Abstract
Purpose
The role of increased femoral antetorsion (femAT) as a contributor to patellofemoral (PF) osteoarthritis (OA) is unknown. The purpose of this study was to investigate whether increased femAT was associated with advanced cartilage degeneration in the lateral PF joint.
Methods
Patients who underwent complete radiographic workup for surgical intervention due to OA in any knee joint compartment were included. Cartilage morphology according to the International Cartilage Repair Society (ICRS) cartilage lesion classification system in the PF joint, femoral and tibial torsion, frontal leg axis, and tibial tuberosity-trochlear groove (TT-TG) distance were assessed. Increased femAT was defined as > 20° according to previous reports.
Results
A total of 144 patients were included. Ninety-seven patients had a femAT of < 20° and 45 of > 20°. A significant odds ratio (OR) was found for lateral retropatellar (OR 3.5; p = 0.02) ICRS grade 3 and 4 cartilage degeneration and increased femAT ≥ 20°. In the medial PF compartment, increased femAT had an inverse effect (OR 0.16; p = 0.01). No significant ORs were found for TT-TG distance, tibial torsion, or leg axis. The lateral retropatellar ICRS grade showed a linear correlation to increased femAT values. In valgus knees, isolated lateral PF OA had an even more pronounced correlation to increased femAT (p = 0.004).
Conclusion
Increased femAT showed higher grades of lateral retropatellar cartilage degeneration, which was even more pronounced in valgus knees.
Level of Evidence
Cohort study: Level III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
With a prevalence of 7–28% [29, 31], anterior knee pain is common in active individuals across the lifespan [14, 32]. Furthermore, patellofemoral (PF) osteoarthritis (OA) is an underrecognized yet important subgroup of knee OA [4]. Isolated PF OA can be found in 13–24% of women and in 11–15% of men older than 55 years [5, 19]. Moreover, in a population-based study, combined osteoarthritis of all knee compartments frequently arose from a sequence in which the PF joint was affected first by degeneration followed by the addition of the tibiofemoral joint [10]. A variety of factors alter the mechanics of the PF joint and increase joint stress. These include genu valgum [2, 26, 27, 36], increased tuberosity tibiae-trochlear groove (TT-TG) distance, and trochlear morphology [19, 27]. Other risk factors are recurrent lateral patella dislocations [33], history of trauma, as well as sex and body mass index (BMI) [3].
Increased femoral torsion (femAT) is assumed to be another risk factor for PF pain and cartilage degeneration because of compensatory internal rotation of the distal femur and thereby excessive pressure on the lateral aspect of the PF compartment [22, 37]. Even more, knee pain risk and severity were reported to be more dramatic with cartilage loss isolated to or inclusive of the lateral PF compartment [39]. Up to this date, however, no study was able to prove the hypothesis that increased femAT might cause degeneration in the PF joint [30]. No study exists which simultaneously investigated torsional malalignment of the lower extremity and cartilage degeneration of the PF joint with contemporary state of the art imaging modalities. However, effective prevention and delay of OA depend on comprehension of the risk factors responsible for development and progression of the disease. Therefore, the purpose of this study was to investigate whether increased femAT was associated with unilaterally accentuated OA in the PF joint. The hypothesis of the study was that higher values of femAT correlate with higher degrees of OA in the lateral, and lower presence of OA in the medial PF compartment.
Materials and methods
This study was approved by the Institutional Review Board and the ethical committee (Zurich Cantonal Ethics Commission, 74 KEK 2020-00809). It was conducted entirely at the authors’ institution.
