Abstract
Purpose
To identify and quantify passive anterior tibial subluxation on MRI using a standardized measurement protocol and determine the diagnostic threshold of subluxation for complete anterior cruciate ligament tears.
Methods
A retrospective case–control study was performed. Patients who underwent surgery for a complete isolated ACL tear between 2009 and 2015 were matched for age and gender to controls with an intact ligament on knee MRI. All subjects underwent 1.5 T closed field MR imaging with the same protocol. Measurements were performed on axial sequences to evaluate translation of the medial and lateral condyles compared to the tibial plateau. Each compartment was measured between the vertical tangent to the posterior femoral condyles and the most posterior part of the tibial plateau. The main criterion was global passive subluxation measurements on MRI, corresponding to mean medial and lateral compartment subluxation. The reproducibility and diagnostic value of passive subluxation were calculated.
Results
Sixty (30/30) subjects were included, mean age 27.1 ± 1.7 years, 20 women and 40 men. Patients had a significantly higher global passive subluxation than controls (3.3 ± 0.6 mm vs 0.6 ± 0.2 mm, respectively p < 0.00001). Reproducibility was excellent and the diagnostic value of passive subluxation for a complete ACL tear was fair. A passive subluxation threshold of 3.5 mm had a sensitivity of 55.2%, a specificity of 100% and 77.6% of well-classified subjects.
Conclusion
The calculated cutoff value for global passive subluxation to identify patients with a complete ACL tear was 3.5 mm, with excellent specificity and a high positive likelihood ratio. Suboptimal clinical results following ACL reconstruction could be partially due to failure to restore an anatomical femorotibial relationship.
Level of evidence
III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Anterior cruciate ligament (ACL) tears are common injuries. The Lachman test provides a clinical assessment of anterior tibial translation with the knee in 20° flexion and can confirm an ACL tear with a sensitivity of 0.87 (95% CI 0.84–0.90) and a specificity of 0.91 (95% CI 0.89–0.93) [8]. The anterior compartment may also be quantified by arthrometer, compared to the contralateral side [1]. MRI usually confirms the ACL tear with a sensitivity of 90–95% and a specificity of 95–100% depending on the study [11].
Spontaneous anterior tibial translation is sometimes observed in patients with ACL tears. Numerous studies have been published on this subject, first using radiography [2, 3] then MRI [6, 14, 16, 17, 19], and it is generally agreed to call this event passive anterior tibial subluxation (PATS). According to Mishima et al. [16], subluxation in this compartment is significantly and positively correlated with anterior laxity of the knee measured on KT-1000. These studies show that although patients can present with PATS on MRI even in a healthy knee, the measurement in this compartment is usually higher in the presence of an ACL tear. The study by Chan et al. [6] is the only report that has proposed a threshold for PATS for the diagnosis of a complete ACL tear based on the receiver operating characteristic (ROC) curve. The threshold in that study was 5 mm, with a sensitivity of 86% and a specificity of 99%. For the moment, the prognostic value of PATS is unknown. Thus, it is first necessary to find an effective diagnostic tool for PATS, then follow patients to evaluate whether surgery corrects this event and if its presence is a negative predictive factor for the long-term radiological and clinical outcome. This threshold should be as specific and accurate as possible but not especially sensitive because there are already effective tools to diagnose complete ACL tears [11, 15].
The main goal of this preliminary study was to identify and quantify PATS on MRI with a standardized measurement protocol. The secondary goal was to determine the diagnostic PATS threshold for a complete ACL tear.
Materials and methods
A retrospective single0center case–control study was performed. Included patients were chosen randomly from the radiological database of our hospital for the period from 2009 to 2015according to study selection criteria. There were two groups: “patients” and “controls” paired for age (± 1 year) and gender.
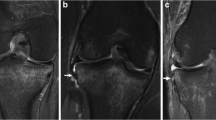
Included patients underwent surgery for a complete isolated ACL tear that was confirmed by arthroscopy. All patients underwent preoperative MRI of the knee at our hospital. Control subjects underwent an MRI of the knee in the same radiology department for a reason other than knee injury. All controls underwent a clinical examination to confirm ACL congruency. An intact ACL on MRI was defined as a fibrillar band with a hypo-intense signal and no local thickening or thinning.
