Abstract
Purpose
The purpose of this study was to compare the accuracy of the preoperative planning method using a three-dimensional (3D) printed model with that of a method using picture archiving and communication system (PACS) images in high tibial osteotomy (HTO).
Methods
Patients who underwent HTO using a 3D printed model (20 patients) and a method based on PACS images (20 patients) from 2012 to 2016 were compared. After obtaining the correction angle, in the 3D printed method, the wedge-shaped 3D printed model was designed. The PACS method used preoperative radiographs. The accuracy of HTO for each method was compared using radiographs obtained at the first postoperative year. The preoperative and postoperative posterior tibial slope angles were also compared.
Results
The weight-bearing line was corrected 21.2 ± 11.8% from preoperatively to 61.6 ± 3.3% postoperatively in the 3D group and from 19.4 ± 12.3% to 61.3 ± 8.1% in the PACS group. The mean absolute difference with the target point was lower in the 3D group (2.3 ± 2.5) than in the PACS group (6.2 ± 5.1; p = 0.005). The number of patients in an acceptable range was higher in the 3D group than in the PACS group. The posterior tibial slope angle was not significantly different in the 3D group (8.6°–8.9°), but was significantly different in the PACS group (9.9°–10.5°, p = 0.042).
Conclusions
In open-wedge HTO, a more accurate correction for successful results could be obtained using the 3D printed model.
Level of evidence
IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
High tibial osteotomy (HTO) is an effective treatment option for patients with degenerative or osteonecrotic changes in the medial knee joint compartment with varus deformity [1, 3, 10, 21]. Correction accuracy is the most important factor for successful results in HTO [8, 15, 23].
Several planning methods, including intraoperative check using a radiopaque line and preoperative radiography of the lower extremity, have been reported [4, 11, 13, 14, 16]. Among these methods, actual-sized print or digital images using a picture archiving and communication system (PACS) or software, such as mediCAD, is usually used by many surgeons. This method can be applied simply and easily. Moreover, several studies have reported the use of a navigation system in HTO [12, 19]. However, these methods have several disadvantages. An intraoperative checking method could increase radiation exposure [17], and the method using a PACS or software could correct only the coronal plane, without maintaining the sagittal plane [9]. Recently, the use of a three-dimensional (3D) printing technique has become popular in craniomaxillofacial surgery [18, 24]. Moreover, the simulation of a real-sized model or cutting guide for osteotomy using this technique in orthopaedic surgery has been reported [15, 22, 25]; further, the simulation method with a 3D printed model using porcine legs was also introduced [9]. Using a 3D printed model, good radiological results in both the coronal and sagittal planes could be obtained.
In this study, better results were hypothesised to be obtained with the method using a 3D printed model than with that using PACS images only in HTO. The purpose of this study was to compare the accuracy of these two methods in open-wedge HTO.
Materials and methods
This study retrospectively evaluated 40 patients (seven men and 33 women) with varus deformity and medial osteoarthritis. From 2012 to 2016, patients underwent open-wedge HTO using either a 3D printed model (20 knees, 3D group) or a method based on PACS images (20 knees, PACS group). From January 2016 to October 2016, 20 patients underwent HTO using a 3D printed model. This group was matched with a control group of 20 patients selected from 92 patients who underwent HTO using a method based on PACS images from January 2012 to December 2015. Matching was performed for age, sex, direction of the knee, preoperative medial deviation of the mechanical axis, mechanical femorotibial angle (mFTA), and posterior tibial slope angle (Table 1).
The median age of the patients was 55 years (range 47–61 years). The median preoperative mFTA was varus 6.7° (range 0.8°–13.7°). The inclusion criteria were as follows: (1) age < 65 years, (2) body mass index (BMI) < 30 kg/m2, (3) pain on the medial side only, (4) high level of activity other than running or jumping, (5) mFTA < varus 15°, and (6) knee flexion > 90°. The exclusion criteria were as follows: (1) flexion contracture > 25°, (2) bicompartmental osteoarthritis, (3) elderly patients with impaired mobility, (4) BMI > 30 kg/m2, and (5) subtotal or total meniscectomy in the compartment. Patients who underwent partial meniscectomy were not excluded.