Study population
Out of the clinic’s comprehensive database, all patients who underwent complete clinical and radiographic (long-leg standing view, lateral and anteroposterior radiograph, axial view of the patella) work-up because of symptomatic OA of the knee (lateral, medial and/or PF) between 2012 and 2019 were recorded. Patients were included when a magnetic resonance imaging (MRI) of the knee and a computed tomography (CT) of the affected lower extremity using a special developed CT protocol scanning the regions of interest (i.e. proximal femur, knee centre with distal femur and proximal tibia, ankle joint centre with distal tibia, distal fibula and talus) were available (Fig. 1). CT scan was performed for preoperative CT-based planning of patient specific instrumented knee replacement. Medical records were reviewed regarding history of knee trauma, patellar dislocation or previous surgery. Patients with a history of patellar fracture or another intra-articular fracture of the knee were excluded (Fig. 1). Further exclusion criteria were: chronic patellar dislocation, malformation (or malunion after a fracture) of the affected lower limb, a history of surgical procedures affecting bony alignment, and knee arthroplasty. Only two patients (1.4%) of this cohort suffered from recurrent patellar dislocation, for which reason this risk factor was excluded for further statistical analysis.
The descriptive statistics of the demographical data of 144 included knees and the main parameters are shown in Table 1.
Radiographic assessment
Parameters of interest were: condition of cartilage in the PF joint, and bony parameters as femoral and tibial torsion, frontal mechanical leg axis, TT-TG distance, and trochlear dysplasia.
Radiographs, CT, and MRI of all included patients were analyzed on a picture archiving and communicating system (PACS) workstation by two independent observers (one senior orthopedic resident and one fellowship-trained musculoskeletal radiologist). In the event of discrepancies concerning the ICRS grade, the case was discussed among the co-authors to reach a consensus. This was necessary in 21% of all knees. The same principle was pursued concerning the grade of trochlear dysplasia. Parameters measured as Interclass Correlation Coefficients (ICCs) were calculated to determine the interobserver and intraobserver reproducibility and are given in the methods section.
All patients were examined on clinical 1.5 Tesla or 3 Tesla MR scanners. All included MRI consisted of fluid sensitive fat suppressed and non-fat suppressed MR sequences in three orthogonal planes, including sagittal and axial cartilage sensitive sequences.
CT slice thickness was 2 mm for the proximal femur, 1 mm for the knee and 2 mm for the ankle joint, with increments of 1 mm, 0.5 mm, and 1 mm, respectively. All examinations were performed on clinical 40-slice or 64-slice CT scanner with image reformations using a bone kernel. CT examinations were performed with patients in supine position, with symmetric pelvis and straightened parallel legs.
Measurement (accuracy per pixel: 0.1 mm and 0.1°) were performed in a standardized technique as described in detail below. Regarding clinical relevance, outcome variables are given by one decimal.
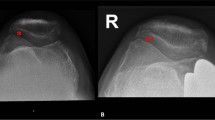
Cartilage of the patellofemoral joint
MRI-based cartilage grading was performed for the medial and lateral patella and at the medial and lateral trochlea facet separately using the International Cartilage Repair Society (ICRS) cartilage lesion classification system, which is currently used as the international standard. It classifies superficial lesions as grade 1, lesions extending down to < 50% of cartilage depth as grade 2, lesions extending down to > 50% as grade 3, and complete loss of cartilage thickness, bone marrow lesions, or intra-articular osteophytes as grade 4 (Fig. 2, left).
Left Cartilage morphology was assessed on axial MR images using the International Cartilage Repair Society (ICRS) classification system. Here, an isolated grade 4 lesion (complete loss of cartilage thickness and bone marrow lesion) of the lateral retropatellar facet is shown. Right CT-based measurement of femoral torsion according to the method described by Murphy [28]. The femoral head center (green circle) is connected with the center of the base of the femoral neck (orange line) directly superior to the lesser trochanter. The distal femoral reference was a line connecting the medial and lateral posterior condyles (blue lines). In this example, femoral antetorsion is 38°
Frontal mechanical axis
Mechanical axis knee alignment was measured on long-leg standing radiographs as the angle between the mechanical femoral and mechanical tibial axis, according to Strecker et al. [40]. Positive values indicate varus alignment and negative values indicate valgus. Inter- and intraobserver repeatability for the measurement of frontal leg axis were both 0.9.
