Abstract
Purpose
This prospective study was undertaken to evaluate the diagnostic accuracy of the Synovasure™ α-defensin lateral flow assay to detect or exclude infection and to compare it to the sensitivity and specificity of other diagnostic criteria according to the International Consensus Group on Periprosthetic Joint Infection (PJI).
Methods
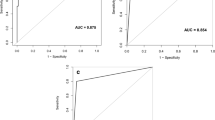
All patients who have undergone revision total knee arthroplasty (TKA) from September 2015 to July 2016 were included: 16 chronic (more than 3 months after performing arthroplasty) infections and 35 aseptic joints were identified. The diagnostic performance of single test was assessed by receiver operating characteristic (ROC) curve analyses. The sensitivity and specificity were calculated for each of the cut-off values and the area under the curve (AUC) was also calculated.
Results
The median synovial fluid (SF) leukocyte count, as well as the neutrophil percentage, was significantly higher in patients with PJI than in those with aseptic failure (p < 0.001). The sensitivity of α-defensin was 87.5% (95%; CI 74.6–94.7), the specificity was 97.1% (95% CI 86.9–99.7), the positive predictive value 93.3% (95% CI 81.8–98.1), and negative predictive value was 94.4% (95% CI 83.2–98.6). The results in terms of sensitivity and negative predictive value were greater than those of the other tests (cultures, synovial cell count, erythrocyte sedimentation rate, and C-reactive protein). The diagnostic accuracy of α-defensin, with an area under the curve of 0.92, was found to be higher than all the minor criteria for PJI.
Conclusions
In this study, the α-defensin lateral flow test was found to have the highest performance of all tests studied to identify PJI. Synovasure™ holds the potential to be included in the daily clinical practice.
Level of evidence
Level I diagnostic study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Periprosthetic joint infection (PJI) is one of the most serious complications after total knee arthroplasty (TKA). PJI can cause pain and extensive morbidity and imposes a major economic burden on healthcare systems [4, 21]. Although making an accurate and early diagnosis of PJI is essential for proper surgical decision-making, doing so still remains a challenge as there is no gold-standard test available for PJI. In an attempt to overcome this limitation, the Musculoskeletal Infectious Society (MSIS) proposed a multi-criteria definition of PJI based on a combination of clinical findings, laboratory tests, and tissue histology [25]. Even though these criteria, as modified during the International Consensus Meeting in 2013, provide a useful tool for retrospective diagnosis and research, the definition of PJI continues to be controversial [24].
In the last few years, the attention of diagnosticians of PJI has been focused on synovial fluid biomarkers, and in particular on α-defensin [11, 13, 16, 17, 19, 23]. This peptide is released in the synovial fluid by polymorphonuclear leukocytes in response to bacterial pathogens, and it is viewed as a promising biomarker of PJI [13, 22, 23]. Reports on the diagnostic accuracy of α-defensin measured in a laboratory setting with immunoassay of the synovial fluid suggest a high accuracy with a sensitivity ranging from 63 to 100% for diagnosing PJI [4, 16, 18, 23]. Recently, a new rapid test that can be used intra-operatively to detect the presence of α-defensin (Synovasure™, Zimmer, Warsaw, IN, USA) has been introduced. Thus far, only three clinical studies have reported the diagnostic value of this lateral flow assay, and their results should be corroborated by other clinical trials on selected case series of patients underwent knee or hip revision surgery [6, 20, 26].
For these reasons, this prospective study was undertaken to evaluate the diagnostic accuracy of the Synovasure α-defensin lateral flow assay to detect or exclude infection and to compare it to the sensitivity and specificity of other diagnostic criteria according to the International Consensus Group on PJI in a cohort of patients with failed total knee arthroplasty.
Materials and method
Data for all patients who have undergone TKA revision in two orthopaedic centres between September 2015 and July 2016 were analysed. All patients who presented with failed or painful joint arthroplasty underwent standardised diagnostic protocol to identify those with a PJI. The standard workup included clinical evaluation coupled with C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR); joint aspiration for white blood cell (WBC) count, percentage of polymorphonuclear leukocytes (PMN), and cultures. The diagnosis of chronic infection (> 90 days after the index procedure) was made based on International Consensus Group (ICM) definition of PJI [24]. Chronic inflammatory joint diseases (e.g. rheumatoid arthritis, psoriatic arthritis); acute (< 90 days after the index procedure) and late haematogenous (symptoms of less than 3 weeks duration) infections [9]; and an inadequate amount of synovial fluid (≤ 10 mL) for culture, WBC, and PMN (neutrophil) percentage determinations were considered as exclusion criteria. Patients included in the study had to withdraw any antibiotic treatment at least 2 weeks before the diagnostic procedure.