Preoperative planning using the PACS method and making a 3D model
In the preoperative planning stage, the target angle was first calculated using radiographs in both methods. The patients underwent full-length anteroposterior lower limb weight-bearing radiography, with valgus stress applied to the knee joint to correct the widening of the lateral joint space induced by ligament laxity. This preoperative radiograph was used to draw the lower limb weight-bearing line (line A). After determining the point 62.5% (the target, known as the Fujisawa point) from the medial border along the medial-to-lateral width of the tibial plateau [6], an extension line connecting the centre of the femoral head and the target point was drawn (line B). Thereafter, a line connecting the lateral tibial osteotomy site (C) and the centre of the ankle joint, and a line connecting the lateral osteotomy site were drawn. The angle formed by the two lines was the target angle (Fig. 1).
Measurement of the target angle. Full-length anteroposterior lower limb weight-bearing radiograph was preformed with valgus stress applied to the joint. From the centre of the hip joint, the lower limb weight-bearing line is drawn (line A). After determining the point 62.5% (the target, known as the Fujisawa point) from the medial border along the medial-to-lateral width of the tibial plateau, an extension line connecting the centre of the femoral head and the target point is drawn (line B). Thereafter, a line connecting the lateral tibial osteotomy site (C) and the centre of the ankle joint and a line connecting the lateral osteotomy site were drawn. The angle formed by the two lines was the target angle
In the method using PACS images, a predicted osteotomy line was drawn from the proximal tip of the fibular head to the predicted medial tibial osteotomy site (approximately, 4 cm inferior to the medial border of the tibial plateau), and a predicted opening line was drawn at the determined correction angle. Using the triangle formed, the predicted correction gap (wedge gap, in millimetres) was measured at the cortical bone of the posteromedial tibia (Fig. 2).
Correction gap using picture archiving and communication system images. A predicted osteotomy line is drawn from the proximal extremity of the fibular head to the predicted medial osteotomy site (approximately, 4 cm inferior to the medial border of the tibial plateau), and a predicted opening line is drawn from the lateral tibial osteotomy site (C) at the determined correction angle. Using the triangle formed, the predicted correction gap at the cortical bone of the posteromedial tibia was measured
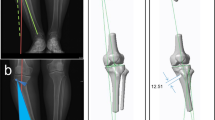
In the method using the 3D printed model, open-wedge HTO was simulated using computed tomography (CT) images, obtained using 3D Slicer software (Brigham and Women’s Hospital, Boston, MA, USA). The medial osteotomy site was determined at 4 cm under the medial tibial plateau, and the lateral hinge point was determined at the upper margin of the fibular head on the proximal tibiofibular joint. The osteotomy gap was opened at the target angle calculated on the preoperative radiograph, with the posterior tibial slope angle maintained. Based on the osteotomy section and target angle, the 3D model was designed and printed (Fortus 450mc, Stratasys, Israel). The biocompatible material, ABS-M30i (Stratasys, Israel), was used for printing (Fig. 3).
Designing of the 3D model. a A 3D image is reconstructed using a software program. b The medial osteotomy site was determined at 4 cm under the medial tibial plateau, and the lateral hinge point was determined at the upper margin of the fibular head on the proximal tibiofibular joint. c Use of the osteotomy plane. d The osteotomy gap was opened at the target angle, and the 3D model was designed using the osteotomy plane. e Designed 3D model. f Printed 3D model. 3D three-dimensional
Surgical technique
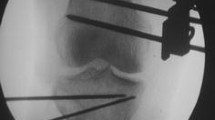
All surgeries were performed by a single surgeon. The patients underwent diagnostic knee arthroscopy prior to osteotomy to assess the condition of the articular surface and meniscus, followed by debridement or meniscectomy, if needed. After the pes anserinus was completely separated, and the superficial medial collateral ligament was elevated from the periosteum, the patient underwent biplanar osteotomy behind the tibial tuberosity. Thereafter, the posteromedial tibial osteotomy site was opened using a chisel and bone spreader, and the osteotomy site was spread.
In the method using PACS images, the gap was measured with a ruler and maintained using a bone spreader. Then, TomoFix locking plate (Synthes GmbH, Solothurn, Switzerland) was fixed.
