Abstract
Introduction and hypothesis
The premise of midurethral sling (MUS) surgery is to apply a tension-free vaginal tape in the midurethra that does not constrict the urethra at rest but stabilizes the urethra and prevents downward descent and opening of the urethra during stress maneuvers, but current technology has limitations in measuring urethral pressures during dynamic conditions. Our objective was to describe the change in maximum urethral closure pressures (MUCPs) after MUS surgery using an 8F high-resolution manometry (HRM) system that can measure urethral pressures during cough and strain maneuvers (ManoScan® ESO; Covidien) without migration or withdrawal limitations.
Methods
We measured rest, cough, and strain MUCPs in 26 women before and after retropubic or transobturator MUS for stress urinary incontinence using the HRM system.
Results
The objective success rate after MUS was 92.3 % based on postoperative cough stress testing. Mean resting MUCPs measured by HRM did not change after surgery (59.3 before vs. 59.7 cm H2O after surgery; p = 1.0). Mean cough MUCPs measured by HRM increased from 36.9 to 100.7 cm H2O (p < 0.001), and strain MUCPs increased from 35.0 to 92.7 cm H2O (p < 0.001).
Conclusions
Advanced HRM technology to measure MUCPs under cough and strain conditions without withdrawal techniques provides new insights into the continence mechanism after tension-free MUS: MUCPs do not change at rest but do increase significantly during cough and strain maneuvers.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Urinary incontinence affects 16 % of adult women [1]. Stress urinary incontinence (SUI), the involuntary loss of urine on effort or physical exertion such as cough and strain [2], can be treated with pelvic floor muscle exercises, pessaries, and surgery, with surgery being the most successful treatment [3]. Approximately 260,000 stress incontinence surgical procedures are performed each year in the US [4]. The most frequently performed surgical treatment for SUI is mesh midurethral sling (MUS) surgery, which has a success rate of approximately 80 % [5].
The premise of MUS surgery is to apply a tension-free vaginal tape in the midurethra that does not constrict the urethra at rest but stabilizes the urethra and prevents downward descent and opening of the urethra during stress maneuvers. Indeed, most studies have shown that resting maximum urethral closure pressures (MUCPs) do not change significantly after MUS surgery [6–8]. It is more difficult to assess and understand the function of the urethra during typical stress maneuvers such as cough and strain. Current technologies are hindered by slow response times or the need for withdrawal techniques. Instruments that measure a single point of pressure in the urethra can be displaced from the maximum pressure zone with a cough or strain and therefore changes may merely be artifact. Pressure transmission ratios measure the ratio of urethral pressure to bladder pressure with repetitive coughs while withdrawing a microtip catheter through the urethra. These ratios have generally been shown to increase after SUI surgery [9], but in several decades, these ratios have never become a widespread or clinically useful tool. The search for a simple tool that can measure urethral pressures during dynamic conditions and help us understand successful or failed treatments remains elusive.
A high-resolution manometry (HRM) system (ManoScan® ESO; Covidien, Culver City, CA) has recently been shown to be well tolerated in the bladder and urethra and to provide pressure measurements that correlate well with water-perfusion urethral pressure profilometry measurements at rest [10]. The potential advantage of this technology is that it has a fast 25-ms response time and can measure circumferential pressures at many points along the urethra at once without a withdrawal technique. Because of its ability to capture MUCPs during cough and strain, it may be clinically useful in evaluating outcomes after MUS for SUI. Although resting MUCPs may not change after surgery, the more important question is whether cough and strain MUCPs increase after MUS, and HRM technology can measure this.
The purpose of this investigation was to determine if this new HRM technology allows us to better understand how MUS affects urethral pressures under dynamic conditions. Specifically, we sought to measure changes in rest, cough, and strain MUCPs after MUS. We hypothesized that the MUS functions by increasing urethral pressures during cough and strain maneuvers but not at rest.
Materials and methods
The HRM system we used is a pediatric esophageal catheter and pressure-sensing software produced by Covidien for use in gastroenterology (ManoScan® ESO) [11]. This catheter is 2.75 mm in diameter (approximately 8F) and has circumferential pressure sensors along 26.5 cm of its length. The miniature solid-state sensors are 4 mm long with 2 mm of active sensing area separated by 3 mm of flexible molding giving a 7.5 mm on center spacing between each of the 36 sensors. Each individual sensor has 16 pressure-sensitive segments circumferentially distributed around it (Fig. 1). Computer processing of the signal comes from the pressure-sensing elements and calculates average circumferential pressures. Pressures between sensing elements are interpolated, and the data are presented on a color graphic display (Fig. 2).
