Abstract
Introduction and hypothesis
Obstetric anal sphincter injuries (OASIs) are the leading cause of anal incontinence in women. Modification of various risk factors and anatomical considerations have been reported to reduce the rate of OASI.
Methods
A PubMed search (1989–2014) of studies and systematic reviews on risk factors for OASI.
Results
Perineal distension (stretching) of 170 % in the transverse direction and 40 % in the vertical direction occurs at crowning, leading to significant differences (15–30°) between episiotomy incision angles and suture angles. Episiotomies incised at 60° achieve suture angles of 43–50°; those incised at 40° result in a suture angle of 22°. Episiotomies with suture angles too acute (<30°) and too lateral (>60°) are associated with an increased risk of OASI. Suture angles of 40–60° are in the safe zone. Clinicians are poor at correctly estimating episiotomy angles on paper and in patients. Sutured episiotomies originating 10 mm away from the midline are associated with a lower rate of OASIs. Compared to spontaneous tears, episiotomies appear to be associated with a reduction in OASI risk by 40–50 %, whereas shorter perineal lengths, perineal oedema and instrumental deliveries are associated with a higher risk. Instrumental deliveries with mediolateral episiotomies are associated with a significantly lower OASI risk. Other preventative measures include warm perineal compresses and controlled delivery of the head.
Conclusions
Relieving pressure on the central posterior perineum by an episiotomy and/or controlled delivery of the head should be important considerations in reducing the risk of OASI. Episiotomies should be performed 60° from the midline. Prospective studies should evaluate elective episiotomies in women with a short perineal length and application of standardised digital perineal support.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstetric anal sphincter injuries (OASIs) are the leading cause of anal incontinence (AI) in women. A meta-analysis of 717 patients, found that 30 % of women were symptomatic 1 year after OASI [1]. A 25-year prospective follow-up study of women with OASI revealed persistent AI in 40 % [2]. The probability of longer-term AI and urgency has been reported to be 53 % to 80 % [3, 4]. The incidence of OASI in first vaginal births is 5.9 % in England [5], and the corresponding figure for the whole of the UK is 6.1 % (range 0–15 %) [6].
There are modifiable risk factors for OASI including length of the second stage, occipitoposterior position [7–11], use of oxytocin and epidural analgesia, which do not have credible alternatives. Common intervention choices made in the second stage of labour such as the decision to allow spontaneous tears versus performing an episiotomy, the geometric characteristics of the episiotomy performed, and the choice of instrument for operative vaginal deliveries are to an extent modifiable and can be critical factors in the causation of OASIs. For instance, there is growing evidence to suggest that the chance of sustaining an OASI is 40–50 % higher in women who have a spontaneous perineal tear during their first vaginal birth rather than an episiotomy [5, 12]. However, there still remains considerable morbidity due to episiotomies that are either too acute (≤30°) [13, 14] or too lateral (≥60°) [15], or originate too close to the midline [15].
Manual perineal protection has also been the subject of considerable interest in the prevention of OASIs [16–19]. There are two components of manual perineal protection. The first is slow controlled delivery of the head aiming to prevent a speed-driven precipitous ‘explosive’ tearing of the perineum when the ‘strain’ in the tissues exceeds their ‘stiffness’. Indeed, slow stretching of the perineum has been advocated as a protective factor [20]. The second component is the application of fingers on the posterior perineum at crowning in a manner that dissipates or relieves pressure on its central part, where the stress is maximal, and which if it tears, would most likely result in a direct breach of the anal sphincters. There could be interindividual variations to this technique, and the true contribution of this technique to the prevention of OASI would be difficult to quantify, unless pressure measurements of actual perineal stretching or deformation are available [21, 22].
We present a review of recent data, including studies of techniques used to prevent OASI in which measurements were taken and for which descriptions are provided in the articles. A PubMed search of articles between 1989 and 2014 was performed including the MeSH search words, episiotomy, perineal tears, perineal length (PL), obstetric anal sphincter injury, third and fourth degree tears, perineum, forceps, vacuum, instrumental births, length of second stage, occipitoposterior position, oxytocin and epidural analgesia.
Anatomical and tissue factors
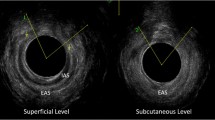
Perineal length
The measurement of perineal body length as described in the Pelvic Organ Prolapse Quantification system (POP-Q) is from the posterior fourchette to the midpoint of the anal canal. The International Continence Society (ICS) describes a perineal body length of <30 mm (nonpregnant state) as being associated with weakness of the anatomical support of the pelvic organs [23]. Associations between short PL and pelvic organ prolapse and pelvic floor dysfunction have also been highlighted [24, 25].
PL has been studied and its association with OASI evaluated by many investigators. Table 1 shows the studies involving PL measurements antenatally, and in the first and/or second stage of labour. The average PL is 39 mm (range 37–41 mm) in the late antenatal period or first stage of labour [26–31] and PL has increased by 50–60 % at crowning to 60 mm [31–33].
Patients with PL ≤25 mm (measured during the first stage) had a significantly greater risk of OASI (40 % vs. 5.6 %, p = 0.004) [26]. A recent study using 3D endoanal ultrasound showed a similar OASI rate of 40 % in women with a PL of <30 mm measured at 35–37 weeks versus 11 % in those with a longer PL [30].
Aytan et al. [34] compared the characteristics of midline and mediolateral episiotomies (with a 45° incision) in a cohort of 400 women undergoing spontaneous delivery. The incidence of OASI was three times higher in women who underwent a midline episiotomy than in those with a mediolateral episiotomy. The incidence of OASI was as high as 30 % in women who underwent a midline episiotomy with PL <30 mm compared to 0.5 % in women with PL >30 mm. With midline episiotomies, the length of the cut and the PL were significantly associated with OASI. If the PL was <30 mm or if the cut was >30 mm (after suturing), then a direct breach of the anal sphincter muscles was more likely. A receiver operating characteristic curve did not reveal an association between mediolateral episiotomy and PL.
