Abstract
Purpose
The present study assessed the effect of insert articular surface geometry (anatomical versus conventional insert design) on anteroposterior (AP) translation and varus-valgus (VV) laxity in balanced posterior cruciate ligament (PCL) retaining total knee arthroplasty (TKA). Secondly, we evaluated if the AP translation and VV laxity in the reconstructed knee resembled the stability of the native knee.
Methods
Nine fresh-frozen full-leg cadaver specimens were used in this study. After testing the native knee, anatomical components of a PCL-retaining implant were implanted. The knee joints were subjected to anteriorly and posteriorly directed forces (at 20° and 90° flexion) and varus-valgus stresses (at 20°, 45° and 90° flexion) in both non-weightbearing and weightbearing situations in a knee kinematics simulator. Measurements were performed in the native knee, TKA with anatomical insert geometry (3° built-in varus, medial concave, lateral convex), and TKA with symmetrical insert geometry.
Results
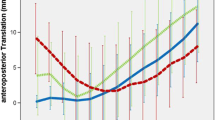
In weightbearing conditions, anterior translations ranged between 2.6 and 3.9 mm at 20° flexion and were < 1 mm at 90° flexion. Posterior translation at 20° flexion was 2.7 mm for the native knee versus 4.0 mm (p = 0.047) and 7.0 mm (p = 0.02) for the symmetrical insert and the anatomical insert, respectively. Posterior translation at 90° flexion was < 1.1 mm and not significantly different between the native knee and insert types.
In non-weightbearing conditions, the anterior translation at 20° flexion was 5.9 mm for the symmetrical and 4.6 mm for the anatomical insert (n.s.), compared with 3.0 mm for the native knee (p = 0.02). The anterior translation at 90° flexion was significantly higher for the reconstructed knees (anatomical insert 7.0 mm; symmetrical insert 9.2 mm), compared with 1.6 mm for the native knee (both p = 0.02). Varus-valgus laxity at different flexion angles was independent of insert geometry. A valgus force in weightbearing conditions led to significantly more medial laxity (1°–3° opening) in the native knee at 45° and 90° flexion compared with the reconstructed knee for all flexion angles.
Conclusions
Insert geometry seems to have a limited effect with respect to AP translation and VV laxity, in the well-balanced PCL-retaining TKA with an anatomical femoral component. Secondly, AP translation and VV laxity in the reconstructed knee approximated the laxity of the native knee.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Posterior cruciate ligament (PCL) retention in total knee arthroplasty (TKA) may lead to better proprioception compared with PCL-sacrificing (PS) TKA, due to the presence of mechanoreceptors in the ligament [4, 13]. To obtain near-normal knee kinematics in PCL-retaining TKA, the normal articulating position of the medial femoral condyle on the tibia should be restored [6]. Next to a correct contact point, proper PCL balancing will help to reproduce healthy/normal anteroposterior (AP) translation; a PCL which is too loose in flexion results in increased translation in flexion and paradoxical forward femoral sliding [2, 23].
Good functional outcomes have been reported with an AP translation less than 10 mm [15, 17]. However, the optimal anteroposterior and varus-valgus laxity after TKA, and its relation with postoperative achieved patient satisfaction, postoperative ROM, and knee function are unclear [12, 14]. Seah et al. reported that patients obtain a beneficial result from surgery if they have less than 5° of combined varus-valgus laxity postoperatively [16].
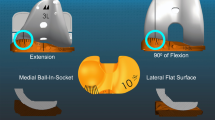
In addition to proper PCL-balancing by adjusting the tibial slope and restoring the natural step-off, a well-designed implant is an important factor for a successful TKA [18]. Recently, implants were introduced that resemble the anatomy of the native knee. These implants have 3° of joint line obliquity in the coronal plane and an accommodating insert. In the anatomical design, the medial surface of the insert is concave and the lateral surface is convex, consistent with the native anatomy of the tibia surface. However, a convex lateral insert surface geometry could result in more lateral AP translation due to the less constraining design compared to a dished insert, but may be compensated for by the concave medial surface with a clear posterior rim.
