Abstract
Purpose
To investigate whether cartilage thickness in the lateral femoral posterior condyle affects the femoral rotation angles on navigation and clinical outcomes of navigation-assisted total knee arthroplasty (TKA).
Methods
This is a prospective randomized study of navigation-assisted TKA. Fifty cases underwent TKA without removal of the lateral posterior femoral cartilage (Group 1), and 56 cases underwent TKA with removal of the lateral posterior femoral cartilage (Group 2). The femoral rotation was evaluated using CT and compared with navigation values. The angle between the clinical transepicondylar axis and posterior condylar axis measured on CT was defined as the femoral rotation angle on CT. Elevation of the joint line and patellar measurements were also evaluated.
Results
The clinical outcomes were not statistically different in the two groups. The radiographic measurements were not statistically different except femoral rotation angle on navigation. The mean femoral rotation angle of navigation was 4.0° ± 2.2° without cartilage removal and 5.1° ± 2.5° with cartilage removal. The reliability and validity were high between the femoral rotation angle on navigation in the cartilage removal group and that on CT, but there were no differences in clinical outcomes between the two groups.
Conclusion
There was little effect of navigation-assisted TKA on radiographic and clinical outcomes, although femoral rotational differences were caused by the lateral femoral posterior condylar cartilage. Although the rotational differences due to cartilage would be within the clinical safety margin, surgeons should consider that difference during TKA.
Level of evidence
Lower quality randomized trial (no masking), Level II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rotational alignment of the femoral component in total knee arthroplasty (TKA) affects patellofemoral and tibiofemoral knee kinematics [6, 18,19,20, 23]. Femoral component mal-rotation is a common cause of pain after TKA and negatively affects clinical outcome [3, 6, 17,18,19, 22, 23, 32]. For that reason, many methods have been developed to measure femoral component rotation. Traditional methods for determining the proper rotational alignment of the femoral component in TKA include the Whiteside line [43], surgical or clinical transepicondylar axis [28, 36, 44, 45], 3° external rotation of the posterior femoral condyles [26], and the gap balancing technique [37]. However, controversies remain over which axis should be used to determine the correct rotational alignment of TKA. To establish the precise femoral component rotation on an individual basis, some surgeons advocated preoperative TKA planning on computerized tomography (CT) [1, 2, 4, 39,40,41] or MRI [12, 29, 38].
Recently, navigation-assisted systems have been developed and showed more precise alignment of the components in comparison with conventional methods [7, 8, 44]. With regard to femoral component rotation, controversies remain on whether navigation systems are a more reliable tool to establish precise femoral rotational alignment compared to conventional techniques [24, 30, 44].
In addition to these problems of practical implementation, there is still lack of consensus concerning the correct component rotation; therefore, many methods have been used to determine the preoperative femoral component rotation, although each of them has limitations. In CT, there could be errors because it could not detect the cartilage status on posterior femoral condyles [4, 38]. MRI could be used to evaluate the cartilage of posterior femoral condyles, but this has not yet been fully validated and is difficult to perform preoperatively for TKA due to cost [12, 29, 35, 38]. If navigation-assisted TKAs were performed, the instrument for identifying the anatomical landmark would be placed on the cartilage of the posterior femoral condyles, which could affect the femoral component rotation angle for cartilage that is or is not intact. A number of studies have evaluated the differences of rotation angle with or without cartilage in the radiologic point of view [1, 2, 12, 33, 40], but few comparisons have been made of a navigation-assisted measured resection in TKA before and after removal of femoral cartilage in the surgical field [13].
The purpose of this study is to investigate whether differences in cartilage thickness on lateral femoral posterior condyles affect the femoral component rotation angle measured in a navigation system and the femoral rotational angles in navigation before and after removing the lateral femoral posterior cartilage would be validated with CT-measured rotational angle. It is hypothesized that the clinical and radiologic outcomes would be affected if the cartilage thickness causes differences in femoral component rotation especially when using the navigation system, and that the femoral component rotation angle in navigation after removing the remnant cartilage would be validated with CT-measured rotation angle.