It is noteworthy that 14–20 % of women have been reported to have a short PL of <30 mm [26, 27, 30] (measured in the late third trimester or first stage of labour, with no significant differences in values) and this is a group that is at higher risk of OASI. Interventions to reduce the risk of OASI will need to take this group into account. It has been suggested that these women would benefit from a prophylactic mediolateral episiotomy [32], but prospective studies are lacking.
Perineal deformation/distension
Kalis et al. were the first to report data on the difference between the incision angle and suture angle of the episiotomy [35, 36]. A 40° premarked episiotomy results in a postdelivery suture angle of 22°, while a 60° premarked episiotomy results in a suture angle of 45°. This suggests a significant degree of perineal deformation during birth. Similar degrees of perineal distension have also been observed on the opposite side of the episiotomy (intact side of the perineum), ruling out an effect of the episiotomy itself. This degree of perineal distension has been observed even when performing episiotomies at 60° with the Episcissors-60™ (Medinvent Ltd., Romsey, UK) in instrumental deliveries (43°) [37] and spontaneous deliveries (50°) [38]. Table 2 summarises studies in which the incision and suture angles of episiotomies were measured.
The biomechanics of birth have been studied by clinical observation [33, 35, 36], MRI studies [39] and stereophotogrammetry [21]. The anal orifice has been found to dilate to 25 mm in the anteroposterior and transverse diameters during crowning, implying a circular dilatation [33]. Lien et al. [39] found a 2.5-fold to 3-fold increase in different parts of the levator muscle dimensions during birth. The largest stretch ratios of 300 % occurred in the medial-most part of the pubococcygeus due to the location of its origins near the midline. It was uncertain whether the stretch would be transmitted to the caudal perineal body, which could be a passive structure. Stereophotogrammetry of the perineum has shown a maximum stretching of 177 % in the transverse diameter, and 43 % in the anteroposterior diameter [21].
Eliashiv et al. [40] suggested a perineal distension of 30° from the first stage of labour to crowning. Perineal distension was observed at 50–100 % in angular terms with no differences noted between nulliparous and parous women. However, they did not record any postdelivery angles. No similar data exist for the incision distance away from the midline. However, the stereophotogrammetry data showed a transverse distension of 2.7-fold [21]. Lai et al. [31] found an interesting correlation between the degree of perineal stretching and the degree of tearing. They found that nulliparous women who stretched less, sustained higher order tears, indicating a significantly higher degree of stiffness and lower perineal compliance. Conversely, Walfisch et al. [32] found that excessive stretching (>150 %) was associated with perineal tearing.
Perineal oedema
Perineal oedema due to prolonged labour and position of the parturient may be a factor in determining the extent of the tear. Samuelsson et al. [41] found an association between OASI with perineal oedema and manual perineal protection. In their prospective study of 2,883 women, Manual perineal protection was effective in nulliparous women in reducing the risk of OASI by two-thirds. Severe perineal oedema increased the risk of OASI sixfold in univariate analysis, but was no longer significant in multivariate analysis.
Impact of race/ethnicity on OASI
Short PL and ‘low resistance to tearing’ or low perineal compliance [20] could be factors that predispose certain racial/ethnic groups to OASIs. Handa et al. [42] analysed data from two million vaginal deliveries in California and found an OASI rate of nearly 6 %. Women of Indian descent (OR 2.5) and Filipina women (OR 1.5) were at higher risk of OASI. Other studies have found Oriental races to be at higher risk of OASI [20, 43, 44]. Hopkins et al. [44] compared the rates of perineal lacerations (second, third and fourth degrees) and vaginal and cervical lacerations. Although they found women of Chinese and Filipina descent to have significantly more perineal tears, they found no such differences between vaginal and cervical lacerations. Tsai et al. [29] and Lai et al. [31] found no difference in PL between women of different ethnic backgrounds. There may be other factors such as fetal weight and head circumference that contribute to a higher rate of severe perineal lacerations between women of certain ethnicities living in their native countries compared to those who become westernised. Howard et al. [45] found a lower rate of perineal laceration in black women compared to white women (10 % vs. 20 %, p = 0.003, adjusted OR 2.1) and hypothesised that differences in connective tissue collagen content might be responsible.
Modifiable second stage interventions
Length of second stage of labour
Whilst a longer second stage of labour has been generally found to be associated with a higher OASI risk [9, 46–49], no such association has been found for spontaneous deliveries [50]. A 6 % increase in OASI risk per 15 min in the second stage of labour before instrumental delivery has been found. Attempts to modify the duration of the second stage to prevent sphincter injuries are unlikely to be beneficial and may be detrimental [50]. A prolonged second stage may also be responsible for increased perineal oedema, which is an independent risk factor for OASI [41]. A randomised trial found no difference between early and delayed pushing in the second stage [51].
Oxytocin use in labour
Whilst some authors have found no association [52], oxytocin augmentation has been found to be associated with a higher risk of OASI in women giving birth spontaneously to infants weighing <4 kg [53]. However, there are no credible alternatives to oxytocin for labour augmentation.
Epidural analgesia
Whilst some authors have found a reduction in the rate of OASI with epidural analgesia [53–55], others have found no difference [12, 41]. Roos et al. [56] found that epidural analgesia was the only independent factor that predicted OASI. There may not be credible alternatives to epidural analgesia for sustained and safe pain relief, and it may not strictly be a modifiable factor.
