses as this is the position with minimal urethral cross-sectional area at a given pressure (Fig. 4) [16, 22].
The top three graphs show the cross-sectional area (y-axis) vs the distance into the urethra (x-axis). See Fig. 3. As the pressure in the system increases, the urethra opens. The circles mark the high-pressure zone. The bottom graph displays the urethral pressure (y-axis) vs the cross-sectional area (x-axis) and shows how the urethral high-pressure zone opens and closes and displays the parameters opening pressure, closing pressure, opening elastance, closing elastance, and hysteresis
Parameters
Measurements from the HPZ are plotted on a graph showing the cross-sectional area at increasing pressure levels (Fig. 4). Analysis of the graph reveals important parameters: five parameters at rest, two during squeezing, and three during straining.
Opening pressure (cmH2O) is measured as the air pressure needed to open the collapsed urethra, which agrees with the physical definition of pressure (Fig. 4) [17]. During rest, it is a measurement of the permanent closing forces provided from the surrounding submucosa, smooth muscle, striated muscle, fibroelastic structures, and neural stimuli, which enable the urethra to remain closed [1].
Opening pressure during squeezing, however, is an expression of the permanent closing forces and the voluntary sphincter function [25]. During straining, opening pressures are measured at different abdominal pressures, representing additional forces that act on the urethra during stress (see below).
Closing pressure (cmH2O) is the pressure at which the urethra closes subsequent to dilation (Fig. 4) [25].
Elastance is an object’s resistance to deformation when exposed to an external force. It simply determines how easily the urethra will open and close in response to a certain bladder pressure. In the urethra, it is measured as the relationship between pressure and the cross-sectional area. The opening elastance expresses the urethra’s resistance against dilation, whereas the closing elastance expresses the urethra’s ability to close against pressure (Fig. 4). Thus, a strong urethral sphincter has a high opening and closing elastance, whereas a urethral stricture has a high opening elastance and a low closing elastance [16, 25]. Opening elastance is measured at rest and during squeezing, whereas closing elastance is measured only at rest.
Hysteresis, measured only at rest, is an expression of energy loss in a structure during stretching. Each type of fiber in the body has its own hysteresis; variations in hysteresis may be expressions of different fibrous compositions. For instance, a high value may indicate fibrosis in the urethra. During UPR, the hysteresis is measured as the energy dissipated during inflation and deflation of the polyurethane bag, and is expressed as a percentage of energy loss (Fig. 4) [16]. However, hysteresis should be interpreted with caution after the introduction of the syringe because hysteresis depends on the speed at which the urethra opens, which may be subject to interpersonal variation when it comes to handling the syringe.
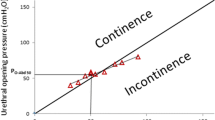
The abdominal to urethral pressure impact ratio (APIR) expresses the effect of increasing abdominal pressure on urethral pressure. Where opening pressure at rest is an expression of the permanent closing forces, APIR most likely represents the adjunctive closing forces that are recruited during stress such as straining, coughing, laughing, etc. (Fig. 5) [18]. Measurements during straining are carried out at different intensities and the related values of opening pressures and abdominal pressures are plotted into an abdomino-urethral pressuregram. The slope of the line expresses the APIR.
a The graphs show urethral pressure (y-axis) vs cross-sectional area (x-axis). The red dots are the opening pressures. Each graph displays the opening of the urethra at a given abdominal pressure (all from the same patient). As abdominal pressure increases, urethral pressure increases as well. b Abdomino-urethral pressuregram with opening pressures (y-axis) plotted against abdominal pressures (x-axis). The abdominal to urethral pressure impact ratio (APIR) and opening pressures at standardized abdominal pressures can be derived from this graph. The patient will become incontinent if the abdominal pressure exceeds the urethral pressure. The upper blue trace (crosses) is from a continent patient with a P O-Abd 50 of 123 cmH2O and the lower red trace (triangles) is from a patient with SUI; her P O-Abd 50 is 54 cmH2O. SUI stress urinary incontinence
P O-Abd 50 and P O-Abd 100, opening pressures at abdominal pressures of 50 cmH2O and 100 cmH2O respectively: these opening pressures express the combination of permanent and adjunctive closing forces at a particular abdominal pressure. The abdomino-urethral pressuregram allows for the calculation of opening pressures at standardized abdominal pressures, i.e., 50 cmH2O and 100 cmH2O (Fig. 5b) [18].