Tibial tuberosity–trochlear groove distance and trochlear dysplasia
Pre- and postoperative TT-TG measurements were performed using the same methodology as described by Schoettle et al. [35]. Dejour’s criteria [6] for trochlear dysplasia on axial MRI scans were used and graded into mild (Dejour type A) and severe (Dejour type B, C and D) dysplasia, according to Lippacher et al. [24].
Femoral torsion
CT-based measurement of femoral torsion was performed according to the method described by Murphy et al. [28], as it most closely reflects true femoral torsion [34]. Compared to other measurement methods, Murphy et al. defined the proximal femoral reference axis at the level just superior to the lesser trochanter [28] (Fig. 2, right). The remaining two landmarks (femoral head center and the posterior distal femoral condyles) are identical to all other methods [34].
Sutter et al. [41] modified the method of Murphy and compared mean values and standard deviation of asymptomatic volunteers to patients with femoroacetabular impingement. FemAT in the control group was 13° ± 10. Based on available data, the cut-off for increased femoral antetorsion was set to 20° [12, 18, 43, 45]. In the present analysis, interrater and intrarater ICC for femoral torsion were both 0.9.
Tibial torsion
Tibial torsion was defined as the angle between a tangential line aligned at the posterior tibial cortex just superior to the fibular tip, and a bimalleolar line drawn through the middle dense surfaces of the malleoli [13]. Test–retest repeatability for the measurement of tibial torsion was 0.9 (intra- and inter-observer reliability).
Statistical analysis
Descriptive analyses of patient characteristics were performed with use of means and standard deviations for continuous variables and with frequencies and percentages for discrete or dichotomous variables. A power analysis (2-Sample Non-Inferiority or Superiority) was performed for the comparison of the means between the femAT groups (< 20°, n = 97 and > 20°, n = 47) to demonstrate a minimum difference of 5° between populations, which was used as cut-off for clinical significance: 1–β = 100%,
A logistic binary model was constructed due to the dichotomous nature of the dependent variables used (advanced osteoarthritis including ICRS Grade 3 and 4 yes/no and increased femAT yes/no) to assess the relationship between two groups of risk factors and the incidence of PF arthritis (retropatellar or trochlear and medial or lateral, respectively). The first group consisted of demographic factors such as: age, gender, BMI and previous trauma. The second group of risk factors included radiographic parameters: leg axis (varus/valgus), grade of trochlear dysplasia, TT-TG distance and tibial torsion. In the multivariate analysis, all of the following were treated as dichotomous variables: previous trauma, gender, femAT (less or more than 20°).
An a priori power analysis for a subsequent hierarchical multiple regression revealed a minimum required sample size of 58 for an anticipated effect size (f2) = 0.15 (medium effect size) and a desired statistical power of 0.8 (total number of predictors: 4). This was done to first match the population based on the following variables: BMI, age, gender and previous trauma. The analysis allowed the inclusion of these covariates in the regression equation for calculation of femAT as risk factors for lateral retropatellar OA. The study sample size achieved this minimal requirement with n = 144.
Furthermore, a linear regression analysis with scatter plots was performed to represent the linear correlation of quantitative changes in femAT with the ICRS grades of OA. Anatomical risk factors for isolated lateral or medial PF arthritis were investigated in a subgroup analysis. Group comparison (isolated lateral PF arthritis vs. isolated medial PF arthritis) was performed with Chi square test, Mann–Whitney U test, or unpaired t test, as appropriate. A binary logistic regression model was used for odds ratio between different parameters. In a further subgroup analysis, only valgus knees were investigated. The Receiver-Operator Characteristic (ROC) curve was used to identify the best cutoff of femAT, which would have predicted an optimal (ICRS 0-2 in the lateral PF joint) or non-optimal (ICRS 3/4 in the lateral PF joint) outcome.
All statistical tests were 2-sided, and p value of < 0.05 was considered statistically significant. All analysis was performed with SPSS (version 23.0; IBM SPSS Statistics).