Episiotomy use and characteristics
The protection of the perineum by episiotomy in delivery at term seems a paradox. How is it possible by incising the perineum to protect it from injury? … Incision of the perineum or vulvar outlet at childbirth is our only prophylactic of merit against irreparable pelvic-floor injury. Martin, 1921 [57]
The above statement reflects the historic nature of the debate about the merits of performing episiotomy. Enlarging the birth passage in the face of a rigid, unyielding perineum is the most obvious indication for an episiotomy. It has also been suggested as a means of relieving perineal pressure, and preventing pelvic floor relaxation associated with spontaneous perineal tears, which occur in a majority of first vaginal births [57]. A mediolateral episiotomy is designed to avoid injuring the perineal body (a level three injury), the support of the pelvic viscera [58], the insertion raphe of the decussating fibres of the transverse perinei, the bulbocavernosus, and the anal sphincter complex. It also aims to avoid damaging the levator ani muscle (more likely to be encountered with a horizontal/lateral cut). Indeed, some studies have shown a protective effect in reducing the incidence of uterovaginal prolapse [59–63].
However, given that mediolateral episiotomies (as defined by a postdelivery angle of >30°) are not truly mediolateral or ‘non-median’ [13], there seems little to differentiate them from episiotomies that are intended to be midline or ‘median’ [64]. Indeed, mediolateral episiotomies have not been shown to be protective, and a case series of primiparous women in a centre that practises restrictive mediolateral episiotomy showed a 24 % incidence of OASI [13], similar to the 20 % described in a centre that practises restrictive midline episiotomies [64]. Therefore, previous studies, including randomised controlled trials, showing no beneficial effects of mediolateral episiotomy need to be questioned, as the angle of the episiotomy was not controlled for.
Routine versus restrictive
A Cochrane review [65] compared routine episiotomy (75 %) with restrictive episiotomy (28 %) and found a lower rate of OASI in the restrictive group. The authors were unable to comment on the choice of midline versus mediolateral types, nor did they differentiate between the use of episiotomy in operative vaginal deliveries and spontaneous vaginal deliveries. In view of the significantly higher incidence of OASI without episiotomies, the National Institute for Health and Care Excellence (NICE) recommends that episiotomies should be performed for instrumental deliveries [66].
To eliminate the impact of confounders such as the indication for the episiotomy, Raisanen et al. [67] reported on a matched pair analysis of nearly 64,000 vaginal births. Subjects were matched for baseline OASI risk factors including age, birth weight, instrumental delivery, length of second stage, and parity. They found that episiotomy reduced the odds ratio of OASI by 23 % in first vaginal births, while it increased it in subsequent vaginal births by 63 %. They concluded that many indications for episiotomy are also risk factors for OASI, and benefits or harms of episiotomy noted in observational studies were due to the indications for its use, rather than a treatment effect.
Angle of the episiotomy
Historically, episiotomies have been classed as midline or mediolateral by stated intent. While some authors have defined mediolateral episiotomies as those at 60° at the time of cutting [68, 69], others have suggested an angle of >30° from the midline as the criterion [70]. The problem with these definitions is that there was no accurate way of measuring these angles. Table 3 shows all studies concerning OASIs where episiotomy angles were measured. There is evidence that episiotomies angled too close to the midline are at higher risk of causing OASI. The incidence of OASI in units that practise midline episiotomies is 7–20 % [19, 64, 71, 72]. In a quasirandomised trial, Coats et al. [73] found that 24 % of midline episiotomies in primiparous women were associated with OASIs in contrast to 2 % of mediolateral episiotomies. With mediolateral episiotomies, the absolute risk of OASI is 10 % with a suture angle of 25°. This risk reduces by 50 % for every 6° the episiotomy is angled away from the midline, and reduces to 0.5 % with a 45° suture angle [13–15]. However, if the episiotomy angle becomes nearly horizontal (90°), the pressure on the perineum is not relieved and the incidence of OASI increases ninefold [15].
The current NICE recommendation is to cut an episiotomy at 45–60° lateral to the midline. However, it has been shown that a 40° episiotomy results in a suture angle of 22–24° [35, 74]. Based on this work and other perineal distension data [36–38, 74], it would be reasonable to infer that a 45° episiotomy will result in a suture angle of <30°, and therefore increase the risk of OASI. An episiotomy cut at 60° has been shown to result in a suture angle of 43° in a series of instrumental deliveries [37], 45° in a combined series of spontaneous and instrumental births [36] and 50° in spontaneous births [38]. A recent randomised study in Egypt in nulliparous women found OASI in 2.4 % of those who had an episiotomy cut at 60° versus 5.5 % in those who had an episiotomy cut at 40° to the midline, although the difference is not statistically significant because the study was underpowered [74]. In view of the current evidence, the guidelines of the Royal College of Obstetricians and Gynaecologists (UK) recommend a 60° episiotomy at crowning (RCOG, in press).
Current practice of performing non-median episiotomies
Andrews et al. [13] found that no midwives and only 22 % of doctors were performing mediolateral episiotomies resulting in a suture angle of 40–60°. The mean angle achieved by midwives was 20° and that by doctors was 27°. Only one-third of episiotomies were ≥40°. In a study of 300 episiotomies, Fodstad et al. found considerable variation in the angle and distance from the midline [19]: 7 % were median/midline (suture angles <25°), 13 % were mediolateral (25–60° and distance from posterior fourchette ≤3 mm), 36 % were described as ‘nonclassifiable’, and 44 % were lateral (25–60° and sutured episiotomy >10 mm away from posterior fourchette). However this may be a reflection of the difficulty in perceiving the size and angle of an episiotomy. There seems to be difficulty in visually estimating angles even in ex-vivo settings. Tincello et al. [70] found only one-third of clinicians were able to draw an episiotomy of ≥40° on paper. A recent study using a simulation model found that only 13 % of midwives and 7 % doctors were able to perform an accurate mediolateral episiotomy [76]. When asked to cut an episiotomy at 60° with straight Mayo scissors on a perineum drawn on paper, only 15 % of doctors were able to cut an angle in the range 58–62°, and 36 % in the range 55–65° [77], and 44 % underestimated the angle (<55°) and 18 % overestimated the angle (>65°). In another study, Naidu et al. found a poor correlation between actual and perceived length of the index finger and anal sphincter in simulation models [78].