Women with primary or recurrent urinary incontinence who were scheduled to undergo full-length MUS surgery at our institution were recruited to have HRM bladder and urethral pressure measurements before and 6 weeks after surgery. The study was approved by our Institutional Review Board, and written consent was obtained. All subjects were at least 18 years of age, not pregnant, without evidence of a UTI, and without pelvic organ prolapse beyond the hymen. Women with prior prolapse or incontinence surgery were not excluded. All subjects had positive standing cough stress tests (CST) prior to surgery. Each subject completed demographic information including age, height, weight, parity, medical history, and surgical history as well as the Incontinence Severity Index (ISI, scale 0 to 12) [12], Incontinence Impact Questionnaire Short Form (IIQ-7, scale 0 to 100), and Urogenital Distress Inventory Short Form (UDI-6, scale 0 to 100) questionnaires [13]. Question 3 of the UDI-6 was specifically used to capture subjective SUI: “Do you experience and, if so, how much are you bothered by urine leakage related to activity, coughing, or sneezing?” Questionnaires were repeated 6 weeks after surgery.
Prior to obtaining pressure measurements, subjects’ bladders were drained with a sterile catheter and then filled with 250 ml sterile water or with the maximum volume she could comfortably hold for 15 min if this was less than 250 ml. This catheter was removed, and the HRM catheter was placed such that the tip was approximately 5 cm inside the bladder. Bladder and urethral pressures were obtained after 10 s of rest, during three coughs, and during three strain maneuvers. For strain maneuvers, subjects were instructed to bear down or push as though trying to have a baby or a bowel movement. MUCPs were calculated by subtracting the maximum bladder pressures 2 cm proximal to the urethrovesical junction from the maximum urethral pressure anywhere along the urethra during each maneuver. Because each 4-mm sensor has a 2-mm sensing area and there are 3-mm spaces between sensors, there are 5-mm sections along the urethra that are not measured with this system. Our previous experiments, in which the catheter was moved several millimeters and pressure recordings repeated, demonstrated that the location of this non-measured area does not appear to affect maximum pressure measured [10].
The primary endpoint was change in MUCP during dynamic maneuvers (cough and strain) after compared with before MUS surgery. We pooled retropubic and transobturator MUS because these types of MUS, with only small differences in placement and outcomes, are thought to function similarly [5]. Preoperative and postoperative MUCPs were compared using paired t-tests, questionnaire scores were compared using paired Wilcoxon tests, and the change in the percent of patients with positive CST before and after surgery was analyzed with the chi-squared test. Tests were adjusted for multiple comparisons using the Bonferroni method, and p < 0.01 was considered significant. We recruited 26 subjects in order to have 80 % power to detect a mean change of 14 cm H2O (standard deviation 20 cm H2O) during cough and strain after MUS surgery based on previous studies [14] with an 85 % success rate after MUS surgery [15] and 20 % drop-out rate. Analyses were performed using R (http://r-project.org). In a secondary analysis, we defined composite surgical success as objective negative postoperative CST and subjective improvement in ISI score, and we compared composite success rates in subjects with increased postoperative cough and strain MUCPs to those in subjects with decreased postoperative MUCPs using Fisher’s exact test.
Results
Included in this study were 26 women, of whom 20 had retropubic and 6 transobturator MUS surgery. Their median age was 53.5 years (range 38 – 77 years), median BMI 27.9 kg/m2 (range 20.8 – 37.2 kg/m2), and median vaginal parity 2 (range 0 – 5). Seven subjects (26.9 %) had had at least one prior continence surgery. Preoperative and postoperative continence severity, quality of life measures, CST, and MUCPs are shown in Table 1. All continence severity and quality of life measures improved significantly after surgery. All subjects had positive CST before surgery, and 2 had positive stress tests 6 weeks after surgery (objective success rate of 92.3 %). ISI scores improved in 96.2 % (25/26) of subjects. Composite success (negative CST and improvement in ISI) was 88.5 % (23/26).