Results
The binary logistic regression model showed significant OR for lateral retropatellar cartilage degeneration (ICRS grade 3 and 4) and increased femAT greater than 20° (OR 3.5, p = 0.02) (Table 2), and vice versa (Table 3). No significant correlation was found for leg axis, TT-TG distance, trochlear dysplasia, or tibial torsion. After matching the population for demographics in a hierarchical multiple regression analysis, increased femAT emerged as a significant positive predicting risk factor for lateral retropatellar OA (positive coefficient, 0.234; 95% CI 0.014–0.832; p = 0.043). The lateral retropatellar ICRS grade showed a linear correlation to increased femAT values (Fig. 3). On the other hand, increased femAT showed significant lower grades of cartilage degeneration on the medial trochlea (OR, 0.16; 95% CI 0.04–0.64; p = 0.01) (Fig. 3).
The subgroup-analysis revealed a higher mean femAT in patients with isolated lateral PF joint OA (21.7 ± 11°) compared to patients with isolated OA in the medial compartment (8.2 ± 6.5°) (p = 0.02), whereas other anatomical factors showed no correlation.
Considering valgus knees only, the logistic regression analysis showed an even more pronounced correlation between isolated lateral PF OA and increased femAT (p = 0.004). Genu varum showed no correlation to medial or lateral OA (n.s.). In contrast, isolated medial PF OA correlated with lower (or normal) femAT (p < 0.05). Likewise, patients with increased femAT (> 20°) but low grade (ICRS 0-2) lateral and high grade (ICRS 3 and 4) medial PF OA had varus knees (mean 6.3 ± 2°; p < 0.05), underlining varus leg axis as a protective factor for cartilage degeneration in the lateral PF compartment in case of increased femAT (Fig. 4). For valgus knees, the ROC curve analysis provided an ideal cutoff at 18° femAT for lateral PF OA, with a sensitivity of 60.5%, a specificity of 100%, and area under the curve of 82%.
Reference lines represent mean values (femoral antetorsion and frontal axis) of the study population. a No distribution pattern is recognizable between high (red dots) and low grade (blue dots) patellofemoral (PF) osteoarthritis (OA) in terms of femoral antetorsion and frontal leg axis when both medial and lateral retropatellar chondral status is matched. b When comparing isolated lateral versus medial PF OA, an obvious distribution emerges. No cases of isolated lateral OA (red dots) were found in patients with increased femoral antetorsion and varus alignment
Discussion
The most important finding of this study was that increased femAT showed higher grades of lateral retropatellar cartilage degeneration, which was even more pronounced in valgus knees.
Rotational malalignment was recently identified, among other anatomic variables, as a contributor to PF instability [9]. Accordingly, derotational osteotomies have been proven to be a reliable option for correction of torsional pathologies in patellofemoral instability and anterior knee pain [7, 16, 38]. Anterior knee pain is triggered by increased stress loads on the lateral aspect of the PF compartment due to greater internal femoral rotation [21]. Lee et al. studied the impact of femAT on quadriceps tension and PF contact pressure [23]. At twenty degrees of rotational deformity of the femur, only a slight PF contact pressure increase was noted on the contralateral facets of the patella. However, at thirty degrees rotational deformity, contact pressure increased significantly [23]. To investigate whether there was a relationship between femAT and the presence and pattern of OA of the PF joint, Oppermann et al. used seventy-eight human cadaveric lower extremities [30]. The location and degree of PF cartilage degeneration was recorded with a digital processor. In this study population, there was no significant correlation between femAT and cartilage damage of the lateral facet of the PF joint. However, femAT averaged 13.3 ± 7.4°, with only 15 subjects having a femAT over 15° [30]. Eighty-four patients with radiographically diagnosed OA of the knee were classified into three subsets of PF OA, medial femorotibial OA and lateral femorotibial OA in the study of Takai et al. [42]. FemAT in patients with PF OA (22.7°) was significantly greater than in subjects with femorotibial OA (16°) [42]. In accordance with these results, significant ORs were found in the present study for lateral retropatellar OA and increased femAT greater than 20°, and vice versa. Moreover, the lateral retropatellar ICRS grade showed a linear correlation to increased femAT values. On the other hand, lower ICRS grades of the medial trochlea were found when increased femAT was present. A similar conclusion was found in the biomechanical analysis of Liska et al. [25], where external derotation of the distal femur led to a redistribution of retropatellar pressure to the medial patellar facet. Moreover, Kang et al. [22] indicated the different load distribution in the PF joint after increase of femAT in rabbits. Kaiser et al. [20] demonstrated that there was a significant center of force shift towards the lateral side of the PF joint with increased internal femAT. Interestingly, only lateral retropatellar cartilage was affected in our study. Ambra et al. [1] made similar observations and found that patellar cartilage lesions were more closely associated with anatomic risk factors when compared to trochlear lesions. In conclusion, femAT seems to be a contributor in the development of PF OA.