Areas investigated using UPR: what do we know so far?
The very first study with UPR was published in 2005 where in vitro recordings revealed that simultaneous measurements of pressure and cross-sectional area in a collapsed tube were in fact possible [22]. The technique was then applied in the female urethra and demonstrated how continuous measurements of pressure and cross-sectional area, along the entire length of the urethra, could be performed with a negligible influence on the urethra’s natural shape and orientation [16], as opposed to conventional methods of measuring urethral pressure [14, 15]. UPR has been compared with urethral pressure profilometry (UPP) in terms of reproducibility and applicability of results, with the results clearly in favor of UPR (Fig. 6) [23, 26].
Bland–Altman plot: the difference in two consecutive measurements of the urethral pressure reflectometry (UPR) and urethral pressure profilometry (UPP) respectively in 143 women is plotted against the mean urethral pressure. The variability (2 SD) was less with UPR (9.5 cmH2O) than with UPP (13.8 cmH2O); p < 0.001. Reprinted from Klarskov and Lose [23], with permission from Wiley, New York
In 2008, a comparative study by Klarskov and Lose demonstrated how opening pressures, at rest and during squeezing, measured with UPR are better at discriminating healthy women from those with SUI compared with conventional UPP [26]. Nonetheless, even UPR showed an overlap in resting opening pressures in women with and without SUI. However, this is probably a mere reflection of the complexity of SUI and its underlying causes. SUI has been described as being caused by either sphincter deficiency or urethral hypermobility, when, in fact a most patients probably have both to different extents [27, 28]. In 2013, Saaby et al. [18] conducted a unique study with 26 women with SUI and 10 controls. By introducing simultaneous abdominal pressure recordings they managed to examine the women with UPR during straining, giving rise to new and valuable parameters. Saaby et al. demonstrated that PO-Abd 50, the opening pressure at an abdominal pressure of 50 cmH2O, completely separated women with SUI from continent women and suggested that PO-Abd 50 might be used as a diagnostic test for SUI. PO-Abd 50 represents a combination of the permanent and adjunctive closing forces. It is a measurement of both sphincter function and the support system and thus allows for an assessment that covers the entire spectrum in SUI. The study also showed negative correlation between PO-Abd 50 and the International Consultation on Incontinence Questionnaire (ICIQ-SF) score, the pad test, and the number of incontinence episodes, suggesting that PO-Abd 50 might be used as a severity measure. This is the first urodynamic parameter that has ever been able to diagnose SUI and correlate it with patients’ symptoms. Table 1 provides an overview of all the parameters measured using UPR and what they each represent.
The introduction of tension-free vaginal tape (TVT) has drawn more attention to the support system [28]. However, because of a lack of reliable and objective measurements of the urethra, it has been challenging to establish how the TVT actually works. Therefore, Saaby et al. [29, 30] sought to find out if measurements made using UPR could reveal and explain the mechanism of TVT. They examined 22 patients before and after TVT surgery and found that both APIR and opening elastance increased after TVT placement, indicating that TVT enhances the adjunctive closing forces and enables the urethra to become more resistant against dilatation, which is in agreement with some previous studies [31–33]. Saaby et al. found no effect on resting urethral opening pressure, indicating that the increase in APIR compensates for a potentially low opening pressure in these patients. The authors hypothesized that a certain preoperative level of APIR might be able to predict postoperative success or failure.
