Abstract
Purpose
The medial patellotibial ligament (MPTL), the medial patellofemoral ligament (MPFL), and the medial patellomeniscal ligament (MPML) support the stability of the patellofemoral joint. The purpose of this systematic review was to report the surgical techniques and clinical outcomes of the repair or reconstruction of the MPTL in isolation or concomitant with the MPFL and/or other procedures.
Methods
A systematic review of the literature was conducted. Inclusion criteria were articles in the English language that reported clinical outcomes of the reconstruction of the MPTL in isolation or in combination with the MPFL and/or other procedures. Included articles were then cross-referenced to find additional journal articles not found in the initial search. The methodological quality of the articles was determined using the Coleman Methodology Score.
Results
Nineteen articles were included detailing the clinical outcomes of 403 knees. The surgical procedures described included hamstrings tenodesis with or without other major procedures, medial transfer of the medial patellar tendon with or without other major procedures and the reconstruction of the MPTL in association with the MPFL. Overall, good and excellent outcomes were achieved in > 75% of cohorts in most studies and redislocations were < 10%, with or without the association of the MPFL. An exception was one study that reported a high failure rate of 82%. Results were consistent across different techniques. The median CMS for the articles was 66 out of 100 (range 30–85).
Conclusion
Across different techniques, the outcomes are good with low rates of recurrence, with one article reporting a high rate of recurrence. Quality of the articles is variable, from low to high. Randomized control trials are needed for a better understanding of the indications, surgical techniques, and clinical outcomes. This systematic review suggests that the reconstruction of the MPTL leads to favorable clinical outcomes and supports the role of the procedure as a valid surgical patellar stabilization procedure.
Level of evidence
IV: systematic review of level I–IV studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
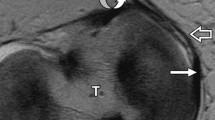
Lateral patellar dislocation is a significant cause of knee injuries with associated hemarthrosis, especially in young patients [1]. The medial patellotibial ligament (MPTL), in association with the medial patellofemoral ligament (MPFL) and the medial patellomeniscal ligament (MPML), is responsible for maintaining the stability of the patellofemoral (PF) joint. While the MPFL is the primary stabilizer of the PF joint (contributing ~ 50–60% to medial restriction during early flexion), the function of the MPTL should not be understated [8, 9, 17, 20, 35]. It has been shown that the contribution of the MPTL and MPML in the restriction of lateral patellar translation increases from 26% at full extension to 46% at 90◦ flexion [36]. In addition, the influence of the MPTL and MPML in resisting lateral patellar tilt at 90◦ flexion was 72% [36].
In 1922, Galeazzi [12] described a semitendinosus (ST) patellar tenodesis for treating patellar instability. In 1998, Rillmann et al. [37] described a transfer of the medial portion of the patellar tendon (PT). Both surgical techniques are analogous to a MPTL reconstruction. Many other authors have reported their results with these procedures, in isolation or combined with procedures other than the MPFL (e.g., lateral retinaculum release, tibial tuberosity osteotomy—TTO, Roux–Goldthwait) [3, 23, 26, 29, 31]. With the introduction of the MPFL reconstruction in the early 2000s, the reconstruction of the MPTL has fallen out of favor. More recently, however, combined MPFL and MPTL reconstruction has been reported [5, 10, 11, 13, 18, 39].
The MPTL reconstruction and analogous procedures have been part of the surgical armamentarium for surgical treatment of patella instability for decades [3, 26, 37]; despite this, clinical reported outcomes have remained sparse. The purpose of this systematic review is to report the techniques and clinical outcomes of the reconstruction of the MPTL in isolation and in combination with the MPFL and/or other procedures, in patients with lateral patellofemoral instability. The hypothesis of this review is that reconstruction of the MPTL leads to favorable clinical outcomes with minimal morbidity.
