Abstract
Purpose
To investigate the stabilizing effect of a lateral meniscus posterior root repair in an ACL and root deficient knee.
Methods
The hypothesis of the current study was that a sequential transection of the posterior root and the meniscofemoral ligaments in an ACL-deficient knee increases rotational instability, and conversely, a repair of the meniscus root reduces the internal tibial rotation. Therefore, eight human knee joints were tested in a robotic setup (5 N m internal torque, 50 N m anterior translation load). Five conditions were tested: intact, ACL cut, ACL cut + lateral meniscus posterior root tear (LMRT), ACL cut + LMRT + transection of the MFL and ACL cut + lateral meniscus root repair. The angles of internal tibial rotation as well as anterior tibial translation were recorded.
Results
Transection of the lateral meniscus posterior root increased the internal tibial instability as compared to the ACL-insufficient state. A significant increase was detected in 60° and 90° of flextion. Sectioning of the meniscofemoral ligament further destabilized the knees significantly at all flexion angles as compared to the ACL-deficient state. Even in 30°, 60° and 90° a significant difference was detected as compared to the isolated root tear. A tibial fixation of the lateral meniscus root reduced the internal tibial rotation in all flexion angles and led to a significant decrease of internal tibial rotation in 30° and 90° as compared to the transection of the root and the MFL. The anterior tibial translation was increased in all conditions as compared to the native state.
Conclusion
A lateral meniscus root repair can reduce internal tibial rotation in the ACL-deficient knee. To check the condition of the lateral posterior meniscus root attachment is clinical relevant as a lateral meniscus root repair might improve rotational stability.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lateral meniscal posterior root tears are common concomitant injuries in case of a rupture of the anterior cruciate ligament (ACL). The reported incidence of these tears adds up from 14 to 15% [7, 13, 25].
The consequences of these tears are strongly influenced by the integrity of the meniscofemoral ligaments [11, 15].
The intact meniscofemoral ligaments stabilize the meniscal ring and diminish the negative effect of a posterior meniscus root tear in the lateral compartment. A significant increase in the intraarticular pressure due to a rupture of the complete ring can only be expected in case of a complete posterior detachment with an additional rupture of the meniscofemoral ligaments [11, 15, 21]. Thus, lateral meniscus root tears might have a better prognosis in case of an intact meniscofemoral attachment than root tears with a complete rupture of the root and the meniscofemoral ligaments [11, 21].
Unfortunately, untreaded or overseen isolated lateral meniscus root tears left in situ at the time of an ACL reconstruction lead to slight joint space narrowing over time and promoted an early onset of an osteoarthristis [31].
To overcome this, a fixation of the meniscus is useful to restore the intraarticular pressure distribution and therefore should be performed additionally to the ACL reconstruction [12]. The positive effect of a transtibial repair of the lateral meniscus posterior horn to restore the intraarticular pressure in case of a complete lateral meniscus posterior root tear (root tear and rupture of the MFL) was pointed out by several studies [11, 15, 21].
Biomechanical studies prove that a loss or rupture of the meniscus tissue leads to an increased laxity in the ACL-deficient knee [1, 27, 28, 32].
Today, the role of the meniscofemoral ligaments as a secondary stabilizer against the posterior drawer is well known [3, 16], but their contribution to rotational stability in case of a root tear and an ACL rupture was investigated by two studies only [14, 32]. Furthermore, only one of these biomechanical studies distinguished between an isolated root tear of the lateral meniscus and a transection of the meniscofemoral ligaments [14]. Also clinical data demonstrate an expectable increase of anterolateral rotational instability in case of an ACL rupture and an additional lateral meniscus root tear [26].
Despite many recommendations to perform a root repair in case of a root tear [5, 12, 14, 17, 26], a study proving that rotational instabilitiy can be reduced by a root repair, is still missing. The hypothesis of the current study is that a sequential transection of the posterior root and the meniscofemoral ligaments in an ACL-deficient knee increases rotational instability, and conversely, a repair of the meniscus root reduces the internal tibial rotation. A repair of the meniscus root is clinically relevant in the ACL injured and root deficient knee.