For all of the subjects included in the study, we have collected the following data: demographics (sex and age), medical history, initial clinical presentation, laboratory investigations, and microbiological analysis. A preoperative joint aspiration was performed after a 2-week antibiotic-free period under sterile conditions. The synovial fluid (SF) aspirate was processed for a cell count and microbiological analysis to establish the diagnosis of PJI before the surgery. According to ICM PJI criteria, SF WBC values of more than 3000 cells/µL and a PMN percentage higher than 80% were classified as positive results.
The SF aspirate was transferred into two different vials: the one for the cell counts contained ethylenediaminetetraacetic acid (EDTA with either K2 or K3) and 4–5 mL of the aspirate was inoculated into aerobic and anaerobic blood culture bottles (Bact-Alert FA, FN; bioMerieux, Marcy l’Etoile, France) and incubated for 14 days. The PJI lateral flow tests were performed preoperatively or in the operating room during surgery by a trained operator. The intraoperative aspiration was performed after surgical incision but before capsulotomy to avoid any contamination with blood. Subsequently, synovial fluid was serially diluted in disposable tubes before the specimen was added to the premeasured dilution buffer. Finally, three drops of the diluted synovial fluid sample were applied to the Synovasure PJI testing cassette. Test results were available within 10 min. Results of the PJI lateral flow test were not used to make changes in the operative plan.
Additionally, at least five samples for periprosthetic tissue were also collected in different sterile universal receptacles in all patients for microbiological analysis. Tissue specimens were homogenised in 3 mL of brain–heart infusion broth (bioMerieux) for 1 min, and the homogenate was inoculated into aerobic and anaerobic blood culture bottles (Bact-Alert FA, FN; bioMerieux) and incubated at 37° for 14 days. The broth was then subcultured onto a blood agar plate and a chocolate agar plate and incubated under a CO2-enriched atmosphere for 7 days and onto a Schaedler agar plate incubated in an anaerobic atmosphere for 7 days as soon as it becomes cloudy or on the 14th day [5]. Ethical approval was obtained from the Internal Review Board (IRB) of Istituto Fiorentino di Cura e Assistenza, Florence, Italy, in accordance with the Declaration of Helsinki (ID 166bis).
Statistical analysis
Descriptive statistics were used for continuous variables, and proportions for categorical variables. Continuous variables were compared by the Mann–Whitney U test and categorical variables by Fisher’s exact test or Chi-squared test.
The sensitivity, specificity, positive predictive value, and negative predictive value of single diagnostic tests were calculated using 2 × 2 contingency tables with the International Consensus Group definition criteria of PJI as the diagnostic standard. Receiver operating characteristic (ROC) curves, which depict the relationship between true-positive results (sensitivity) and false-negative results (1—specificity), were constructed and areas under the ROC curves (AUC) were also assessed to better evaluate the diagnostic accuracy of a single test. An AUC of 1 represents an ideal test with 100% sensitivity and 100% specificity, whereas an area AUC < 0.5 indicates that the diagnostic test is less useful. A p value of < 0.05 was considered statistically significant.
Sample size was calculated based on a one-sample comparison of proportions. The reference proportion was the sensitivity value reported by Sigmund et al. of 69% [26]. An expected increment of 15% was compared to this value. With a value of alpha of 0.05 and a power of 0.8, the required sample size was of 47 patients. Considering a 0.35 ratio between PJI and aseptic loosening, the patients required in each group were 16 and 31, respectively.
SPSS Statistical software 21.0.0.1 (IBM Corp, Armonk, NY, USA) was used for the database construction and the statistical analysis.
Results
Fifty-one patients (45% men) with a median age of 63 (interquartile range, or IQR of 48–79) years were enrolled. The baseline demographic findings are reported in Table 1. On the basis of the criteria specified above, 16 knees were judged to be infected. The most common types of microorganism identified by positive cultures were coagulase-negative Staphylococci. One case was considered to be infected despite negative pre- and intra-operative cultures.
Table 2 provides a summary of the median and IQR of the preoperative ESR and CRP levels, WBC count and percentage of PMNs in the SF aspirated from both infected and non-infected knees. All values were significantly different between the two groups. A significant correlation between all diagnostic measures and PJI (p < 0.001) except for a single positive culture was retrieved (Table 3). The single positive culture was higher in patients with aseptic loosening of the TKA (11/35, 31.4%) than in those with septic TKA (3/16, 18.7%) but this finding was not statistically significant. Coagulase-negative Staphylococci were cultured in all cases without infection. In two of these patients, the single positive culture was associated with elevated serum CRP and ESR values, without any other diagnostic criteria of infection.