Materials and methods
Literature search
The Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) protocol for reporting systematic reviews and meta-analyses [27] was followed. Clinical studies of the reconstruction of the MPTL were identified with the goal of summarizing current evidence and elucidating the effectiveness of these surgical procedures. Two authors (CAB and ELP) independently conducted a broad search of PubMed (NLM), and Medline (OvidSP) employing the predetermined search terms: “MPTL”, “medial patellotibial ligament”, “medial patellotibial ligament reconstruction”, “patellar dislocation reconstruction”, “Galeazzi”, “semitendinosus tenodesis”, “patellar tenodesis”, for English-language articles prior to May 20, 2017. All peer-reviewed journal articles that provided any clinical outcomes concerning the reconstruction of the MPTL were included. Exclusion criteria were surgical technique articles, review articles, and clinical studies that did not report any clinical outcomes. Discrepancies were resolved by one senior author (BBH). In addition, the articles’ references were reviewed to locate journal articles not identified in the initial search.
Data extraction and analysis
All study data was extracted using a standardized predetermined criterion: study (first author and year), number of knees, follow-up, indications, graft/technique used for the MPTL reconstruction, associated risk factors, associated procedures, and clinical results. To interpret results, the studies were grouped by technique, and further grouped by the association with, or absence of, other major procedures. For this purpose, associated procedures considered major were procedures that significantly changed patellofemoral morphology or alignment, such as tibial tuberosity osteotomy (TTO), Roux–Goldthwait procedure (medial transfer of the lateral half of the patellar tendon), Green’s procedure (transfer of the medial head of the quadriceps to the lateral patella with a duplication of the medial patella retinaculum and joint capsule), Insall’s proximal realignment (medial advancement of a medial flap created by a medial parapatellar arthrotomy, with lateral retinacular release) and trochleoplasty. In addition, the combined reconstruction of the MPTL with the MPFL was considered a separate group. Redislocation was recorded as a further episode of lateral patellar dislocation. Other stability-related issues such as lateral subluxation, apprehension, medial instability, or subjective instability complaints were recorded separately, as complications.
Quality assessment
The methodological quality of the articles included in this systematic review was assessed by the Coleman Methodology Score (CMS) [7]. Two authors independently applied the CMS (CAB and ELP); and then, a final score was reached by consensus. The CMS is computed by summation of ten separate criteria (study size, follow-up, number of procedures, type of study, diagnostic certainty, description of surgical technique, rehabilitation and compliance, outcome criteria, outcome assessment, and selection process), leading to a total possible score of 100 [7]. The higher the score, the more probable the study avoids chance and other biases characteristic of poor methodology.
Statistical analysis
Mean and standard deviation (SD) were calculated for each criterion. Differences between the groups (by technique, and with or without associated major procedures) were tested by Student’s T test (SigmaPlot 13.0), with significance set at p ≤ 0.05.
Results
Literature search
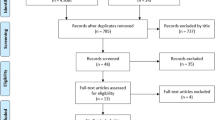
The articles included in this study were published between the years of 1972 and 2016. No randomized control trial was found in our search, and all articles are case reports or case series. The flowchart of search, exclusion, and inclusion is shown in Fig. 1.
Data extraction
Table 1 shows the results of the data that were extracted.
In the 19 papers, a total of 403 knees were included. Mean follow-up ranged from 5.5 months to 8.1 years. The mean follow-up was less than 2 years: n = 10 (2%), 2–5 years: n = 212 (53%), 5–10 years: n = 181 (45%).
There were five articles that discussed ST tenodesis without other major procedures (130 knees, 32%), four articles that discussed ST tenodesis with other major procedures (45 knees, 11%), three articles that discussed medial transfer of the patellar tendon without other major procedures (103 knees, 26%), two articles that discussed the medial transfer of the patellar tendon with other major procedures (47 knees, 12%), and five articles that discussed MPTL reconstruction associated with MPFL reconstruction (78 knees, 19%, mostly without other major procedures).
Reconstruction of the MPTL was indicated for the treatment of patellar instability; mostly objective instability with recurrent lateral patellar dislocations. Some authors indicate the procedure in the absence of risk factors [5, 10, 34, 39] and others in the presence of anatomic patellar instability risk factors or factors associated with worse outcomes [16, 18, 23, 25, 33]. More specific indications were reported in only one paper by Hinckel el al [18]. These indications were: subluxation in extension, instability in flexion, knee hyperextension with ligamentous laxity, and skeletal immaturity with associated risk factors.
From the MPTL reconstruction without the MPFL, most knees did not undergo other major procedures, 233 knees versus 92 with other major procedures. For MPTL reconstruction, all used autograft tissue: hamstrings (ST or G) (242 knees, 60.3%), medial patellar tendon (157 knees, 39%), or the iliotibial band (3 knees, 0.7%). One repair was described. In the surgical technique utilizing ST/G, the hamstring tibial insertion was preserved in 231 (95%). In the medial patellar tendon transfer techniques, an associated distal bone plug for tibial fixation was harvested in 83 (53%).