Therefore, a biomechanical robotic setup was established to investigate the stabilizing effect of lateral meniscus root tears with and without disruption of the meniscofemoral ligaments in a human ACL-deficient knee. In addition to that, the study examined the effect of a root reconstruction/refixation on stability restoration against internal tibial rotation of the root injured knee.
Methods
Eight human cadaveric knees were used in this study. The knee joints were obtained from MedCure, Orlando, USA (median age 62 years, range 54–70). Exclusion criteria were previous known ligament/ meniscal trauma, ligament /meniscus surgery and severe osteoarthritis. The specimens were thawed at room temperature for 24 h in advance.
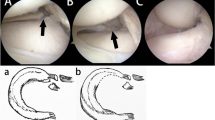
Prior to biomechanical testing all specimens were examined by MRI to confirm intact ligament and meniscus structures as well as evidence of at least one meniscofemoral ligament (Fig. 1) (MFL; anterior or posterior meniscofemoral ligament) The status of the cartilage, the meniscus and ligaments and the specimens age and sex are given in Table 1.
The femur and the tibia were dissected from soft tissue and muscles at least 15 cm proximal and distal to the joint line. The specimens were embedded with a polyurethane system (RenCast® FC isocyanate/FC 52 polyol) in a custom-made carrier.
The femur of the specimens was mounted to the robotic system Stäubli RX 90 B (Stäubli, Germany, Bayreuth). The acting loads were measured by a JR3 90M40A3 force torque sensor (JR3 Inc. USA, Woodland). The tibia was rigidly connected to the base of the setup fully extended. By neutralizing hyperextension to neutral (0° of extension) the flexion angles (0°; 30°; 60°; 90°) and the loading coordinate system were determined. To eliminate the influence of the femur mass and the potting device and to measure the acting forces on the level of the joint line, half of every specimen’s weight was subtracted from the force measurements. All forces perpendicular to the tibia axis and the torques within the sagittal plane were neutralized. The axial force during all testing conditions was set to 20 N compression. Then a torque of ± 5 N m around the tibial axis was applied for internal rotation. The angle of internal rotation was measured at 5 N m of applied torque with a tolerance of ± 0.1 N m. The rotation was determined with direct kinematics. The accuracy was 0.5 mm and 0.001°.
In addition to that, the anterior tibial translation at 20° of flexion was measured for all conditions. A force of 50 N was applied to translate the femur in a posterior direction to measure the distance of tibial translation against the femur.
Prior to testing a posterolateral approach was created in all specimens. First, the popliteus muscle was visualized. Then the posterior lateral capsule was incised and the anterior and the posterior cruciate ligament, the lateral meniscus and the meniscofemoral ligaments were identified (Fig. 2a, b).
Posterolateral approach to a right knee. a The capsule is dissected above the popliteus muscle, the lateral meniscus and the meniscofemoral ligaments are intact. b The lateral meniscus posterior horn is detached from the tibia and the meniscofemoral ligaments are detached. A suture (2#fiber wire, Arthrex, Naples, USA) was led through the lateral meniscus posterior horn for tibial fixation
Five different conditions were tested as follows:
-
1.
Intact structures (intact)
-
2.
ACL cut (ACL cut)
-
3.
ACL cut and lateral meniscus posterior root tear (ACL cut + LMRT)
-
4.
ACL cut and lateral meniscus posterior root tear and transection of the meniscofemoral ligament (ACL cut + LMRT + MFL)
-
5.
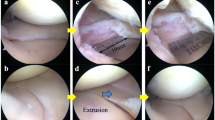
ACL cut and lateral meniscus posterior root tear and transection of the meniscofemoral ligament (MFL) and transtibial fixation of the lateral posterior meniscus root. (ACL cut + LMRR) (Fig. 3).
The fixation of the lateral meniscus posterior horn was reattached to its anatomical origin using a modified Mason-Allen stitch in the lateral meniscus posterior horn (2# fiber wire, Arthrex, USA, Naples). The suture was passed through a tibial tunnel (diameter 2 mm) (ACL cut + LMRR) in the center of the anatomical origin of the posterior lateral meniscus root insertion [18, 19]. Then the suture was fixed to the anteromedial cortex of the proximal tibia and tensioned close to extension using a button plate (DepuySynthes, USA, Warsaw).