The PJI lateral flow test showed positive results in 15 patients and negative results in 36. When matching these data with the diagnosis based on ICM PJI criteria, the test correctly identified 14 of 16 patients with an infection and 34 of 35 aseptic revision patients. The test results were considered false positive in one case and false negative in two cases. The sensitivity, specificity, positive predictive value, and negative predictive value for all the diagnostic criteria including α-defensin test are shown in Table 4. The sensitivity of α-defensin was 87.5% (95%; CI 74.6–94.7), the specificity was 97.1% (95% CI 86.9–99.7), the positive predictive value 93.3% (95% CI 81.8–98.1), and negative predictive value was 94.4% (95% CI 83.2–98.6). The results in terms of sensitivity and negative predictive value were greater than those of the other tests (cultures, synovial cell count, erythrocyte sedimentation rate, and C-reactive protein) (Table 4). ROC curves obtained for each parameter are shown in Fig. 1.
Graph showing (*) receiver operating characteristic (ROC) curve and area under curve (AUC) for α-defensin (area under ROC curve = 0.92; 95% CI 0.82–1.0); (**) ROC curve and AUC for two positive periprosthetic cultures (area under ROC curve = 0.88; 95% CI 0.74–0.95); (***) ROC curve and AUC for neutrophil percentage (PMN% > 80%) (area under ROC curve = 0.86; 95% CI 0.73–0.99); (****) ROC curve and AUC for synovial fluid leukocyte count (WBC count > 3000/µL) (area under ROC curve = 0.83; 95% CI 0.69–0.97); (*****) ROC curve and AUC for increased inflammatory markers (ESR > 30 mm/h and CRP > 10 mg/L) (area under ROC curve = 0.82; 95% CI 0.68–0.95); (******) ROC curve and AUC for the presence of sinus tract communicating with the joint (area under ROC curve = 0.63; 95% CI 0.45–0.80); (*******) ROC curve and AUC for single positive culture (area under ROC curve = 0.47; 95% CI 0.27–0.70)
Discussion
The most important finding of this present study was the highest performance of α-defensin lateral flow assay of all ICM criteria in the diagnosis of chronic knee prosthetic infections.
Although a definite preoperative diagnosis of septic failure of a TKA is imperative for proper treatment and management, the diagnosis of PJI remains clinically challenging. Preoperative aspiration with fluid analysis represents the best diagnostic tool because it is rapid and inexpensive, and does not require specialised equipment [1, 3]. Recently, however, the use of synovial fluid biomarkers such as α-defensin has been proposed with promising results [12,13,14,15, 23]. This study evaluated the diagnostic accuracy of a novel α-defensin lateral flow assay (Synovasure) in the diagnosis of knee periprosthetic joint infection using the PJI definition revised by the International Consensus Group. It was then compared with other currently available clinical tests, specifically, cell count, culture, ESR, and CRP. The results of the Synovasure assay reported in this study had excellent sensitivity and specificity and were consistent with previously reported data [6, 20, 26]. At 87.5 and 97.1%, respectively, the sensitivity and specificity of these results were higher than those reported in previous studies that used the Synovasure PJI Lateral Flow Test Kit [20, 26], except for sensitivity reported by Berger et al. [6].
In addition, the sensitivity, specificity and diagnostic accuracy of the Synovasure test, which is a qualitative assessment of α-defensin, are comparable with the quantitative enzyme-linked immunosorbent assay (ELISA) assessment of α-defensin [7, 8, 12,13,14,15, 17]. We reported only one false-positive test, which occurred in a 65-year-old woman with two positive minor criteria (increased inflammatory markers and increased WBC count in synovial fluid) who underwent one stage revision arthroplasty. Pre- and intra-operative cultures were all negative and the patient did not show any signs or symptoms of infection at 15-month follow-up. False-positive results were also reported in previous studies [6,7,8, 13, 17]. Bingham et al. [7] reported on two patients with false-positive results. In those patients, other markers of inflammation such as CRP, cell count, and ESR were elevated as well. They theorised that aseptic inflammation might be responsible for elevated α-defensin levels. A possible interpretation of these data could be that in cases of elevated synovial α-defensin levels and less than three minor criteria according to the ICM PJI criteria, the presence of possible metal debris should be considered. Two false-negative results are also reported. These patients were considered infected because of two positive cultures (Staphylococcus epidermidis in one case and Staphylococcus aureus in the other). As in the current series, Deirmengian et al. [13] and Bonananzinga et al. [8] also reported only one false-negative result. In both series, the cultures were negative but the diagnosis was done by matching other ICM PJI criteria. In the series of Frangiamore et al. [17], there was one false-negative result in a subject who had a positive culture that was considered to be due to contamination.