The combination of urethral opening pressures and opening elastance provides a whole new multi-dimensional description of the urethral closure mechanism. Unlike UPP, UPR enables continuous measurements of increasing cross-sectional area, with corresponding pressure, during the opening of the urethra. Therefore, it can discriminate between different types of abnormal closure function and provide insight into specific conditions. In fact, Klarskov and Lose found that it is possible to distinguish between SUI women with a rigid urethra and SUI women with urethral hyperlaxity [16]. A rigid and fibrotic urethra will have a low opening pressure, but a high opening elastance as scar tissue has a high resistance toward the opening of the urethra. On the other hand, a woman with urethral hyperlaxity will have a low opening pressure and a low opening elastance (Fig. 7). It is plausible that the patient with a rigid urethra has intrinsic sphincter deficiency, a condition that is often considered synonymous with a low-pressure urethra [34]. However, Fig. 7 clearly depicts two patients with low-pressure urethras due to different types of urethral dysfunction who probably respond differently to treatment. The categorization of different types of urethral dysfunction is not possible using conventional UPP because it measures the urethral pressure at a specific cross-sectional area and the results depend on the size of the catheter used. Therefore, the differentiation of SUI patients with low-pressure urethras has not been possible before.
The UPR measurements of two patients with SUI: patient 1 had an opening pressure of 23.1 cmH2O and an opening elastance of 1.0 cmH2O/mm2, patient 2 had an opening pressure of 18.9 cmH2O and an opening elastance of 3.1 cmH2O/mm2. The measurements thus show that patient 1 had urethral hyperlaxity whereas patient 2 had a rigid urethra. The two patients were also examined using conventional UPP, with a Ch 8 catheter (5.1 mm2). UPP revealed almost identical maximum urethral pressures of 30 and 31 cmH2O in patients 1 and 2 respectively. Interestingly, the opening curves of both patients (the upper solid and dotted lines) cross each other at 5.1 mm2 during UPR measurements. This simply shows that it is impossible for UPP to discriminate between urethral hyperlaxity and a rigid urethra. Reprinted from Klarskov and Lose [16], with permission from Wiley, New York
The interaction between the bladder and the urethra is another interesting aspect in the mechanism of incontinence. In 2011, Saaby et al. [35] performed UPR and cystometry simultaneously in 18 women who had either SUI, urgency urinary incontinence with detrusor overactivity or were continent, with the intention of testing the feasibility of the setup. The authors found that it was possible to perform both examinations simultaneously, giving rise to new opportunities in examining the bladder and the urethra as a functional unit.
In 2008, the influence of injection therapy (for SUI treatment) on urethral function was investigated. The study included 15 women who all completed the ICIQ-SF. UPR was performed before and after treatment. Ten women reported subjective improvement after treatment and UPR revealed increased opening pressure during squeezing in the women compared with the remaining five who experienced no improvement. As a result, the authors concluded that bulking could improve the force of the urethral sphincter by increasing the urethra’s central filler volume [36].
Traditionally, clinical trials that evaluate the efficacy of a certain drug therapy use investigative tools such as diaries to assess the effect on incontinence episodes. Studies with UPP have attempted to see how the target organ, the urethra, in women with SUI is affected by drug therapy. Unfortunately, they have failed to show any effect on urethral pressure [37, 38]. However, studies with UPR have shown groundbreaking results. The first study conducted was a randomized, double-blinded, placebo-controlled crossover study with 4 mg of esreboxetine, a highly selective norepinephrine reuptake inhibitor. Patients were examined using UPR and UPP before and after treatment. The authors found that because of the higher reproducibility, UPR enables more efficient study designs with fewer subjects needed in a single study. They established an objective effect of esreboxetine by showing how opening pressure increased significantly in women with SUI in comparison with placebo treatment [39]. This finding was confirmed in a study with healthy volunteers using the same drug [40]. Recently, a randomized, double-blinded, placebo-controlled crossover study on the efficacy of fesoterodine, an antimuscarinic agent, in the treatment of SUI, was performed. Patients were again examined with UPR before and after treatment, only this time, the drug had no effect on urethral function [41]. Last, yet another randomized, placebo-controlled crossover study has shown how opening pressures increase after the administration of a single oral dose of duloxetine, midodrine or reboxetine [42].
All of the aforementioned studies on UPR have been conducted on women, with the female urethra being the target of investigation. However, two studies on UPR measurements in the male urethra have also been conducted and published. The authors of those studies argued that as passive mechanical obstruction may be of importance in patients with benign prostatic obstruction, UPR could reveal exactly where the urethra is obstructed, enabling more localized treatment with possibly less surgical trauma. The technique was proven feasible in terms of catheter insertion and measurement of parameters [43, 44]. It remains unclear whether UPR is of any importance in the preoperative assessment of patients with benign prostatic obstruction in terms of surgical techniques and postoperative outcomes.