Episiotomy (or more accurately ‘perineotomy’) per se will relieve pressure on the central posterior perineum as long as it is not started too lateral and has a postdelivery suture angle of >60° [15]. If it is too close to the midline (<30° postdelivery suture angle), then there is a likelihood of direct physical injury to the anal sphincters of about 10 % [14]. There might also be an association between OASI and the length and depth of the episiotomy. Based on current evidence, it would appear that an episiotomy suture angle of 40–60° would place it within the safe zone. However, it should be appreciated that perineal distension/stretching at crowning makes it difficult to estimate the required incision angle.
Origination point of episiotomy
A lateral episiotomy is defined as an incision that begins in the vaginal introitus 1–2 cm lateral to the midline and is directed downwards towards the ischial tuberosity [15, 19]. The risk of OASI has been shown to reduce by 56 % for every 4.5 mm away from the midline [15]. In another study, nearly all the women with OASI had an episiotomy within 10 mm of the midline [19]. Safe distances of 9 mm [15] and 10.5 mm [19] from the posterior fourchette have been suggested to reduce the risk of OASI.
Length and depth of episiotomy
Perineal pressure on the central posterior perineum may be relieved only by episiotomies of a certain length and depth. Stedenfeldt et al. [15] found that the rate of OASI is lower for sutured episiotomies longer than 17 mm with a depth of >16 mm. The risk reduces by 75 % for every 5.5-mm increase in length of the episiotomy.
Perineal protection
A Cochrane review of perineal protection techniques [16] found no difference in the incidence of OASIs between ‘hands-on’ and ‘hands-off’ approaches, and no significant difference when the Ritgen manoeuvre was used. Warm perineal compresses were beneficial in reducing the incidence of OASI. Although the mechanism of action remains uncertain, this approach may well reduce perineal oedema. A Cochrane review of antenatal perineal massage [79] found no reduction in the incidence of OASI.
Two studies have compared the impact of hands-on versus hands-off approaches in time-series analyses [17, 18]. Laine et al. [17] reported their findings from a single centre in Norway. They reported OASI rates during two consecutive, 3-year time periods. During the second period they introduced an intervention programme consisting of the following: (a) training on a pelvic delivery model, (b) hands on supervision at delivery, (c) two accoucheurs at delivery during the training phase, (d) slowing delivery of the head, asking the woman not to push, applying perineal support with the thumb, first and second fingers to reduce pressure on the middle part of the posterior perineum, and (e) training in performing non-median episiotomy away from the midline. No documentation of the type of episiotomy was available, nor was the angle of the sutured episiotomy recorded. The incidence of OASI declined from 4 % to 1.9 % from the first to the second triennial period, but it is difficult to weight the different components of the intervention programme. The number of nulliparous women who had an episiotomy during spontaneous delivery declined from 24 % to 22 %. The incidence of OASI in this group declined from 4 % to 2.2 %, a relative risk reduction of 45 %. However, the incidence of OASI in women who did not have an episiotomy during spontaneous delivery also declined from 5 % to 2.5 %, a relative risk reduction of 50 %. In this group, there does not appear to have been any contribution of training in the different episiotomy technique. The effect size of manual perineal protection could have been contributory to a reduction in the OASI rate in both groups, or alternatively, the presence of a second accoucheur could have contributed qualitatively to better decision-making regarding episiotomies. Whether these data are applicable to countries with lower episiotomy rates such as the UK needs to be established. However, there is emerging evidence from a study in the UK that manual perineal support may reduce the risk of severe OASI [80].
In women having an instrumental delivery, the incidence of episiotomy increased from 60 % to 85 % between the first and second triennial period. The OASI rate reduced from 11.1 % to 3.8 % in women with an episiotomy, either due to an increase in the number of episiotomies or a change in the episiotomy technique. The incidence of OASI in women without an episiotomy during instrumental delivery remained similar at 12 % and 10.9 % in the two triennial periods, respectively (p = 0.064). This suggests that an increase in the number of episiotomies or possibly a change in episiotomy technique was contributory to the reduction in the rate of OASI. However, it would be difficult to quantify the effect size without data on postdelivery episiotomy angles. In a study by the same authors [19], conducted in the same institution during 2010–2011 (after the second triennial period), the overall OASI rate was 4 %. This study revealed a spectrum of episiotomy performance. The incidence of OASI was 20 % (4/20) in midline group, 10 % (4/38) in the mediolateral group, and 4 % in the nonclassifiable group; OASI did not occur in the lateral group. This study illustrates that despite training, clinicians find it difficult to consistently get the angles and measurements right at the time of cutting the episiotomy.
Fretheim et al. [18] reevaluated a five-hospital intervention programme in Norway, which had previously shown a reduction in the rate of OASI from 4–5 % to 2 % following the introduction of the hands-on technique. Their re-analysis showed a 2 % absolute reduction in the rate of OASI. However, with a 10 % average increase in postintervention episiotomy rate to 25 %, they questioned whether hands-on delivery or episiotomy was responsible for the decreased OASI rate.