To date, the effects of anatomical insert design on anteroposterior and varus-valgus laxity have not been investigated in PCL-retaining TKA. However, several in vitro studies have investigated the amount of laxity after non-anatomical TKA compared to the native knee [1, 5, 8, 11]. Hunt et al. found comparable laxity in the single radius PCL-retaining TKA compared to the native knee in a cadaveric study [8] whereas Lo et al. found [11] increased posterior laxity in PCL-retaining TKA with symmetrical inserts compared to the native knee and the bicruciate-retaining (BCR) TKA.
Therefore, the aim of the present study was to test the anterior–posterior and varus-valgus stability of the anatomical insert and evaluate the effect of anatomical insert geometry (medial concave – lateral convex), compared to the conventional symmetrical concave insert design on anterior–posterior (AP) translation and varus-valgus (VV) laxity in PCL-retaining TKA. We hypothesized that (1) an anatomical insert results in similar anteroposterior translation compared with the symmetrical insert, (2) AP translation in the reconstructed knee resembles the stability of the native knee, and (3) VV laxity is independent of insert design.
Materials and methods
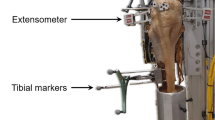
In this cadaveric study, knee joints were subjected to anteriorly and posteriorly directed forces and varus-valgus stresses under different flexion angles in both non-weightbearing and weightbearing situations using a knee kinematics simulator. AP translation and varus-valgus laxity were recorded using six infrared motion capture cameras. The measurements were repeated for the native knee, TKA with anatomical insert geometry, and TKA with symmetrical insert geometry (Fig. 1). Trials were performed in triplicate and the averages of the three measurements were calculated and used for further analysis.
Design of anatomical insert with medial concave and lateral convex surface geometry (a), and design of symmetrical insert (b) and projections of the contour lines of both inserts (c). Rim heights are given with respect to the corresponding sulcus. The medial sulcus lies 2.5 mm lower than the lateral sulcus for the anatomical insert
Specimens
A total of nine freshly frozen, full-leg cadaver specimens were used. Medical records of the donors showed that they had no known history of musculoskeletal problems at the investigated knee joint. Four specimens were left specimens; two specimens were from female donors. The donors’ ages ranged from 61 to 80 years, with an average of 71 (SD 8.7) years.
Experimental setup and specimen preparation
The experimental setup and methodology have been described in detail previously [6, 20]. In short, after identifying the centres of the femoral head and the ankle with the navigation system, the femoral head and ankle were removed and the femur and tibia plus fibula were cut to lengths of 32 and 28 cm, respectively. Both bones were cleaned and embedded in aluminum fixtures with PMMA, ensuring proper alignment in the coronal and sagittal planes. Afterwards, the quadriceps tendon was dissected, stripped from all muscle tissue and securely fixed in a clamp. Also, the medial (semitendinosus and semimembranosus) and lateral (biceps femoris) hamstrings tendons were dissected, and suture wires were attached to enable loading of the hamstrings (50 N on medial and 50 N on the lateral side) during testing [20].
Surgical technique and implant
After measurements (see detailed description below) of the native knee, the knee was opened and the integrity of the PCL in the specimens was confirmed visually as well as by posterior laxity testing at 90° flexion. Subsequently, components of a Journey CR TKA (Smith and Nephew, Memphis, TN, USA) were implanted. The Journey CR TKA is an anatomically designed implant, with an asymmetrical tibial baseplate and an accommodating insert with a concave medial and a convex lateral surface geometry (Fig. 1a). The femoral component has an extended posterior condyle facilitated by an upslope posterior bone cut [6]. A computer navigation system (PiGalileo, Smith and Nephew, Memphis, TN, USA) was used to assist with the bone cuts. The knee prosthesis was implanted using a measured resection technique, removing an amount of bone of femur and tibia equal to the prosthesis thickness in extension and flexion. First, mediolateral balancing in extension was performed with a spacer. A 3° external rotation jig was used to determine the femoral component rotation. A bony island around the PCL attachment on the tibia was preserved, and all ligaments were intact after finishing the bone cuts. No releases of the collateral ligaments or the PCL were performed. In this study, we used the spacer technique to balance the PCL, which has previously been described in detail [6, 22]. In essence, by reconstructing the natural step-off, the PCL will be balanced. If the step-off is too large after the bone cuts, the PCL is too tight. Where applicable, this was corrected by performing a recut of the tibia with the addition of slope.