The principles of UPR have been applied to anal measurements as well. In 2010, the first study with anal acoustic reflectometry (AAR) was published [45], and in 2011 its reproducibility for the assessment of anal sphincter function was verified [46]. AAR provides new insight into the anal continence mechanism. Like conventional methods, AAR reveals differences in the parameters of continent and incontinent patients. However, the parameters of AAR also correlate with the severity of fecal incontinence and the technique enables discrimination between the patterns of fecal incontinence [47, 48]. Furthermore, AAR has shown promising results as a predictor of successful treatment with sacral nerve stimulation, an established treatment option for fecal incontinence [49].
Complications and limitations
The value of objective examinations of the urethra has been limited because of the lack of reliable methods. UPP has been the method of choice so far, but the use of stiff catheters makes measurements in a collapsed urethral tube impossible. Whether using microtip transducers, water-perfused catheters or air-charged balloon catheters, the insertion of a stiff catheter will both dilate the urethra and change its natural shape, which is why measurements cannot represent actual urethral function. To obtain measurements throughout the entire urethral length, UPP requires withdrawal during the examination, which leads to movement artefacts [14, 15]. UPR circumvents all these pitfalls, has a higher reproducibility compared with UPP and, most importantly, respects the laws of physics, as it measures urethral pressure as the air pressure needed to force the urethra open.
Like any other technology, UPR also carries some limitations. If the bag is completely compressed the sound cannot be reflected from the area behind the compression. Therefore, as the bladder neck is distal to the HPZ, it cannot be measured accurately. Furthermore, sound may escape from the bag at very low pressures, leading to false measurements of the cross-sectional area at low pressures. To limit the impact of these artifacts, measurements up to a cross-sectional area of 1–2 mm2 are disregarded [16, 22].
Urethral pressure reflectometry has been proven to be less uncomfortable than both UPP and a standard gynecological examination [23]. The risk of urinary tract infection is the same as with any other invasive urodynamic investigation [39, 50], but there is no history of serious complications after UPR [25].
Conclusion
The implementation of a new investigation in any clinical setting has some requirements. The resources spent must be reasonable, taking into account the benefits of the examination. How does the new information help us to diagnose, treat or monitor a patient? Also, what are the risks and discomforts for the patients undergoing the investigation? Does the end justify the means? UPR allows for the mapping of urethral function and provides parameters that are reproducible and trustworthy. It is the only method that respects the laws of physics and, therefore, the first method to provide true urethral parameters such as urethral opening pressure. UPR is easily performed with limited bother for the patient, and the method circumvents the drawbacks of conventional methods. UPR has revealed some valuable and relevant parameters. The objective discrimination of patients with SUI is the first step toward revealing the underlying urethral dysfunction, which may be helpful when tailoring individual treatment modalities. It is now possible to assess the sphincter’s function and support system separately, which may be especially useful in complicated cases where treatment is unsuccessful or the patient experiences recurrent SUI. In addition, the evaluation of the bladder and the urethra as a functional unit provides a whole new dimension in the understanding of lower urinary tract function/dysfunction.
The introduction of acoustic reflectometry in the assessment of the anal sphincter has shown the diversity and possibilities of the technique. It is plausible for the technique to be applied in other organs, such as the uterus, where it may be of assistance in diagnosing cervical insufficiency, or in the esophagus, where it may be used to diagnose strictures. UPR allows for up to 20 measurements per second and, therefore, examination during a cough is theoretically possible. As some patients only experience incontinence during coughing or sneezing, examinations during these scenarios may be of clinical value. Whether or not UPR can provide reliable measurements under these circumstances remains to be elucidated.
Even though drug therapy has been available for the treatment of SUI for quite some time, no method has ever been able to establish an objective effect on the urethra. UPR provides a reliable and objective assessment of the urethra. It is now possible to measure how drug therapy affects the urethra and thereby obtain an objective evaluation of drug therapy. With the increasing interest in the treatment of voiding difficulties, UPR can be used to assess the effect of drug therapy for this condition, in addition to other conditions. Consequently, pharmaceutical companies may be able to develop more targeted and efficient drugs.