An IRB approval was not obtained in this study. All specimens were obtained from med Cure, Orlando, USA for biomechanical testing. The use and disposal of the specimen was in accordance to med Cure guidelines.
Statistical analysis
Statistical analysis was performed using MATLAB R2016 a (MathWorks, Natick, USA). Continuous variables were expressed as means and standard deviation. The results were expressed in bar diagrams. To test for significant changes first a two-way ANOVA was performed. Then a Fisher’s least significant difference procedure was used to compare the different conditions against each other. The level of significance was set at a p value of 0.05.
A post hoc power analysis was performed using G*Power 3.1.9.2 (Franz Paul, Kiel, Germany) to determine the power of the results. An effect size of 0.66 and an alpha value of 0.05 in a cohort of 8 specimens led to a power of 0.85 at 30° of flexion. At 60° (effect size 0.93) 0.99 and at 90° (effect 1.54) 1.00. The results at 0° were underpowered with an effect size of 0.19 and a power of 0.12.
Results
The findings of this study are expressed below in tables and bar diagrams. The results are presented as means (± SD). For better traceability the bar diagrams show the intact subtracted angles only. In contrast to that, the results of the simulated Lachman test demonstrate the distances in mm as compared to the intact condition.
Internal tibial rotation (5 N m torque)
Cutting the lateral meniscus posterior root led to a slight increase of internal rotation in all flexion angles as compared to the intact and ACL-insufficient state. The additional transection of the MFL increased the internal tibial rotation significantly as compared to the ACL-insufficient state in all flexion angles. Even in 30° (p = 0.001), 60° (p = 0.001) and 90° (p = 0.001) the internal rotational instability significantly increased as compared to the lateral meniscus root tear alone. A root repair, addressing the lateral posterior root alone without a fixation of the MFL reduced the internal rotational instability in all conditions and resulted in a significant decrease of internal rotational instability as compared to the additional MFL transection in 30° (p = 0.002), 60° (p = 0.017) and 90° (p = 0.000) of flexion Tables 2, 3; Fig. 4.
Anterior tibial translation at 20° of flexion (20 N axial load; 50 N anterior load)
The anterior tibial translation increased by sequential transection of all structures. The increase was significant as compared to the intact state for all conditions (ACL cut; p = 0.004; ACL cut + LMRT; p = 0.001; ACL cut + LMRT + MFL; p = 0.001). Comparing the different conditions (ACL cut; ACL cut + LMRT; ACL cut + LMRT + MFL) the instability progressed but the differences were not significant. The lateral meniscal root repair reduces the anterior translation without significant changes as compared to the cutting conditions of the root, the MFL and the ACL (Table 4; Fig. 5).
Discussion
The most important finding of this study was the stabilizing effect of a transosseous lateral meniscus root repair on internal tibial rotation in the ACL and root deficient knee. A root repair restored the function of the meniscus ring and reduced the internal tibial rotation. This root repair was efficient although the meniscofemoral ligaments were left transected. Especially in 30° and 90° of flexion the single root repair led to a significant restoration of the tibial internal rotation as compared to the complete meniscus detachment (ACL cut + LMRT + MFL).
The function of the meniscofemoral ligaments as contributors to posterior stability is well known [3, 4, 16, 24] and the stabilizing effects of the meniscofemoral ligaments and the posterior lateral meniscus root on internal rotation in the ACL-insufficient knee were proven by Frank et al. [14] recently. They demonstrated a significant increase of tibial internal rotation in case of a complete transection of the meniscofemoral ligaments and the cut of the meniscus posterior root. The results of the current study confirm these findings. A sequential transection of these structures resulted in an increase of the internal rotational instability.
Regarding the anterior tibial translation, the results of the current study reveal the increase of antero-posterior instability due to a root injury and a MFL transection. However, the increase of antero-posterior translation was not significant when comparing the different transection modes with each other.
Taken together, a repair of the meniscus root in case of a detachment and an ACL tear seems to be reasonable to restore the stability of the injured knee (Table 4).