To test the effect of insert surface geometry, the anatomical insert was removed and replaced by a symmetrical insert (Genesis 2, Smith and Nephew, Memphis, TN, USA). The test symmetrical inserts (Fig. 1b) were custom adapted by the manufacturer (Smith and Nephew, Memphis, TN, USA) to the anatomic knee system by changing the joint line from perpendicular to the tibial axis to 3° angulation to fit with the anatomic system. The surface geometry was not changed.
Measurements
After preparation, the specimen was mounted in a dynamic knee simulator system, based on the Oxford Rig, which was designed to simulate and record motions and loads during squatting [6].
The knee was brought to the required flexion angle by moving the hip joint down over the predefined distance. When the correct knee flexion angle was reached, the hip position was fixed. Where a weightbearing laxity test was performed, the hamstring tendons were hooked to the constant force springs and the quadriceps motor then started pulling gently on the tendon until the 3D force sensor, which was mounted underneath the ankle joint of the simulator registered the correct vertical ankle force of 130 N. If the laxity test was done in the non-weightbearing condition, no tension was applied to the quadriceps nor to the hamstring tendons. Previously, Victor et al. showed that this technique is sufficiently accurate and precise [19].
Trials were performed in triplicate and the averages of the three measurements were calculated and used for further analysis.
Laxity measurements
Anteroposterior translation
AP translation was tested by manually applying an anterior pulling force (i.e., anterior drawer) and posterior pushing (i.e., posterior drawer) force of 89 N at 20° flexion and 90° flexion, respectively, with a dynamometer. Anterior pulling was performed with a hook on the dynamometer, perpendicular to the tibia just below the joint line. Posterior pushing was performed with an adaptor on the dynamometer and perpendicular to the tibia. For the laxity test, AP translation of the specimens was defined as the difference in position of the femoral knee centre relative to the tibial knee centre. AP translation was reported in millimeters (mm). The marker trajectories during testing were recorded using six infrared motion capture cameras (Vicon, Oxford, UK) at 100 Hz.
Varus-valgus laxity
Varus-valgus stress tests were performed at 20°, 45° and 90° flexion with a force of 50 N perpendicular to the tibia at 30 cm below the joint line creating an external moment of 15 Nm by pulling with a dynamometer [FMI-220C5 Force Gauge (range 0–500 N, resolution 0.1 N) Alluris, Germany]. Weightbearing and non-weightbearing measurements for all laxity measurements were recorded. Varus-valgus laxity was reported in degrees. The marker trajectories during testing were recorded using six infrared motion capture cameras (Vicon, Oxford, UK) at 100 Hz.
Statistical analysis
Descriptive statistics were used to summarise the data. Differences in AP translation and varus-valgus laxity between the native knee, and the reconstructed knee with anatomical and symmetrical insert were tested using Friedman’s one-way repeated measures analysis of variance by ranks, followed by pairwise comparisons using Wilcoxon signed rank tests. Holm’s procedure was used to correct for multiple testing.
Results were reported as median (interquartile range). Statistical analyses were performed using R version 3.5.1 (R Foundation for Statistical Computing, Vienna, Austria). p < 0.05 was considered statistically significant.
Results
Anterior–posterior translation—weightbearing conditions
Median anterior translation at 20° flexion was 2.6 mm (1.4–3.3 mm) for the native knee versus 2.7 mm (1.7–3.5 mm) for the reconstructed knee with symmetrical insert, and 3.9 mm (2.1–4.9 mm) for the reconstructed knee with anatomical insert (Fig. 2). Median anterior translations for all tested knee conditions at 90° flexion were below 1.0 mm (Fig. 2).
There were no statistically significant differences in anterior translation between the native knee and the two insert types for the anterior drawer test at 20° and 90° flexion.