Materials and methods
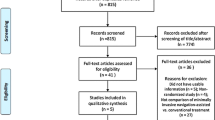
This is a prospective randomized study of patients who underwent navigation-assisted TKA with a minimum of 5 years of follow-up. A total of 145 patients who underwent primary fixed bearing posterior stabilized (PS) TKA (Aesculap, Tuttlingen, Germany) using the OrthoPilot navigation system were enrolled in this study. The inclusion criteria were osteoarthritis (OA) cases with varus only. The varus/valgus alignment was assessed by the mechanical axes of the femur and tibia in an entire standing leg radiograph. The exclusion criteria were as follows: valgus knees, previous surgery history, bony defects, a flexion contracture greater than 30°, or cases in which femoral epicondyles could not be precisely visualized on the CT images due to spurs or deformities. Cases with no relatively intact lateral femoral posterior cartilage intraoperatively (over ICRS gr 2) were also excluded to reduce bias. Thirty-nine cases were excluded on the basis of the exclusion criteria because these factors can interfere with the results of navigation-assisted TKAs.
After applying the exclusion criteria, 106 cases were enrolled in this study. In all cases, the femoral component rotation angle was measured by a navigation system without removal of lateral posterior femoral cartilage and then again after removal of lateral posterior femoral cartilage. After measurement of femoral component rotation with or without removal of cartilage, the patients were divided into two groups randomly with a computer-generated random number table. Among them, 50 cases were underwent TKA using the femoral component rotation angle without removal of the lateral posterior femoral cartilage (Group 1), and 56 cases underwent TKA using the femoral component rotation angle with removal of the lateral posterior femoral cartilage (Group 2) (Fig. 1). Patient demographics are summarized in Table 1.
To compare the outcomes of the two groups, serial postoperative evaluations were performed at 1, 3, 6 and 12 months and every 12 months thereafter. Preoperative and postoperative scores were obtained using the Knee Society knee and functional Score (KSS), Hospital for Special Surgery (HSS) scores, Western Ontario and McMaster Universities (WOMAC) scores, and the patellofemoral (PF) scoring system of Feller et al. [10] Because inadequate femoral component rotation could influence patellar alignment and induce anterior knee pain, patella-associated pain score was also compared between the groups.
Radiographic analysis
Preoperative radiographic measurements of femoral rotation were performed using CT with 1.2-mm-thick sections. The distal femoral scan was performed perpendicularly to the anatomical axis of the femur in 30° flexion position. The transverse images through the most prominent points of the medial and lateral femoral epicondyles were used for the measurements. The transepicondylar axis (TEA) was defined as a line connecting the most prominent points of the medial epicondyle and the lateral epicondyle. The posterior condylar axis (PCA) was defined as a line connecting the most prominent points of the medial and lateral femoral posterior condyles [24]. The angle between the two axes measured on the CT images was defined as the preoperative femoral rotation angle on CT (TEA-PCA) and was compared with the femoral rotation angle determined on navigation with or without cartilage removal (Fig. 2).
Intraoperatively, the angles of femoral rotation were recorded by the navigation system based on the registered anatomical data, without and with removal of lateral posterior femoral condylar cartilage (Fig. 3). The posterior femoral cartilage was removed to the subchondral bone.
Postoperative evaluation of the femoral component rotation was performed using postoperative CT images evaluated in the same way as preoperative measurement.
The measurements of joint line elevation [27], patellar tilt angle, and patellar height were performed using postoperative plain radiograph to evaluate patellar alignment. The joint line level was defined as the distance from the distal femoral condyle to the tibial tuberosity in the lateral radiographs [27].
All measurements were performed on a PACS (Picture Archiving and Communications System; General Electric, Chicago, IL, USA).
