Abstract
Purpose
Increasing importance has been placed on the posterolateral corner (PLC) in maintaining varus and rotational stability of the knee. The goal of this study was to evaluate knee function and clinical stability following a single-graft PLC reconstruction technique and identify factors associated with poor knee function.
Methods
This study identified patients with a multi-ligament knee injury between 2006 and 2013. Patients who received a single-graft fibular collateral ligament and PLC reconstruction with a single-stage surgery during the study period and had a minimum follow-up of 2 years after surgery were included. Functional outcomes were assessed using Lysholm and IKDC scores. Varus and rotational knee laxity and range of motion were assessed using physical examination.
Results
The final study cohort included 61 patients who underwent PLC reconstruction using a single-graft technique. The mean IKDC score was 74.1 (± 22.3) and the mean Lysholm score was 80.3 (± 21.8) at mean follow-up of 3.8 years (range 2–9 years). Mean range of motion at final follow-up measured from 0° to 126° [range flexion: 95–145, range extension: 0–5]. Fifty-eight patients (95%) had grade 0 varus laxity in full knee extension, and 54 patients (88.5%) had grade 0 varus laxity at 30° of knee flexion. Female gender was associated with a lower postoperative IKDC score (p = 0.04).
Conclusion
Surgical treatment of the PLC using a single-graft technique can result in satisfactory knee function and stable physical examination findings at minimum 2 years after surgery. Female gender was predictive of poor knee function after PLC reconstruction. Surgical treatment of PLC injuries should be individualized based on the timing of surgery, specific injured knee structures, and physical examination findings. This study helps validate the use of a single-graft technique for PLC reconstruction and can be used to help counsel patients about expected knee function after surgical treatment of PLC injuries.
Level of evidence IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Increasing evidence demonstrates the importance of the posterolateral corner (PLC) for varus and rotational knee stability [20, 24]. Advancements in magnetic resonance imaging (MRI) and improved physician awareness have both resulted in a more consistent and timely diagnosis of this significant injury [27]. PLC injuries most commonly present in the setting of multi-ligament knee trauma, but isolated PLC injuries have also been reported [11,12,13, 19]. These injuries have previously been treated with anatomic repair; however, several studies have demonstrated that PLC reconstruction results in a lower rate of failure and better knee function at intermediate-term follow-up [11, 12, 19, 21, 23, 31]. Various surgical techniques have been developed to reconstruct the PLC but can generally be classified into a single-graft, fibula-based construct [29] or a dual-graft, combined fibula and tibia-based construct [2, 8, 17, 20, 26, 30].
Several cadaveric and clinical studies report adequate restoration of varus and rotational stability after PLC reconstruction [28]. In a cadaveric study, LaPrade et al. [20] showed that an anatomic dual-graft technique reliably restored stability in knees with grade III PLC injuries. A subsequent cadaveric study revealed that anatomic reconstruction using both single- and dual-graft techniques restored varus stability [22]. A similar retrospective study of 24 patients reported that PLC reconstruction consistently restored varus and rotational stability at 3 years of follow-up [28]. Additional studies have reported improvement in knee function and low failure rates following various PLC reconstruction techniques although objective outcomes such as stress radiography are limited [12, 13, 18, 23, 31, 34].
The purpose of this study was to report the functional and clinical outcomes after PLC reconstruction using the single-graft surgical technique (Fig. 1). Additionally, predictors of poor knee function after PLC reconstruction will be reported. The results of this study may help validate a surgical technique to reconstruct the PLC and further describe knee function after surgically treated PLC injuries. Surgeons may use this information to help prepare patients for expected knee function after PLC injuries.