Median posterior translation at 20° flexion was 2.7 mm (2.2–4.9 mm) for the native knee, versus 4.0 mm (3.7–5.2 mm) for the reconstructed knee with symmetrical insert (n.s.). In the reconstructed knee with anatomical insert, a median posterior translation of 7.0 mm (6.2–7.9 mm) was measured at 20° flexion (Fig. 2). This was statistically significantly higher compared to the native knee (p = 0.047), as well as compared to the reconstructed knee with symmetrical insert (p = 0.02).
Median posterior translation at 90° flexion was 0.8 mm (0.6–1.1 mm) for the native knee, versus 0.3 mm (0.2–0.3 mm) for the reconstructed knee with symmetrical insert (p = 0.02). In the reconstructed knee with anatomical insert, a median posterior translation of 0.4 mm (0.3–0.8 mm) was recorded at 90° flexion. Compared to the native knee, this was not significant (n.s.). No statistically significant difference was found between the two insert types (n.s.).
Anterior–posterior translation—non-weightbearing conditions
Median anterior translation at 20° flexion was 3.0 mm (1.1–4.6 mm) for the native knee, versus 5.9 mm (3.3–6.8 mm) for the reconstructed knee with symmetrical insert (n.s.), and 4.6 mm (3.6–9.9 mm) for the anatomical insert (Fig. 2). The anterior translation in the anatomical insert was significantly higher compared with the native knee (p = 0.02), but no statistically significant difference was found between the two insert types (n.s.).
Median anterior translation at 90° flexion was 1.6 mm (1.5–1.8 mm) for the native knee, versus 9.2 mm (2.9–9.7 mm) for the reconstructed knee with the symmetrical insert and 7.0 mm (3.2–7.8 mm) for the anatomical insert (Fig. 2). The anterior translation for both insert types was also significantly higher compared to the native knee (anatomical insert p = 0.02; symmetrical insert p = 0.02), but no statistically significant difference was found between the two insert types (n.s.).
Median posterior translation at 20° flexion was 3.0 mm (2.2–3.9 mm) for the native knee, versus 6.5 mm (5.0–6.7 mm) for the reconstructed knee with a symmetrical insert (n.s.), and 5.4 mm (4.2–6.9 mm) for the anatomical insert (Fig. 2). There was no statistically significant difference between the anatomical insert and the native knee (n.s.). No statistically significant difference was found between the two insert types at 20° flexion (n.s).
Median posterior translation at 90° flexion was 2.3 mm (1.8–4.4 mm) for the native knee, versus 3.5 mm (2.7–5.9 mm) for the symmetrical insert (n.s.), and 2.9 mm (1.9–3.5 mm) for the anatomical insert (Fig. 2). There was no statistically significant difference between the anatomical insert and the native knee nor between the two insert types at 90° flexion (n.s.).
Varus-valgus laxity—weightbearing conditions
There were no statistically significant differences in varus laxity in response to a varus force between the anatomical and symmetrical insert and the native knee (Fig. 3).
Median valgus laxity in 20° flexion was 3.6° (2.1°–5.9°) for the native knee, versus 2.9° (1.0°–3.4°) for the reconstructed knee with symmetrical insert, and 2.4° (0.6°–3.3°) for the anatomical insert (Fig. 3). No statistically significant difference was found between the native knee and the symmetrical insert and between the two insert types (n.s.). There was no statistically significant difference between the native knee and the anatomical insert (n.s.).
Median valgus laxity at 45° flexion was 3.9° (2.5°–5.2°) for the native knee, versus 1.2° (0.7°–1.4°) for the reconstructed knee with symmetrical insert, and 1.3° (0.9°–2.4°) for the reconstructed knee with anatomical insert (Fig. 3). A statistically significant difference was found between the native knee and the symmetrical insert (p = 0.02), and for the native versus anatomical insert (p = 0.03).
Median valgus laxity at 90° flexion was 1.8° (1.3°–2.0°) for the native knee, versus 0.6° (0.4°–1.1°) for the reconstructed knee with symmetrical insert, and 1.4° (1.0°–1.5°) for the reconstructed knee with anatomical insert (Fig. 3). A statistically significant difference was found between the native knee and the symmetrical insert (p = 0.047), but not for the symmetrical insert versus anatomical insert (n.s.).