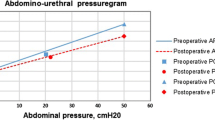
Figure 3 shows preoperative and postoperative MUCPs after MUS surgery for rest, cough, and strain in each subject. Resting MUCPs generally did not change after surgery while cough and strain MUCPs increased in the vast majority of subjects. Cough and/or strain MUCPs decreased after surgery in three subjects; the composite success rate in these subjects was 66.7 % (2/3), compared to 91.3 % (21/23) in subjects in whom cough and strain MUCPs increased. The difference in success rates between the two groups was not statistically significant (p = 0.3), but this study was not powered for this secondary analysis.
Mean resting MUCPs were not different after surgery (59.3 before vs. 59.7 cm H2O after surgery; p = 1.0). Mean cough MUCPs increased from 36.9 to 100.7 cm H2O (p < 0.001) and strain MUCPs increased from 35.0 to 92.7 cm H2O (p < 0.001); Table 1, Fig. 4).
Analyzing retropubic and transobturator MUS subjects separately, the trends remained similar to those seen in all subjects. There were enough subjects who underwent retropubic MUS (20) to meet our power calculation because no subjects dropped out of the trial, and, similar to our primary endpoint for all subjects, cough and strain MUCPs increased significantly (p < 0.001), while rest MUCPs did not change significantly (p = 0.2). In subjects who underwent transobturator MUS, the same trends were seen, but there were not enough of these subjects (6) to show statistical significance in this subgroup: change in cough and strain nearly met significance (p = 0.05 and p = 0.02, respectively), while change in rest MUCP was not significant (p = 0.16).
We included women with prior continence surgery in this study because they were surgical failures and candidates for MUS surgery regardless of what surgery had been done in the past. Similar results were obtained from subjects with and without prior continence surgery analyzed separately with only slightly better results in those without prior surgery (data not shown).
Discussion
The major finding of our study is that the mean MUCPs during cough and strain measured by a HRM system increase markedly (60 cm H2O) and significantly after MUS surgery. Postoperative cough and strain MUCPs were similar to MUCPs seen in continent women [10]. We found a high mean increase even when we included those subjects who did not improve after surgery. In contrast to the change after surgery in MUCP with cough or strain, the resting MUCP did not change. These results support our hypothesis that MUS does not appreciably affect the urethra at rest but has a profound effect on the urethra with cough and strain. No change in resting pressure after MUS surgery is consistent with the findings of most previous studies using other technologies [6–8, 16]. The increase observed in MUCPs after surgery during dynamic conditions is also consistent with the findings of studies that have found increased pressure transmission ratios after surgery [6, 9], but the magnitude of the effect can only be appreciated with this non-withdrawal technique.
Most cough and strain MUCPs increased after surgery, and the few subjects in whom MUCPs did not increase had somewhat worse though not significantly different postoperative outcomes. This suggests that this technology may be clinically useful for measuring success after MUS surgery and may even help clinicians determine whether a sling revision, sling tightening, or an additional sling is likely to improve continence in patients who remain incontinent after MUS surgery. Since this was a preliminary pilot study using this new technology before and after surgery, and we had few failures, additional studies with sufficient power are needed to determine its clinical utility in differentiating success from failure.
HRM technology is an improvement over other urodynamic measurements because of its fast response rate and multiple pressure-sensing segments that ensure it can register millisecond pressure changes during coughs and capture maximum pressures along the length of the urethra even if the catheter changes position. There remain some limitations to its accuracy because its inherent rigidity and circumference can produce artifact. Nonetheless, it has allowed us to dramatically demonstrate the mechanism of action of MUS in improving continence and may prove to be clinically useful in diagnosing and assessing treatment success in women with SUI.
Advanced HRM technology to measure MUCPs under cough and strain conditions without withdrawal techniques provides new insights into the continence mechanism after tension-free MUS surgery. MUCPs do not change at rest, but marked increases occur during cough and strain maneuvers. Future studies are planned to evaluate this technology as an intraoperative tool to adjust sling tensioning or understand surgical failures.