The possible stabilizing effect of a root repair of the lateral meniscus posterior horn was not investigated yet. Therefore, a fixation was performed using a typical transosseous fixation technique. A variety of fixation techniques have been described already [2, 6, 12, 17, 22, 23]. Until recently the impact of meniscus root tears was mainly discussed regarding the pressure distribution in the knee and their potential contribution to the onset of an osteoarthritis [9, 29,30,31]. Therefore, root repairs of the medial and lateral meniscus are performed to restore the intraarticular pressure distribution. In case of an isolated posterior root tear of the lateral meniscus and an intact meniscofemoral ligament a significant increase of the intraarticular pressure cannot be expected [11, 15]. A significant increase can be expected in case of a type 3 lesion (complete detachment of the root and the meniscofemoral ligament) [11, 13, 20] only. However, the destabilizing effect of a lateral meniscectomy on the ACL-deficient knee was described by Musahl et al. [28]. They found an increase of anterior tibial translation of the ACL-deficient knee in case of a lateral meniscectomy in a biomechanical study simulating a pivot shift maneuver.
The current study shows a destabilizing effect of a transection of the lateral meniscus posterior attachments on the ACL-deficient knee. These findings highlight the importance to check the integrity of the posterior meniscus attachments in case of an ACL reconstruction.
The fixation of the lateral meniscus posterior root led to a significant decrease of the rotational instability as compared to the complete detachment of the meniscus posterior horn and the meniscofemoral ligament by readapting the meniscus ring to the tibia alone without reconstruction of the meniscofemoral attachment.
The results of this recent biomechanical study prove the value and the efficacy of a root repair of the lateral meniscus in the ACL-deficient knee to reduce the tibial rotational instability.
The studies of Frank et al. and Shybut et al. [14, 32] as well as clinical data by Minami et al. [26] suggest that a repair of the lateral meniscus posterior horn is recommended to restore the meniscus ring to reduce the tibial internal rotation of the ACL and root injured knee.
Some limitations apply to this study. The robot study did not simulate possible stabilizing effects of muscle and surrounding soft tissue activation, although this study provided data supporting a stabilizing effect of lateral meniscus root repair, without taking other structures into consideration. Studies have shown that a root repair itself is a weak construct that does not resist close to native forces as compared to the intact meniscus [6, 8, 10, 22]. Therefore, the presented data serve as a time zero study without investigating survivability and healing of the repair. Further, the created defects were artificial and may not reflect all facets of possible meniscus injuries. Lastly, the fixation of the meniscus was performed under ideal circumstances, which may be more challenging in a clinical situation. However, in this setup the construct was robust enough to resist the forces and torques applied in this study (50 N, 5 N m). But load to failure testing reveals a potential risk of slippage and failure of the construct [6, 10, 22].
In summary, the study supports the positive stabilizing effect of the meniscus root attached to the tibia in case of a complete artificial detachment in the ACL-deficient knee.
Therefore a repair of the lateral meniscus posterior root seems to be clinically relevant in case of a typical combination of an ACL tear and an additional root tear. Leaving these tears untreated in situ might reduce postoperative knee stability after isolated ACL reconstruction.
Conclusion
Lateral meniscus root tears and an additional tear of the meniscofemoral ligaments contribute to an increase of instability of the ACL-deficient knee. A repair of the lateral meniscus posterior root can reduce the amount of internal rotational instability. When performing an ACL reconstruction these lateral meniscus root tears should not be left untreated. The surgeon should aim to restore the tibial attachment of the meniscus posterior root.