Next to increased femAT, other structural factors contribute to patellofemoral malalignment, such as higher values of tibial external rotation [44]. A significant correlation between femAT and tibial torsion was found in patients with PF disorders [17], with significant differences compared to a control group [11]. Promising results with PF stability and pain relief were shown after torsional osteotomy in cases of tibial maltorsion [8]. In the present study, however, there was no correlation between increased external torsion of the tibia and advanced cartilage damage of the lateral PF compartment. A possible explanation might be, that the mean tibial torsion was 23 ± 9° in our cohort, whereas surgical treatment for excessive tibial torsion was described for patients with a mean value of 47 ± 5.4° (range, 37–66) [8].
Other anatomic abnormalities are reported to have a correlation to cartilage lesions in the PF joint, such as trochlear dysplasia [1], TT-TG distance and genu valgum [2, 26, 27]. Recurrent lateral patella dislocation [33], history of direct blunt trauma, as well as sex and BMI [3] were described risk factors for PF OA. However, with a binary logistic regression model no significant relationship between the above-mentioned risk factors and PF cartilage degeneration was found. First, only two patients had a history of recurrent lateral patella dislocations. This is the reason that this risk factor was excluded from statistical analysis. Nevertheless, both patients had cartilage degeneration ICRS grade 4 equally distributed in the whole PF joint. Second, trochlear dysplasia and patellar instability probably become clinically relevant at a younger age. With the exception of one patient, all subjects with low or high grade trochlear dysplasia showed at least ICRS grade 3 in the lateral PF compartment. Finally, in the current cohort, the missing correlation of the remaining risk factors might be attributed to normal mean values. For example, mean TT-TG was 9.2 ± 4 mm, whereas pathological values are reported to be > 20 mm [15]. Similarly, mean leg axis was 2.4 ± 10° varus. Nevertheless, a relationship between the frontal leg axis and PF joint OA could be shown: Valgus knees revealed a more pronounced correlation between isolated lateral PF OA and increased femAT (p = 0.004), whereas genu varum showed less lateral OA despite increased femAT (Fig. 4).
The present study should be interpreted in light of its potential limitations. To minimize selection bias, clear and comprehensible exclusion criteria were defined (Fig. 1). However, even though patients who have PF OA often demonstrate malalignment, these results do not allow judgment if patients who have malalignment have a greater disposition to OA. Considering the anatomic variability, this needs to be verified by further studies, with a bigger sample size, performed in a prospective manner. Moreover, this study gives no clear indications of which factors contribute the most and should surgically be treated. For example, there was only a small group of patients with trochlear dysplasia. For this reason, the missing of any correlation is most likely false negative. It should therefore be interpreted with caution. Regarding the cut-off for increased femAT used in this study, 20° might be considered as a high-normal value. However, considering the linear correlation between cartilage degeneration and femAT, the conclusion remains the same. Additionally, previous studies defined a femAT of < 20° as normal, and as increased if > 20° [12, 18, 45].
These results are of clinical relevance: First, distal femoral derotation osteotomies in case of pathological femAT have the potential of preventing PF OA in addition to re-stabilization of the patella and reduction of anterior knee pain. Second, owing to the complexity of bony malalignment in PF disorders, every patient should undergo advanced imaging to analyze rotational and frontal plane alignment, since the influence of femAT on the PF compartment is more pronounced in valgus knees.
