Abstract
Purpose
Traumatic knee dislocations (KDs) are unusual yet limb-threatening injuries; the timing of surgical intervention is still debated. A systematic review was performed to determine the optimal timing of surgery with respect to injury pattern.
Methods
A comprehensive search of Medline, EMBASE, and Cochrane Central Register of Controlled Trials was performed for studies published between 1 January 1974 and 20 April 2014 on the surgical management of “knee dislocation” and “multiligament knee injuries”. Surgical timing was classified as acute, chronic, or staged. A systematic review was performed for patients with KD-III according to Schenck’s classification using individual patient data.
Results
Twelve studies including 150 patients (153 knees) with KDs fulfilled the study requirements. Sixty-nine cases with KD-IIIM and 84 cases with KD-IIIL were identified. Excellent or good results were demonstrated in 79.1 % (34 cases) of cases managed with staged treatment versus 58.4 % (45 cases) of cases undergoing acute surgery (p = 0.02), and versus 45.5 % (15 cases) of cases undergoing chronic surgery (p = 0.002). No statistically significant difference was found in the percentage of excellent or good results between the acute and chronic surgery groups (n.s.), or between the KD-IIIM and KD-IIIL groups (n.s.).
Conclusion
Staged treatment yields the best clinical results for patients with KD-III. No statistically significant difference was shown in the clinical results between acute surgery and chronic surgery groups.
Level of evidence
IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Knee dislocation (KD) is an uncommon but serious injury accounting for <0.2 % of orthopaedic injuries [17, 20]. There is a lack of high-level literature regarding treatment, and the optimal approach remains contested. Most surgeons advocate surgical management due to the poor outcomes of nonoperative treatment [1, 2, 4, 10, 14, 15, 21, 24, 28, 30, 33, 37, 42, 43]. Operative treatment was shown to be superior with regard to Lysholm scores and range of motion (ROM) in a meta-analysis [4].
There is also no consensus regarding timing of surgery. Many authors recommended that operative intervention be performed within 3 weeks [10, 14, 15, 21, 24, 28, 33, 42, 43]. A recent systematic review showed that patients undergoing early surgery achieved better clinical and functional results compared with delayed surgery [21]. Staged treatment has been widely accepted (first collateral ligamentous structures or posterior cruciate ligament in the acute phase and then residual ligamentous structures in the chronic phase) with good clinical outcomes [1, 2, 28, 37].
Despite the differentiation of various injury patterns, they have commonly been reported together. Most studies did not correlate clinical results with surgical timing and injury patterns.
Schenck [31] described an anatomic classification system based on the pattern of injured structures in KD, which is helpful in achieving homogeneity among different treatment groups. Schenck’s classification of injury pattern greatly affects clinical results [9]. A lack of homogeneity in injury patterns can result in difficulties when comparing outcomes between treatment groups.
With regard to timing of surgical treatment, existing systematic reviews or meta-analyses did not consider injury patterns or the lack of homogeneity therein [21, 27]. The purpose of this study was to review applicable literature to compare the clinical outcomes of acute, chronic or staged treatment of KDs, with respect to injury pattern.
Materials and methods
A comprehensive search of Medline, EMBASE and Cochrane Central Register of Controlled Trials was performed for studies published between 1 January 1974 and 20 April 2014 on the surgical management of “knee dislocation” and “multiligament knee injuries”. The reference lists of eligible articles were also reviewed. All studies providing individual patient data—pattern of injury, surgical timing, and follow-up evaluation in the text (including table and figure)—were included. Exclusion criteria were as follows: case reports; review articles; technique papers; surgical management of patients with KD-I, KD-II, and KD-IV; irreducible knee dislocations; minimum follow-up time of <1 year; and a paucity of data on International Knee Documentation Committee (IKDC) or Lysholm scores.