References
Ahn JH, Bae TS, Kang KS, Kang SY, Lee SH (2011) Longitudinal tear of the medial meniscus posterior horn in the anterior cruciate ligament-deficient knee significantly influences anterior stability. Am J Sports Med 39(10):2187–2193
Ahn JH, Lee YS, Yoo JC, Chang MJ, Park SJ, Pae YR (2010) Results of arthroscopic all-inside repair for lateral meniscus root tear in patients undergoing concomitant anterior cruciate ligament reconstruction. Arthroscopy 26(1):67–75
Amadi HO, Gupte CM, Lie DT, McDermott ID, Amis AA, Bull AM (2008) A biomechanical study of the meniscofemoral ligaments and their contribution to contact pressure reduction in the knee. Knee Surg Sports Traumatol Arthrosc 16(11):1004–1008
Amis AA, Bull AM, Gupte CM, Hijazi I, Race A, Robinson JR (2003) Biomechanics of the PCL and related structures: posterolateral, posteromedial and meniscofemoral ligaments. Knee Surg Sports Traumatol Arthrosc 11(5):271–281
Bhatia S, LaPrade CM, Ellman MB, LaPrade RF (2014) Meniscal root tears: significance, diagnosis, and treatment. Am J Sports Med 42(12):3016–3030
Cerminara AJ, LaPrade CM, Smith SD, Ellman MB, Wijdicks CA, LaPrade RF (2014) Biomechanical evaluation of a transtibial pull-out meniscal root repair: challenging the bungee effect. Am J Sports Med 42(12):2988–2995
Feucht MJ, Bigdon S, Mehl J, Bode G, Muller-Lantzsch C, Sudkamp NP, Niemeyer P (2014) Risk factors for posterior lateral meniscus root tears in anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc 23(1):140–145
Feucht MJ, Grande E, Brunhuber J, Rosenstiel N, Burgkart R, Imhoff AB, Braun S (2014) Biomechanical comparison between suture anchor and transtibial pull-out repair for posterior medial meniscus root tears. Am J Sports Med 42(1):187–193
Feucht MJ, Kuhle J, Bode G, Mehl J, Schmal H, Sudkamp NP, Niemeyer P (2015) Arthroscopic transtibial pullout repair for posterior medial meniscus root tears: a systematic review of clinical, radiographic, and second-look arthroscopic results. Arthroscopy 31(9):1808–1816
Forkel P, Foehr P, Meyer JC, Herbst E, Petersen W, Brucker PU, Burgkart R, Imhoff AB (2016) Biomechanical and viscoelastic properties of different posterior meniscal root fixation techniques. Knee Surg Sports Traumatol Arthrosc 25(2):403–410
Forkel P, Herbort M, Sprenker F, Metzlaff S, Raschke M, Petersen W (2014) The biomechanical effect of a lateral meniscus posterior root tear with and without damage to the meniscofemoral ligament: efficacy of different repair techniques. Arthroscopy 30(7):833–40
Forkel P, Petersen W (2012) Posterior root tear fixation of the lateral meniscus combined with arthroscopic ACL double-bundle reconstruction: technical note of a transosseous fixation using the tibial PL tunnel. Arch Orthop Trauma Surg 132(3):387–391
Forkel P, Reuter S, Sprenker F, Achtnich A, Herbst E, Imhoff A, Petersen W (2015) Different patterns of lateral meniscus root tears in ACL injuries: application of a differentiated classification system. Knee Surg Sports Traumatol Arthrosc 23(1):112–118
Frank JM, Moatshe G, Brady AW, Dornan GJ, Coggins A, Muckenhirn KJ, Slette EL, Mikula JD, LaPrade RF (2017) Lateral meniscus posterior root and meniscofemoral ligaments as stabilizing structures in the ACL-deficient knee: a biomechanical study. Orthop J Sports Med 5(6):2325967117695756
Geeslin AG, Civitarese D, Turnbull TL, Dornan GJ, Fuso FA, LaPrade RF (2016) Influence of lateral meniscal posterior root avulsions and the meniscofemoral ligaments on tibiofemoral contact mechanics. Knee Surg Sports Traumatol Arthrosc 24(5):1469–1477
Gupte CM, Smith A, McDermott ID, Bull AM, Thomas RD, Amis AA (2002) Meniscofemoral ligaments revisited. Anatomical study, age correlation and clinical implications. J Bone Joint Surg Br 84(6):846–851
Harnden E, Lin T, Wilson A, Reid JB 3rd (2017) Technique for transtibial knotless repair of lateral meniscus root avulsion. Arthrosc Tech 6(3):e845-e851
Johannsen AM, Civitarese DM, Padalecki JR, Goldsmith MT, Wijdicks CA, LaPrade RF (2012) Qualitative and quantitative anatomic analysis of the posterior root attachments of the medial and lateral menisci. Am J Sports Med 40(10):2342–2347