Instrumental deliveries
Two randomised trials showed a lower rate of OASI with vacuum delivery than with forceps [81, 82]. A Cochrane review [83] found that the incidence of OASI was significantly higher with forceps than with vacuum delivery (RR 1.9, 1.5–2.4), irrespective of whether an episiotomy had been performed. Due to heterogeneity among the different studies, a difference in outcomes between episiotomies and spontaneous tears could not be established. However, the authors noted that women who sustained an OASI were more likely to have a forceps delivery following a failed ventouse delivery. Analysis of Hospital Episode Statistics (HES) data from half of all first vaginal births in England for the period April 2000 to March 2012 showed that OASI rates were threefold to fourfold higher with forceps delivery without episiotomy (22 %) than with forceps delivery with episiotomy (6 %). A similar threefold increase was seen for ventouse deliveries (2.3 % vs. 6.4 %) [5].
Analysis of data from the Danish National Registry for the period 2000 to 2010 showed that mediolateral episiotomy is protective against OASI in vacuum delivery (OR 0.60) [54]. Analysis of data from the New South Wales birth registry for the period 2001 to 2009 showed a sixfold increased risk of OASI in forceps delivery without episiotomy [84]. Similarly, analysis of the Dutch National Registry showed that mediolateral episiotomy is protective against OASI in both vacuum delivery (OR 0.11) and forceps delivery (OR 0.08) [85]. NICE recommends mediolateral episiotomy for instrumental births [66].
Sequential instrumental use of vacuum and forceps has been shown to increase the risk of OASI 1.8-fold compared with single instrument use [86]. This highlights the need to choose the most appropriate instrument at first attempt and in particular, the best type of cup for vacuum deliveries. If the appropriately chosen instrument is applied correctly and fails, caesarean section should be considered.
Conclusion
To reduce the risk of OASI, relieving pressure on the central part of the posterior perineum by performing a safely angled episiotomy at 60° when indicated, and slow controlled delivery of the head should be important considerations in vaginal delivery. Application of digital perineal support to relieve perineal pressure needs to be standardised, and is an area for further research. Women with a short PL in the first stage of labour (<30 mm) are more likely to sustain perineal tears in general and are also at higher risk of sustaining OASI. Episiotomies performed in these women should be angled even further away from the midline to avoid OASI. Further research is needed to determine whether they would benefit from elective episiotomy.
Perineal distension leads to a 50 % increase in PL, a 170 % increase in transverse length and a 50–100 % increase in angular dimensions at crowning. This leads to a 15–30° difference between the incision angle and suture angle of the episiotomy and can make estimating the episiotomy angle, length and depth difficult. An episiotomy will relieve perineal pressure at crowning if it is not too lateral and not too short. The ideal depth of the episiotomy is unknown but if it is inadequate, additional tears or episiotomy extension would be inevitable. The angle of the episiotomy is an important determinant of OASI risk. Irrespective of the stated intention of the accoucheur (i.e. midline or mediolateral), if the resultant episiotomy suture angle is ≤30°, the incidence of OASIs can be as high as 10–20 %. Episiotomies should be performed within the safe zone of 40–60° (as measured after delivery). To achieve this, a 60° episiotomy should be performed. Steps should be taken to reduce human error in performing incorrectly angled episiotomies, by either using special scissors [37, 38] or other validated techniques.
As all randomised studies in the Cochrane review regarding the liberal versus restrictive use of mediolateral episiotomies were not controlled for the angle of episiotomy, the data need to be interpreted with caution, and further studies need to be performed with standardised angles of episiotomy. It is also important that doctors and midwives undergo a training programme to detect OASIs [87], as there is considerable evidence that these injuries have been underdiagnosed [88, 89].
References
Oberwalder M, Connor J, Wexner SD (2003) Meta-analysis to determine the incidence of obstetric anal sphincter damage. Br J Surg 90:1333–1337
Mous M, Muller SA, de Leeuw JW (2008) Long term effects of anal sphincter rupture during vaginal delivery: fecal incontinence and sexual complaints. BJOG 115:234–238
Evers EC, Blomquist JL, McDermott KC, Handa VL (2012) Obstetrical anal sphincter laceration and anal incontinence 5-10 years after childbirth. Am J Obstet Gynecol 207:425.e1–425.e6
Soerensen MM, Buntzen S, Bek KM, Laurberg S (2013) Complete obstetric anal sphincter tear and risk of long-term fecal incontinence: a cohort study. Dis Colon Rectum 56:992–1001
