Abstract
Purpose
Recent registry data have demonstrated a higher revision rate of quadriceps tendon (QT) graft compared with hamstring tendon (HT) and patellar tendon (PT) grafts. Clinic routines could be an important factor for revision outcomes. The purpose of this study is to use the Danish Knee Ligament Reconstruction Registry (DKRR) to compare revision rates in patients who have undergone ACLR with QT, HT and PT grafts related to individual clinic surgical routine.
Methods
Data on primary ACLRs entered in the DKRR from 2012 through 2019 were analysed since QT graft usage started in 2012. Revision rates for QT, HT and PT grafts were compared according to clinic activity (0–100 and > 100 procedures). Revision rates for the three autograft cohorts are presented, as well as adjusted revision hazard rates. Instrumented knee stability and pivot-shift tests were performed at a one-year follow-up.
Result
QT revision rate (6.4%) for low-activity clinics was higher than for high-activity clinics (2.9%) (p = 0.003). The adjusted revision hazard ratio for low-activity clinics was 2.3 (p = 0.01). QT autograft was associated with statistically significant, increased side-to-side laxity at follow-up (1.4 mm) compared with HT and PT autografts (1.0 mm) (p < 0.01), as well as an increased positive pivot-shift rate.
Conclusion
QT autografts for ACLR were associated with higher revision rates in clinics with lower than 100 procedures performed from 2012 to 2019. QT graft usage is not associated with a high revision rate when routinely performed. Learning curve is an important factor when introducing QT ACLR.
Level of evidence
Level III
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Quadriceps tendon (QT) graft has recently gained increased interest for anterior cruciate ligament reconstruction (ACLR) due to the introduction of minimally invasive harvesting techniques and low donor site morbidity. Recent Danish registry data have demonstrated a higher revision rate of 4.7% for QT graft compared with hamstring tendon (HT) and patellar tendon (PT) grafts from 2005 to 2017, when looking at all 531 QT grafts for ACLR procedures [14]. The study investigated the potential impacts of age, type of sport and the learning curve, the last one by excluding the first one-third of the patients undergoing the operation. QT grafts for young patients and patients performing contact sports, as well as those performed after the learning curve correction still demonstrated higher revision rates than those of HT and PT grafts. These results have surprised the scientific community of sports traumatology as initial case and randomised clinical trials (RCT) studies have not demonstrated high revision rates. The use of QT graft preserves the HT function, which is believed to be important for postoperative protection of ACL grafts. Some of the criticisms against the study are that with the long recruitment period of 12 years, surgical techniques have changed, and early procedures were performed at a time of limited technical experience. Before the Danish registry study, the literature on QT grafts for ACLR was limited by small study sizes, which prevented valid reporting of revisions and failure rates and outcomes from a generalised surgical population [1, 2, 8, 10, 23]. Two randomised controlled trials demonstrated that ACLRs performed with QT autografts reduced donor site morbidity and demonstrated equivalent clinical outcome scores compared with both PT and HT grafts at 2 years of follow-up and that revision rates were low (0–2%) [13, 15]. Furthermore, a large retrospective study involving 191 patients reported no difference in clinical outcomes and failure rates between PT and QT autografts in the intermediate term [5]. An early systematic review did not report the revision rates due to limited data [18, 25]. A recent review presented a revision rate of 2.1% by pooling data from 21 studies and 1554 QT ACLRs [17]. However, the pooling of data in a meta-analysis is subjected to bias. To provide a better presentation of QT ACLR revision outcomes, a study should focus on a more recent time period when QT graft usage and surgical techniques have become more predictable. The data should also be derived from a general surgical population, as done in a multicentre national registry.
A potential important factor for the initial finding of a high revision rate for QT grafts in Denmark could be the procedural routine of individual departments/clinics that affected the revision outcome. It is, therefore, important to investigate the influence of department routines on the revision outcome for QT ACLR.
In the Danish Knee Ligament Reconstruction Registry (DKRR), over 1000 QT ACLRs and over 25,000 PT and HT ACLRs from 2005 to 2019 enable the comparison of revision rates and objective clinical outcomes for these graft types [12].
