Abstract
Background
Recent evidence that smaller hamstring graft diameter is associated with increased failure risk following anterior cruciate ligament (ACL) reconstruction has increased the popularity of graft configurations that increase graft diameter at the expense of graft length. A key question is how much graft needs to be in contact with the femoral tunnel to ensure that healing occurs. We hypothesize that no difference in two-year patient-reported outcomes or failure risk exists based on the amount of graft in the femoral tunnel.
Methods
Through the use of prospectively collected cohort data augmented with retrospective chart review, 120 of 181 consecutive patients (66.3 %) undergoing primary ACL reconstruction with hamstring autograft were evaluated. Patient and surgical factors along with pre-operative and two-year postoperative knee injury and osteoarthritis outcome score (KOOS) and International Knee Documentation Committee (IKDC) scores and whether each patient underwent revision ACL reconstruction during the two-year follow-up period were recorded.
Results
No differences in two-year patient-reported outcome scores were noted between patients with graft length in the femoral tunnel less than 25 mm and those with graft length in the femoral tunnel of at least 25 mm. Controlling for age, sex, BMI, and femoral tunnel technique, no correlation was noted between KOOS or IKDC scores and either the length of graft in the femoral tunnel or the contact area between the graft and the tunnel.
Conclusions
Variation of the length of hamstring autograft in the femoral tunnel between 14 and 35 mm does not predict KOOS or IKDC scores at 2 years postoperative.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hamstring autografts are frequently utilized for anterior cruciate ligament (ACL) reconstruction. A critical component of ACL reconstruction using soft tissue grafts is graft incorporation with the surrounding bone tunnel. This process occurs over several months and involves maturation and reorganization of collagen fibers that attach the graft to bone as well as remodeling of the trabecular bone architecture [1–3].
A variety of femoral fixation devices currently are available, but suspensory fixation with a cortical button remains the most commonly used method. Recent evidence that smaller graft diameter is associated with increased graft failure risk [4, 5] has increased the popularity of graft configurations that increase graft diameter at the expense of graft length [6]. With limited graft length, a key question is how much graft needs to be in contact with the femoral tunnel to ensure that healing occurs.
Previous animal studies have examined this question, with some demonstrating decreased pullout strength with smaller amounts of graft in the tunnel [7, 8], while others demonstrate no correlation between pullout strength and the amount of graft in the tunnel [9, 10]. We are aware of no human clinical studies evaluating this question.
We hypothesize that no difference in two-year patient-reported outcomes or revision risk exists between patients in whom 25 mm or more of graft is in the tunnel and those in whom less than 25 mm of graft is in the femoral tunnel. We further hypothesize that there is no correlation between the two-year patient-reported outcome scores and the length of graft in the tunnel or surface contact area between the graft and the tunnel.
Methods
Patient population and data collection
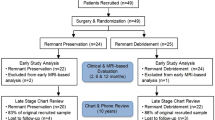
Through the use of prospective data collected as part of the Multicenter Orthopaedic Outcomes Network (MOON) cohort study, 181 consecutive patients undergoing primary ACL reconstruction with hamstring autograft and suspensory femoral fixation between the years of 2007 and 2009 were identified at two academic centers. The database provides demographic information (patient age, sex, and body mass index [BMI]), intra-operative findings (meniscus and cartilage status), surgical technique, and patient-reported outcome scores (knee injury and osteoarthritis outcome score [KOOS] [11] and International Knee Documentation Committee [IKDC] subjective score [12]) pre-operatively and at two-year follow-up. The database also contains information regarding whether patients underwent repeat ipsilateral knee surgery, including revision ACL reconstruction. These data were supplemented by a retrospective chart review to determine the hamstring autograft size and length of graft in the femoral tunnel. All data collection activities have been approved by our institutional review board.
Surgical technique
Procedures were performed by a total of three fellowship-trained sports medicine surgeons at two different institutions. The hamstrings were harvested by standard techniques and four-strand grafts were used in all cases (either doubled semitendinosus and gracilis or quadrupled semitendinosus). ACL reconstruction was performed with either an all-endoscopic- or arthroscopic-assisted technique. Both medial portal and trans-tibial drilling methods were used to create the femoral tunnel. The femoral tunnel was consistently drilled to be the same diameter as the prepared graft. Femoral fixation was achieved with a cortical button in all cases. Tibial fixation depended on surgeon preference and included interference screw fixation, suture tied over a post or button, or a combination of the two. A standard accelerated ACL rehabilitation protocol was used for all patients. No postoperative braces were utilized, and immediate weightbearing was allowed. Patients were allowed to return to sports at 6 months postoperatively.