Of the 403 knees reported in this review, 328 of the knees reported on redislocation rates as an outcome; of which 11 redislocations were reported (3.4%). Overall, there were 11 redislocations (2.7%). Grannat et al. [14] did not report redislocation separately, but reported reoperation due to instability. These cases were likely severely unstable and were reported in this review as “redislocation equivalent”. Redislocation and redislocation equivalent totaled 23 (6%). Although as mentioned it is not clear how many actual redislocations were present in Grannatt et al. [14], the 35% redislocation equivalent reported was much higher than the < 10% reported in all other studies. Redislocation in the MPTL without other major procedures group was 9 (3.8%) and 21 (8.9%), including the redislocation equivalent from Grannatt et al., versus 3 (1.8%) with other major procedures or MPFL. Overall, there were 58 complications (14.4%). Most common complications other than redislocation were wound complications [3, 16, 18, 23], quadriceps atrophy [26], anterior pain [3, 26] and subjective instability complaints [3].
Semitendinosus tenodesis without other major procedures
A modified Galeazzi technique with bone tunnels was performed [2, 3, 14, 26, 30]. A variety of risk factors were present. Lateral retinaculum release and medial retinaculum plication were commonly performed. In addition, Aulisa et al. [2] reported adequate correction of patellar tilt and subluxation, and correction of patellar height without quadriceps contraction; in patients with patella alta, corrections were not maintained during quadriceps contraction.
Semitendinosus tenodesis with other major procedures
These cohorts consisted mostly of patients with risk factors and many highly unstable patients, including habitual dislocation. The major procedures were Roux–Goldthwait procedure, Insall’s proximal realignment and Green procedure. All complications were related to wound problems/skin necrosis at the surgical site.
Medial transfer of the medial patellar tendon without other major procedures
Rillmann et al. utilized the medial portion of the patellar tendon with a bone block from the tibial tuberosity, while Myers et al. and Oliva et al. utilized only the patellar tendon. The presence of risk factors was variable or not mentioned. Rillman et al. performed very few associated procedures while Myers et al. and Oliva et al. performed a vastus medialis advancement and lateral retinaculum release in all knees as part of the “3-in-1 procedure”.
Medial transfer of the medial patellar tendon with other major procedures
Risk factors were very common in these cohorts, and Marcacci et al. [29] had 100% of patients with patella alta and Zaffagnini et al. [41] > 95% of severe trochlea dysplasia (Types B, C, and D of Dejour). To correct these risk factors, Marcacci et al. performed major procedures in almost all knees (most common, was TTO), while Zaffagnini et al. performed them in approximately 25% of the cases (most common was trochleoplasty).
MPTL and MPFL reconstruction
Most studies used hamstrings autograft preserving the tibial attachment [5, 11, 39], and two had free ends fixed in the tibia [10, 18], one using hamstrings [10] and one using the medial patellar tendon [18]. Three techniques permit tensioning of the MPFL and MPTL to be independent [5, 10, 18] while two did not. Mostly, patients had no risk factors, although Ebied and El-Kholy performed TTO in 32% to correct a large quadriceps vector [11]. In addition, in Hinckel et al. cohort, high-grade dysplasia was present in 43%, patella alta in 71% of patients and large quadriceps vector in 43%. Specific correction to address the risk factor was performed in only 14% (one patient) by shortening of the patellar tendon due to restrictions by open physis in most patients.
Description and details of the surgical techniques are abridged in the Appendix.
Quality assessment
The results of the CMS are systematized in Table 2. There was a large range of CMS values, 30–91, and the mean was 64.1. Many studies had small study sizes, short follow-ups, unclear outcome criteria and assessments, and poor patient selection processes, and were retrospective. Therefore, scores were particular low across studies in the CMS criterion of study size, type of study, and outcome assessment. There was no statistically significant difference between subgroups (Table 3).
Discussion
The most important findings were that a considerable number of articles (N = 19) with a substantial number of knees (N = 403) reported favorable outcomes with low rates of redislocation associated with the reconstruction of the MPTL. Quality of the articles is variable, from low to high.