Surgical technique
A conventional medial parapatellar approach was performed with sacrifice of posterior cruciate ligaments [25]. Coronal alignment was accepted within 0°–2° of varus after the tracker pin was established and initial soft tissue release. After the distal femoral and proximal tibia bones were cut, a clinical TEA line was set on the cut surface, and the anteroposterior (AP) axis was drawn perpendicular to the TEA in order to position the probe in the same location when recoding the anatomical position [28]. The femoral rotational angle measured in this navigation system was the angle between the anteroposterior (AP) axis and PCA [2, 12, 33, 40]. At this step, to evaluate the effect of lateral femoral posterior cartilage, the femoral component rotational angle in navigation was recorded two times, with and without removal of lateral femoral posterior cartilage, by positioning the probe in the same anatomical location. These angles were compared with the rotation angle of preoperative CT. After recording, the femoral component rotation angle was randomly set to that measured in group 1 without posterior condyle cartilage removal or to that in group with posterior condyle cartilage removal. After all bone cutting was performed, the prostheses were implanted with cement.
The study was approved by the Institutional Review Boards of Chung-Ang University Hospital [ID: C2013213(1173)] and was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki.
Statistical analysis
Statistical analyses were conducted using SPSS for Windows version 19.0 (SPSS, Chicago, IL, USA) and G*power analysis (ver 3.1.5).
The mean angles or the rates between the groups were compared using an independent paired t test, Mann–Whitney test, or Chi-square analysis. The correlations between the preoperative femoral rotation angles on CT and navigation in each group were analysed using Pearson’s correlation coefficient. The strength of correlation was indicated by the correlation coefficient (r) as strong (>0.75), moderate (0.40–0.75), or weak (<0.40). Reliability was established using intraclass correlations (ICCs) with a two-way random effect model, in which absolute agreement, average measurement, and validity were established by calculating the standard error of measurement (SEM) and 95% confidence interval (95% CI of SEM = 1.96*SEM) with the Pearson correlation coefficient value [14, 42]. Additionally, Bland–Altman plots and 95% limits of agreement (95% LOA) were used to assess the agreement between the navigation value and preoperative CT value [5]. The Shapiro–Wilks test was used to confirm that the measured data followed a normal distribution at a 0.05 level of significance, and an ICC of 0.70 was selected as the minimally acceptable value for reliability [34, 42].
Test–retest was performed by two orthopedic surgeons 2 weeks from the first radiological measurement. However, the intraoperative navigation measurements were performed two times by the senior surgeon only at the same time due to the patient’s safety. The intra- and interobserver reliability values were also calculated using the intraclass correlation coefficient (ICC).
The primary outcome measure of the study was to find the differences of the mean femoral rotation angles calculated by the navigation system before and after removal of the lateral femoral cartilage. Because there were no previous reports on the femoral rotation angles in navigation according to cartilage removal, a pilot study was performed. The patients in the pilot study were not enrolled in the main study. An allocation ratio was set at 1:1, and a sample size calculation was based on a pilot study of 22 patients in each group. The mean and standard deviation in the pilot study was 3.2° ± 1.9° in the without cartilage removal group and 4.6° ± 2.6° in the cartilage removal group. A two-sided α error of 5% and β error of 20% was accepted to detect any significant difference. Based on these calculations, the required study size was 42 in each group.
Results
Differences between the femoral rotation angle of navigation and preoperative CT
The differences between the navigation value and preoperative CT value are summarized in Table 2. There were statistical differences between the angle without cartilage removal and preoperative CT (p = 0.003), but no differences were found between the angle with cartilage removal and preoperative CT (p = 0.094). Removal of the lateral femoral posterior cartilage increased the TEA-PCA angle by 1.4°. Moreover, the correlation coefficients between navigation and preoperative CT values were found to be moderate to strong, although stronger correlation was found in the angle with cartilage removal (Table 2).
Reliability and validity, which were determined by the SEM and 95% LOA in Bland–Altman plots, and the minimum value to detect true differences between the navigation value and preoperative CT value are summarized in Table 3 (Fig. 4a, b).
Clinical and radiologic findings
The clinical and radiological outcomes between group 1 and 2 were not statistically different in all measurements after 5-year follow-up except the intraoperative navigation value (Tables 4, 5). Even though randomization was performed intraoperatively, the pre- and postoperative TEA-PCA angles on CT were not statistically different between the two groups. Only the selected femoral rotation angle on navigation was statistically different due to randomization (4.0° in group 1; 5.1° in group 2; p = 0.018). In terms of patellofemoral evaluation, there were no significant differences in pain or function (Tables 4, 5).