Exclusion criteria included the presence of another ligament injury to the knee or a partial ACL tear. Exclusion criteria for controls were any ligament injury on MRI and a history of ligament injury reported by the patient or noted in the medical file. Patients and controls with a body mass index (BMI) > 25, requiring another MRI antenna were also excluded.
MR imaging and measurement protocol
All MR imaging exams were performed using a closed 1.5 T OPTIMA MR 450W device (General Electric Health Care Milwaukee, USA). Our usual standardized institutional protocol was applied.
All included subjects were positioned in the prone position, with the knee flexed at 20° in neutral rotation and a standard cushion beneath the thigh knee and calf to ensure that the muscles were relaxed.
Classic sequences were obtained with proton density-weighted MRI sequences on the sagittal, coronal and axial planes and T1-weighted sequences on the sagittal plane. Slice thicknesses were 3 mm on the sagittal and coronal sequences and 4 mm on axial sequences.
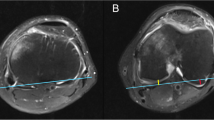
Measurements were obtained on axial plane sequences by evaluating the translation of the medial and lateral condyles compared to the tibial plateau. PATS was quantified in both the medial and lateral compartments. Like Lerat et al. [12], Donell et al. [7] and Tardieu et al. [18] we performed measurements using the most posterior points of the femoral condyles and the tibial plateau. Sagittal and axial sequences were used. A vertical line was drawn from the posterior aspect of the tibial plateau. Global PATS was then calculated as the mean of the lateral and medial condyle values (Fig. 1). The tibial slope was measured according to Hudek and al protocol [9]. MR sequences were analyzed twice by two radiologists a few days apart, using OsiriX v 3.7.1-32 bit.
Ethical approval was obtained for this study from the Comité de Protection des Personnes Ile-de-France IV (CPP IDF IV), Hôpital Saint-Louis.
Statistical analysis
Statistical analyses were performed using Stata/IC V 10.0 software. Thirty patients were empirically included in each group. A post hoc power analysis was performed on the main evaluation criterion (global PATS) only if a significant difference was found after the study was completed, using the obtained sample and effect sizes in the two groups. Measurements were accurate to two decimal places. Testing for normal distribution of data and equality of variances was based on the Shapiro–Wilk and Bartlett tests, respectively. The non-parametric Mann–Whitney test was used for quantitative variables and the Fisher exact for qualitative data. The relationship between each observer’s two measurements and between the two observers’ measurements were determined with non-parametric Spearman’s correlation coefficient. The strength of the correlation was classified as strong (r > 0.5), moderate (0.3 < r < 0.5), weak (0.1 < r < 0.3), or none (r < 0.1). The reliability of intra- and inter-observer measurements and the strength of agreement between measurements were evaluated by the intra-class correlation coefficient (ICC) which was classified as 0 (no agreement) or 1 (total agreement). The strength of agreement was classified as excellent (r > 0.75), good (0.40 < r < 0.75), or poor (r < 0.40). All correlations were tested for statistical significance using the p-value. The optimal laxity threshold was determined with the ROC (receiver operating characteristic) with sensitivity on the x-axis and specificity on the y-axis. This threshold value was chosen to obtain a specificity (Sp) of 100% with the best proportion of correctly classified subjects (accuracy). The positive likelihood ratios (LR+) and negative likelihood ratios (LR−) were calculated so that the diagnostic value of a result increases as the LR+ increases and decreases with the LR−.The diagnostic value of the test was evaluated by the area under the curve (AUC) of ROC: null (AUC 0.5), poorly informative (0.5 < AUC < 0.7), fairly informative (0.7 ≤ AUC < 0.9), highly informative (0.9 ≤ AUC < 1), perfect (AUC 1). A p value of < 0.05 was considered to be significant.
Results
Two groups of 30 patients were included, 40 men and 20 women, mean age 27.1 ± 1.7 years.