Conclusion
Patients with increased femAT showed significantly higher grades of lateral retropatellar OA and significantly lower grades of medial trochlear cartilage degeneration. Furthermore, varus axis had a protective effect on lateral PF joint OA in case of increased femAT, whereas an additional valgus axis showed a more pronounced correlation between isolated lateral PF OA and femAT. Therefore, the results highlight the importance of femAT, especially in combination with mechanical valgus axis, which might be underestimated and neglected in diagnostic workups regarding development and progression of PF OA.
References
Ambra LF, Hinckel BB, Arendt EA, Farr J, Gomoll AH (2019) anatomic risk factors for focal cartilage lesions in the patella and trochlea: a case-control study. Am J Sports Med 47:2444–2453
Cahue S, Dunlop D, Hayes K, Song J, Torres L, Sharma L (2004) Varus-valgus alignment in the progression of patellofemoral osteoarthritis. Arthritis Rheum 50:2184–2190
Cicuttini F, Wluka A, Wang Y, Stuckey S (2002) The determinants of change in patella cartilage volume in osteoarthritic knees. J Rheumatol 29:2615–2619
Crossley KM, Hinman RS (2011) The patellofemoral joint: the forgotten joint in knee osteoarthritis. Osteoarthritis Cartilage 19:765–767
Davies AP, Vince AS, Shepstone L, Donell ST, Glasgow MM (2002) The radiologic prevalence of patellofemoral osteoarthritis. Clin Orthop Relat Res 402:206–212
Dejour D, Saggin P (2010) The sulcus deepening trochleoplasty-the Lyon’s procedure. Int Orthop 34:311–316
Dickschas J, Harrer J, Pfefferkorn R, Strecker W (2012) Operative treatment of patellofemoral maltracking with torsional osteotomy. Arch Orthop Trauma Surg 132:289–298
Dickschas J, Tassika A, Lutter C, Harrer J, Strecker W (2017) Torsional osteotomies of the tibia in patellofemoral dysbalance. Arch Orthop Trauma Surg 137:179–185
Diederichs G, Kohlitz T, Kornaropoulos E, Heller MO, Vollnberg B, Scheffler S (2013) Magnetic resonance imaging analysis of rotational alignment in patients with patellar dislocations. Am J Sports Med 41:51–57
Duncan R, Peat G, Thomas E, Hay EM, Croft P (2011) Incidence, progression and sequence of development of radiographic knee osteoarthritis in a symptomatic population. Ann Rheum Dis 70:1944–1948
Erkocak OF, Altan E, Altintas M, Turkmen F, Aydin BK, Bayar A (2016) Lower extremity rotational deformities and patellofemoral alignment parameters in patients with anterior knee pain. Knee Surg Sports Traumatol Arthrosc 24:3011–3020
Fabricant PD, Fields KG, Taylor SA, Magennis E, Bedi A, Kelly BT (2015) The effect of femoral and acetabular version on clinical outcomes after arthroscopic femoroacetabular impingement surgery. J Bone Joint Surg Am 97:537–543
Goutallier D, Van Driessche S, Manicom O, Sariali E, Bernageau J, Radier C (2006) Influence of lower-limb torsion on long-term outcomes of tibial valgus osteotomy for medial compartment knee osteoarthritis. J Bone Joint Surg Am 88:2439–2447
Hall R, Barber Foss K, Hewett TE, Myer GD (2015) Sport specialization’s association with an increased risk of developing anterior knee pain in adolescent female athletes. J Sport Rehabil 24:31–35
Hochreiter B, Hirschmann MT, Amsler F, Behrend H (2019) Highly variable tibial tubercle-trochlear groove distance (TT-TG) in osteoarthritic knees should be considered when performing TKA. Knee Surg Sports Traumatol Arthrosc 27:1403–1409
Imhoff FB, Cotic M, Liska F, Dyrna FGE, Beitzel K, Imhoff AB et al (2019) Derotational osteotomy at the distal femur is effective to treat patients with patellar instability. Knee Surg Sports Traumatol Arthrosc 27:652–658