In the method using the 3D printed model, the printed 3D model was inserted in the osteotomy gap (Fig. 4). Thereafter, OhtoFix locking plate (Ohtomedical Co. Ltd., Goyang, Korea) was fixed, and the 3D printed model was removed from the osteotomy site.
Allogeneic bone chips mixed with an autologous bone marrow were harvested from the ipsilateral anterior superior iliac spine and grafted into the osteotomy gap. The osteotomy site was covered with the superficial medial collateral ligament, and the pes anserinus was resutured to the periosteal membrane. In all 40 patients, lateral cortical hinge fracture did not occur. Active range of motion was started on the second postoperative day, and a night splint was maintained until the second postoperative week. Weight-bearing was allowed in the second postoperative week, as tolerable, and the patients were protected by applying a brace for 4 weeks. Crutches were not recommended.
Evaluation and measurement
For comparative evaluation, full-length lower limb radiographs were obtained preoperatively and at the first postoperative year; the percentages of crossing points between the weight-bearing line and tibial plateau were compared with respect to the medial border. Preoperative and postoperative mFTA and posterior tibial slope angles were also compared. The acceptable range was determined to be within 5% of the target point (57.2–67.5%). Regarding the mFTA, an acceptable range of valgus from 3° to 6° was reported by Hernigou et al. [7]. The posterior tibial slope angle was measured as the angle between the line perpendicular to the tangent to the posterior tibia and the tangent to the tibial plateau. The measurements were evaluated twice independently by two raters with an interval of 1 week.
This study was approved by the institutional review board (IRB) of Kyungpook National University Hospital (IRB no. KNUH 2016-12-030-002).
Statistical analyses
The mean values of the measurements were used as the basis for assessment of the intra- and inter-observer reliabilities by calculation of the intra-class correlation coefficients (ICCs). Values > 0.75 were considered significant. The reliability is shown in Table 2. The ICC for every measurement was significant.
An independent t test was used to compare the preoperative and postoperative values (crossing points of the weight-bearing line and tibial plateau, mFTA, posterior tibial slope angle, and absolute difference with the target point) between the two groups. Paired t tests were used to compare the preoperative and postoperative posterior tibial slope angles. One-sample t test was used to evaluate the degree of proximity to the target point postoperatively. A Chi-square test was used to compare the ratio of the acceptable range between the two groups.
Statistical significance was assumed at p values of < 0.05. All statistical analyses were performed with SPSS Statistics version 21.0 (IBM Co., Armonk, NY, USA).
Results
The results are shown in Table 3.
The weight-bearing line on the tibial plateau was corrected from 21.2 ± 11.8% preoperatively to 61.6 ± 3.3% postoperatively in the 3D group and from 19.4 ± 12.2 to 61.3 ± 8.1% in the PACS group. The postoperative result was not significantly different between the two groups. The proximity of the target point also did not significantly differ between the groups. Regarding the weight-bearing line, the number of patients with values in an acceptable range was higher in the 3D group than in the PACS group (p = 0.028). The mean absolute difference with the target point in the 3D group (2.3 ± 2.5) was lower than that in the PACS group (6.2 ± 5.1; p = 0.005).
The mFTA was corrected from a preoperative mean varus angle of 7.4° ± 2.7° to a postoperative mean valgus of 3.5° ± 1.2° in the 3D group and from a preoperative mean varus angle of 6.9° ± 3.1° to a postoperative mean valgus angle of 3.1° ± 2.3° in the PACS group. The postoperative result was not significantly different between the two groups. Regarding the mFTA, the number of patients in an acceptable range was higher in the 3D group than in the PACS group (p = 0.013).
The posterior tibial slope angle was not significantly different in the 3D group, which changed from 8.6° to 8.9°, but was significantly different in the PACS group, which changed from 9.9° to 10.5° (p = 0.042).
Discussion
The most important finding of this study was more satisfactory correction was possible when using a 3D printed model than when using PACS images, whereas good result of alignment correction could be obtained using both the 3D printed model and PACS images.