Johnson DL, Swenson TM, Livesay GA, Aizawa H, Fu FH, Harner CD (1995) Insertion-site anatomy of the human menisci: gross, arthroscopic, and topographical anatomy as a basis for meniscal transplantation. Arthroscopy 11(4):386–394
LaPrade CM, James EW, Cram TR, Feagin JA, Engebretsen L, LaPrade RF (2015) Meniscal root tears: a classification system based on tear morphology. Am J Sports Med 43(2):363–369
LaPrade CM, Jansson KS, Dornan G, Smith SD, Wijdicks CA, LaPrade RF (2014) Altered tibiofemoral contact mechanics due to lateral meniscus posterior horn root avulsions and radial tears can be restored with in situ pull-out suture repairs. J Bone Joint Surg Am 96(6):471–479
LaPrade RF, LaPrade CM, Ellman MB, Turnbull TL, Cerminara AJ, Wijdicks CA (2015) Cyclic displacement after meniscal root repair fixation: a human biomechanical evaluation. Am J Sports Med 43(4):892–898
LaPrade RF, LaPrade CM, James EW (2015) Recent advances in posterior meniscal root repair techniques. J Am Acad Orthop Surg 23(2):71–76
Lertwanich P, Martins CA, Kato Y, Ingham SJ, Kramer S, Linde-Rosen M, Smolinski P, Fu FH (2010) Contribution of the meniscofemoral ligament as a restraint to the posterior tibial translation in a porcine knee. Knee Surg Sports Traumatol Arthrosc 18(9):1277–1281
Matheny LM, Ockuly AC, Steadman JR, LaPrade RF (2015) Posterior meniscus root tears: associated pathologies to assist as diagnostic tools. Knee Surg Sports Traumatol Arthrosc 23(10):3127–3131
Minami T, Muneta T, Sekiya I, Watanabe T, Mochizuki T, Horie M, Katagiri H, Otabe K, Ohara T, Katakura M, Koga H (2017) Lateral meniscus posterior root tear contributes to anterolateral rotational instability and meniscus extrusion in anterior cruciate ligament-injured patients. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-017-4569-8
Musahl V, Bedi A, Citak M, O’Loughlin P, Choi D, Pearle AD (2011) Effect of single-bundle and double-bundle anterior cruciate ligament reconstructions on pivot-shift kinematics in anterior cruciate ligament- and meniscus-deficient knees. Am J Sports Med 39(2):289–295
Musahl V, Citak M, O’Loughlin PF, Choi D, Bedi A, Pearle AD (2010) The effect of medial versus lateral meniscectomy on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med 38(8):1591–1597
Petersen W, Forkel P, Feucht MJ, Zantop T, Imhoff AB, Brucker PU (2014) Posterior root tear of the medial and lateral meniscus. Arch Orthop Trauma Surg 134(2):237–255
Schillhammer CK, Werner FW, Scuderi MG, Cannizzaro JP (2012) Repair of lateral meniscus posterior horn detachment lesions: a biomechanical evaluation. Am J Sports Med 40(11):2604–2609
Shelbourne KD, Roberson TA, Gray T (2011) Long-term evaluation of posterior lateral meniscus root tears left in situ at the time of anterior cruciate ligament reconstruction. Am J Sports Med 39(7):1439–1443
Shybut TB, Vega CE, Haddad J, Alexander JW, Gold JE, Noble PC, Lowe WR (2015) Effect of lateral meniscal root tear on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med 43(4):905–911
Funding
The study received funding by Deutsche Arthrosehilfe e.V.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors describe the following conflicts of interest with this study: Philipp Forkel: none. Constantin von Deimling: none. Lucca Lacheta: none. Florian B. Imhoff: none. Peter Foehr: none. Lukas Willinger: none. Wolf Petersen: aap, Karl Storz, Otto Bock. Andreas B. Imhoff: Arthrex, Arthrosurface. Rainer Burgkart: none.
Ethical Approval
An IRB approval was not obtained in this study. All specimen were obtained from medCure for biomechanical testing only. The use and disposal of all specimen was in accordance to medCure guidelines.
Rights and permissions
About this article
Cite this article
Forkel, P., von Deimling, C., Lacheta, L. et al. Repair of the lateral posterior meniscal root improves stability in an ACL-deficient knee. Knee Surg Sports Traumatol Arthrosc 26, 2302–2309 (2018). https://doi.org/10.1007/s00167-018-4949-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-4949-8