Imhoff FB, Funke V, Muench LN, Sauter A, Englmaier M, Woertler K et al (2019) The complexity of bony malalignment in patellofemoral disorders: femoral and tibial torsion, trochlear dysplasia, TT-TG distance, and frontal mechanical axis correlate with each other. Knee Surg Sports Traumatol Arthrosc 28:897–904
Ito K, Minka MA 2nd, Leunig M, Werlen S, Ganz R (2001) Femoroacetabular impingement and the cam-effect. A MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br 83:171–176
Iwano T, Kurosawa H, Tokuyama H, Hoshikawa Y (1990) Roentgenographic and clinical findings of patellofemoral osteoarthrosis. With special reference to its relationship to femorotibial osteoarthrosis and etiologic factors. Clin Orthop Relat Res 252:190–197
Kaiser P, Loth F, Attal R, Kummann M, Schuster P, Riechelmann F et al (2020) Static patella tilt and axial engagement in knee extension are mainly influenced by knee torsion, the tibial tubercle-trochlear groove distance (TTTG), and trochlear dysplasia but not by femoral or tibial torsion. Knee Surg Sports Traumatol Arthrosc 28:952–959
Kalichman L, Zhu Y, Zhang Y, Niu J, Gale D, Felson DT et al (2007) The association between patella alignment and knee pain and function: an MRI study in persons with symptomatic knee osteoarthritis. Osteoarthritis Cartilage 15:1235–1240
Kang H, Lu J, Li F, Dai Y, Dong Z, Dong C et al (2020) The effect of increased femoral anteversion on the morphological and trabecular microarchitectural changes in the trochlea in an immature rabbit. J Adv Res 23:143–149
Lee TQ, Anzel SH, Bennett KA, Pang D, Kim WC (1994) The influence of fixed rotational deformities of the femur on the patellofemoral contact pressures in human cadaver knees. Clin Orthop Relat Res 302:69–74
Lippacher S, Dejour D, Elsharkawi M, Dornacher D, Ring C, Dreyhaupt J et al (2012) Observer agreement on the Dejour trochlear dysplasia classification: a comparison of true lateral radiographs and axial magnetic resonance images. Am J Sports Med 40:837–843
Liska F, von Deimling C, Otto A, Willinger L, Kellner R, Imhoff AB et al (2019) Distal femoral torsional osteotomy increases the contact pressure of the medial patellofemoral joint in biomechanical analysis. Knee Surg Sports Traumatol Arthrosc 27:2328–2333
Macri EM, Felson DT, Ziegler ML, Cooke TDV, Guermazi A, Roemer FW et al (2019) The association of frontal plane alignment to MRI-defined worsening of patellofemoral osteoarthritis: the MOST study. Osteoarthritis Cartilage 27:459–467
Macri EM, Stefanik JJ, Khan KK, Crossley KM (2016) Is tibiofemoral or patellofemoral alignment or trochlear morphology associated with patellofemoral osteoarthritis? a systematic review. Arthritis Care Res 68:1453–1470
Murphy SB, Simon SR, Kijewski PK, Wilkinson RH, Griscom NT (1987) Femoral anteversion. J Bone Joint Surg Am 69:1169–1176
Myer GD, Ford KR, Di Stasi SL, Foss KD, Micheli LJ, Hewett TE (2015) High knee abduction moments are common risk factors for patellofemoral pain (PFP) and anterior cruciate ligament (ACL) injury in girls: is PFP itself a predictor for subsequent ACL injury? Br J Sports Med 49:118–122
Oppermann J, Bredow J, Wissussek B, Spies CK, Boese CK, Chang SM et al (2017) Does increased femoral antetorsion predispose to cartilage lesions of the patellofemoral joint? Knee Surg Sports Traumatol Arthrosc 25:2695–2701
Rathleff MS, Roos EM, Olesen JL, Rasmussen S (2015) Exercise during school hours when added to patient education improves outcome for 2 years in adolescent patellofemoral pain: a cluster randomised trial. Br J Sports Med 49:406–412