The method using an intraoperative radiopaque line, which is frequently used, has disadvantages, including measurement in a non-weight-bearing position and increased radiation exposure, which could consequently increase the possibility of contamination by a fluoroscopy machine [17]. Recently, preoperative planning using PACS images has generally shown good results [11, 13]. In comparison with the method using an intraoperative radiopaque line, a more accurate correction was obtained by several authors [26]. However, the method using PACS images has disadvantages of only planning of the coronal plane, without the consideration of the change in the sagittal plane (e.g., the increase in the posterior tibial slope angle).
The 3D printing technique has been used recently in surgeries, especially in craniomaxillofacial surgery [18, 24]. In orthopaedic surgery, the simulation of a real-sized model or cutting guide for osteotomy using this technique was reported [15, 22, 25]. HTO using a 3D printed model in porcine knee was reported by Kwun et al. [9]. They reported good radiological results in both the coronal and sagittal planes, maintaining the posterior tibial slope angle; therefore, the method could be applicable to HTO in patients with varus deformity. In this study, the correction measurement could be obtained easily using only a 3D printed model intraoperatively, and good radiological results were also obtained.
El-Azab et al. [5] and Brouwer et al. [2] reported that the posterior tibial slope angle also changed during correction of the coronal angle in HTO. Especially, medial open-wedge HTO can increase the posterior tibial slope angle, which causes extension restriction and overload on the anterior cruciate ligament. To maintain the posterior tibial slope angle, the method of opening an anterior gap of 67% of the posterior gap was reported by Song et al. [20]. In this study, the posterior slope angle was not significantly different preoperatively and postoperatively using the 3D printed model. The 3D printed model, which was created during 3D simulation while maintaining the posterior tibial slope angle, allows for maintenance of the slope angle in actual surgeries easily.
The limitations of this study are as follows: small number of patients and retrospective study design. Different locking plates were used between the two groups. Moreover, CT evaluation for obtaining 3D images could be harmful to the patients because of radiation exposure. Finally, we evaluated only radiographic results, excluding the clinical results. Further prospective large-scale studies that include clinical results should be conducted.
Despite these limitations, a more accurate correction for successful results could be obtained using a 3D printed model in HTO.
Conclusion
In this study, good results were obtained after open-wedge HTO using both a 3D printed model and PACS method. A more accurate correction of limb alignment with maintenance of the sagittal plane can be attained using a 3D printed model.
References
Amendola A, Bonasia DE (2010) Results of high tibial osteotomy: review of the literature. Int Orthop 34(2):155–160
Brouwer RW, Bierma-Zeinstra SM, van Koeveringe AJ, Verhaar JA (2005) Patellar height and the inclination of the tibial plateau after high tibial osteotomy. The open versus the closed-wedge technique. J Bone Jt Surg Br 87(9):1227–1232
Coventry MB (1965) Osteotomy of the upper portion of the tiba for degenerative arthritis of the knee. A preliminary report. J Bone Jt Surg Am 47:984–990
Coventry MB (1985) Upper tibial osteotomy for osteoarthritis. J Bone Jt Surg Am 67(7):1136–1140
El-Azab H, Halawa A, Anetzberger H, Imhoff AB, Hinterwimmer S (2008) The effect of closed- and open-wedge high tibial osteotomy on tibial slope: a retrospective radiological review of 120 cases. J Bone Jt Surg Br 90(9):1193–1197
Fujisawa Y, Masuhara K, Shiomi S (1979) The effect of high tibial osteotomy on osteoarthritis of the knee. An arthroscopic study of 54 knee joints. Orthop Clin N Am 10(3):585–608
Hernigou P, Medevielle D, Debeyre J, Goutallier D (1987) Proximal tibial osteotomy for osteoarthritis with varus deformity. A ten to thirteen-year follow-up study. J Bone Jt Surg Am 69(3):332–354