The individual patient data extracted from the eligible studies were as follows: age; gender; mechanism of injury; Schenck’s classification of injury pattern; time from injury to surgery; follow-up period; and clinical outcomes. Timing of surgery was divided into three categories: (1) acute surgery (ligamentous surgery performed <3 weeks after injury); (2) chronic surgery (ligamentous surgery performed more than 3 weeks after injury); and (3) staged treatment (both acute and chronic surgery). One of the approaches to staged treatment was defined as staged A in this study [1, 2, 37], and the other strategy was defined as staged B [28].
Clinical outcomes were graded as “excellent”, “good”, “fair”, and “poor” according to IKDC scores or, if unavailable, according to Lysholm scores [1, 16, 25, 39]. Furthermore, clinical outcomes were aggregated to a dichotomous variable classified as “excellent or good” and “fair or poor”.
Statistical analysis
Weighted means for categorical variables were obtained as follows. The proportion of an outcome variable in each treatment group was decided by dividing the total number of cases with an occurrence in all studies by the total number of cases in all studies. Schenck’s classification of injury pattern and surgical timing were associated with surgical outcome, a dichotomous variable characterized as “excellent or good” and “fair or poor”. Pooling of eligible data from all included studies for surgical timing, and the subsequent aggregate analysis was performed to determine frequencies of “excellent or good” and “fair or poor” and to compare outcomes of different treatment groups. The Chi-squared test was used to compare dichotomous variables across groups. A p value of <0.05 was considered to be statistically significant. All statistical analysis was performed with SPSS version 16.0 software (SPSS Inc., Chicago, IL, USA).
Results
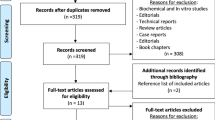
Twelve articles were eligible for this study (Fig. 1). Among the identified articles, 150 patients (153 knees) were included. Sixty-nine cases with KD-IIIM and 84 cases with KD-IIIL according to Schenck’s classification were identified (Table 1). Seventy-seven cases underwent acute surgery, 33 underwent chronic surgery, and 43 underwent staged treatment (34 staged A and 9 staged B; Table 2).
Excellent or good results were demonstrated in 79.4 % (27 cases) of cases managed with staged A, compared with 77.8 % (7 cases) of cases undergoing staged B (Table 3). No statistically significant difference was shown in the percentage of excellent or good results between staged A and staged B groups (n.s.).
Excellent or good results were demonstrated in 79.1 % (34 cases) of cases managed with staged treatment versus 58.4 % (45 cases) of cases undergoing acute surgery (p = 0.02), and versus 45.5 % (15 cases) of cases undergoing chronic surgery (p = 0.002). No statistically significant difference was found in the percentage of excellent or good results between the acute and chronic surgery groups (n.s.), or between the KD-IIIM and KD-IIIL groups (n.s.).
Discussion
The most important finding of the present systematic review was that the best results were yielded by staged treatment. Excellent or good results were achieved by staged treatment in 79.1 % (34 cases) of cases with KD-III. In addition, acute surgery can also achieve a favourable outcome. However, there was no statistically significant difference in the proportion of excellent or good results between acute and chronic surgery groups. This systematic review ensured similar injury patterns to allow comparison of findings between groups.
To our knowledge, this study is the first systematic review on surgical timing using individual data of patients with KD-III to achieve homogeneity in different treatment groups.
Acute surgery is usually defined as operative management performed <3 weeks after injury. Most authors advocate acute surgery for the treatment of KDs, prior to scar formation and tissue retraction [23, 32]. This is particularly relevant for collateral structures, where developing scar tissue can complicate the operative field. Due to the risk of fluid extravasation, arthroscopic treatment of KDs may increase the risk of compartment syndrome within the first day after injury [38]. Hence, a delay of 1–2 weeks after injury is usually recommended to diminish acute inflammation and soft tissue swelling prior to surgery.