The introduction of MPFL reconstruction has resulted in a shift from the reconstruction of the MPTL to the MPFL, due to its favorable biomechanics in resisting lateral translational restraint near extension [8, 9, 17, 35]. However, with a 12% persistence of objective or subjective instability [38] after isolated MPFL reconstruction, interest in the MPTL as an augmentation has grown. Anatomical, histological, and biomechanical studies have shown that the MPTL is a proper ligament, with biomechanical characteristics (load to failure and stiffness) that can be advantageous to the patellofemoral tracking and stability [20, 24, 36]. By providing this additional ligamentous support in carefully selected patients, combined reconstruction of the MPTL and MPFL can potentially improve outcomes relative to isolated MPFL reconstructions [5, 10, 11, 13, 18, 39]. In addition, this combination may reduce surgical morbidity by decreasing the need for additional bony procedures, thereby defining a different surgical threshold for when to add a TTO or a trochleoplasty [21]. This systematic review summarizes the clinical evidence of the MPTL reconstruction in isolation or in combination with other minor or major procedures, and/or the MPFL. Acknowledging the benefits and complications from the MPTL reconstruction may help the surgeon decide if it is worthy to consider the addition of the procedure to current patellar instability algorithms.
Even though no meta-analysis could be made, we conclude that, in general, good clinical outcomes were achieved. This is supported by the low rate of redislocations (mostly < 10%), similar to redislocations reported after isolated MPFL reconstructions surgeries [4, 6, 22, 28, 42]. When analyzing redislocations, it is important to recognize that three studies did not adequately report them [2, 11, 14]. In addition, good and excellent outcomes were achieved in > 75% of cohorts in most studies. In the papers that reported the presence of risk factors or factors associated with worse outcomes, their presence did not seem to negatively affect clinical outcomes. Frequently, patients with risk factors had additional procedures such as trochleoplasty, TTO, Roux–Goldthwait, or MPFL reconstruction [16, 18, 23, 25, 29, 33, 41]. However, in some cohorts, the MPTL reconstruction was in essence isolated and nothing but minor procedures were added [26, 37]. Therefore, the presence of risk factors is seemingly not a contraindication to the procedure. The study from Grannatt et al., which included 34 knees, has worse outcomes than the other studies collectively [14]. Considering the study from Grannatt et al. had far worse outcomes, results and complications should be analyzed with this consideration in mind [14]. Other than redislocations, there were few complications reported. Of these, two of the studies that reported wound complications, in about 30% of the patients each, had a population of habitual dislocations and other major procedures were performed [16, 23]. Therefore, wound problems should be related to extensive exposure and releases. As such, they should be avoided when possible. Other concerning complications that could be associated with the increase in the medial and distal restriction by the MPTL, such as patella baja and arthritis, were rare. The slightly higher rate of complications in the MPTL and MPFL reconstruction could be a result of the combination of procedures, but may also be just a reflect of better reporting characteristic of more recent studies.
In aggregate, this is encouraging information and the authors believe that the MPTL reconstruction can be added to current patellar instability algorithms with low risk of additional morbidity. However, it should not be included as a standard procedure for all patellar instability patients, neither substitute MPFL reconstruction, owing to the fact that many patients do well with isolated MPFL reconstruction [4, 6, 22, 28, 42]. In addition, the addition of a MPTL reconstruction might decrease the need for bony procedures, such as TTO in patients with borderline patella alta/lateralized force vector or trochleoplasty in patients with moderate dysplasia. However, bony procedures will likely continue to have an important role in correcting more severe malalignment and maltracking. Due to lack of randomized control trial or comparative studies, and scarce study of specific conditions or situations associated with patellar stability that would benefit from the procedure, we are unable to define the ideal indications for MPTL reconstruction from the clinical data reviewed. Nonetheless, the authors believe that the indications suggested by Hinckel et al. [18, 19] (subluxation in extension, instability in flexion, knee hyperextension with ligamentous laxity, and skeletal immaturity with associated risk factors) are supported by some clinical data as well as anatomical and biomechanical studies, and can be used with caution until stronger clinical evidence is available.