Varus-valgus laxity—non-weightbearing conditions
There was no statistically significant difference in medial and lateral laxity in response to a valgus or varus force for the anatomical and symmetrical insert versus the native knee (Fig. 3).
Discussion
The most important finding in this study was that the anatomical insert had a very limited effect on anterior–posterior translation compared with the symmetrical insert in PCL-retaining (CR) TKA. Only the posterior translation at 20° flexion was slightly higher (3 mm) for the anatomical insert under weightbearing conditions compared with the symmetrical insert. Secondly, anteroposterior translation for the anatomical insert was slightly increased in non-weightbearing conditions, with more anterior translation at 20° and 90° flexion compared to the native knee. Thirdly, varus-varus laxity was independent of insert type.
Anteroposterior translation of the anatomical insert resembled the amount of translation of the symmetrical insert. This is an important finding, because the lateral convex design is intrinsically less constrained. Only the posterior translation at 20° flexion in weightbearing conditions was increased compared to the symmetrical insert. This can be explained by the lower anterior rim of the anatomic insert combined with limited resistance of the PCL to posterior translation at 20° flexion. Apparently, the amount of dishing of the medial concave surface in combination with an increased posterior rim is sufficient to prevent extreme anterior translation. The symmetrical inserts have been used in vivo for years without concerns regarding longevity or stability. Whether the anatomical insert design translates into superior patient outcomes and long-term survival remains to be investigated in clinical studies.
Anteroposterior translation was mildly increased for the reconstructed knee compared to the native knee, especially in non-weightbearing conditions. The increased anterior translation can be explained by the effect of resection of the ACL [1]. Furthermore, at 20° flexion, the increase in anterior translation was less than 6 mm for the reconstructed knee. However, this increased laxity is less than previous biomechanical studies reported [5, 9, 11], although Arnout et al. found slightly decreased laxity in anatomical CR TKA [1]. In weightbearing conditions, these differences diminished. Posterior translation at 20° flexion in loaded conditions was increased for the anatomical insert compared to the native knee. As mentioned above, this can be explained by the less constrained design on the anteromedial side. In contrast, at 90° flexion in weightbearing conditions, posterior translation was higher for the native knee compared to the reconstructed knee independent of insert type. However, all conditions showed below 1 mm translation, so this difference seems not be clinically relevant. In our opinion, precise PCL balancing, by restoring the natural step-off, is an important contributor to the prevention of posterior translation.
Overall, at 90° flexion in weightbearing conditions, the native and reconstructed knee were very stable. This is in accordance with previous studies [19, 21]. In the present biomechanical study, this may be explained by the stabilising effect of the quadriceps force pushing the femoral and tibial articular surfaces (native and reconstructed) together and leading to less AP translation as a result.
Several biomechanical studies report inferior results in terms of AP translation in PCL-retaining TKA compared to the native knee [5, 11]. This is in contrast to our results, in which AP translation in the reconstructed knee resembled the translation of the native knee, independent of insert geometry. The total AP laxity after TKA in this study was slightly increased in the non-weightbearing knee at 20° flexion, but within the limits of the clinically-advised 10 mm [15, 17]. In our opinion, proper balancing of the PCL, for example with a spacer [6], is the key to a posteriorly stable knee and good kinematics. Unfortunately, most other studies do not report details about their PCL balancing technique [5, 11].
The currently tested insert designs differ from the medial pivot design. In medial pivot knees (and dished inserts in general), the dished shape leads to a ball and socket effect. Since the lowest point of the insert on the medial side is typically located in the posterior third of the AP distance of the tibia [3], this causes the femur to move posteriorly in extension. The design of the anteromedial side of the anatomical insert of the used implant system is much flatter to prevent this subluxation effect in extension [18]. Nevertheless, Jones et al. reported better sagittal stability and higher PROMs in medial pivot knees in vivo at 30 and 90° flexion when compared to non-medial pivot knees [10]. Further research is needed to clarify the clinical outcomes for these different designs.