Excellent and good results were found in 58.4 % (45 cases) of cases managed with acute surgery; other authors also reported acceptable outcomes [12, 14, 21, 29]. Ibrahim et al. [14] found a mean Lysholm score of 91 points at a minimum of 24-month follow-up in 20 patients with KDs who underwent operative treatment 2–3 weeks after injury. Patients with multiligament knee injuries who undergo acute surgery have a significantly better outcome compared with chronic surgery [37]. Conversely, acute surgery of KDs should be avoided due to the increased risk of arthrofibrosis [11, 26, 34, 35]. Harner et al. [12] reviewed 31 KDs, including 19 patients managed with acute surgery and 12 patients with chronic surgery. At a minimum follow-up period of 2 years, only four cases managed with acute surgery required manipulation because of loss of flexion [12].
Chronic surgery is defined as surgical treatment performed more than 3 weeks after injury. And 3 weeks after injury was widely considered to be the critical time between “acute” and “chronic” [6, 13, 22, 40, 41]. Chronic surgery can achieve good clinical results and has shown a lower incidence of arthrofibrosis compared with acute surgery [5, 8, 18]. However, chronic repair of collateral ligaments and posterolateral structures is insufficient due to excessive scar tissue and difficulty in identifying anatomic structures [12, 22, 23]. Moreover, chronic multiligament knee injuries may change limb alignment and generate knee deformities [3, 19]. There is a lack of published studies which directly compare acute and chronic surgery in patients with KDs, to indicate improvement in clinical results after acute surgery. Fanelli et al. [7] reported that there was no statistically significant difference between acute and chronic multiligament knee injuries evaluated with Tegner, Lysholm, and Hospital Special Surgery knee scales postoperatively in 20 patients.
Excellent or good results were shown in 45.5 % (15 cases) of cases managed with chronic surgery, compared with 58.4 % (45 cases) of cases undergoing acute surgery, with no statistically significant difference between the acute and chronic groups. However, surgical timing depends on the neurovascular status of the extremity, multiple traumas, skin condition, open versus closed knee injury, and other orthopaedic injuries. Furthermore, coexisting injuries frequently preclude acute surgery, and in certain cases surgical management must be delayed until patients are in a stable condition.
Staged treatment has been adopted by many authors [1, 2, 28, 37]. After acutely surgical treatment of the collateral ligamentous structures or reconstruction of the posterior cruciate ligament is performed as the first stage, accurate alignment of the knee aids in the natural healing of residual structures. Staged treatment simplifies the operative process and shortens operative time in the acute phase, decreasing the rate of arthrofibrosis compared with acute surgery or repairing or reconstructing all injured ligaments [28, 37]. This strategy can produce better subjective outcomes and knee stability, it is convenient for patients to undergo postoperative rehabilitation, and therefore, the best ROM is achieved [27]. Nonetheless, patients undergoing staged treatment are as likely to require additional treatment for recovery of full ROM as those who undergo acute surgery [2]. Moreover, this strategy entails a greater duration of recovery than repair or reconstruction of all torn ligaments in the acute stage [2].
Several limitations were presented in the present systematic review. First, a paucity of high-level literature was found on the topic. All of the included studies are retrospective case series, which contain inherent biases. Second, there is heterogeneity with regard to surgical techniques, materials for reconstruction and fixation, mechanisms of injury, and the method of classifying “excellent or good” and “fair or poor” according to IKDC scales or Lysholm scores. Finally, due to a lack of sufficient data on individual patients’ outcome measures in the included studies, only a single measurement was compared between different treatment groups. Staged treatment yields the best clinical results for patients with KD-III in this study. However, there is a need of higher-level comparative studies on surgical timing to support.
Conclusion
Staged treatment yields the best clinical results for patients with KD-III. No statistically significant difference was shown in the clinical outcomes between acute surgery and chronic surgery groups.