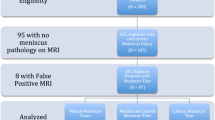
Les Shapiro–Wilk and Bartlett tests were significant so that the hypotheses of a normal distribution and equality of variances were rejected (Fig. 2). Thus, non-parametric tests were used. The mean PATS measurement was significantly higher in the patient group, both for overall PATS and in the medial and lateral compartments (Table 1). A post hoc analysis based on these parameters shows that the power of the test was > 95%. Mean subluxation was smaller in the medial than in the lateral compartment in both groups. No significant difference was found in tibial slope between the cases and controls (4.8 ± 1.2° vs 4.3 ± 1.1°, n.s.) and no significant correlation was found between the global PATS and the tibial slope (r = 0.1, n.s.).
In the control group subluxation was null (0) in the medial compartment in 28 (93.3%) subjects and in the lateral compartment in 21 (70%) subjects, respectively. In patients operated for a complete ACL tear, translation was null in the medial compartment in 11 (36.7%) patients and in 8 (26.7%) patients in the lateral compartment (Fig. 2).
Global PATS was “fairly informative” for the diagnosis of a complete ACL tear with an area under the curve (AUC) of 0.80 (95% CI 0.69–0.91). The global PATS threshold was 3.53 mm for a specificity of 100% (± 3.6, 95% CI), a sensitivity of 55.2% (± 17.8, 95% CI), a percentage of well-classified patients of 77.6%, a positive likelihood ratio (LR+) of 16 and a negative likelihood ratio (LR−) of 0.4 (Fig. 3).
The test–retest correlation was strong and significant for the intra-observer reliability of measurements both in the medial and lateral compartments. The ICC of the agreement between a physician’s initial score and his/her rerating of the same patient was excellent and significant (Table 2).
The inter-observer reliability of measurements was strong and the ICC for agreement between physicians’ ratings of patients were excellent and significant (Table 3).
Discussion
The main finding of this study is that the calculated cutoff value for global PATS to identify patients with a total ACL tear was 3.5 mm, with a specificity of 100%, an accuracy of 77.6% and a positive likelihood ratio of 16. Above this threshold, all patients had a complete ACL tear. The analysis of the AUC showed that PATS was fairly informative. About one quarter of the patients with a complete ACL tear had no PATS.
The threshold in this study was determined using the ROC curve to obtain a specificity of 100%. Chan et al. [6] also used the ROC curve and obtained a threshold of 5 mm with a sensitivity of 86% and a specificity of 99%. The threshold in the current study was lower because most of the control patients had a global PATS of 0, unlike those included in the study by Chan et al. In the study by Vahey et al. [19], with a 5-mm cutoff, intact ligaments were distinguished from torn ligaments with a sensitivity of 58%, a specificity of 93% and an accuracy of 69%. These parameters were based on a 7-mm cutoff with a sensitivity, specificity and accuracy of 38%, 100% and 58% respectively. Mc Donald et al. [14] classified their patients based on a threshold of 6 mm then 10 mm. Healthy knees were found to have a maximum PATS of 5.6 mm with a mean value of 0.01 mm, while patients with ACL tears had a maximum PATS of 10.3 mm with a mean value of 1.08 mm (Table 4). Knees with failed ACLR had significantly more PATS than with primary ACL deficiency [14].
The method of measurement of PATS used in the current study was different from that in previous studies. Axial images were used instead of the sagittal images found in the studies by Lerat et al. [12], Donell et al. [7] and Tardieu et al. [18] for several reasons. The choice of axial sequences is justified. First, it is difficult to draw a perpendicular line to the tibial plateau on sagittal views because the lateral tibial slope is difficult and inaccurate and the top of the lateral tibial plateau is convex. Moreover, the most posterior parts of the tibial plateau and the condyle are not necessarily visible on the same sagittal sequence. By using axial sequences for these measurements, a possible error is avoided, as subluxation is being measured with a line that goes through the most posterior part of the tibial plateau and another through the most posterior part of the condyles.