Statistics
Summary statistics including mean and standard deviations were calculated for continuous variables. The length of graft in the femoral tunnel was then dichotomized at 25 mm and patient-reported outcome scores and revision risk were compared between the two groups. Baseline characteristics of the two groups were compared with t tests (for continuous variables) and Fisher’s exact test (for categorical variables). Adjusted means were reported for two-year postoperative patient-reported outcome scores (adjusted for age, sex, BMI, femoral tunnel drilling technique, and pre-operative patient-reported outcome score). A power analysis based on previously reported two-year patient-reported outcomes of ACL reconstruction [13] indicated that 36 patients were required in each group to detect a clinically significant difference (11.5 points) [14, 15] in subjective IKDC score between the groups with 80 % power with α set at 0.05. The relatively small number of events (revision operations) in the series precluded modeling of the revision data by logistic regression analysis.
The relationship between the length of graft in the femoral tunnel (as a continuous variable) and patient-reported outcome scores at 2 years postoperative was determined by multiple linear regression analysis controlling for age, sex, BMI, femoral tunnel drilling technique, and pre-operative patient-reported outcome score. This analysis was repeated to evaluate the relationship between graft surface area in contact with the femoral tunnel and patient-reported outcome measures. The graft surface area in contact with the tunnel was calculated as a function of graft diameter and graft length in the femoral tunnel. Using the rule of thumb that 15 subjects are required for each predictor [16], at least 90 subjects were required for the multiple linear regression model utilized in this study that contained six predictors. All statistical analyses were performed using Stata, version 12.1 (StataCorp, College Station, TX, USA).
Results
The length of graft in the femoral tunnel was available for 120 of the 181 patients eligible for inclusion (66.3 %). The 120 patients included 73 males and 47 females and ranged in age from 13 to 58 years (mean 25.2 ± 9.4 years). The mean length of graft in the femoral tunnel was 23.7 ± 3.8 mm (range 14 to 35 mm).
There were 61 patients with at least 25 mm of graft in the tunnel and 59 patients with less than 25 mm in the tunnel. The less than 25 mm group contained a significantly higher proportion of patients in whom the femoral tunnel was drilled via a medial portal technique (p < 0.001). There were no significant differences in patient demographics or pre-operative patient-reported outcome scores between the two groups (Table 1). After adjusting for age, sex, BMI, femoral tunnel drilling technique, and pre-operative patient-reported outcome score, no differences in two-year patient-reported outcome scores were noted between patients with graft length in the femoral tunnel less than 25 mm and those with graft length in the femoral tunnel of at least 25 mm (Table 2).
Graft length in the tunnel and contact area between the graft and the tunnel were then evaluated as continuous variables. After controlling for age, sex, BMI, femoral tunnel drilling technique, and pre-operative patient-reported outcome score, no correlation was noted between patient-reported outcome scores at 2 years and either the length of graft in the femoral tunnel (Table 3) or the contact area between the graft and the tunnel (Table 4).
Seven patients (5.8 %) underwent repeat ipsilateral knee surgery in the two-year follow-up period, including two patients (1.6 %) who underwent revision ACL reconstruction. The patients in whom revision reconstruction was performed included one 18-year-old patient with 15 mm of an 8 mm diameter graft in the tunnel and one 21-year-old patient with 22 mm of a 7.5 mm diameter graft in the tunnel. Both grafts were noted at the time of revision surgery to have failed in their mid-substance without tunnel pullout.
Discussion
The most important finding in this study was that variation of the length of hamstring autograft in the femoral tunnel between 14 and 35 mm did not predict patient-reported outcome scores at 2 years postoperative. This finding is quite relevant, as medial portal drilling (which is being used more frequently) generally results in shorter tunnels and new all-inside fixation techniques with quadrupled semitendinosus grafts frequently results in relatively small amount of graft in the femoral tunnel. Larger numbers are required to determine whether graft length in the femoral tunnel affects risk of revision surgery.
While this study represents the first study in humans that assesses the influence of graft length in the femoral tunnel on outcomes following primary ACL reconstruction with hamstring autograft, several authors have addressed similar questions in animal models. Zantop et al examined the influence of graft length in the femoral tunnel in 36 goats [10]. The authors randomized 18 of the animals to have 15 mm of graft length in the femoral tunnel while the other 18 had 25 mm of graft in the femoral tunnel. They found that at 6 weeks, ACL reconstructions with 15 mm of graft in the femoral tunnel actually had less anterior tibial translation than those with 25 mm, but this difference became nonsignificant at 12 weeks.