References
Acharya KKV, Pandey V, Rao PS (2010) Knee dislocation with multi-ligament injury: evaluation, treatment and results. J Musculoskelet Res 13(3):119–126
Bin SI, Nam TS (2007) Surgical outcome of 2-stage management of multiple knee ligament injuries after knee dislocation. Arthroscopy 23(10):1066–1072
Bispo RZ Jr, Kawano CT, Guedes AV (2008) Chronic multiple knee ligament injuries: epidemiological analysis of more than one hundred cases. Clinics (Sao Paulo) 63(1):3–8
Dedmond BT, Almekinders LC (2001) Operative versus nonoperative treatment of knee dislocations: a meta-analysis. Am J Knee Surg 14(1):33–38
Fanelli GC, Edson CJ (2002) Arthroscopically assisted combined anterior and posterior cruciate ligament reconstruction in the multiple ligament injured knee: 2- to 10-year follow-up. Arthroscopy 18(7):703–714
Fanelli GC, Edson CJ, Beck JD (2010) How I treat the multiple-ligament injured knee. Oper Tech Sports Med 18(4):198–210
Fanelli GC, Edson CJ (2004) Combined posterior cruciate ligament-posterolateral reconstructions with achilles tendon allograft and biceps femoris tendon tenodesis: 2- to 10-year follow-up. Arthroscopy 20(4):339–345
Fanelli GC, Giannotti BF, Edson CJ (1996) Arthroscopically assisted combined posterior cruciate ligament/posterior lateral complex reconstruction. Arthroscopy 12(5):521–530
Frosch KH, Preiss A, Heider S, Stengel D, Wohlmuth P, Hoffmann MF, Lill H (2013) Primary ligament sutures as a treatment option of knee dislocations: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 21(7):1502–1509
Gauffin H, Rockborn P (2014) Knee dislocations: is reconstruction of the posterior cruciate ligament crucial? Eur J Orthop Surg Traumatol 24(3):371–377
Harner CD, Irrgang JJ, Paul J, Dearwater S, Fu FH (1992) Loss of motion after anterior cruciate ligament reconstruction. Am J Sports Med 20(5):499–506
Harner CD, Waltrip RL, Bennett CH, Francis KA, Cole B, Irrgang JJ (2004) Surgical management of knee dislocations. J Bone Joint Surg Am 86A(2):262–273
Howells NR, Brunton LR, Robinson J, Porteus AJ, Eldridge JD, Murray JR (2011) Acute knee dislocation: an evidence based approach to the management of the multiligament injured knee. Injury 42(11):1198–1204
Ibrahim SA, Ahmad FH, Salah M, Al Misfer AR, Ghaffer SA, Khirat S (2008) Surgical management of traumatic knee dislocation. Arthroscopy 24(2):178–187
Ibrahim SA, Ghafar S, Salah M, Abo Alnas M, Al Misfer A, Farouk H, Al Haran H, Khirait S (2013) Surgical management of traumatic knee dislocation with posterolateral corner injury. Arthroscopy 29(4):733–741
Irrgang JJ, Ho H, Harner CD, Fu FH (1998) Use of the International Knee Documentation Committee guidelines to assess outcome following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 6(2):107–114
Jones RE, Smith EC, Bone GE (1979) Vascular and orthopedic complications of knee dislocation. Surg Gynecol Obstet 149(4):554–558
Karataglis D, Bisbinas I, Green MA, Learmonth DJ (2006) Functional outcome following reconstruction in chronic multiple ligament deficient knees. Knee Surg Sports Traumatol Arthrosc 14(9):843–847
Kawano CT, Bispo RZ Jr, de Oliveira MG, Soejima AT, Apostolopoulos SDB (2007) Posterolateral knee instability: an alternative proposal for surgical treatment. Clinics (Sao Paulo) 62(3):371–374
Klimkiewicz JJ, Petrie RS, Harner CD (2000) Surgical treatment of combined injury to anterior cruciate ligament, posterior cruciate ligament, and medial structures. Clin Sports Med 19(3):479–492