The intra- and interobserver reliability values by ICC were found to range from 0.723 to 0.932 in radiologic measurements. The interobserver reliability by ICC was lowest value for the measurement of femoral rotation angle in preoperative CT.
Discussion
The most important finding was that the thickness of the lateral posterior femoral condylar cartilage could affect the angle of femoral component rotation in navigation-assisted TKAs; however, when considered together with the clinical and radiologic outcomes, the differences of rotation alignment according to lateral posterior femoral condylar cartilage did not significantly affect clinical outcomes. In addition, the preoperative femoral rotation angles on CT (TEA-PCA) were validated with the femoral rotation angles with removal of lateral femoral posterior cartilage on navigation.
Although the importance of proper alignment in TKA surgery is recognized, determination of rotational alignment is controversial compared to determination of axial alignment. Many surgeons use the posterior femoral condyles as anatomical landmarks, and many navigation systems use the same anatomical references in order to produce the rectangular flexion gap [1, 20, 21, 33, 40]. However, an articular cartilage defect localized only in one compartment might produce an inaccurate femoral angle [38]. The mal-rotated femoral component theoretically causes increased polyethylene wear, particularly in early flexion [3, 6, 17, 18, 23], but the safety range of the rotation angles without mechanical problems has not yet been defined. Recent studies indicated that a change of 2°–3° in alignment during knee flexion or a change of 2–3 mm in bone cut on the posterior femoral condyle can make a difference in the ligament balance and clinical functional outcome, and the remnant cartilage of the posterior femoral condyle could contribute to those differences [4, 15, 31, 38].
In this study, the rotation angle was also influenced an average of 1.4° after removal of the remnant cartilage of the lateral femoral condyle. This result means that if the femoral component in the navigation system is set referencing the PCA after cartilage removal, the femoral component is positioned with an external rotation of approximately 1.4° compared with the position without cartilage removal. The external rotation of 1.4° in this study was consistent with previous studies although somewhat smaller. Tashiro et al. [38] reported that the femoral component can be implanted with more than 2° of external rotation if the difference in cartilage thickness between the two posterior condyles is not considered. Asada et al. [4] reported that the remnant cartilage of the posterior femoral condyle could affect the femoral component rotation, although the difference due to cartilage remnants was small and within the safety margin of 2° external rotation [31]. After removal of the remnant cartilage, the angles recorded in navigation showed stronger correlation to the value of the preoperative femoral rotation on CT even though both groups showed strong correlation. However, the SEM value was similar regardless of lateral femoral posterior cartilage removal. The 95% CI for SEM revealed that the ranges of both groups were acceptable with regard to the preoperative CT value, although the range of the 95% CI in the cartilage removal group seemed to be more acceptable. The Bland–Altman plots and 95% LOA also revealed that both groups were acceptable, and the range of 95% LOA with cartilage removal seemed also to be more acceptable than that of without cartilage removal. The reason for that tendency could be that the angle from CT was obtained from the bony landmark, not from the cartilage tissue. The preoperative femoral rotation angles on CT could serve as a supplementary guide for preoperative planning of TKA with regard to femoral rotation, especially in navigation measurements.
To analyse whether different implantation of femoral component rotation could affect the patellofemoral alignment, patella measurements were evaluated. The mean values of each of the patella parameters and clinical outcomes were not statistically different in the two groups. This also means that different implantation of femoral component rotation could occur after remnant cartilage removal, but does not affect postoperative outcomes. The acceptable postoperative patellofemoral alignment and clinical outcomes in the two groups provided additional evidence that the differences in rotational angle are within a safe range.