Materials and methods
This retrospective study was performed at a tertiary academic sports medicine clinic between 2006 and 2013. Subjects were identified through a prospectively gathered database of patients with multi-ligament knee injuries. Patients were included if they sustained a multi-ligament knee injury (defined as ≥2 ligaments), were treated with PLC reconstruction using the single-graft technique in a single stage [29], and had a minimum 2-year follow-up (Fig. 2). Patients were excluded if they had an isolated posterolateral corner ligament injury, had a two ligament injury consisting of combined ACL and MCL tear (medial collateral ligament injury), had less than 2-year follow-up, had a fibular head avulsion, received PLC repair with or without graft augmentation, were treated with a dual-graft reconstruction technique, or were treated with a two-stage reconstruction. All patients in this cohort were treated with a single-stage multi-ligament reconstruction with a single graft. The age at time of injury, gender, associated meniscal or articular cartilage injury, ligamentous injury, and details of surgical treatment were recorded for each subject. Primary functional outcomes measured included Lysholm [32] and International Knee Documentation Committee (IKDC) [1] scores. Clinical outcomes included varus and rotatory laxity grading and knee range of motion on physical examination.
Previously defined subgroups for both the IKDC score and the Lysholm score were utilized. The IKDC score subgroups included: “poor” <70, “fair” 71–80, “good” 81–90, and “excellent” >90 points [25]. The Lysholm subgroups included: “poor” <65, “fair” 65–83, “good” 84–94, and “excellent” ≥95 points [3, 25].
Study cohort
The final study cohort included 61 patients who underwent posterolateral corner reconstruction using a single-graft posterolateral corner technique (single stage) between 2006 and 2013 (see Fig. 1). Mean age was 32.0 years (± 11.1 years) and 49 patients (80.3%) were male. Patients were classified by knee dislocation (KD) grade: 25 KD-1, 24 KD-3L, 7 KD-4, and 5 KD-5. One patient underwent prior high tibial osteotomy (HTO) for varus deformity. Twelve patients (19.6%) were treated acutely (within 3 weeks of injury) and 49 patients (80.3%) were treated after 3 weeks from injury.
There was a high rate of associated injuries at the time of diagnosis as 26 patients (42.6%) had meniscal tears and 20 patients (32.8%) had associated articular cartilage injury. Furthermore, 18 patients (29.5%) had an isolated peroneal nerve injury and 4 patients (6.6%) had a combined peroneal nerve and vascular injury.
Surgical technique
Only the anatomic single-graft reconstruction technique was employed in this cohort and has been previously described in detail by Schechinger et al. [29] PLC reconstruction (with soft tissue autograft or allograft) was performed when the preoperative MRI showed high-intensity signal throughout the PLC [5, 19] or if the structures were found to be attenuated or unrepairable (unable to mobilize or repair to anatomic origin) at the time of surgery and in all cases of delayed surgery. All patients in this cohort received only PLC reconstruction with a consistent single-graft technique, and no repair of PLC structures was made (tissue quality not amenable for repair). Patients who received concomitant repair with PLC reconstruction were excluded from analysis. Additionally, patients treated with a dual-graft technique were also excluded from this study. The author’s indication for a dual-graft technique was asymmetric knee hyperextension on examination (indicating disrupted popliteus and/or posterior capsule) and preoperative or intraoperative evidence of popliteus tendon disruption [10, 20].
Postoperative rehabilitation
All patients followed a standardized rehab protocol as described by Fanelli and Edson [7, 9]. Patients were maintained in full extension for 3 weeks postoperatively after multi-ligament reconstruction and subsequently began progressive knee range of motion (ROM) [7, 10]. Weight bearing was delayed for 6 weeks, hamstring activation was delayed for 4 months, and patients generally returned to sports or vigorous activity at 8–12 months after surgery. This study was conducted after approval from the institutional review board at the supporting institutions (07-004018).