The purpose of the present study is to use the DKRR to compare revision rates in patients who have undergone ACLR with QT, HT, and PT as graft for ACLR related to individual clinic surgical activities. It was hypothesised that low clinic volume of the new QT grafts would result in higher revision rates compared to high-volume clinics.
Materials and methods
The study is based on the DKRR, a prospective, nationwide and web-based clinical database initiated in 2005. The registry contains data on primary and revision anterior and posterior cruciate ligament reconstructions, as well as collateral ligament and multiligament reconstructions performed in Denmark. Both public and private hospitals supply data to this registry [11]. The operating surgeon records preoperative, operative and one-year follow-up data, using a standardised form via a secure Internet portal. Furthermore, patients independently report their subjective knee function using self-assessed instruments—the Knee injury Osteoarthritis Outcome Score (KOOS) and the Tegner Activity Scale Score [22, 26]. The surgeon or the physician’s assistant records objective instrumented Lachman laxity and pivot-shift test results at a one-year follow-up. The patients enter their KOOS and Tegner Activity Scale data on a web-based form before the surgery and 1 year after the surgery. No written consent is necessary in Denmark for studies based on data from the National Board of Health-approved national healthcare registries. However, the study was approved by the Regional Centre for Clinical Quality Development and the National Data Protection Agency (Approval number 1-16-02-65-17).
Patients
In Denmark, QT graft usage has increased since 2012 from 2 to 11% in 2019. Therefore, this study limited the patient data to patients who underwent the operations from 2012 to 2019. The inclusion criteria were primary ACLRs with QT, HT or PT autograft. In total, 12,559 reconstructions were eligible for inclusion. The exclusion criteria were previous ligament procedure (1224 excluded), age below 16 years (1196 excluded), previous contralateral ACL injury (75 excluded), other graft types (376 excluded) and any previous meniscus or cartilage surgery on the affected knee (3365 excluded). Three study populations were identified based on the graft choice for ACLR: patients with QT autografts (n = 1194), patients with HT autografts (n = 10,547) and patients with PT autografts (n = 818).
The completeness of the surgical registration was determined by correlating the registry data with the data in the national registry of patients in which all public and private hospital contacts and procedures are registered. The overall completeness of ACL procedure registration in the ACL registry was 91% for the study data [19].
The completeness of the one-year follow-up using objective knee stability assessment was 53%. The completeness of the patient-reported outcome data was 34% preoperatively and 25% at the one-year follow-up. A validation study from the DKRR demonstrated no difference in epidemiologic characteristics, clinical outcomes and revision rates between responders and non-responders [19]. Due to low completeness, the data from KOOS and Tegner Activity Scale scores are not included in the present paper.
Patient characteristics
The patients’ average age was 27.2 years (range: 16–68 years), and 62% of the patients were males. Sports participation was the cause of injury in 86.5% of the cases occurred while performing sports. There were differences among the three graft groups, with QT graft patients having moderately lower ages, as well as the presence of meniscus and cartilage injuries at the time of surgery (Table 1).
Outcomes
The primary outcome was ACLR failure, expressed as the need for ACLR revision. This need was decided by individual surgeons and informed consent based on continued instability or reinjury.
The secondary outcome was objective knee stability in terms of instrumented sagittal knee stability testing and pivot-shift scores. The sagittal stability test measured the difference in sagittal stability between the operated knee and the healthy knee using the Knee Translation 1000 instrument (KT-1000) or the Rolimeter. The pivot-shift test is a dynamic but passive test of the knee that measures the rotational and anterior tibial translation stability of the ACL. The pivot-shift test is graded on a 4-point scale, where 0 = negative, 1 = glide, 2 = clunk and 3 = gross [9]. The pivot-shift data were divided into negative and positive pivot-shift tests.