Kettelkamp DB, Wenger DR, Chao EY, Thompson C (1976) Results of proximal tibial osteotomy. The effects of tibiofemoral angle, stance-phase flexion-extension, and medial-plateau force. J Bone Jt Surg Am 58(7):952–960
Kwun JD, Kim HJ, Park J, Park IH, Kyung HS (2017) Open wedge high tibial osteotomy using three-dimensional printed models: experimental analysis using porcine bone. Knee 24(1):16–22
Lee DC, Byun SJ (2012) High tibial osteotomy. Knee Surg Relat Res 24(2):61–69
Lee YS, Kim MK, Byun HW, Kim SB, Kim JG (2015) Reliability of the imaging software in the preoperative planning of the open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 23(3):846–851
Lutzner J, Gross AF, Gunther KP, Kirschner S (2009) Reliability of limb alignment measurement for high tibial osteotomy with a navigation system. Eur J Med Res 14(10):447–450
Marx RG, Grimm P, Lillemoe KA, Robertson CM, Ayeni OR, Lyman S, Bogner EA, Pavlov H (2011) Reliability of lower extremity alignment measurement using radiographs and PACS. Knee Surg Sports Traumatol Arthrosc 19(10):1693–1698
Miniaci A, Ballmer FT, Ballmer PM, Jakob RP (1989) Proximal tibial osteotomy. A new fixation device. Clin Orthop Relat Res (246):250–259
Pérez-Mañanes R, Burró JA, Manaute JR, Rodriguez FC, Martín JV (2016) 3d surgical printing cutting guides for open-wedge high tibial osteotomy: do it yourself. J Knee Surg 29(08):690–695
Pape D, Seil R, Adam F, Rupp S, Kohn D, Lobenhoffer P (2004) Imaging and preoperative planning of osteotomy of tibial head osteotomy. Orthopade 33(2):122–134
Peters PG, Laughlin RT, Markert RJ, Nelles DB, Randall KL, Prayson MJ (2012) Timing of C-arm drape contamination. Surg Infect (Larchmt) 13(2):110–113
Poukens J, Haex J, Riediger D (2003) The use of rapid prototyping in the preoperative planning of distraction osteogenesis of the cranio-maxillofacial skeleton. Comput Aided Surg 8(3):146–154
Ribeiro CH, Severino NR, Fucs PM (2013) Preoperative surgical planning versus navigation system in valgus tibial osteotomy: a cross-sectional study. Int Orthop 37(8):1483–1486
Song EK, Seon JK, Park SJ, Jeong MS (2010) The complications of high tibial osteotomy: closing-versus opening-wedge methods. J Bone Jt Surg Br 92(9):1245–1252
Sprenger TR, Doerzbacher JF (2003) Tibial osteotomy for the treatment of varus gonarthrosis. Survival and failure analysis to twenty-two years. J Bone Jt Surg Am 85(3):469–474
Starosolski ZA, Kan JH, Rosenfeld SD, Krishnamurthy R, Annapragada A (2014) Application of 3-D printing (rapid prototyping) for creating physical models of pediatric orthopedic disorders. Pediatr Radiol 44(2):216–221
Tjornstrand B, Egund N, Hagstedt B, Lindstrand A (1981) Tibial osteotomy in medial gonarthrosis. The importance of over-correction of varus deformity. Arch Orthop Trauma Surg 99(2):83–89
Wilde F, Cornelius C-P, Schramm A (2014) Computer-assisted mandibular reconstruction using a patient-specific reconstruction plate fabricated with computer-aided design and manufacturing techniques. Craniomaxillofac Trauma Reconstr 7(2):158–166
Wu XB, Wang JQ, Zhao CP, Sun X, Shi Y, Zhang ZA, Li YN, Wang MY (2015) Printed three-dimensional anatomic templates for virtual preoperative planning before reconstruction of old pelvic injuries: initial results. Chin Med J (Engl) 128(4):477–482
Yoon SD, Zhang G, Kim HJ, Lee BJ, Kyung HS (2016) Comparison of cable method and miniaci method using picture archiving and communication system in preoperative planning for open wedge high tibial osteotomy. Knee Surg Relat Res 28(4):283–288
Funding
This study received no funding to complete.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the institutional review board (IRB) of Kyungpook National University Hospital (IRB no. KNUH 2016-12-030-002).
Informed consent
Patients gave informed consent prior to study inclusion.
Rights and permissions
About this article
Cite this article
Kim, HJ., Park, J., Shin, JY. et al. More accurate correction can be obtained using a three-dimensional printed model in open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 26, 3452–3458 (2018). https://doi.org/10.1007/s00167-018-4927-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-4927-1