Tardieu et al. [18] found that translation of the femoral condyle could be reproduced using an orthesis and applying force to reproduce the Lachman test and measured on MRI with good intra and inter-observer reliability. Although this was a dynamic study, the measurements were the same as the current study. They determined a threshold of 1.1 mm for anterior drawer and 2.8 mm for posterior drawer that ensured a good sensitivity and specificity for the diagnosis of an ACL tear. The intra- and inter-observer reproducibility was excellent in the current study. Iwaki et al. [10] described a technique using sagittal sequences but with a model of the condyle as a circle. Tanaka [17] is the only author to report the inter-rater reliability using Iwaki’s [10] technique, with values of 0.72 for the medial compartment and 0.96 for the lateral compartment.
PATS was initially based on radiograph measurements; thus care should be taken when comparing results with previous studies because weight-bearing radiographs were used and tibial slope tends to increase the PATS with this technique. Also radiographs result in a significant bias because translation due to the medial vs lateral condyles cannot be assessed. Almekinders [3] used lateral radiographs to show that placing standardized posterior force on the tibia induced 4.0 mm posterior drawer that could not be reproduced in the ACL tear group. In 2004 the same authors [4] did not find any difference between normal knees and the ACL tear group for maximum posterior tibial position.
In the current study, the mean delay between injury and MRI was not recorded. Mishima et al. [16] showed that PATS increases as the delay between the injury and surgery increases and is positively correlated with instability. PATS measurement on MRI during acute injury could be influenced by muscle contractions in reaction to pain. Patients with failed ACL reconstruction showed a significant increase in anterior tibial subluxation compared to acute ACL tears [14, 17].
The clinical relevance of PATS requires further studies. The results of the current study and the studies in the literature show that there is a relationship with ACL tears. The 3.5-mm threshold is highly specific. In addition to the anatomical logic of restoring an anatomic relationship between the femur and the tibia, PATS has been shown to be associated with the pivot shift. Using a computer navigation system, Bedi et al. [5] showed that a threshold of 6 mm of anterior tibial subluxation in the lateral compartment was needed to create a pivot shift. Grade 1 pivot shift was associated with an average of 10 mm of anterior tibial subluxation. It is, therefore, important to reduce or correct this with surgery and immediate postoperative MRI could help confirm how effectively surgery reduces PATS. It is also necessary to evaluate whether it has a negative predictive value for long-term clinical results, in particular if it is not surgically repaired.
In this case–control study, patients and controls were paired for gender and age. Indeed, according to the literature [13], young women present with physiological anterior laxity. However, Mac Donald et al. [4] did not find any significant correlation between PATS and age. The groups were not paired for two other criteria that also seem to be associated with significantly higher physiological anterior laxity of the knee: the dominant side and hyperextension.
The current study has several limitations. The number of subjects necessary for the study was not calculated. Nevertheless, a high confidence interval for an excellent specificity was obtained. Large epidemiological studies are needed to determine the prevalence of PATS in both healthy subjects and those with ACL tears. Also, the duration of this study was long, which could result in a recruitment bias. This study has included only patients who had undergone an MRI in one hospital to ensure a standardized position of the knee during measurements. Finally, the thickness of MRI slices (4 mm) could also create a bias, because the determined critical value of PATS is similar to this.
At present it would seem reasonable to quantify the PATS using this threshold value on all preoperative MRI. Suboptimal clinical results following ACL reconstruction could be partially due to failure to restore an anatomical femorotibial relationship.
Conclusion
The calculated cutoff value of the global PATS to identify patients with a total ACL tear was 3.5 mm with a very good specificity and a high positive likelihood ratio.