At the moment, UPR is not commercially available and has only been used for research purposes in three university departments (one gynecological, one urological, and one gastrointestinal department) and two phase I clinical trial units. However, there is great reason to believe in its clinical use, both in terms of feasibility and relevance in daily clinical practice.
References
Lose LG (1992) Simultaneous recording of pressure and cross-sectional area in the female urethra: a study of urethral closure function in healthy and stress incontinent women. Neurourol Urodyn 11:55–89. doi:10.1002/nau.1930110202
Susset JG, Shoukry I, Schlaeder G et al (1974) Stress incontinence and urethral obstruction in women: value of uroflowmetry and voiding urethrography. J Urol 111:504–513
Harris JH, Therkelsen EE, Zinner NR (1971) Electrical measurement of ureteral flow. In: Boyarsky S, Tanagho EA, Gottschalk CW, Zimskind PD (eds) Urodynamics. Academic Press, London, pp 465–472
Rask-Andersen H, Djurhuus JC (1976) Development of a probe for endoureteral investigation of peristalsis by flow velocity and cross section area measurement. Acta Chir Scand Suppl 472:59–65
Colstrup H, Mortensen SO, Kristensen JK (1983) A probe for measurements of related values of cross-sectional area and pressure in the resting female urethra. Urol Res 11:139–143
Lose G, Colstrup H, Saksager K, Kristensen JK (1986) New probe for measurement of related values of cross-sectional area and pressure in a biological tube. Med Biol Eng Comput 24:488–492
Gregersen H, Andersen MB (1991) Impedance measuring system for quantification of cross-sectional area in the gastrointestinal tract. Med Biol Eng Comput 29:108–110
Andersen IS, Gregersen H, Buntzen S et al (2004) New probe for the measurement of dynamic changes in the rectum. Neurogastroenterol Motil 16:99–105
Mortensen S, Djurhuus JC, Rask-Andersen H (1983) A system for measurements of micturition urethral cross-sectional areas and pressures. Med Biol Eng Comput 21:482–488
Colstrup H, Mortensen SO, Kristensen JK (1983) A new method for the investigation of the closure function of the resting female urethra. J Urol 130:507–511
Colstrup H (1984) Rigidity of the resting female urethra. II. Dynamic measurements. J Urol 132:82–86
Thind P (1995) The significance of smooth and striated muscles in the sphincter function of the urethra in healthy women. Neurourol Urodyn 14:585–618
Thind P, Lose G, Colstrup H (1991) How to measure urethral elastance in a simple way. Elastance: definition, determination and implications. Urol Res 19:241–244
Schäfer W (2001) Some biomechanical aspects of continence function. Scand J Urol Nephrol Suppl 35(207):44–60; discussion 106–125
Weber AM (2001) Is urethral pressure profilometry a useful diagnostic test for stress urinary incontinence? Obstet Gynecol Surv 56:720–735
Klarskov N, Lose G (2007) Urethral pressure reflectometry; a novel technique for simultaneous recording of pressure and cross-sectional area in the female urethra. Neurourol Urodyn 26:254–261. doi:10.1002/nau.20283
Lose G, Griffiths D, Hosker G et al (2002) Standardisation of urethral pressure measurement: report from the Standardisation Sub-Committee of the International Continence Society. Neurourol Urodyn 21:258–260
Saaby M-L, Klarskov N, Lose G (2013) Urethral pressure reflectometry during intra-abdominal pressure increase-an improved technique to characterize the urethral closure function in continent and stress urinary incontinent women. Neurourol Urodyn 32:1103–1108. doi:10.1002/nau.22368
Claerbout J (1968) Synthesis of a layered medium from its acoustic transmission response. Geophysics 33:264–269. doi:10.1190/1.1439927
Sondhi MM, Gopinath B (1971) Determination of vocal-tract shape from impulse response at the lips. J Acoust Soc Am 49:1867–1873