The results of this study revealed that the change of rotation alignment according to lateral posterior femoral condylar cartilage did not influence clinical outcome in patients undergoing TKA. To the best of our knowledge, this is the first study that investigated the influence of lateral posterior femoral condylar cartilage thickness on clinical outcomes in terms of tibiofemoral joint and patellofemoral joint. The measurements of femoral component angle on navigation could be affected by the remnant cartilage of the lateral posterior femoral condyle, but there were no effects on the clinical outcomes or radiologic evaluation after 5 years of follow-up. Although the rotation angle on navigation with removal of the lateral posterior femoral cartilage seemed more reliable and validated to the preoperative CT value, it could not be proven what the angle would be more appropriate because of the similar clinical outcomes were found between groups. These findings do not support our hypothesis that a difference in the femoral component rotation according to cartilage thickness can affect clinical outcomes. A recent editorial paper indicated that a change of 2°–3° in alignment during knee flexion or a change of 2–3 mm in bone cut on the posterior femoral condyle can make a difference in the ligament balance and clinical functional outcome [15]. This review was not consistent with the result of this study, possibly because that paper discussed the results of PCL balancing and so is more applicable to cruciate-retaining TKA. However, in this study, all of the cases were performed using fixed bearing PS TKA prosthesis; thus, the change of rotational alignment based on lateral posterior femoral cartilage status without deformity might be too small to affect clinical and radiologic outcomes.
The current study had some limitations. First, there could be differences in the patients with more advanced degenerative change in the lateral femoral posterior condyle, including severe varus/valgus patients. Second, the patients were limited to Koreans; therefore, even though the findings were statistically meaningful, there might be anatomic differences compared to the Caucasian population because of different life styles. For this reason, the results of this study should be interpreted with caution. Third, the follow-up period was relatively short to evaluate the survival rate and wear, and more long-term follow-up will be needed. Fourth, there could be bias in measuring the femoral component rotation angle with 2D-CT, although this conclusion is uncertain [9, 11, 16, 25]. Further study with 3D-CT scan is needed to precisely evaluate the femoral rotation using navigation measurements. Finally, it is difficult to determine how much cartilage should be removed; due to individual differences, there could be errors in the removal procedure. However, one surgeon performed all TKAs using the same technique, allowing us to isolate the attributes of the procedure.
The results of this study revealed that remnant cartilage of the lateral posterior femoral condyle would not affect the clinical outcome of primary TKA. Thus, the decision on femoral component rotation should be made considering other factors, such as flexion gap, regardless of remnant cartilage of the lateral posterior femoral condyle.
Conclusion
In conclusion, there was little effect of femoral component rotational differences on radiologic alignment or clinical outcomes in navigation-assisted TKA with regard to cartilage remnants of the lateral posterior femoral condyle. Whether using navigation or not, the rotational differences caused by lateral femoral cartilage would be within a safe margin, although surgeons should consider the results of this study when determining femoral rotation using navigation or CT.
References
Akagi M, Matsusue Y, Mata T, Asada Y, Horiguchi M, Iida H et al (1999) Effect of rotational alignment on patellar tracking in total knee arthroplasty. Clin Orthop Relat Res 366:155–163
Akagi M, Yamashita E, Nakagawa T, Asano T, Nakamura T (2001) Relationship between frontal knee alignment and reference axes in the distal femur. Clin Orthop Relat Res 388:147–156