Statistical analyses
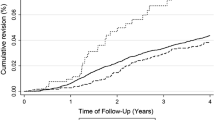
To investigate the impact of department routine. Departments were divided into low-activity clinics (0–100 procedures) and high-activity clinics (> 100 procedures). The descriptive data are presented as means and standard deviations and compared with the Student’s-t test or the Chi-square test for proportional data. The Cox regression analysis was used to compare the revision risk within the first 2 years after primary ACL surgery among patients in the three graft groups. By applying the Kaplan–Meier method, the revision probability was estimated for the three graft groups for the total follow-up period. Hazard ratios were computed as measures of relative risk (RR), both crudely and adjusted for potentially confounding factors. The included confounding factors were gender, age (≤ 20 and > 20 years), cartilage damage > 1 cm2 (no/yes or missing data) and surgical treatment of meniscal injury, either resection or repair (yes/no or missing data). The confounding factors were chosen based on the known factors influencing the ACLR outcome. P values < 0.05 were considered statistically significant. For sample size calculation an expected 3% difference in revision rates between low-and high-activity clinics was used. With a power of 0.8, this required 749 cases per graft group. All statistical analyses were computed using Stata Version 16 (Stata Release 12, College Station, TX).
Results
Revision rates
Overall revision rates for QT, HT and PT grafts were 4.2, 2.2 and 3.7%, respectively, with no difference in adjusted hazard rates (Fig. 1). The QT revision rate for low-activity clinics (0–100 procedures) was 6.4%, which was significantly higher than the 2.9% rate for high-activity clinics (> 100 procedures) (p = 0.003). The adjusted revision hazard ratio for low-activity clinics was 2.3 (p = 0.01) (Fig. 2). The distribution of revision rates between the clinics demonstrated a large variation; clinics with < 100 procedures had revision rates ranging from 0 to 14%, whereas clinics with > 100 procedures had revision rates lower than 2.0%, ranging from 1.2% to 1.9% (Fig. 3).
Plot of revision rates for quadriceps tendon graft usage in relation to clinic surgical experience. It shows that clinics with > 100 procedures (Circle A) all have good revision rates below 2% and clinics with 0–100 procedures (Circle B) have more varying and higher revision rates, contributing to a national average of 4.0%
The HT revision rates for low-activity and high-activity clinics were 1.9% and 2.3%, respectively (ns). The PT revision rates for low-activity and high-activity clinics were 3.2% and 2.2%, respectively (ns).
Objective knee laxity
The knee laxity, as determined by the side-to-side difference with a knee arthrometer, was significantly decreased by ACLR surgery in all three graft groups. At the one-year follow-up, QT autograft was associated with more objective knee laxity than HT and PT autografts, producing 1.4 mm, 1.0 mm and 1.0 mm of postoperative laxity, respectively (QT versus HT, p < 0.01; QT versus PT, p < 0.01) (Table 2).
A positive postoperative pivot-shift test was found in the QT autograft (25%), the HT (17%) and the PT (16%) cohorts, with QT grafts having significantly more positive pivot shift than HT and PT grafts (p < 0.01), whereas no difference was observed between PT and HT graft groups (Table 2).
Discussion
The most important finding of the present study was that the high-volume clinics obtained similar revision outcomes for QT, HT and PT grafts. These data are in contrast with a recent DKKR study that found a high revision rate for QT grafts compared with HT and PT grafts [14]. These results suggest that failures after QT grafts ACLR are affected by the routine of the clinics where the surgeries are performed. In the above-mentioned first QT graft study based on a large registry, there was an attempt to correct for the learning curve impact by removing the first one-third of QT procedures in each clinic. However, after this correction, the QT graft still had significantly higher revision rates than those of HT and PT grafts. Several previous studies reported a learning curve when harvesting the QT graft and when using the harvesting systems available on the market [4, 24]. A mix of techniques exists, varying from 5-mm thickness (known as partial thickness) to 8-mm graft thickness (known as full thickness) and 10-mm to 12-mm QT graft width. A potential reason why the present study found no difference among the graft groups in high-volume clinics could be that the included patient data came from a more recent period (2012–2019), whereas the first DKKR study covered a longer period (2005–2017). Surgical techniques and graft fixation principles can have changed more over the long period compared with the present study’s more recent period [3]. Moreover, the patient sample of 1194 in the present study was twice as high as that of the first DKRR study. This reduced the risk of selection bias. The demographic comparison data of the three graft cohorts indicated that QT graft patients were slightly younger (by 1.5–1.9 years) and had a slight predominance of males (4%) than HT and PT graft cohorts. Both of these factors posed a known higher risk of graft failure. However, the hazard rate data presented were corrected for both age and gender differences, so selection bias was not expected to be a problem for the revision rate results.