Fredberg JJ, Wohl ME, Glass GM, Dorkin HL (1980) Airway area by acoustic reflections measured at the mouth. J Appl Physiol 48:749–758
Klarskov N, Rasmussen SB, Lose G (2005) Pressure reflectometry: in vitro recordings with a new technique for simultaneous measurement of cross-sectional area and pressure in a collapsible tube. Physiol Meas 26:269–280. doi:10.1088/0967-3334/26/3/011
Klarskov N, Lose G (2007) Urethral pressure reflectometry vs urethral pressure profilometry in women: a comparative study of reproducibility and accuracy. BJU Int 100:351–356. doi:10.1111/j.1464-410X.2007.06922.x
Klarskov N, Saaby M-L, Lose G (2013) A faster urethral pressure reflectometry technique for evaluating the squeezing function. Scand J Urol 47:529–533. doi:10.3109/21681805.2013.776629
Klarskov N (2012) Urethral pressure reflectometry. A method for simultaneous measurements of pressure and cross-sectional area in the female urethra. Dan Med J 59:B4412
Klarskov N, Lose G (2008) Urethral pressure reflectometry and pressure profilometry in healthy volunteers and stress urinary incontinent women. Neurourol Urodyn 27:807–812. doi:10.1002/nau.20617
Chapple CR, Wein AJ, Artibani W et al (2005) A critical review of diagnostic criteria for evaluating patients with symptomatic stress urinary incontinence. BJU Int 95:327–334. doi:10.1111/j.1464-410X.2005.05293.x
DeLancey JOL (2010) Why do women have stress urinary incontinence? Neurourol Urodyn 29:S13–S17. doi:10.1002/nau.20888
Saaby M-L, Klarskov N, Lose G (2012) Urethral pressure reflectometry before and after tension-free vaginal tape. Neurourol Urodyn 31:1231–1235. doi:10.1002/nau.22239
Saaby M-L, Klarskov N, Lose G (2015) The impact of tension-free vaginal tape on the urethral closure function: mechanism of action. Neurourol Urodyn 34:50–54. doi:10.1002/nau.22513
Koelle D, Windisch J, Doerfler D et al (2006) Effect of tension-free vaginal tape operation on urethral closure function. Urology 67:524–528. doi:10.1016/j.urology.2005.09.063; discussion 528–529
Lo TS, Wang AC, Horng SG et al (2001) Ultrasonographic and urodynamic evaluation after tension free vagina tape procedure (TVT). Acta Obstet Gynecol Scand 80:65–70
Mutone N, Mastropietro M, Brizendine E, Hale D (2001) Effect of tension-free vaginal tape procedure on urodynamic continence indices. Obstet Gynecol 98:638–645
Abrams P, Cardozo L, Khoury S, Wein A (2012) Incontinence—5th International Consultation on Incontinence, Paris, 5 February
Saaby ML, Klarskov N, Lose G (2011) Simultaneous cystometry and urethral pressure reflectometry (UPR)—a new method. Neurourol Urodyn 30:787–1206
Klarskov N, Lose G (2008) Urethral injection therapy: what is the mechanism of action? Neurourol Urodyn 27:789–792. doi:10.1002/nau.20602
Bump RC, Benson JT, Yalcin I et al (2004) Biomechanical and electrophysiological effects of duloxetine in women with stress urinary incontinence. J Pelvic Med Surg 10 [Suppl 1]:37–38
Weil EH, Eerdmans PH, Dijkman GA et al (1998) Randomized double-blind placebo-controlled multicenter evaluation of efficacy and dose finding of midodrine hydrochloride in women with mild to moderate stress urinary incontinence: a phase II study. Int Urogynecol J Pelvic Floor Dysfunct 9:145–150
Klarskov N, Scholfield D, Soma K et al (2009) Measurement of urethral closure function in women with stress urinary incontinence. J Urol 181:2628–2633. doi:10.1016/j.juro.2009.01.114, discussion 2633
Klarskov N, Scholfield D, Darekar A et al (2010) Urethral pressure reflectometry is valuable for evaluating pharmacological therapies for stress urinary incontinence. Int Urogynecol J 21:166–168
Klarskov N, Darekar A, Scholfield D et al (2014) Effect of fesoterodine on urethral closure function in women with stress urinary incontinence assessed by urethral pressure reflectometry. Int Urogynecol J 25:755–760. doi:10.1007/s00192-013-2269-6