References
Nygaard I, Barber MD, Burgio KL, Kenton K, Meikle S, Schaffer J, Spino C, Whitehead WE, Wu J, Brody DJ (2008) Prevalence of symptomatic pelvic floor disorders in US women. JAMA 300(11):1311–1316. doi:10.1001/jama.300.11.1311
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, Monga A, Petri E, Rizk DE, Sand PK, Schaer GN (2010) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn 29(1):4–20. doi:10.1002/nau.20798
Labrie J, Berghmans BL, Fischer K, Milani AL, van der Wijk I, Smalbraak DJ, Vollebregt A, Schellart RP, Graziosi GC, van der Ploeg JM, Brouns JF, Tiersma ES, Groenendijk AG, Scholten P, Mol BW, Blokhuis EE, Adriaanse AH, Schram A, Roovers JP, Lagro-Janssen AL, van der Vaart CH (2013) Surgery versus physiotherapy for stress urinary incontinence. N Engl J Med 369(12):1124–1133. doi:10.1056/NEJMoa1210627
FDA (2011) Urogynecologic surgical mesh: update on the safety and effectiveness of transvaginal placement for pelvic organ prolapse. United States Food and Drug Administration, White Paper, p 6
Richter HE, Albo ME, Zyczynski HM, Kenton K, Norton PA, Sirls LT, Kraus SR, Chai TC, Lemack GE, Dandreo KJ, Varner RE, Menefee S, Ghetti C, Brubaker L, Nygaard I, Khandwala S, Rozanski TA, Johnson H, Schaffer J, Stoddard AM, Holley RL, Nager CW, Moalli P, Mueller E, Arisco AM, Corton M, Tennstedt S, Chang TD, Gormley EA, Litman HJ (2010) Retropubic versus transobturator midurethral slings for stress incontinence. N Engl J Med 362(22):2066–2076
Mutone N, Mastropietro M, Brizendine E, Hale D (2001) Effect of tension-free vaginal tape procedure on urodynamic continence indices. Obstet Gynecol 98(4):638–645
Wadie BS, El-Hefnawy AS (2009) Urethral pressure measurement in stress incontinence: does it help? Int Urol Nephrol 41(3):491–495. doi:10.1007/s11255-008-9506-9
Lo TS, Horng SG, Chang CL, Huang HJ, Tseng LH, Liang CC (2002) Tension-free vaginal tape procedure after previous failure in incontinence surgery. Urology 60(1):57–61
Rosenzweig BA, Bhatia NN, Nelson AL (1991) Dynamic urethral pressure profilometry pressure transmission ratio: what do the numbers really mean? Obstet Gynecol 77(4):586–590
Kirby AC, Tan-Kim J, Nager CW (2014) Measurement of dynamic urethral pressures with a high-resolution manometry system in continent and incontinent women. Female Pelvic Med Reconstr Surg. doi:10.1097/SPV.0000000000000135
Fox MR, Bredenoord AJ (2008) Oesophageal high-resolution manometry: moving from research into clinical practice. Gut 57(3):405–423. doi:10.1136/gut.2007.127993
Sandvik H, Seim A, Vanvik A, Hunskaar S (2000) A severity index for epidemiological surveys of female urinary incontinence: comparison with 48-hour pad-weighing tests. Neurourol Urodyn 19(2):137–145
Uebersax JS, Wyman JF, Shumaker SA, McClish DK, Fantl JA (1995) Short forms to assess life quality and symptom distress for urinary incontinence in women: the Incontinence Impact Questionnaire and the Urogenital Distress Inventory. Continence Program for Women Research Group. Neurourol Urodyn 14(2):131–139
Tan-Kim J, Weinstein MM, Nager CW (2010) Urethral sleeve sensor: a non-withdrawal method to measure maximum urethral pressure. Int Urogynecol J 21(6):685–691
Nilsson CG, Kuuva N, Falconer C, Rezapour M, Ulmsten U (2001) Long-term results of the tension-free vaginal tape (TVT) procedure for surgical treatment of female stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 12(Suppl 2):S5–S8
Cholhan HJ, Lotze PM (2008) Urodynamic changes after tension-free sling procedures: Mycromesh-Plus vs TVT sling. Int Urogynecol J Pelvic Floor Dysfunct 19(2):217–225. doi:10.1007/s00192-007-0418-5
Acknowledgments
Technical assistance and loan of the HRM catheter were provided by Tom Parks and Dave Costarella at Covidien.
Funding
Support for this work was provided by NIH/NIDDK grant number R21DK090434-02.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was performed at the UC San Diego Health System.
Rights and permissions
About this article
Cite this article
Kirby, A.C., Tan-Kim, J. & Nager, C.W. Dynamic maximum urethral closure pressures measured by high-resolution manometry increase markedly after sling surgery. Int Urogynecol J 26, 905–909 (2015). https://doi.org/10.1007/s00192-014-2622-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-014-2622-4