Gurol-Urganci I, Cromwell D, Edozien L, Mahmood T, Adams E, Richmond D, Templeton A, van der Meulen J (2013) Third- and fourth-degree perineal tears among primiparous women in England between 2000 and 2012: time trends and risk factors. BJOG 120(12):1516–1525
Thiagamoorthy G, Johnson A, Thakar R, Sultan AH (2014) National survey of perineal trauma and its subsequent management in the United Kingdom. Int Urogynecol J 25(12):1621–1627
Sultan AH, Kamm MA, Hudson CN, Bartram CI (1994) Third degree obstetric anal sphincter tears: risk factors and outcome of primary repair. BMJ 308:887–891
Fitzpatrick M, McQuillan K, O'Herlihy C (2001) Influence of persistent occiput posterior position on delivery outcome. Obstet Gynecol 98:1027–1031
de Leeuw JW, Struijk PC, Vierhout ME, Wallenburg HC (2001) Risk factors for third degree perineal ruptures during delivery. BJOG 108:383–387
Wu JM, Williams KS, Hundley AF, Connolly A, Visco AG (2005) Occiput posterior fetal head position increases the risk of anal sphincter injury in vacuum-assisted deliveries. Am J Obstet Gynecol 193:525–529
Benavides L, Wu JM, Hundley AF, Ivester TS, Visco AG (2005) The impact of occiput posterior fetal head position on the risk of anal sphincter injury in forceps-assisted vaginal deliveries. Am J Obstet Gynecol 192:1702–1706
Revicky V, Nirmal D, Mukhopadhyay S, Morris EP, Nieto JJ (2010) Could a mediolateral episiotomy prevent obstetric anal sphincter injury? Eur J Obstet Gynecol Reprod Biol 150:142–146
Andrews V, Thakar R, Sultan AH, Jones PW (2005) Are mediolateral episiotomies actually mediolateral? BJOG 112:1156–1158
Eogan M, Daly L, O'Connell PR, O'Herlihy C (2006) Does the angle of episiotomy affect the incidence of anal sphincter injury? BJOG 113:190–194
Stedenfeldt M, Pirhonen J, Blix E, Wilsqaard T, Vonen B, Qian P (2012) Episiotomy characteristics and risks for obstetric anal sphincter injury: a case-control study. BJOG 119:724–730
Aasheim V, Nilsen ABV, Lukasse M, Reinar LM (2011) Perineal techniques during the second stage of labour for reducing perineal trauma. Cochrane Database of Systematic Reviews, Issue 12. Art. No.: CD006672. doi:10.1002/14651858.CD006672.pub2
Laine K, Skjeldestad FE, Sandvik L, Staff AC (2012) Incidence of obstetric anal sphincter injuries after training to protect the perineum: cohort study. BMJ Open 2, e001649. doi:10.1136/bmjopen-2012-001649
Fretheim A, Odgaard-Jensen J, Røttingen J-A et al (2013) The impact of an intervention programme employing a hands-on technique to reduce the incidence of anal sphincter tears: interrupted time-series reanalysis. BMJ Open 3, e003355. doi:10.1136/bmjopen-2013-003355
Fodstad K, Laine K, Staff AC (2013) Different episiotomy techniques, postpartum perineal pain, and blood loss: an observational study. Int Urogynecol J 24:865–872
Green JR, Soohoo S (1989) Factors associated with rectal injury in spontaneous deliveries. Obstet Gynecol 73:732–738
Zemcik R, Karbanova J, Kalis V, Lobovsky L, Jansova M, Rusavy Z (2012) Stereophotogrammetry of the perineum during vaginal delivery. Int J Gynaecol Obstet 119:76–80
Jansova M, Kalis V, Rusavy Z, Zemcik R, Lobovsky L, Laine K (2014) Modelling manual perineal protection during vaginal delivery. Int Urogynecol J 25:65–71
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, Shull BL, Smith AR (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–17
Cundiff GW, Harris RL, Coates K, Low VH, Bump RC, Addison WA (1997) Abdominal sacral colpoperineopexy: a new approach of posterior compartment defects and perineal descent associated with vaginal vault prolapse. Am J Obstet Gynecol 177:1345–1353
Delancey JO, Hurd WW (1998) Size of the urogenital hiatus in the levator ani in normal women and women with pelvic organ prolapse. Obstet Gynecol 91:364–368
Deering SH, Carlson N, Stitely M, Allaire AD, Satin AJ (2004) Perineal body length and lacerations at delivery. J Reprod Med 49:306–310
Rizk DEE, Abadir MN, Thomas LB, Abu-Zidan F (2005) Determinants of the length of episiotomy or spontaneous perineal lacerations during vaginal birth. Int Urogynecol J 16:395–400
Dua A, Whitworth M, Dugdale A, Hill S (2009) Perineal length: norms in gravid women in the first stage of labour. Int Urogynecol J 20:1361–1364
Tsai PS, Oyama IA, Hiraoka M, Minaglia S, Thomas J, Kaneshiro B (2012) Perineal body length among different racial groups in the first stage of labour. Female Pelvic Med Reconstr Surg 18:165–167
Geller EJ, Robinson BL, Matthews CA, Celauro KP, Dunivan GC, Crane AK, Ivins AR, Woodham PC, Fielding JR (2014) Perineal body length as a risk factor for ultrasound-diagnosed anal sphincter tear at first delivery. Int Urogynecol J 25:631–636
Lai CY, Cheung HW, His Lao TT, Lau TK, Leung TY (2009) Is the policy of restrictive episiotomy generalizable? A prospective observational study. J Matern Fetal Neonatal Med 22:1116–1121
Walfisch A, Hallak M, Harley S, Mazor M, Shoham-Vardi I (2005) Association of spontaneous perineal stretching during delivery with perineal lacerations. J Reprod Med 50:23–28
Kalis V, Karbanova J, Bukacova Z, Bednarova B, Rokyta Z, Kralickova M (2010) Anal dilatation during labor. Int J Gynaecol Obstet 109:136–139
Aytan H, Tapisiz OL, Tuncay G, Avsar FA (2005) Severe perineal lacerations in nulliparous women and episiotomy type. Eur J Obstet Gynecol Reprod Biol 121:46–50