The varus-valgus laxity was independent of insert design. This was to be expected, because only surface geometry was changed; thickness of the inserts was unchanged and therefore there was no difference in gap filling. This presumably results in a similar amount of ligament tension. With respect to varus-valgus laxity, we found that valgus laxity in the reconstructed knee was decreased compared to the native knee at 45 and 90° flexion under weightbearing conditions. However, the absolute differences are small, and this seems not to be clinically relevant. Decreased varus-valgus laxity in the reconstructed knee compared to the native knee is in accordance with other in vitro studies [1, 7, 9]. An explanation could be that the relative elasticity of the cartilage of the native knee is replaced by stiffer polyethylene, resulting in less laxity. A second explanation could be the relative loss of cartilage, but in the present study the human cadavers had no signs of osteoarthritis.
Limitations
Some potential limitations of this study must be discussed. Firstly, AP translation was measured from the centre of the femur; therefore it is possible that increased AP translation could be caused by increased lateral rotation in the reconstructed knee with anatomical insert geometry due to the lateral convex surface. However, Arnout et al., who studied the same implant, did not find significant differences between the medial and lateral compartment in AP translation [1].
Secondly, one might argue that it is better to report AP translation in percentages instead of millimetres. We investigated this, and found no correlation between AP laxity and the size of the knee. Besides, comparison with existing literature is more feasible when using millimeters.
Currently, there is no gold standard for in vitro testing in terms of amount of loading. As a result, absolute numbers in terms of translation and laxity are difficult to compare due to different amounts of loading or absence of hamstring loading. Therefore, we present the weightbearing and non-weightbearing results.
The results of the anatomical insert in PCL-retaining TKA in this study are promising in terms of laxity. Furthermore, Heesterbeek et al. found tibiofemoral kinematics close to the native knee with this anatomical insert [6]. Whether this combination translates into superior patient outcome and long-term survival remains to be investigated.
Conclusions
Insert geometry seems to have a limited effect with respect to anterior–posterior translation and varus-valgus laxity in the well-balanced PCL-retaining TKA with an anatomical femoral component. Secondly, anterior–posterior translation and varus-valgus laxity in the reconstructed knee approximate the laxity of the native knee.
References
Arnout N, Victor J, Vermue H, Pringels L, Bellemans J, Verstraete MA (2020) Knee joint laxity is restored in a bi-cruciate retaining TKA-design. Knee Surg Sports Traumatol Arthrosc 28:2863–2871
Banks S, Bellemans J, Nozaki H, Whiteside LA, Harman M, Hodge WA (2003) Knee motions during maximum flexion in fixed and mobile-bearing arthroplasties. Clin Orthop Relat Res 410:131–138
Barnes CL, Blaha JD, DeBoer D, Stemniski P, Obert R, Carroll M (2012) Assessment of a medial pivot total knee arthroplasty design in a cadaveric knee extension test model. J Arthroplasty 27(1460–1468):e1461
Baumann F, Bahadin O, Krutsch W, Zellner J, Nerlich M, Angele P et al (2017) Proprioception after bicruciate-retaining total knee arthroplasty is comparable to unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25:1697–1704
Halewood C, Traynor A, Bellemans J, Victor J, Amis AA (2015) Anteroposterior laxity after bicruciate-retaining total knee arthroplasty is closer to the native knee than ACL-resecting TKA: a biomechanical cadaver study. J Arthroplasty 30:2315–2319
Heesterbeek PJ, Labey L, Wong P, Innocenti B, Wymenga AB (2014) A new spacer-guided, PCL balancing technique for cruciate-retaining total knee replacement. Knee Surg Sports Traumatol Arthrosc 22:650–659
Heyse TJ, Slane J, Peersman G, Dirckx M, van de Vyver A, Dworschak P et al (2017) Kinematics of a bicruciate-retaining total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25:1784–1791
Hunt NC, Ghosh KM, Blain AP, Athwal KK, Rushton SP, Amis AA et al (2014) How does laxity after single radius total knee arthroplasty compare with the native knee? J Orthop Res 32:1208–1213