Klarskov N, Cerneus DP, Sawyer AW et al (2015) The effect of single oral doses of duloxetine, reboxetine and midodrine on the urethral pressure in healthy female subjects, using urethral pressure reflectometry in a placebo-controlled, randomized, crossover study. 40th Annual Meeting—Nice, France June 9–13, 2015: oral presentations. Int Urogynecol J 26(1 Suppl):1–21
Aagaard M, Klarskov N, Sønksen J et al (2012) Urethral pressure reflectometry; a novel technique for simultaneous recording of pressure and cross-sectional area: a study of feasibility in the prostatic urethra. BJU Int 110:1178–1183. doi:10.1111/j.1464-410X.2012.10997.x
Aagaard M, Klarskov N, Sønksen J et al (2014) Urethral pressure reflectometry, a novel technique for simultaneous recording of pressure and cross-sectional area in the prostatic urethra: testing in men without bothersome lower urinary tract symptoms. Scand J Urol 48:195–202. doi:10.3109/21681805.2013.831946
Mitchell PJ, Klarskov N, Hosker G et al (2010) Anal acoustic reflectometry: a new technique for assessing anal sphincter function. Colorectal Dis Off 12:692–697. doi:10.1111/j.1463-1318.2010.02194.x
Mitchell PJ, Klarskov N, Telford KJ et al (2011) Anal acoustic reflectometry: a new reproducible technique providing physiological assessment of anal sphincter function. Dis Colon Rectum 54:1122–1128. doi:10.1097/DCR.0b013e318223fbcb
Mitchell PJ, Klarskov N, Telford KJ et al (2012) Viscoelastic assessment of anal canal function using acoustic reflectometry: a clinically useful technique. Dis Colon Rectum 55:211–217. doi:10.1097/DCR.0b013e31823b2499
Hornung BR, Mitchell PJ, Carlson GL et al (2012) Comparative study of anal acoustic reflectometry and anal manometry in the assessment of faecal incontinence. Br J Surg 99:1718–1724. doi:10.1002/bjs.8943
Hornung BR, Carlson GL, Mitchell PJ et al (2014) Anal acoustic reflectometry predicts the outcome of percutaneous nerve evaluation for faecal incontinence. Br J Surg 101:1310–1316. doi:10.1002/bjs.9586
Latthe PM, Foon R, Toozs-Hobson P (2008) Prophylactic antibiotics in urodynamics: a systematic review of effectiveness and safety. Neurourol Urodyn 27:167–173. doi:10.1002/nau.20501
Acknowledgements
The authors would like to thank Laborie for the supply of catheters used for urethral pressure reflectometry.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Yasmine Khayyami and Gunnar Lose have received honoraria as investigators from Astellas. Niels Klarskov has received honoraria as a speaker/investigator and travel grants from Astellas.
Glossary
- Urethral pressure
-
The air pressure required to force the urethra open
- Cross-sectional area
-
The area of the opened lumen of the urethra
- High-pressure zone (HPZ)
-
The area with minimal urethral cross-sectional area at a given pressure
- Opening pressure
-
A measurement of the permanent closing forces that enable the urethra to remain closed
- Closing pressure
-
The pressure at which the urethra closes subsequent to dilation
- Elastance
-
Expresses the urethra’s resistance to deformation when exposed to an external force
- Hysteresis
-
Expresses the energy loss in the urethra during stretching
- Abdominal to urethral pressure impact ratio (APIR)
-
Expresses the effect of increasing abdominal pressure on urethral pressure
- PO-Abd 50
-
Opening pressure at an abdominal pressure of 50 cmH2O
- PO-Abd 100
-
Opening pressure at an abdominal pressure of 100 cmH2O
Rights and permissions
About this article
Cite this article
Khayyami, Y., Klarskov, N. & Lose, G. The promise of urethral pressure reflectometry: an update. Int Urogynecol J 27, 1449–1458 (2016). https://doi.org/10.1007/s00192-016-2964-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-016-2964-1