Statistical analysis
Statistical analyses were carried out with study demographic data and injury descriptors such as popliteal artery and peroneal nerve injury. The data were summarized by means with standard deviations as a measure of variability. Sample size was taken into account for all calculations. A Wilcoxon rank-sum test was used when comparing means of continuous variables due to the nonparametric nature of the data and associated small sample size. Fisher’s exact test was used for comparison of categorical variables. A multivariate model using standard least squares analysis was constructed to analyse the relationship of IKDC and Lysholm scores with dependent variables such as age, gender, peroneal nerve injury, vascular injury, knee dislocation grade (KD grade), and cartilage or meniscus damage. For a multivariate standard least squares model accounting for the effects of age, gender, peroneal nerve injury, vascular injury, and associated cartilage and meniscus injury, it was determined that at least 10 events (in this case, knee dislocations) were necessary per variable used to have enough power in the multivariate model. For a total of 6 included variables, a total of 60 or more patients with knee dislocations would be an adequate sample size per previously mentioned standards. Statistical analyses were completed employing JMP software (version 7, SAS 135 Institute, Inc., Cary, NC). All statistical tests were two-sided and p-values <0.05 were considered statistically significant.
Results
The mean IKDC score was 74.1 (±22.3) and the mean Lysholm score was 80.3 (±21.8) at mean follow-up of 3.8 years (range 2–9 years). The IKDC scores were rated excellent or good in 31 patients (50.8%), fair in 6 patients (9.8%), and poor in 24 patients (39.3%). The final Lysholm scores were rated excellent or good in 39 patients (63.9%), fair in 9 patients (14.8%), and poor in 13 patients (21.3%). Mean range of motion at final follow-up measured from 0° to 126° [range flexion: 95–145, range extension: 0–5]. Fifty-eight patients (95.1%) had grade 0 varus laxity in full knee extension, while 3 patients (4.9%) had grade 1 laxity. Similarly, 54 patients (88.5%) had grade 0 varus laxity at 30° of knee flexion, 6 patients (9.8%) had grade 1 laxity, and 1 patient (1.7%) had grade 2 laxity. No patients demonstrated a posterolateral drawer on postoperative examination. Two patients developed arthrofibrosis and required manipulation under anaesthesia. One patient received a total knee replacement (TKA) 4 years after surgery (age at TKA was 62 years).
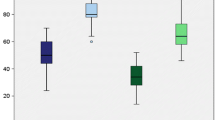
Multivariate regression analysis demonstrated an association between female gender and a lower postoperative IKDC score (p = 0.04). Female gender was not predictive of a lower postoperative Lysholm score. No association was found with age, KD grade, meniscal injury, articular cartilage injury, vascular injury, and isolated peroneal nerve injury and lower postoperative functional knee scores (Figs. 3, 4).
Discussion
The most important finding of the present study was satisfactory functional knee outcomes and stable physical examination findings after using a single-graft PLC reconstruction technique at a minimum 2-year follow-up. Additionally, female gender was associated with poor knee function after reconstruction.
The functional knee scores demonstrated in this cohort are comparable to previously published knee scores after PLC reconstruction [12, 18, 34]. Yang reported mean Lysholm and IKDC scores of 87 and 78, respectively, at 3 years following PLC reconstruction using a fibular sling method [34]. A prospective series reported IKDC scores of 79 among patients with combined PLC and cruciate ligament injuries treated with PLC reconstruction with or without concomitant repair [11]. Similarly, LaPrade reported mean IKDC scores of 63 at an average of 4 years following PCL reconstruction using an anatomic dual-graft technique [19]. In contrast, Jakobsen reported higher functional scores in 27 patients with isolated PLC injuries that had anatomic reconstruction of the LCL and popliteus tendon [13]. In their study, 71% of patients obtained normal or near normal IKDC scores [13]. Functional knee scores after PLC reconstruction should be interpreted in the context of normal values. Several studies have reported IKDC and Lysholm scores among the general population as reference values. For example, a cross-sectional survey of 5246 knees reported IKDC scores of 89 among patients aged 18–34 with a progressive decrease in scores with increasing age [1]. Similarly, the mean Lysholm knee score has been estimated to be between 94 and 99 among patients in the general population [3, 6]. Together these data suggest that patients with isolated PLC injuries treated with ligament reconstruction may achieve knee function approaching normal levels. However, it is important to recognize that there was only one patient in this cohort with an isolated PLC injury. In contrast, patients with high-energy multi-ligament knee injuries (possibly associated with knee dislocation) may have IKDC and Lysholm scores well below normal values found in the general population.