The present study’s findings on QT grafts resulting in revision rates ranging from 1.2 to 1.9% in high-volume clinics are similar to some previous studies’ reported results. In a RCT, Lund et al. compared 30 ACLRs with bone plug QT grafts to 30 PT grafts. They found no failures in the QT group at 24 months [15]. In another randomised study, Lind et al. found a 2% revision rate (1/50 patients) [13]. Geib et al. compared in 191 patients ACL reconstructions with QT grafts, both with and without bone plug, to PT grafts. They reported 11 (5.7%) failures in the QT group and only 1 in the PT group [5]. Runer et al. compared in 80 patients’ QT grafts with a bone plug to HT grafts. They reported no differences in failures between graft types after 24 months of follow-up [23]. Finally, Gorschewsky et al. compared QT grafts with a bone plug compared to PT grafts in 194 patients with a minimum follow-up of 2 years and reported a failure rate of 2.2% after 24 months in the QT group compared to 4.9% in the PT group [7]. The study also found that PT grafts had similar revision rates as those of HT grafts. This is in conflict with several studies based on national registries that consistently demonstrate lower revision rates for PT than HT grafts [6, 16, 20]. Two potential explanations for this could be that PT grafts have been decreasingly used during the existence of the ACL registry and that anatomical reconstruction techniques have been predominant in the most recent period. Since anatomical techniques have been shown to be associated with higher revision rates [21], a higher revision rate is expected when investigating the PT grafts performed in a more recent period.
The present study observed a significant higher postoperative, objective Lachman laxity of 0.4 mm and 7–9% more positive pivot shift when using QT autografts compared with HT and PT grafts. The randomised studies that have compared QT grafts with HT and PT grafts have found similar objective stability values between the graft types [13, 15]. A study by Lee et al. also reported no difference in positive pivot-shift test results and KT-2000 stability values [10]. Although statistically significant due to the high number of patients, the 0.4-mm difference in sagittal laxity and the slightly higher percentage of positive pivot shift are not considered clinically relevant.
The hypothesis that QT ACLRs performed in low-volume clinics would result in higher failure rates was confirmed. This result suggests that the previous findings on higher revision rates for QT grafts recorded in the DKRR were due to a learning curve issue, where the lack of surgical routine caused higher revision rates in some clinics. The present study’s findings also suggest that QT graft for ACLR can result in revision rates similar to those of HT and PT grafts when performed routinely. This calls for QT graft usage in ACLR since this graft type in several level-1 studies has also been shown to have the least donor site morbidity [13, 15].
The most important strength of this study is the large sample size of all three investigated graft groups, which is important for an accurate evaluation of the rare failure parameter of revision reoperation, which for ACLR has an incidence typically below 5% 2 years after the procedure [12]. Another strength is the inclusion of patients from several centres nationwide, with a high level of completeness (> 90%). This type of registry data provides more generalisable results since it represents a generalised surgical population. Registry data have high external validity due to the prospective data collection, the high volume from multiple centres and surgeons and the absence of any a priori data collection purpose, which could bias the data collection.
This study has its limitations as well. Selection bias is an important issue for registry data, especially for new techniques such as QT graft usage, as the motivation for using the new graft type is not recorded in the registry. The evaluations of knee stability outcomes with instrumented knee laxity measurements and pivot-shift tests are performed by the operating surgeons in the majority of the clinics. This can cause a bias towards better stability measurements, which should be taken into account when evaluating the objective outcomes. Revision surgery has been used as the endpoint of failure, but this parameter does not include the group of patients who have subjective or objective graft failures but have not undergone revision surgery.