References
Ahldén M, Hoshino Y, Samuelsson K, Araujo P, Musahl V, Karlsson J (2012) Dynamic knee laxity measurement devices. Knee Surg Sports Traumatol Arthrosc 20:621–632
Almekinders LC, Chiavetta JB, Clarke JP (1998) Radiographic evaluation of anterior cruciate ligament graft failure with special reference to tibial tunnel placement. Arthroscopy 14:206–211
Almekinders LC, de Castro D (2001) Fixed tibial subluxation after successful anterior cruciate ligament reconstruction. Am J Sports Med 29:280–283
Almekinders LC, Pandarinath R, Rahusen FT (2004) Knee stability following anterior cruciate ligament rupture and surgery. The contribution of irreducible tibial subluxation. J Bone Jt Surg Am 86-A:983–987
Bedi A, Musahl V, Lane C, Citak M, Warren RF, Pearle AD (2010) Lateral compartment translation predicts the grade of pivot shift: a cadaveric and clinical analysis. Knee Surg Sports Traumatol Arthrosc 18:1269–1276
Chan WP, Peterfy C, Fritz RC, Genant HK (1994) MR diagnosis of complete tears of the anterior cruciate ligament of the knee: importance of anterior subluxation of the tibia. AJR Am J Roentgenol 162:355–360
Donell ST, Marshall TJ, Darrah C, Shepstone L (2006) Cruciate ligament assessment in MRI scans: a pilot study of a static drawer technique. Knee 13:137–144
Huang W, Zhang Y, Yao Z, Ma L (2016) Clinical examination of anterior cruciate ligament rupture: a systematic review and meta-analysis. Acta Orthop Traumatol Turc 50:22–31
Hudek R, Schmutz S, Regenfelder F, Fuchs B, Koch PP (2009) Novel measurement technique of the tibial slope on conventional MRI. Clin Orthop Relat Res 467:2066–2072
Iwaki H, Pinskerova V, Freeman MA (2000) Tibiofemoral movement 1: the shapes and relative movements of the femur and tibia in the unloaded cadaver knee. J Bone Jt Surg Br 82:1189–1195
Klass D, Toms AP, Greenwood R, Hopgood P (2007) MR imaging of acute anterior cruciate ligament injuries. Knee 14:339–347
Lerat JL, Moyen BL, Cladière F, Besse JL, Abidi H (2000) Knee instability after injury to the anterior cruciate ligament. Quantification of the Lachman test. J Bone Jt Surg Br 82:42–47
Lin HC, Lai WH, Shih YF, Chang CM, Lo CY, Hsu HC (2009) Physiological anterior laxity in healthy young females: the effect of knee hyperextension and dominance. Knee Surg Sports Traumatol Arthrosc 17:1083–1088
McDonald LS, van der List JP, Jones KJ, Zuiderbaan HA, Nguyen JT, Potter HG et al (2017) Passive anterior tibial subluxation in the setting of anterior cruciate ligament injuries: a comparative analysis of ligament-deficient states. Am J Sports Med 45:1537–1546
McCauley TR, Moses M, Kier R, Lynch JK, Barton JW, Jokl P (1994) MR diagnosis of tears of anterior cruciate ligament of the knee: importance of ancillary findings. AJR Am J Roentgenol 162:115–119
Mishima S, Takahashi S, Kondo S, Ishiguro N (2005) Anterior tibial subluxation in anterior cruciate ligament-deficient knees: quantification using magnetic resonance imaging. Arthroscopy 21:1193–1196
Tanaka MJ, Jones KJ, Gargiulo AM, Delos D, Wickiewicz TL, Potter HG et al (2013) Passive anterior tibial subluxation in anterior cruciate ligament-deficient knees. Am J Sports Med 41:2347–2352
Tardieu M, Luciani J-F, Bordet B, Le Pogam M-A, Dejour D, Pialat J-B (2011) Evaluation of anterior knee laxity on MRI. J Radiol 92:208–225
Vahey TN, Hunt JE, Shelbourne KD (1993) Anterior translocation of the tibia at MR imaging: a secondary sign of anterior cruciate ligament tear. Radiology 187:817–819
Funding
There was no external funding source for the current study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declare that they have no competing interests.
Ethical approval
Ethical approval was obtained for this study from the Comité de Protection des Personnes Ile-de-France IV (CPP IDF IV), Hôpital Saint-Louis. The database was declared at the National Commission for Data Protection (Commission Nationale de l’Informatique et des Libertés, CNIL, no. 470235).
Rights and permissions
About this article
Cite this article
Hardy, A., Klouche, S., Szarzynski, P. et al. A threshold value of 3.5 mm of passive anterior tibial subluxation on MRI is highly specific for complete ACL tears. Knee Surg Sports Traumatol Arthrosc 27, 885–892 (2019). https://doi.org/10.1007/s00167-018-5159-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5159-0