In a similar study in a canine model, Greis et al. evaluated the pullout strength of extensor digitorum longus tendon from an extra-articular metaphyseal bone tunnel [7]. At 6 weeks, the group with 1 cm of tendon within the tunnel was shown to have only 60 % of the pullout strength as the group with 2 cm of tendon in the tunnel. More recently, Qi et al. performed ACL reconstructions with Achilles tendon autograft in 40 adult dogs [8]. There were four groups of dogs, each having progressively more graft length within the tibial tunnel (group I = 5 mm, group II = 10 mm, group III = 15 mm, and group IV = 20 mm). Biomechanical testing at 6 weeks revealed that mean graft pullout strength improved from group I to group IV, but there was no statistically significant difference between groups III and IV. At 12 weeks, more tibial-sided pullout was found in group I than the other groups. The authors concluded that tendon-bone healing in ACL reconstruction at an early stage will be delayed if graft length is less than 15 mm. Finally, Yamazaki et al. performed ACL reconstructions in 24 adult beagle dogs using autogenous flexor tendon grafts [9]. Twelve of the dogs had 5 mm of graft length in the tibial tunnel (group I), while 12 had 15 mm in the tibial tunnel (group II). There was no statistically significant difference between the two groups in ultimate failure load and linear stiffness of the graft-tibia complex harvested at 6 weeks. The authors thus concluded that increasing tendon length in a bone tunnel does not necessarily improve its biomechanical strength.
The animal studies outlined above demonstrate no clear minimum amount of tendon that is required to be present in a tunnel to ensure healing. Similarly, no clear minimum amount of graft required for healing in humans has been defined. The animal data most applicable to this clinical study are those from Zantop et al. as they study femoral tunnel [10]. The other work cited above utilized tibial tunnel assessments [7–9]. Differences in bone density and vascular supply of the distal femur and proximal tibia may limit the applicability of tibial data to the femur. For this reason, 25 mm of graft in the tunnel was chosen as the point to dichotomize the data, facilitating comparison of the results of the current study to their finding that decreasing tunnel length to less than 25 mm did not influence results. The results of the current study suggest that as little at 15 mm can be used without adverse consequences; however, the data do not allow for assessments of shorter lengths that are created with certain new fixation techniques.
There are several limitations of the current study. The first is that only 120 of 181 (66.3 %) consecutive patients undergoing primary ACL reconstruction were evaluated due to inconsistent documentation of the length of graft in the tunnel. A related limitation is that the study required a review of the operative reports to determine the length of graft in the femoral tunnel. Frequently, the amount of graft in the femoral tunnel had to be calculated based on the total tunnel length and length of the suspensory fixation device used. Therefore, if the measurement of the total tunnel length was inaccurate, the graft length in the tunnel calculation would also be inaccurate. Third, the current study focuses only on the influence of the femoral tunnel rather than the tibial tunnel. The operative reports generally did not comment of the amount of graft in the tibial tunnel; however, the techniques utilized by each surgeon resulted in at least 25 mm of graft in the tunnel in all cases. Further limitations of the study include the relatively low numbers that preclude an accurate assessment of the influence of graft length in the tunnel of graft failure risk, which is perhaps the most pressing question related to the issue of graft length in the tunnel. Further, due to the retrospective nature of the study, data regarding other factors such as how tightly the graft fits into the tunnel are unavailable. Such factors may be critical to tendon-bone healing as demonstrated by Greiss et al. in their canine model [7]. We also lack data regarding associated meniscal and cartilage injuries that may influence patient-reported outcome scores between the two groups. Finally, objective evaluation of knee laxity (such as KT-1000 data) is not available for these patients. Such data may give further insight into differences between the two groups. Prospective comparative studies with larger patient numbers are needed to better understand the relationship between graft length in the femoral tunnel, patient-reported outcomes, and risk of revision ACL reconstruction.
Variation of the length of hamstring autograft in the femoral tunnel between 14 and 35 mm does not predict KOOS or IKDC scores at 2 years postoperative. Larger numbers are required to determine whether graft length in the femoral tunnel affects risk of revision surgery.