Female gender was associated with a poor IKDC score after PLC reconstruction. This finding agrees well with King et al. [15] who reported inferior outcomes in female patients after surgical treatment of KDIII knee dislocations. An additional series of 65 patients with knee dislocations (KDIII-M and KDIV) reported significantly lower Lysholm knee scores in females compared to male patients [33]. The reason for lower outcomes in females is unclear and difficult to determine due to relatively small retrospective cohorts currently available. However, this information can be used preoperatively to counsel female patients about expectations following surgery. In contrast, peroneal nerve injury was not associated with poor knee function after PLC reconstruction which is similar to conclusions from two previous series of patients with knee dislocations [15, 16]. Although poorly understood, partial or complete nerve recovery at 2-year follow-up may result in similar function between patients with and without a nerve injury. Alternatively, the relatively small cohort size of currently available studies and the lack of recognition of peroneal nerve injury in current patient-reported outcomes may explain why no association was detected between nerve injury and knee function. Newer outcome scores are currently being validated, which are tailored to multi-ligament knee injury patients, and take into account nerve function and other associated factors [4].
Despite the consistent technique utilized in this cohort, surgical treatment of multi-ligament injured knees should be individualized based on ligament injury pattern and associated injuries. PLC reconstruction should be used when the PLC tissue quality is considered unacceptable for repair based on preoperative MRI or intraoperative assessment [5, 19, 21, 30]. Surgeons must choose between previously described single- and dual-graft reconstruction techniques [2]. Dual-graft techniques using independent grafts for reconstruction of the popliteus tendon can be used when physical examination reveals evidence of asymmetric knee hyperextension indicating a loss of popliteus function [9]. Other authors have suggested using a dual-graft technique when there is disruption of the proximal tibiofibular joint [2] or joint space widening of greater than 4 mm varus stress views [20].
The results of this study should be interpreted with the following limitations. Retrospective analysis of the prospectively recorded data, combined with the wide variability in ligament injury patters and associated injures may limit the generalizability of the findings. Similarly, the relatively small patient cohort reduces study power, especially for the multivariate analyses where real differences may not be apparent. The improvement in knee function after PLC surgery could not be assessed because preoperative functional knee scores were not available. Selection bias resulted from surgical decision making for each patient based on the injury pattern and the status of the soft tissue. This series included only those patients treated with a single-stage operation. However, one systematic review and other studies have shown satisfactory outcomes between staged and non-staged reconstructions [8, 9, 14]. Radiographic varus instability was not consistently assessed using preoperative or postoperative stress views to document asymmetric laxity between knees and limits the objective knee stability reported [18]. In addition, the operating surgeon performed all postoperative physical examinations without blinded verification which may introduce bias. Likewise, postoperative immobilization in knee extension for 3 weeks may have contributed to a decrease in the final knee flexion obtained and may have contributed to lower knee function at final follow-up. Limitations of knee flexion may have contributed to poor knee function after treatment of PLC injuries. Despite these, the strengths of this study include the relatively long-term follow-up, use of a single surgical technique, exclusion of patients with concomitant PLC repair, and standardized rehabilitation protocols.
Conclusion
Surgical treatment of the PLC using a single-graft technique can result in satisfactory knee function and stable physical examination findings at minimum 2 years after surgery. Female gender was predictive of poor knee function after PLC reconstruction. Surgical treatment of PLC injuries should be individualized based on the timing of surgery, specific injured knee structures, and physical examination findings. This study helps validate the use of a single-graft technique for PLC reconstruction and can be used to help counsel patients about expected knee function after surgical treatment of PLC injuries.