In addition, because of the higher diagnostic accuracy of the α-defensin lateral flow assay with respect to other diagnostic tests (clinical signs, inflammatory markers, synovial fluid WBC count and differential), the Synovasure test provides additional data to the ICM PJI criteria. Synovasure has the additional advantage over other tests that it gives a rapid result (10 min). This conclusion is in contrast to that of Sigmund et al. [26], who reported a lower diagnostic accuracy for the α-defensin test than for frozen section, bacteriology with at least two positive cultures, sonication cultures, and serum CRP levels. However, our relatively small sample may overestimate the accuracy of the test, so further studies are needed to evaluate the performance of Synovasure and its role in the diagnosis of infected arthroplasty.
Moreover, in our study, the presence of a sinus tract, even if is considered pathognomonic for PJI, reported worse AUC result as compared with two positive cultures, WBC count, neutrophil percentage, or increased inflammatory markers. This may be explained by the fact that this major criterion has correctly detected all non-infected patients (100% specificity) but it showed less capacity to identify patients with PJI (25% of sensitivity).
Therefore, because of these false-negative results, the absence of these criteria does not rule out infection.
Finally, this study presents several limitations. First, subjects with inflammatory joint disease, who are known to be associated with high inflammatory markers (ESR, CRP) as well as synovial fluid leukocyte count and neutrophil percentage, were not included. Also, patients with acute or haematogenous infections in which cut-off values of diagnostic criteria are quite different with respect to chronic infections were excluded. Second, the analysed data were from only a small group of patients compared with other studies on PJI diagnosis and α-defensin assays [2, 8, 10]. However, at present, this is still the largest study available in the literature on painful TKA prosthesis using this novel assay. Synovasure™ holds the potential to be included as a diagnostic criterion in the daily clinical practice.
Conclusion
In conclusion, the findings of this study suggest that the α-defensin lateral flow test can play a role in the diagnosis of PJI. The use of the Synovasure test was found to be a useful addition to the diagnosis of these infections and decision making during treatment of painful TKA.
References
Ahmad SS, Shaker A, Saffarini M, Chen AF, Hirschmann MT, Kohl S (2016) Accuracy of diagnostic tests for prosthetic joint infection: a systematic review. Knee Surg Sports Traumatol Arthrosc 24:3064–3074
Alijanipour P, Bakhshi H, Parvizi J (2013) Diagnosis of Periprosthetic Joint Infection: The Threshold for Serological Markers. Clin Orthop Relat Res 471:3186–3195
Ascione T, Pagliano P, Balato G, Mariconda M, Rotondo R, Esposito S (2016) Oral therapy, microbiological findings, and comorbidity influence the outcome of prosthetic joint infections undergoing 2-stage exchange. J Arthroplast. doi: 10.1016/j.arth.2017.02.057
Ascione T, Pagliano P, Mariconda M, Rotondo R, Balato G, Toro A, Barletta V, Conte M, Esposito S (2015) Factors related to outcome of early and delayed prosthetic joint infections. J Infect 70:30–36
Bémer P, Léger J, Tandé D, Plouzeau C, Valentin AS, Jolivet-Gougeon A, Lemarié C, Kempf M, Héry-Arnaud G, Bret L, Juvin ME, Giraudeau B, Corvec S, Burucoa C (2016) How many samples and how many culture media to diagnose a prosthetic joint infection: a clinical and microbiological prospective multicenter study. J Clin Microbiol 54:385–391
Berger P, Van Cauter M, Driesen R, Neyt J, Cornu O, Bellemans J (2017) Diagnosis of prosthetic joint infection with alpha-defensin using a lateral flow device: a multicentre study. B Jt J 99:1176–1182
Bingham J, Clarke H, Spangehl M, Schwartz A, Beauchamp C, Goldberg B (2014) The alpha defensin-1 biomarker assay can be used to evaluate the potentially infected total joint arthroplasty. Clin Orthop Relat Res 472:4006–4009
Bonanzinga T, Zahar A, Dütsch M, Lausmann C, Kendoff D, Gehrke T (2017) How reliable is the alpha-defensin immunoassay test for diagnosing periprosthetic joint infection? A prospective study. Clin Orthop Relat Res 475:408–415