The clinical relevance of the present study is that introduction of QT graft for ACLR can result in increased failure rate and that surgeons and clinics starting with QT graft ACL should have strong focus on potential pitfalls such as graft thickness during harvest and proper fixation method. When performed routinely QT ACLR results in as low failure rate as patella tendon graft. QT ACLR furthermore have documented lower donor morbidity than patellar tendon graft.
Conclusions
QT autografts for ACLR are associated with higher revision rates in clinics with lower than 100 procedures performed from 2012 to 2019. The learning curve and surgical routines in Denmark appear to account for the previously demonstrated high revision rates of QT grafts for ACLR compared with HT and PT grafts. QT graft usage is not associated with high revision rates when routinely performed.
References
Cavaignac E, Coulin B, Tscholl P, Fatmy NMN, Duthon V, Menetrey J (2017) Is Quadriceps tendon autograft a better choice than hamstring autograft for anterior cruciate ligament reconstruction? A comparative study with a mean follow-up of 3.6 years. Am J Sports Med 45(6):1326–1332
DeAngelis JP, Fulkerson JP (2007) Quadriceps tendon–a reliable alternative for reconstruction of the anterior cruciate ligament. Clin Sports Med 26(4):587–596
Eysturoy NH, Nissen KA, Nielsen T, Lind M (2018) The influence of graft fixation methods on revision rates after primary anterior cruciate ligament reconstruction. Am J Sports Med 46(3):524–530
Fink C, Herbort M, Abermann E, Hoser C (2014) Minimally invasive harvest of a quadriceps tendon graft with or without a bone block. Arthroscopy Techniques 3(4):e509–513
Geib TM, Shelton WR, Phelps RA, Clark L (2009) Anterior cruciate ligament reconstruction using quadriceps tendon autograft: intermediate-term outcome. Arthroscopy 25(12):1408–1414
Gifstad T, Foss OA, Engebretsen L, Lind M, Forssblad M, Albrektsen G, Drogset JO (2014) Lower risk of revision with patellar tendon autografts compared with hamstring autografts: a registry study based on 45,998 primary ACL reconstructions in Scandinavia. Am J Sports Med 42(10):2319–2328
Gorschewsky O, Klakow A, Putz A, Mahn H, Neumann W (2007) Clinical comparison of the autologous quadriceps tendon (BQT) and the autologous patella tendon (BPTB) for the reconstruction of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 15(11):1284–1292
Han HS, Seong SC, Lee S, Lee MC (2008) Anterior cruciate ligament reconstruction: quadriceps versus patellar autograft. Clin Orthop Relat Res 466(1):198–204
Jakob RP, Staubli HU, Deland JT (1987) Grading the pivot shift. Objective tests with implications for treatment. J Bone Joint Surg Br 69(2):294–299
Lee JK, Lee S, Lee MC (2016) Outcomes of anatomic anterior cruciate ligament reconstruction: bone-quadriceps tendon graft versus double-bundle hamstring tendon graft. Am J Sports Med 44(9):2323–2329
Lind M, Menhert F, Pedersen AB (2009) The first results from the Danish ACL reconstruction registry: epidemiologic and 2 year follow-up results from 5,818 knee ligament reconstructions. Knee Surg Sports Traumatol Arthrosc 17(2):117–124
Lind M, Menhert F, Pedersen AB (2012) Incidence and outcome after revision anterior cruciate ligament reconstruction: results from the Danish registry for knee ligament reconstructions. Am J Sports Med 40(7):1551–1557
Lind M, Nielsen TG, Soerensen OG, Mygind-Klavsen B, Fauno P (2020) Quadriceps tendon grafts does not cause patients to have inferior subjective outcome after anterior cruciate ligament (ACL) reconstruction than do hamstring grafts: a 2-year prospective randomised controlled trial. Br J Sports Med 54(3):183–187