Armstrong AD, Brien HJ, Dunning CE, King GJ, Johnson JA, Chess DG (2003) Patellar position after total knee arthroplasty: influence of femoral component malposition. J Arthroplasty 18:458–465
Asada S, Akagi M, Matsushita T, Hashimoto K, Mori S, Hamanishi C (2012) Effects of cartilage remnants of the posterior femoral condyles on femoral component rotation in varus knee osteoarthritis. Knee 19:185–189
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1:307–310
Boldt JG, Stiehl JB, Hodler J, Zanetti M, Munzinger U (2006) Femoral component rotation and arthrofibrosis following mobile-bearing total knee arthroplasty. Int Orthop 30:420–425
Bolognesi M, Hofmann A (2005) Computer navigation versus standard instrumentation for TKA: a single-surgeon experience. Clin Orthop Relat Res 440:162–169
Chauhan SK, Clark GW, Lloyd S, Scott RG, Breidahl W, Sikorski JM (2004) Computer-assisted total knee replacement. A controlled cadaver study using a multi-parameter quantitative CT assessment of alignment (the perth CT protocol). J Bone Jt Surg Br 86:818–823
De Valk EJ, Noorduyn JC, Mutsaerts EL (2016) How to assess femoral and tibial component rotation after total knee arthroplasty with computed tomography: a systematic review. Knee Surg Sports Traumatol Arthrosc 24:3517–3528
Feller JA, Bartlett RJ, Lang DM (1996) Patellar resurfacing versus retention in total knee arthroplasty. J Bone Jt Surg Br 78:226–228
Figueroa J, Guarachi JP, Matas J, Arnander M, Orrego M (2016) Is computed tomography an accurate and reliable method for measuring total knee arthroplasty component rotation? Int Orthop 40:709–714
Griffin FM, Insall JN, Scuderi GR (2000) Accuracy of soft tissue balancing in total knee arthroplasty. J Arthroplasty 15:970–973
Hamada D, Wada K, Mikami H, Toki S, Goto T, Tsutsui T et al (2017) The posterior condylar cartilage affects rotational alignment of the femoral component in varus knee osteoarthritis. J Med Invest 64:24–29
Harvill LM (1991) Standard error of measurement. Educ Meas Issues Pract 10:33–41
Heesterbeek PJ, Wymenga AB (2010) PCL balancing, an example of the need to couple detailed biomechanical parameters with clinical functional outcome. Knee Surg Sports Traumatol Arthrosc 18:1301–1303
Hirschmann MT, Konala P, Amsler F, Iranpour F, Friederich NF, Cobb JP (2011) The position and orientation of total knee replacement components: a comparison of conventional radiographs, transverse 2D-CT slices and 3D-CT reconstruction. J Bone Jt Surg Br 93:629–633
Hofmann S, Romero J, Roth-Schiffl E, Albrecht T (2003) Rotational malalignment of the components may cause chronic pain or early failure in total knee arthroplasty. Orthopade 32:469–476
Incavo SJ, Wild JJ, Coughlin KM, Beynnon BD (2007) Early revision for component malrotation in total knee arthroplasty. Clin Orthop Relat Res 458:131–136
Jacobsen K (2009) Stress radiographical measurement of the anteroposterior, medial and lateral stability of the knee joint. Acta Orthop Scand 47:335–344
James EW, Williams BT, LaPrade RF (2014) Stress radiography for the diagnosis of knee ligament injuries: a systematic review. Clin Orthop Relat Res 472:2644–2657
Jung TM, Reinhardt C, Scheffler SU, Weiler A (2006) Stress radiography to measure posterior cruciate ligament insufficiency: a comparison of five different techniques. Knee Surg Sports Traumatol Arthrosc 14:1116–1121
Keshmiri A, Maderbacher G, Baier C, Zeman F, Grifka J, Springorum HR (2016) Significant influence of rotational limb alignment parameters on patellar kinematics: an in vitro study. Knee Surg Sports Traumatol Arthrosc 24:2407–2414
Kessler O, Patil S, Colwell CW Jr, D’Lima DD (2008) The effect of femoral component malrotation on patellar biomechanics. J Biomech 41:3332–3339
Kim YH, Kim JS, Yoon SH (2007) Alignment and orientation of the components in total knee replacement with and without navigation support: a prospective, randomised study. J Bone Jt Surg Br 89:471–476
Konigsberg B, Hess R, Hartman C, Smith L, Garvin KL (2014) Inter- and intraobserver reliability of two-dimensional CT scan for total knee arthroplasty component malrotation. Clin Orthop Relat Res 472:212–217
Laskin RS (1995) Flexion space configuration in total knee arthroplasty. J Arthroplasty 10:657–660