References
Anderson A, Irrgang J, Kocher M, Mann B, Harrast J, International Knee Documentation Committee (2006) The international knee documentation committee subjective knee evaluation form: normative data. Am J Sports Med 34:128–135
Blackman A, Engasser W, Krych A, Stuart M, Levy B (2015) Fibular head and tibial-based (2-tailed) posterolateral corner reconstruction. Sports Med Arthrosc 23:44–50
Briggs K, Steadman J, Hay C, Hines S (2009) Lysholm score and Tegner activity level in individuals with normal knees. Am J Sports Med 37:898–901
Chahal J, Whelan D, Jaglal S, Smith P, MacDonald P, Levy B, Davis A (2014) The multiligament quality of life questionnaire: development and evaluation of test-retest reliability and validity in patients with multiligament knee injuries. Am J Sports Med 42:2906–2916
Collins M, Bond J, Crush A, Stuart M, King A, Levy B (2015) MRI injury patterns in surgically confirmed and reconstructed posterolateral corner knee injuries. Knee Surg Sports Traumatol Arthrosc 23:2943–2949
Demirdjian A, Petrie S, Guanche C, Thomas K (1998) The outcomes of two knee scoring questionnaires in a normal population. Am J Sports Med 26:46–51
Edson C (2001) Postoperative rehabilitation of the multiligament-reconstructed knee. Sports Med Arthrosc Rev 9:247–254
Fanelli G, Edson C (2012) Surgical treatment of combined PCL–ACL medial and lateral side injuries (global laxity): surgical technique and 2 to 18 year results. J Knee Surg 25:307–316
Fanelli G, Orcutt D, Edson C (2005) The multiple-ligament injured knee: evaluation, treatment, and results. Arthroscopy 21:471–486
Fanelli G, Stannard J, Stuart M, MacDonald P, Marx R, Whelan D, Boyd J, Levy B (2010) Management of complex knee ligament injuries. J Bone Joint Surg Am 92:2235–2246
Geeslin A, LaPrade R (2011) Outcomes of treatment of acute grade-III isolated and combined posterolateral knee injuries: a prospective case series and surgical technique. J Bone Joint Surg Am 93:1672–1683
Geeslin A, Moulton S, LaPrade R (2016) A systematic review of the outcomes of posterolateral corner knee injuries, part 1: surgical treatment of acute injuries. Am J Sports Med 44:1336–1342
Jakobson B, Lund B, Christiansen S, Lind M (2010) Anatomic reconstruction of the posterolateral corner of the knee: a case series with isolated reconstruction in 27 patients. Arthroscopy 26:918–925
Jiang W, Yao J, He Y, Sun W, Huang Y, Kong D (2015) The timing of surgical treatment of knee dislocations: a systematic review. Knee Surg Sports Traumatol Arthrosc 23:3108–3113
King A, Krych A, Prince M, Pareek A, Stuart M, Levy B (2016) Surgical outcomes of medial versus lateral multiligament-injured, dislocated knees. Arthroscopy 32:1814–1819
Krych A, Giuseffi S, Kuzma S, Stuart M, Levy B (2014) Is peroneal nerve injury associated with worse function after knee dislocation? Clin Orthop Relat Res 472:2630–2636
Kuzma S, Chow R, Engasser W, Stuart M, Levy B (2014) Reconstruction of the posterolateral corner of the knee with Achilles tendon allograft. Arthrosc Tech 3:e393–e398
LaPrade R, Heikes C, Bakker A, Jakobsen R (2008) The reproducibility and repeatability of varus stress radiographs in the assessment of isolated fibular collateral ligament and grade-III posterolateral knee injuries. An in vitro biomechanical study. J Bone Joint Surg Am 90:2069–2076
LaPrade R, Johansen S, Agel J, Risberg M, Moksnes H, Engebretsen L (2010) Outcomes of an anatomic posterolateral knee reconstruction. J Bone Joint Surg Am 92:16–22