Lind M, Strauss MJ, Nielsen T, Engebretsen L (2020) Quadriceps tendon autograft for anterior cruciate ligament reconstruction is associated with high revision rates: results from the Danish Knee Ligament Registry. Knee Surg Sports Traumatol Arthrosc 28(7):2163–2169
Lund B, Nielsen T, Fauno P, Christiansen SE, Lind M (2014) Is quadriceps tendon a better graft choice than patellar tendon? A prospective randomized study. Arthroscopy 30(5):593–598
Maletis GB, Inacio MC, Funahashi TT (2015) Risk factors associated with revision and contralateral anterior cruciate ligament reconstructions in the Kaiser Permanente ACLR registry. Am J Sports Med 43(3):641–647
Mouarbes D, Menetrey J, Marot V, Courtot L, Berard E, Cavaignac E (2019) Anterior cruciate ligament reconstruction: a systematic review and meta-analysis of outcomes for quadriceps tendon autograft versus bone-patellar tendon-bone and hamstring-tendon autografts. Am J Sports Med 47(14):3531–3540
Mulford JS, Hutchinson SE, Hang JR (2013) Outcomes for primary anterior cruciate reconstruction with the quadriceps autograft: a systematic review. Knee Surg Sports Traumatol Arthrosc 21(8):1882–1888
Rahr-Wagner L, Thillemann TM, Lind MC, Pedersen AB (2013) Validation of 14,500 operated knees registered in the Danish Knee Ligament Reconstruction Register: registration completeness and validity of key variables. Clin Epidemiol 5:219–228
Rahr-Wagner L, Thillemann TM, Pedersen AB, Lind M (2014) Comparison of hamstring tendon and patellar tendon grafts in anterior cruciate ligament reconstruction in a nationwide population-based cohort study: results from the danish registry of knee ligament reconstruction. Am J Sports Med 42(2):278–284
Rahr-Wagner L, Thillemann TM, Pedersen AB, Lind MC (2013) Increased risk of revision after anteromedial compared with transtibial drilling of the femoral tunnel during primary anterior cruciate ligament reconstruction: results from the Danish Knee Ligament Reconstruction Register. Arthroscopy 29(1):98–105
Roos EM, Toksvig-Larsen S (2003) Knee injury and Osteoarthritis Outcome Score (KOOS)—validation and comparison to the WOMAC in total knee replacement. Health Qual Life Outcomes 1:17
Runer A, Wierer G, Herbst E, Hepperger C, Herbort M, Gfoller P, Hoser C, Fink C (2018) There is no difference between quadriceps- and hamstring tendon autografts in primary anterior cruciate ligament reconstruction: a 2-year patient-reported outcome study. Knee Surg Sports Traumatol Arthrosc 26(2):605–614
Slone HS, Ashford WB, Xerogeanes JW (2016) Minimally invasive quadriceps tendon harvest and graft preparation for all-inside anterior cruciate ligament reconstruction. Arthroscopy Techniques 5(5):e1049–e1056
Slone HS, Romine SE, Premkumar A, Xerogeanes JW (2015) Quadriceps tendon autograft for anterior cruciate ligament reconstruction: a comprehensive review of current literature and systematic review of clinical results. Arthroscopy 31(3):541–554
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
Funding
The study was funded internally by the Dept of Orthopedics at Aarhus University Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors state no conflict of interest.
Ethical approval
No written consent is necessary in Denmark for studies based on data from the National Board of Health-approved national healthcare registries. However, the study was approved by the Regional Centre for Clinical Quality Development and the National Data Protection Agency (Approval number 1-16-02-65-17).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lind, M., Strauss, M.J., Nielsen, T. et al. Low surgical routine increases revision rates after quadriceps tendon autograft for anterior cruciate ligament reconstruction: results from the Danish Knee Ligament Reconstruction Registry. Knee Surg Sports Traumatol Arthrosc 29, 1880–1886 (2021). https://doi.org/10.1007/s00167-020-06220-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06220-0