Kalis V, Karbanova J, Horak M, Lobovsky L, Kralickova M, Rokyta Z (2008) The incision angle of mediolateral episiotomy before delivery and after repair. Int J Gynaecol Obstet 103:5–8
Kalis V, Landsmanova J, Bednarova B, Karbanova J, Laine K, Rokyta Z (2011) Evaluation of the incision angle of mediolateral episiotomy at 60 degrees. Int J Gynaecol Obstet 112:220–224
Freeman RM, Hollands H, Barron L, Kapoor DS (2014) Cutting a mediolateral episiotomy at the correct angle: evaluation of a new device: the Episcissors-60. Med Devices (Auckl) 7:23–28. doi:10.2147/MDER.S60056
Patel R, Ubale S (2014) Evaluation of the angled Episcissors-60(®) episiotomy scissors in spontaneous vaginal deliveries. Med Devices (Auckl) 7:253–256
Lien KC, Mooney B, DeLancey JO, Ashton-Miller JA (2004) Levator ani muscle stretch induced by simulated vaginal birth. Obstet Gynecol 103:31–40
Eliashiv O, Ginath S, Weiner E, Sadan O, Golan A, Condrea A (2013) Mediolateral episiotomy-is the angle of incision performed at crowning the correct and desired one? Int Urogynecol J 24:S68
Samuelsson E, Ladfors L, Wennerholm UB, Gareberg B, Nyberg K, Hagberg H (2000) Anal sphincter tears: prospective study of obstetric risk factors. BJOG 107:926–931
Handa VL, Danielsen BH, Gilbert WM (2001) Obstetric anal sphincter lacerations. Obstet Gynecol 98:225–230
Combs CA, Roberston PA, Laros RK (1990) Risk factors for third and fourth degree perineal lacerations in forceps and vacuum deliveries. Am J Obstet Gynecol 163:100–104
Hopkins LM, Caughey AB, Glidden DV, Laros RK Jr (2005) Racial/ethnic differences perineal, vaginal and cervical lacerations. Am J Obstet Gynecol 193:455–459
Howard D, Davies PS, Delancey JOL, Small Y (2000) Differences in perineal lacerations in black and white primiparas. Obstet Gynecol 96:622–624
Donnelly V, Fynes M, Campbell D, Johnson H, O'Connell PR, O’Herlihy C (1998) Obstetric events leading to anal sphincter damage. Obstet Gynecol 92:955–961
Andrews V, Sultan AH, Thakar R, Jones PW (2006) Risk factors for obstetric anal sphincter injury: a prospective study. Birth 33:117–122
Gottvall K, Allebeck P, Ekéus C (2007) Risk factors for anal sphincter tears: the importance of maternal position at birth. BJOG 114:1266–1272
Richter HE, Nager CW, Burgio KL, Whitworth R, Weidner AC, Schaffer J et al (2015) Incidence and predictors of anal incontinence after obstetric anal sphincter injury in primiparous women. Female Pelvic Med Reconstr Surg. doi:10.1097/SPV.0000000000000160
Aiken CE, Aiken AR, Prentice A (2015) Influence of the duration of the second stage of labor on the likelihood of obstetric anal sphincter injury. Birth 42:86–93
Fitzpatrick M, Harkin R, McQuillan K, O'Brien C, O'Connell PR, O'Herlihy C (2002) A randomised clinical trial comparing the effects of delayed versus immediate pushing with epidural analgesia on mode of delivery and faecal continence. BJOG 109:1359–1365
Christianson LM, Bovbjerg VE, McDavitt EC, Hullfish KL (2003) Risk factors for perineal injury during delivery. Am J Obstet Gynecol 189:255–260
Rygh AB, Skjeldestad FE, Körner H, Eggebø TM (2014) Assessing the association of oxytocin augmentation with obstetric anal sphincter injury in nulliparous women: a population-based, case-control study. BMJ Open 4(7), e004592. doi:10.1136/bmjopen-2013-004592
Jango H, Langhoff-Roos J, Rosthoj S, Sakse A (2014) Modifiable risk factors for obstetric anal sphincter injury in primiparous women: a population based cohort study. Am J Obstet Gynecol 210:59.e1–59.e6
Baumann P, Hammoud AO, McNeeley SG, DeRose E, Kudish B, Hendrix S (2007) Factors associated with anal sphincter laceration in 40,923 primiparous women. Int Urogynecol J 18:985–990
Roos A-M, Thakar R, Sultan AH (2010) Outcome of primary repair of obstetric anal sphincter injuries (OASIS): does the grade of tear matter? Ultrasound Obstet Gynecol 36(3):368–374
Martin DL (1921) The protection of the perineum by episiotomy in delivery at term. Cal State J Med 19:229–231
DeLancey JO (1992) Anatomic aspects of vaginal eversion after hysterectomy. Am J Obstet Gynecol 166:1717–1724
Gainey HL (1943) Postpartum observation of pelvic tissue damage. Am J Obstet Gynecol 45:457–466
Gainey HL (1955) Postpartum observation of pelvic tissue damage: further studies. Am J Obstet Gynecol 70:800–807
Ranney B (1990) Decreasing numbers of patients for vaginal hysterectomy and plasty. S D J Med J 43:7–12
Patel DA, Xu X, Thomason AD, Ransom SB, Ivy JS, DeLancey JO (2006) Childbirth and pelvic floor dysfunction: an epidemiological approach to the assessment of prevention opportunities at delivery. Am J Obstet Gynecol 195:23–28
DeLancey JOL (2008) Episiotomy: what’s the angle? Int J Gynaecol Obstet 103:3–4
Fenner DE, Genberg B, Brahma P, Marek L, DeLancey JO (2003) Fecal and urinary incontinence after vaginal delivery with anal sphincter disruption in an obstetrics unit in the United States. Am J Obstet Gynecol 189:1543–1549
Carroli G, Mignini L (2009) Episiotomy for vaginal birth. Cochrane Database of Systematic Reviews, Issue 1. Art. No.: CD000081. doi:10.1002/14651858.CD000081.pub2