LaPrade R, Johansen S, Wentorf F, Engebretsen L, Esterberg J, Tso A (2004) An analysis of an anatomical posterolateral knee reconstruction: an in vitro biomechanical study and development of a surgical technique. Am J Sports Med 32:1405–1414
Levy B, Dajani K, Morgan J, Shah J, Dahm D, Stuart M (2010) Repair versus reconstruction of the fibular collateral ligament and posterolateral corner in the multiligament-injured knee. Am J Sports Med 38:804–809
McCarthy M, Carmarda L, Wijkicks C, Johansen S, Engebretsen L, LaPrade R (2010) Anatomic posterolateral knee reconstructions require a popliteofibular ligament reconstruction through a tibial tunnel. Am J Sports Med 38:1674–1681
Moulton S, Geeslin A, LaPrade R (2016) A systematic review of the outcomes of posterolateral corner knee injuries, part 2: surgical treatment of chronic injuries. Am J Sports Med 44:1616–1623
Nau T, Chevalier Y, Hagemeister N, Deguise J, Duval N (2005) Comparison of 2 surgical techniques of posterolateral corner reconstruction of the knee. Am J Sports Med 33:1838–1845
Pestka J, Bode G, Salzmann G, Steinwachs M, Schmal H, Sudkamp N, Neimeyer P (2014) Clinical outcomes after cell-seeded autologous chondrocyte implantation of the knee: when can success or failure be predicts? Am J Sports Med 42:208–225
Prince M, Stuart M, King A, Sousa P, Levy B (2015) Posterolateral reconstruction of the knee: two-tailed surgical techniques. J Knee Surg 28:464–470
Ranawat A, Baker C, Henry S, Harner C (2008) Posterolateral corner injury of the knee: evaluation and management. J Am Acad Orthop Surg 16:506–518
Rios C, Leger R, Cote M, Yang C, Arciero R (2010) Posterolateral corner reconstruction of the knee: evaluation of a technique with clinical outcomes and stress radiography. Am J Sports Med 38:1564–1574
Schechinger S, Levy B, Dajani K, Shah J, Herrera D, Marx R (2009) Achilles tendon allograft reconstruction of the fibular collateral ligament and posterolateral corner. Arthroscopy 25:232–242
Stannard J, Brown S, Farris R, McGwin G, Volgas D (2005) The posterolateral corner of the knee: repair versus reconstruction. Am J Sports Med 33:881–888
Stannard J, Brown S, Robinson J, McGwin G, Volgas D (2005) Reconstruction of the posterolateral corner of the knee. Arthroscopy 21:1051–1059
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
Werner B, Hadeed M, Gwarthmey F, Gaskin C, Hart J, Miller M (2014) Medial injury in knee dislocations: what are the common injury patterns and surgical outcomes? Clin Orthop Relat Res 472:2658–2666
Yang B, Bae W, Ha J, Lee D, Jang H, Kim J (2013) Posterolateral corner reconstruction using the single fibular sling method for posterolateral rotatory instability of the knee. Am J Sports Med 41:1605–1612
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
No external source of funding.
Ethical Approval
Institutional Review Board approval was granted by Mayo Clinic (07-004018).
Informed consent
Informed consent was obtained for all patients in the study.
Rights and permissions
About this article
Cite this article
Sanders, T.L., Johnson, N.R., Pareek, A. et al. Satisfactory knee function after single-stage posterolateral corner reconstruction in the multi-ligament injured/dislocated knee using the anatomic single-graft technique. Knee Surg Sports Traumatol Arthrosc 26, 1258–1265 (2018). https://doi.org/10.1007/s00167-017-4631-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4631-6