Lee HJ, Lee JS, Jung HJ, Song KS, Yang JJ, Park CW (2011) Comparison of joint line position changes after primary bilateral total knee arthroplasty performed using the navigation-assisted measured gap resection or gap balancing techniques. Knee Surg Sports Traumatol Arthrosc 19:2027–2032
Lee JK, Lee S, Chun SH, Kim KT, Lee MC (2017) Rotational alignment of femoral component with different methods in total knee arthroplasty: a randomized, controlled trial. BMC Musculoskelet Disord 18:217
Matziolis D, Meiser M, Sieber N, Teichgraber U, Matziolis G (2017) Posterior cortical axis: a new landmark to control femoral component rotation in total knee arthroplasty. Orthopedics 40:188–190
Matziolis G, Krocker D, Weiss U, Tohtz S, Perka C (2007) A prospective, randomized study of computer-assisted and conventional total knee arthroplasty. Three-dimensional evaluation of implant alignment and rotation. J Bone Jt Surg Am 89:236–243
Miller MC, Berger RA, Petrella AJ, Karmas A, Rubash HE (2001) Optimizing femoral component rotation in total knee arthroplasty. Clin Orthop Relat Res 392:38–45
Nakahara H, Okazaki K, Hamai S, Okamoto S, Kuwashima U, Higaki H et al (2015) Does knee stability in the coronal plane in extension affect function and outcome after total knee arthroplasty? Knee Surg Sports Traumatol Arthrosc 23:1693–1698
Poilvache PL, Insall JN, Scuderi GR, Font-Rodriguez DE (1996) Rotational landmarks and sizing of the distal femur in total knee arthroplasty. Clin Orthop Relat Res 331:35–46
Shrout PE, Fleiss JL (1979) Intraclass correlations: uses in assessing rater reliability. Psychol Bull 86:420–428
Silva A, Pinto E, Sampaio R (2016) Rotational alignment in patient-specific instrumentation in TKA: MRI or CT? Knee Surg Sports Traumatol Arthrosc 24:3648–3652
Siston RA, Patel JJ, Goodman SB, Delp SL, Giori NJ (2005) The variability of femoral rotational alignment in total knee arthroplasty. J Bone Jt Surg Am 87:2276–2280
Stiehl JB, Cherveny PM (1996) Femoral rotational alignment using the tibial shaft axis in total knee arthroplasty. Clin Orthop Relat Res 331:47–55
Tashiro Y, Uemura M, Matsuda S, Okazaki K, Kawahara S, Hashizume M et al (2012) Articular cartilage of the posterior condyle can affect rotational alignment in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 20:1463–1469
Thienpont E, Schwab PE, Paternostre F, Koch P (2014) Rotational alignment of the distal femur: anthropometric measurements with CT-based patient-specific instruments planning show high variability of the posterior condylar angle. Knee Surg Sports Traumatol Arthrosc 22:2995–3002
Victor J (2009) Rotational alignment of the distal femur: a literature review. Orthop Traumatol Surg Res 95:365–372
Victor J, Van Doninck D, Labey L, Van Glabbeek F, Parizel P, Bellemans J (2009) A common reference frame for describing rotation of the distal femur: a ct-based kinematic study using cadavers. J Bone Jt Surg Br 91:683–690
Weir JP (2005) Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. J Strength Cond Res 19:231–240
Whiteside LA, Arima J (1995) The anteroposterior axis for femoral rotational alignment in valgus total knee arthroplasty. Clin Orthop Relat Res 321:168–172
Yang JH, Dahuja A, Kim JK, Yun SH, Yoon JR (2016) Alignment in knee flexion position during navigation-assisted total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 24:2422–2429
Yoshino N, Takai S, Ohtsuki Y, Hirasawa Y (2001) Computed tomography measurement of the surgical and clinical transepicondylar axis of the distal femur in osteoarthritic knees. J Arthroplasty 16:493–497
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
There is no funding source.
Ethical approval
The study was approved by the Institutional Review Boards of Chung-Ang University Hospital (No.: C2013213(1173)) and was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki.
Rights and permissions
About this article
Cite this article
Kim, S.H., Park, YB., Ham, D.W. et al. No influence of femoral component rotation by the lateral femoral posterior condylar cartilage remnant technique on clinical outcomes in navigation-assisted TKA. Knee Surg Sports Traumatol Arthrosc 25, 3576–3584 (2017). https://doi.org/10.1007/s00167-017-4662-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4662-z