National Institute for Health and Care Excellence (2007) Intrapartum care: care of healthy women and their babies during childbirth. NICE guidelines CG55. London: National Institute for Health and Care Excellence. http://www.nice.org.uk/guidance/cg55
Raisanen S, Selander T, Cartwright R, Gissler M, Kramer MR et al (2014) The association of episiotomy with obstetric anal sphincter injury – a population based matched cohort study. PLoS One 9(9), e107053. doi:10.1371/journal.pone.0107053
Kalis V, Laine K, de Leeuw JW, Ismail KM, Tincello DG (2012) Classification of episiotomy: towards a standardisation of terminology. BJOG 119:522–526
Beischer NA, MacKay EV (1986) Episiotomy. In: Obstetrics and The Newborn. London: Bailliere Tindall. Obstetric procedures. In: Chamberlain GVP (ed). Obstetrics by Ten Teachers. London: Arnold, 1995:285–303
Tincello DG, Williams A, Fowler GE, Adams EJ, Richmond DH, Alfirevic Z (2003) Differences in episiotomy technique between midwives and doctors. BJOG 110:1041–1044
Angioli R, Gomez-Marin O, Cantuaria G, O’Sullivan MJ (2000) Severe perineal lacerations during vaginal delivery: the University of Miami experience. Am J Obstet Gynecol 182:1083–1085
Sooklim R, Thinkhamrop J, Lumbiganon P, Prasertcharoensuk W, Pattamadilok J, Seekorn K, Chongsomchai C, Pitak P, Chansamak S (2007) The outcomes of midline versus medio-lateral episiotomy. Reprod Health 4:10
Coats PM, Chan KK, Wilkins M, Beard RJ (1980) A comparison between midline and mediolateral episiotomies. BJOG 87:408–412
El-Din AS, Kamal MM, Amin MA (2014) Comparison between two incision angles of mediolateral episiotomy in primiparous women: a randomised controlled trial. J Obstet Gynaecol Res 40:1877–1882
Gonzalez-Díaz E, Moreno Cea L, Fernández Corona A (2015) Trigonometric characteristics of episiotomy and risks for obstetric anal sphincter injuries in operative vaginal delivery. Int Urogynecol J 26:235–242
Silf K, Woodhead N, Kelly J, Fryer A, Kettle C, Ismail KM (2015) Evaluation of accuracy of mediolateral episiotomy incisions using a training model. Midwifery 31:197–200
Naidu M, Kapoor DS, Evans S, Vinayakarao L, Thakar R, Sultan AH (2015) Cutting an episiotomy at 60 degrees: how good are we? Int Urogynecol J 26:813–816. doi:10.1007/s00192-015-2625-9
Naidu M, Sultan AH, Thakar R (2014) Getting the size right: are gynaecologists ready for it? Int Urogynecol J 25:S86
Beckmann MM, Stock OM (2013) Antenatal perineal massage for reducing perineal trauma. Cochrane Database of Systematic Reviews, Issue 12. Art. No.: CD005123. doi:10.1002/14651858.CD005123.pub3
Naidu M, Sultan AH, Thakar R (2014) Reducing obstetric anal sphincter injuries using perineal support: a preliminary experience. Female Pelvic Med Reconstr Surg 20:S12
Johanson RB, Rice C, Doyle M, Arthur J, Anyanwu L, Ibrahim J, Warwick A, Redman CW, O’Brien PM (1993) A randomised prospective study comparing the new vacuum extractor policy with forceps delivery. BJOG 100:524–530
Fitzpatrick M, Behan M, O’Connell PR, O’Herlihy C (2003) Randomised clinical trial to assess anal sphincter function following forceps or vacuum assisted vaginal delivery. BJOG 110(4):424–429
O’Mahony F, Hofmeyr GJ, Menon V (2011) Choice of instruments for assisted vaginal delivery. Cochrane Database of Systematic Reviews, Issue 11. Art. No.: CD005455. doi:10.1002/14651858.CD005455.pub2
Ampt AJ, Ford JB, Roberts CL, Morris JM (2013) Trends in obstetric anal sphincter injuries and associated risk factors for vaginal singleton term births in New South Wales 2001-2009. Aust N Z J Obstet Gynaecol 53(1):9–16
De Leeuw JW, de Wit C, Kuijken JP, Bruinse HW (2008) Mediolateral episiotomy reduces the risk of anal sphincter injury during operative delivery. BJOG 115:104–108
Murphy DJ, MacLeod M, Bahl R, Strachan B (2011) A cohort of maternal and neonatal morbidity in relation to use of sequential instruments at operative vaginal delivery. Eur J Obstet Gynecol Reprod Biol 156:41–45
Andrews V, Thakar R, Sultan AH, Kettle C (2005) Can hands-on perineal repair courses affect clinical practice. Br J Midwifery 13(9):562–565
Sultan AH, Kamm MA, Hudson CN, Thomas JM, Bartram CI (1993) Anal sphincter disruption during vaginal delivery. N Engl J Med 329:1905–1911
Andrews V, Thakar R, Sultan AH, Jones PW (2006) Occult anal sphincter injuries – myth or reality? BJOG 113:195–200
Rizk DEE, Thomas L (2000) Relationship between the length of the perineum and position of the anus and vaginal delivery in primigravidae. Int Urogynecol J 11:79–83
Acknowledgments
Funding sources
None.
Conflicts of interest
D.S. Kapoor is a co-inventor of the Episcissors-60 episiotomy scissors. He is a shareholder of Medinvent Ltd., the company that owns the commercial rights to the scissors.
A.H Sultan: none.
R. Thakar: IUGA Secretary.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kapoor, D.S., Thakar, R. & Sultan, A.H. Obstetric anal sphincter injuries: review of anatomical factors and modifiable second stage interventions. Int Urogynecol J 26, 1725–1734 (2015). https://doi.org/10.1007/s00192-015-2747-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-015-2747-0