In this literature review, many different techniques were found. Nevertheless, they are fundamentally variations in graft choice, harvesting, and fixation. There are two major graft options (hamstrings, ST and/or G; and the medial patellar tendon). The hamstrings can be used as a free graft or the tibial attachment can be maintained. With the medial patellar tendon, the patellar attachment is preserved and the distal portion can be detached as soft tissue only or with a bone plug. It is important to acknowledge that hamstrings insertion (distal to proximal tibial growth plate; 41 ± 6.6 mm distal from the joint line and 6.88 ± 1 mm medial to the patellar tendon [15]) is more distal and more midline than the MPTL insertion (≈ 13 mm distal to joint line and ≈ 12 mm medial to patellar tendon [20, 24]) leading to a non-anatomic reconstruction. In addition, in children, the graft should be fixed on the proximal epiphysis of the tibia, so tension can be maintained during growth; this agrees with MPFL surgical principles of fixation distal to the femoral growth plate [21, 32]. For the patellar tendon, the preserved patellar attachment coincides with the MPTL insertion [20, 21, 24]. When concomitant to the MPFL, techniques that permit independent fixation [5, 10, 18, 39] are advantageous. Since, for the MPFL is better to tension it and secure it between 20° and 45° of flexion, while for the MPTL is better to tension it and secure fixation in greater degrees of flexion (close to 90°) to preserve its biomechanical function [36, 40]. Drilling of patellar tunnels can potentially result in patellar fracture, but that complication was not reported. Even though there are advantages and disadvantages with the different techniques, results were consistent and any of them can be used accordingly to surgeon’s preference.
The Coleman score demonstrated that, on average, the studies had moderate quality. In addition, it can be noted that focusing on enlarging samples, utilizing prospective and randomized studies, and employing validated PROs in future studies will improve the most common deficiencies seen. These improvements will aid in determining for which subgroup of patients with patellar instability the MPTL reconstruction should be indicated.
The greatest limitation of this systematic review is the quality of the studies reported. There are no randomized control trials versus non-operative treatment neither comparing different operative treatments or different subgroup of patients. Furthermore, many studies are dated and, therefore, currently used PROs were not often reported. Due to heterogeneity and small size of cohorts, lack of randomized trials, and lack of common PROs among studies, it was not possible to perform a meta-analyzes. The clinical significance of this review is to present the clinical outcomes and complications of the MPTL reconstruction, so that surgeons can appropriately include the procedure in surgical armamentarium of treatment for recurrent patella instability.
Conclusions
Published literature on MPTL reconstruction suggests that it leads to favorable clinical outcomes with minimal morbidity, which supports this as a valid surgical technique for lateral patellar dislocations and that there is a role for MPTL reconstructions in surgical patellar stabilization techniques.
References
Askenberger M, Ekstrom W, Finnbogason T, Janarv P-M (2014) Occult intra-articular knee injuries in children with hemarthrosis. Am J Sports Med 42(7):1600–1606
Aulisa AG, Falciglia F, Giordano M, Savignoni P, Guzzanti V (2012) Galeazzi’s modified technique for recurrent patella dislocation in skeletally immature patients. J Orthop Sci 17(2):148–155
Baker RH, Carroll N, Dewar FP, Hall JE (1972) The semitendinosus tenodesis for recurrent dislocation of the patella. J Bone Joint Surg Br 54(1):103–109
Bitar AC, Demange MK, D’Elia CO, Camanho GL (2012) Traumatic patellar dislocation: nonoperative treatment compared with MPFL reconstruction using patellar tendon. Am J Sports Med 40(1):114–122
Brown GD, Ahmad CS (2008) Combined medial patellofemoral ligament and medial patellotibial ligament reconstruction in skeletally immature patients. J Knee Surg 21(4):328–332
Christiansen SE, Jacobsen BW, Lund B, Lind M (2008) Reconstruction of the medial patellofemoral ligament with gracilis tendon autograft in transverse patellar drill holes. Arthroscopy 24(1):82–87
Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD (2000) Studies of surgical outcome after patellar tendinopathy: Clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports 10(1):2–11
Conlan T, Garth WP Jr, Lemons JE (1993) Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am 75(5):682–693
Desio SM, Burks RT, Bachus KN (1998) Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med 26(1):59–65
Drez D Jr, Edwards TB, Williams CS (2001) Results of medial patellofemoral ligament reconstruction in the treatment of patellar dislocation. Arthroscopy 17(3):298–306
Ebied AM, El-Kholy W (2012) Reconstruction of the medial patello-femoral and patello-tibial ligaments for treatment of patellar instability. Knee Surg Sports Traumatol Arthrosc 20(5):926–932
Galeazzi R (1922) New applications of muscle and tendon transplant. Arch Ortop 38:315–323
Giordano M, Falciglia F, Aulisa AG, Guzzanti V (2012) Patellar dislocation in skeletally immature patients: Semitendinosous and gracilis augmentation for combined medial patellofemoral and medial patellotibial ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 20(8):1594–1598
Grannatt K, Heyworth BE, Ogunwole O, Micheli LJ, Kocher MS (2012) Galeazzi semitendinosus tenodesis for patellofemoral instability in skeletally immature patients. J Pediatr Orthop 32(6):621–625
Grassi CA, Fruheling VM, Abdo JC, Moura MFAD, Namba M, Silva JLVD, Cunha LAMD, Franco APGDO, Costa IZ, Filho ES (2013) Estudo anatômico da inserção dos tendões flexores do joelho/[Hamstring tendons insertion—an anatomical study]. Rev Bras Ortop 48(5):417–420
Hall JE, Micheli LJ, McManama GB Jr (1979) Semitendinosus tenodesis for recurrent subluxation or dislocation of the patella. Clin Orthop Relat Res (144):31–35
Hautamaa PV, Fithian DC, Kaufman KR, Daniel DM, Pohlmeyer AM (1998) Medial soft tissue restraints in lateral patellar instability and repair. Clin Orthop Relat Res (349):174–182
Hinckel BB, Gobbi RG, Bonadio MB, Demange MK, Pécora JR, Camanho GL (2016) Reconstruction of medial patellofemoral ligament using quadriceps tendon combined with reconstruction of medial patellotibial ligament using patellar tendon: initial experience. Rev Bras Ortop 51(1):75–82
Hinckel BB, Gobbi RG, Demange MK, Bonadio MB, Pecora JR, Camanho GL (2016) Combined reconstruction of the medial patellofemoral ligament with quadricipital tendon and the medial patellotibial ligament with patellar tendon. Arthrosc Tech 5(1):e79–e84
Hinckel BB, Gobbi RG, Demange MK, Pereira CAM, Pecora JR, Natalino RJM, Miyahira L, Kubota BS, Camanho GL (2017) Medial patellofemoral ligament, medial patellotibial ligament, and medial patellomeniscal ligament: anatomic, histologic, radiographic, and biomechanical study. Arthroscopy 33(10):1862–1873
Hinckel BB, Gobbi RG, Kaleka CC, Camanho GL, Arendt EA (2017) Medial patellotibial ligament and medial patellomeniscal ligament: anatomy, imaging, biomechanics, and clinical review. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-017-4469-y
Howells NR, Barnett AJ, Ahearn N, Ansari A, Eldridge JD (2012) Medial patellofemoral ligament reconstruction: a prospective outcome assessment of a large single centre series. J Bone Joint Surg Br 94(9):1202–1208
Joo SY, Park KB, Kim BR, Park HW, Kim HW (2007) The ‘four-in-one’ procedure for habitual dislocation of the patella in children: early results in patients with severe generalised ligamentous laxity and aplasis of the trochlear groove. J Bone Joint Surg Br 89(12):1645–1649
Kaleka CC, Aihara LJ, Rodrigues A, de Medeiros SF, de Oliveira VM, de Paula Leite Cury R (2017) Cadaveric study of the secondary medial patellar restraints: patellotibial and patellomeniscal ligaments. Knee Surg Sports Traumatol Arthrosc 25 (1):144–151
Kocon H, Kabacyj M, Zgoda M (2012) The results of the operative treatment of patellar instability in children with Down’s syndrome. J Pediatr Orthop B 21(5):407–410
Letts RM, Davidson D, Beaule P (1999) Semitendinosus tenodesis for repair of recurrent dislocation of the patella in children. J Pediatr Orthop 19(6):742–747
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JPA, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62(10):e1–e34
Ma L-F, Wang F, Chen B-C, Wang C-H, Zhou J-W, Wang H-Y (2013) Medial retinaculum plasty versus medial patellofemoral ligament reconstruction for recurrent patellar instability in adults: a randomized controlled trial. Arthroscopy 29(5):891–897