Cats-Baril W, Gehrke T, Huff K, Kendoff D, Maltenfort M, Parvizi J (2013) International consensus on periprosthetic joint infection: description of the consensus process. Clin Orthop Relat Res 471:4065–4075
Costa CR, Johnson AJ, Naziri Q, Maralunda GA, Delanois RE, Mont MA (2012) Efficacy of erythrocyte sedimentation rate and C-reactive protein level in determining periprosthetic hip infections. Am J Orthop (Belle Mead NJ) 41:160–165
Deirmengian C, Hallab N, Tarabishy A, Della Valle C, Jacobs JJ, Lonner J, Booth RE (2010) Synovial fluid biomarkers for periprosthetic infection. Clin Orthop Relat Res 468:2017–2023
Deirmengian C, Kardos K, Kilmartin P, Cameron A, Schiller K, Booth RE, Parvizi J (2015) The alpha-defensin test for periprosthetic joint infection outperforms the leukocyte esterase test strip. Clin Orthop Relat Res 473:198–203
Deirmengian C, Kardos K, Kilmartin P, Cameron A, Schiller K, Parvizi J (2014) Combined measurement of synovial fluid α-defensin and C-reactive protein levels: highly accurate for diagnosing periprosthetic joint infection. J B Jt Surg Am 96:1439–1445
Deirmengian C, Kardos K, Kilmartin P, Cameron A, Schiller K, Parvizi J (2014) Diagnosing periprosthetic joint infection: has the era of the biomarker arrived? Clin Orthop Relat Res 472:3254–3262
Deirmengian C, Kardos K, Kilmartin P, Gulati S, Citrano P, Booth RE (2015) The alpha-defensin test for periprosthetic joint infection responds to a wide spectrum of organisms. Clin Orthop Relat Res 473:2229–2235
Deirmengian C, Lonner JH, Booth RE (2005) the mark coventry award: white blood cell gene expression. Clin Orthop Relat Res 440:38–44
Frangiamore SJ, Gajewski ND, Saleh A, Farias-Kovac M, Barsoum WK, Higuera CA (2016) α-Defensin accuracy to diagnose periprosthetic joint infection—best available test? J Arthroplast 31:456–460
Frangiamore SJ, Saleh A, Grosso MJ, Kovac MF, Higuera CA, Iannotti JP, Ricchetti ET (2015) α-Defensin as a predictor of periprosthetic shoulder infection. J Shoulder Elb Surg 24:1021–1027
Jacovides CL, Parvizi J, Adeli B, Jung KA (2011) Molecular markers for diagnosis of periprosthetic joint infection. J Arthroplast 26:99–103.e1
Kasparek MF, Kasparek M, Boettner F, Faschingbauer M, Hahne J, Dominkus M (2016) Intraoperative diagnosis of periprosthetic joint infection using a novel alpha-defensin lateral flow assay. J Arthroplast 31:2871–2874
Kurtz SM, Lau E, Watson H, Schmier JK, Parvizi J (2012) Economic burden of periprosthetic joint infection in the United States. J Arthroplast 27:61–65 (e1)
Lehrer RI, Ganz T (1992) Defensins: endogenous antibiotic peptides from human leukocytes. Ciba Found Symp 171:276-290 (293)
Li B, Chen F, Liu Y, Xu G (2017) Synovial fluid α-defensin as a biomarker for peri-prosthetic joint infection: a systematic review and meta-analysis. Surg Infect 18:702–710
Parvizi J, Gehrke T (2014) Definition of periprosthetic joint infection. J Arthroplast 29:1331
Parvizi J, Zmistowski B, Berbari EF, Bauer TW, Springer BD, Della Valle CJ, Garvin KL, Mont MA, Wongworawat MD, Zalavras CG (2011) New definition for periprosthetic joint infection: from the workgroup of the Musculoskeletal Infection Society. Clin Orthop Relat Res 469:2992
Sigmund IK, Holinka J, Gamper J, Staats K, Böhler C, Kubista B, Windhager R (2017) Qualitative α-defensin test (Synovasure) for the diagnosis of periprosthetic infection in revision total joint arthroplasty. B Jt J 99:66–72
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding:
No funding was received for this study.
Research ethics committee:
This study is compliant with the Helsinki Declaration and ethically correct, therefore, is approved by the scientific revision’s internal committee of the IFCA Clinic-Florence.
Device status/drug statement:
The device(s)/drug(s) is/are FDA approved or approved by corresponding national agency for this indication.
Rights and permissions
About this article
Cite this article
Balato, G., Franceschini, V., Ascione, T. et al. High performance of α-defensin lateral flow assay (Synovasure) in the diagnosis of chronic knee prosthetic infections. Knee Surg Sports Traumatol Arthrosc 26, 1717–1722 (2018). https://doi.org/10.1007/s00167-017-4745-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4745-x