Hunt NC, Ghosh KM, Blain AP, Rushton SP, Longstaff LM, Deehan DJ (2015) No statistically significant kinematic difference found between a cruciate-retaining and posterior-stabilised triathlon knee arthroplasty: a laboratory study involving eight cadavers examining soft-tissue laxity. Bone Joint J 97-B:642–648
Jones CW, Jacobs H, Shumborski S, Talbot S, Redgment A, Brighton R et al (2020) Sagittal stability and implant design affect patient reported outcomes after total knee arthroplasty. J Arthroplasty 35:747–751
Lo J, Muller O, Dilger T, Wulker N, Wunschel M (2011) Translational and rotational knee joint stability in anterior and posterior cruciate-retaining knee arthroplasty. Knee 18:491–495
Matsumoto K, Ogawa H, Yoshioka H, Akiyama H (2017) Postoperative anteroposterior laxity influences subjective outcome after total knee arthroplasty. J Arthroplasty 32:1845–1849
Mihalko WM, Creek AT, Mary MN, Williams JL, Komatsu DE (2011) Mechanoreceptors found in a posterior cruciate ligament from a well-functioning total knee arthroplasty retrieval. J Arthroplasty 26:504.e9-504.e12
Roth JD, Howell SM, Hull ML (2015) Native knee laxities at 0 degrees, 45 degrees, and 90 degrees of flexion and their relationship to the goal of the gap-balancing alignment method of total knee arthroplasty. J Bone Joint Surg Am 97:1678–1684
Seah RB, Pang HN, Lo NN, Chong HC, Chin PL, Chia SL et al (2012) Evaluation of the relationship between anteroposterior translation of a posterior cruciate ligament-retaining total knee replacement and functional outcome. J Bone Joint Surg Br 94:1362–1365
Seah RB, Yeo SJ, Chin PL, Yew AK, Chong HC, Lo NN (2014) Evaluation of medial-lateral stability and functional outcome following total knee arthroplasty: results of a single hospital joint registry. J Arthroplasty 29:2276–2279
Seon JK, Park SJ, Yoon TR, Lee KB, Moon ES, Song EK (2010) The effect of anteroposterior laxity on the range of movement and knee function following a cruciate-retaining total knee replacement. J Bone Joint Surg Br 92:1090–1095
Victor J, Bellemans J (2006) Physiologic kinematics as a concept for better flexion in TKA. Clin Orthop Relat Res 452:53–58
Victor J, Labey L, Wong P, Innocenti B, Bellemans J (2010) The influence of muscle load on tibiofemoral knee kinematics. J Orthop Res 28:419–428
Victor J, Van Glabbeek F, Vander Sloten J, Parizel PM, Somville J, Bellemans J (2009) An experimental model for kinematic analysis of the knee. J Bone Joint Surg Am 91(Suppl 6):150–163
Wautier D, Thienpont E (2017) Changes in anteroposterior stability and proprioception after different types of knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25:1792–1800
Wymenga AB, Heesterbeek PJ (2017) Preserving the posterior cruciate ligament. Insall Scott Surg Knee 2017:1509–1518
Yoshiya S, Matsui N, Komistek RD, Dennis DA, Mahfouz M, Kurosaka M (2005) In vivo kinematic comparison of posterior cruciate-retaining and posterior stabilized total knee arthroplasties under passive and weight-bearing conditions. J Arthroplasty 20:777–783
Acknowledgements
We thank Ronny De Corte from the European Centre for Knee Research (EKCR) for his help in preparation, implantation and measurements of the specimens. Specimens and materials used in this study were kindly arranged by the European Centre for Knee Research, Smith and Nephew.
Author information
Authors and Affiliations
Contributions
Study conception and design: A.H.v.H., P.J.C.H., L.L., A.B.W. Acquisition of data: P.J.C.H., L.L., A.B.W. Analysis and interpretation of data: A.H.v.H., P.J.C.H, G.H. Drafting of manuscript: A.H.v.H. Critical revision: P.J.C.H., G.H., L.L., A.B.W.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Funding
Specimen and materials used in this study were arranged by the former European Center of Knee Research (owned by Smith & Nephew). Smith & Nephew partially financed this study (payment to institution of author).
Ethical approval
Not applicable.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
van Houten, A.H., Heesterbeek, P.J.C., Hannink, G. et al. Limited effect of anatomical insert geometry on in vitro laxity in balanced anatomic posterior cruciate ligament retaining total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 30, 1273–1281 (2022). https://doi.org/10.1007/s00167-021-06564-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-021-06564-1