Rathleff MS, Skuldbol SK, Rasch MN, Roos EM, Rasmussen S, Olesen JL (2013) Care-seeking behaviour of adolescents with knee pain: a population-based study among 504 adolescents. BMC Musculoskelet Disord 14:225
Sanders TL, Pareek A, Johnson NR, Stuart MJ, Dahm DL, Krych AJ (2017) Patellofemoral Arthritis After Lateral Patellar Dislocation: a Matched Population-Based Analysis. Am J Sports Med 45:1012–1017
Schmaranzer F, Lerch TD, Siebenrock KA, Tannast M, Steppacher SD (2019) Differences in Femoral Torsion Among Various Measurement Methods Increase in Hips With Excessive Femoral Torsion. Clin Orthop Relat Res 477:1073–1083
Schoettle PB, Zanetti M, Seifert B, Pfirrmann CW, Fucentese SF, Romero J (2006) The tibial tuberosity-trochlear groove distance; a comparative study between CT and MRI scanning. Knee 13:26–31
Sharma L, Song J, Felson DT, Cahue S, Shamiyeh E, Dunlop DD (2001) The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA 286:188–195
Souza RB, Draper CE, Fredericson M, Powers CM (2010) Femur rotation and patellofemoral joint kinematics: a weight-bearing magnetic resonance imaging analysis. J Orthop Sports Phys Ther 40:277–285
Stambough JB, Davis L, Szymanski DA, Smith JC, Schoenecker PL, Gordon JE (2018) Knee pain and activity outcomes after femoral derotation osteotomy for excessive femoral anteversion. J Pediatr Orthop 38:503–509
Stefanik JJ, Gross KD, Guermazi A, Felson DT, Roemer FW, Zhang Y et al (2015) The relation of MRI-detected structural damage in the medial and lateral patellofemoral joint to knee pain: the Multicenter and Framingham Osteoarthritis Studies. Osteoarthritis Cartilage 23:565–570
Strecker W (2006) Planning analysis of knee-adjacent deformities. I. Frontal plane deformities. Oper Orthop Traumatol 18:259–272
Sutter R, Dietrich TJ, Zingg PO, Pfirrmann CW (2012) Femoral antetorsion: comparing asymptomatic volunteers and patients with femoroacetabular impingement. Radiology 263:475–483
Takai S, Sakakida K, Yamashita F, Suzu F, Izuta F (1985) Rotational alignment of the lower limb in osteoarthritis of the knee. Int Orthop 9:209–215
Toogood PA, Skalak A, Cooperman DR (2009) Proximal femoral anatomy in the normal human population. Clin Orthop Relat Res 467:876–885
Turner MS (1994) The association between tibial torsion and knee joint pathology. Clin Orthop Relat Res 302:47–51
Wells J, Nepple JJ, Crook K, Ross JR, Bedi A, Schoenecker P et al (2017) Femoral morphology in the dysplastic hip: three-dimensional characterizations with CT. Clin Orthop Relat Res 475:1045–1054
Authors’ contributions
FA and IFB researched literature and conceived the study. FA, IFB and FSF were involved in protocol development and gaining ethical approval. FA and HA were involved in patient recruitment. Radiological assessment was performed by FA, HA and IFB. IFB, FA and OA were involved in data analysis. FA wrote the first draft of the manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical approval
Ethical approval for this study was obtained from Zurich Cantonal Ethics Comission: KEK 2020-00809.
Informed consent
Written informed consent was obtained from all subjects before the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Flury, A., Hoch, A., Andronic, O. et al. Increased femoral antetorsion correlates with higher degrees of lateral retropatellar cartilage degeneration, further accentuated in genu valgum. Knee Surg Sports Traumatol Arthrosc 29, 1760–1768 (2021). https://doi.org/10.1007/s00167-020-06223-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06223-x