Marcacci M, Zaffagnini S, Lo Presti M, Vascellari A, Iacono F, Russo A (2004) Treatment of chronic patellar dislocation with a modified Elmslie–Trillat procedure. Arch Orthop Trauma Surg 124(4):250–257
Moyad TF, Blakemore L (2006) Modified Galeazzi technique for recurrent patellar dislocation in children. Orthopedics 29(4):302–304
Myers P, Williams A, Dodds R, Bulow J (1999) The three-in-one proximal and distal soft tissue patellar realignment procedure. Results, and its place in the management of patellofemoral instability. Am J Sports Med 27(5):575–579
Nelitz M, Reichel H, Dornacher D, Lippacher S (2012) Anatomical reconstruction of the medial patellofemoral ligament in children with open growth-plates. Arch Orthop Trauma Surg 132(11):1647–1651
Niedzielski KR, Malecki K, Flont P, Fabis J (2015) The results of an extensive soft-tissue procedure in the treatment of obligatory patellar dislocation in children with ligamentous laxity: A post-operative isokinetic study. Bone Joint J 97-B (1):129–133
Oliva F, Ronga M, Longo UG, Testa V, Capasso G, Maffulli N (2009) The 3-in-1 procedure for recurrent dislocation of the patella in skeletally immature children and adolescents. Am J Sports Med 37(9):1814–1820
Panagiotopoulos E, Strzelczyk P, Herrmann M, Scuderi G (2006) Cadaveric study on static medial patellar stabilizers: the dynamizing role of the vastus medialis obliquus on medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc 14(1):7–12
Philippot R, Boyer B, Testa R, Farizon F, Moyen B (2012) The role of the medial ligamentous structures on patellar tracking during knee flexion. Knee Surg Sports Traumatol Arthrosc 20(2):331–336
Rillmann P, Dutly A, Kieser C, Berbig R (1998) Modified Elmslie–Trillat procedure for instability of the patella. Knee Surg Sports Traumatol Arthrosc 6(1):31–35
Shah JN, Howard JS, Flanigan DC, Brophy RH, Carey JL, Lattermann C (2012) A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med 40(8):1916–1923
Sobhy MH, Mahran MA, Kamel EM (2013) Midterm results of combined patellofemoral and patellotibial ligaments reconstruction in recurrent patellar dislocation. Eur J Orthop Surg Traumatol 23(4):465–470
Victor J, Wong P, Witvrouw E, Sloten JV, Bellemans J (2009) How isometric are the medial patellofemoral, superficial medial collateral, and lateral collateral ligaments of the knee? Am J Sports Med 37(10):2028–2036
Zaffagnini S, Grassi A, Marcheggiani Muccioli GM, Luetzow WF, Vaccari V, Benzi A, Marcacci M (2014) Medial patellotibial ligament (MPTL) reconstruction for patellar instability. Knee Surg Sports Traumatol Arthrosc 22(10):2491–2498
Zhao J, Huangfu X, He Y (2012) The role of medial retinaculum plication versus medial patellofemoral ligament reconstruction in combined procedures for recurrent patellar instability in adults. Am J Sports Med 40(6):1355–1364
Funding
There was no funding for this study.
Author information
Authors and Affiliations
Contributions
CAB certifies that he had no conflicts of interest related to this study. ELP certifies that he had no conflicts of interest related to this study. SLS certifies that he had no conflicts of interest directly related to this study (see declaration of disclosure form for indirect activities outside the submitted work). EAA certifies that she had no conflicts of interest directly related to this study (see declaration of disclosure form for indirect activities outside the submitted work). BBH certifies that she had no conflicts of interest related to this study.
Corresponding author
Ethics declarations
Conflict of interest
The authors of this study certify that they had no conflicts of interest directly related to this study (see individual declarations of disclosure for indirect activities outside the submitted work).
Ethical approval
This literature review involved the study of existing data, and approval from IRB was not applicable.
Informed consent
This literature review involved the study of existing data, and informed consent was not applicable.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Baumann, C.A., Pratte, E.L., Sherman, S.L. et al. Reconstruction of the medial patellotibial ligament results in favorable clinical outcomes: a systematic review. Knee Surg Sports Traumatol Arthrosc 26, 2920–2933 (2018). https://doi.org/10.1007/s00167-018-4833-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-4833-6