References
Blickenstaff KR, Grana WA, Egle D (1997) Analysis of a semitendinosus autograft in a rabbit model. Am J Sports Med 25:554–559
Chiroff RT (1975) Experimental replacement of the anterior cruciate ligament. A histological and microradiographic study. J Bone Joint Surg Am 57:1124–1127
Rodeo SA, Arnoczky SP, Torzilli PA, Hidaka C, Warren RF (1993) Tendon-healing in a bone tunnel. A biomechanical and histological study in the dog. J Bone Joint Surg Am 75:1795–1803
Magnussen RA, Lawrence JT, West RL, Toth AP, Taylor DC, Garrett WE (2012) Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy 28:526–531. doi:10.1016/j.arthro.2011.11.024
Park SY, Oh H, Park S, Lee JH, Lee SH, Yoon KH (2012) Factors predicting hamstring tendon autograft diameters and resulting failure rates after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-012-2085-4
Brown CH (2012) Anatomic single-bundle ACL reconstruction using 5-strand (“m5”) autogenous hamstring tendon graft. In: AOSSM Annual Meeting, Baltimore, MD
Greis PE, Burks RT, Bachus K, Luker MG (2001) The influence of tendon length and fit on the strength of a tendon-bone tunnel complex. A biomechanical and histologic study in the dog. Am J Sports Med 29:493–497
Qi L, Chang C, Jian L, Xin T, Gang Z (2011) Effect of varying the length of soft-tissue grafts in the tibial tunnel in a canine anterior cruciate ligament reconstruction model. Arthroscopy 27(6):825–833. doi:10.1016/j.arthro.2011.01.016
Yamazaki S, Yasuda K, Tomita F, Minami A, Tohyama H (2006) The effect of intraosseous graft length on tendon-bone healing in anterior cruciate ligament reconstruction using flexor tendon. Knee Surg Sports Traumatol Arthrosc 14:1086–1093. doi:10.1007/s00167-006-0110-1
Zantop T, Ferretti M, Bell KM, Brucker PU, Gilbertson L, Fu FH (2008) Effect of tunnel-graft length on the biomechanics of anterior cruciate ligament-reconstructed knees: intra-articular study in a goat model. Am J Sports Med 36:2158–2166. doi:10.1177/0363546508320572
Roos EM, Lohmander LS (2003) The knee injury and osteoarthritis outcome score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes 1:64. doi:10.1186/1477-7525-1-64
Irrgang JJ, Anderson AF, Boland AL, Harner CD, Kurosaka M, Neyret P, Richmond JC, Shelborne KD (2001) Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med 29:600–613
Dunn WR, Spindler KP (2010) Predictors of activity level 2 years after anterior cruciate ligament reconstruction (ACLR): a multicenter orthopaedic outcomes network (MOON) ACLR cohort study. Am J Sports Med 38:2040–2050. doi:10.1177/0363546510370280
Wright RW (2009) Knee injury outcomes measures. J Am Acad Orthop Surg 17 (1):31-39. doi:17/1/31 [pii]
Irrgang JJ, Anderson AF, Boland AL, Harner CD, Neyret P, Richmond JC, Shelbourne KD (2006) Responsiveness of the international knee documentation committee subjective knee form. Am J Sports Med 34:1567–1573. doi:10.1177/0363546506288855
Stevens J (2002) Applied multivariate statistics for the social sciences, 4th edn. Lawrence Erlbaum Associates, Mahwah
Acknowledgments
This project was partially funded by grant number 5R01 AR053684 (K.P.S.) and K23 AR063767 (R.A.M.) from the National Institutes of Health/National Institute of Arthritis and Musculoskeletal and Skin Diseases and by grant number 5U18-HS016075 (R.G.M.) from the Center for Education and Research on Therapeutics (Agency of Health Research and Quality). The project was also supported by the Vanderbilt Sports Medicine Research Fund. Vanderbilt Sports Medicine received unrestricted educational gifts from Smith & Nephew Endoscopy and DonJoy Orthopaedics.
We thank the following Multicenter Orthopaedic Outcomes Network (MOON) members, without whom the data utilized in this study would not exist. These members include the following: Kurt P. Spindler, MD; Warren R. Dunn, MD, MPH; Laura J. Huston, MS (Vanderbilt University School of Medicine); Rick W. Wright, MD; Matthew J. Matava, MD; Robert H. Brophy, MD (Washington University School of Medicine at Barnes-Jewish Hospital); Eric C. McCarty, MD; Armando Vidal, MD; Michelle Wolcott, MD (University of Colorado School of Medicine); Robert G. Marx, MD, MSc (Hospital for Special Surgery); Annunziato Amendola, MD; and Brian R. Wolf, MD, MS (University of Iowa).
We thank the following research coordinators, analysts, and support staff from the Multicenter Orthopaedic Outcomes Network (MOON) sites, whose efforts make this consortium possible: Lynn Borzi, Julia Brasfield, Maxine Cox, Michelle Hines, Pam Koeth, Leah Schmitz (Cleveland Clinic Foundation), Kari Stammen (Ohio State University), Carla Britton, Catherine Fruehling-Wall (University of Iowa), Christine Bennett, Paula Langner (University of Colorado), Linda Burnworth, Robyn Gornati, Amanda Haas (Washington University in St. Louis), Brian Boyle, Patrick Grimm, Kaitlynn Lillemoe, Lana Verkuil (Hospital for Special Surgery), Emily Reinke, John Shaw, Suzet Galindo-Martinez, Zhouwen Liu, Thomas Dupont, Erica Scaramuzza, and Lynn Cain (Vanderbilt University).
Disclosure
David C. Flanigan is a consultant for Sanofi and Smith & Nephew.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mariscalco, M.W., Magnussen, R.A., Mitchell, J. et al. How much hamstring graft needs to be in the femoral tunnel? A MOON cohort study. Eur Orthop Traumatol 6, 9–13 (2015). https://doi.org/10.1007/s12570-014-0275-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12570-014-0275-x