Levy BA, Dajani KA, Whelan DB, Stannard JP, Fanelli GC, Stuart MJ, Boyd JL, MacDonald PA, Marx RG (2009) Decision making in the multiligament injured knee: an evidence based systematic review. Arthroscopy 25(4):430–438
Levy BA, Stuart MJ (2012) Treatment of PCL, ACL, and lateral-side knee injuries: acute and chronic. J Knee Surg 25(4):295–305
Liow RY, McNicholas MJ, Keating JF, Nutton RW (2003) Ligament repair and reconstruction in traumatic dislocation of the knee. J Bone Joint Surg Br 85(6):845–851
Li X, Liu T (2013) Surgical management of multiple knee ligament injuries. Eur J Orthop Surg Traumatol 23(6):691–697
Lo YP, Hsu KY, Chen LH, Wang CJ, Yeh WL, Chan YS, Chen WJ (2009) Simultaneous arthroscopic reconstruction of the anterior and posterior cruciate ligament using hamstring and quadriceps tendon autografts. J Trauma 66(3):780–788
Mohtadi NG, Webster-Bogaert S, Fowler PJ (1991) Limitation of motion following anterior cruciate ligament reconstruction. A case-control study. Am J Sports Med 19(6):620–625
Mook WR, Miller MD, Diduch DR, Hertel J, Boachie-Adjei Y, Hart JM (2009) Multiple-ligament knee injuries: a systematic review of the timing of operative intervention and postoperative rehabilitation. J Bone Joint Surg Am 91(12):2946–2957
Ohkoshi Y, Nagasaki S, Shibata N, Yamamoto K, Hashimoto T, Yamane S (2002) Two-stage reconstruction with autografts for knee dislocations. Clin Orthop Relat Res 398:169–175
Owens BD, Neault M, Benson E, Busconi BD (2007) Primary repair of knee dislocations: results in 25 patients (28 knees) at a mean follow-up of four years. J Orthop Trauma 21(2):92–96
Ríos A, Villa A, Fahandezh H, de José C, Vaquero J (2003) Results after treatment of traumatic knee dislocations: a report of 26 cases. J Trauma 55(3):489–494
Schenck R Jr (2003) Classification of knee dislocation. Oper Tech Sports Med 11(3):193–198
Schenck RC Jr (1994) The dislocated knee. Instr Course Lect 43:127–136
Shelbourne KD, Haro MS, Gray T (2007) Knee dislocation with lateral side injury: results of an En Masse surgical repair technique of the Lateral Side. Am J Sports Med 35(7):1105–1116
Shelbourne KD, Porter DA, Clingman JA, McCarroll JR, Rettig AC (1991) Low-velocity knee dislocation. Orthop Rev 20(11):995–1004
Shelbourne KD, Wilckens JH, Mollabashy A, DeCarlo M (1991) Arthro-fibrosis in acute anterior cruciate ligament reconstruction. The effect of timing of reconstruction and rehabilitation. Am J Sports Med 19(4):332–336
Strobel MJ, Schulz MS, Petersen WJ, Eichhorn HJ (2006) Combined anterior cruciate ligament, posterior cruciate ligament, and posterolateral corner reconstruction with autogenous hamstring grafts in chronic instabilities. Arthroscopy 22(2):182–192
Subbiah M, Pandey V, Rao SK, Rao S (2011) Staged arthroscopic reconstructive surgery for multiple ligament injuries of the knee. J Orthop Surg (Hong Kong) 19(3):297–302
Tay AK, MacDonald PB (2011) Complications associated with treatment of multiple ligament injured (dislocated) knee. Sports Med Arthrosc 19(2):153–161
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
Van Tongel A, MacDonald PB (2010) How I manage the multiple-ligament injured knee. Oper Tech Sports Med 18(4):245–249
Vyas D, Harner CD (2011) How I manage the multiple-ligament injured (dislocated) knee. Oper Tech Sports Med 19(1):2–11
Wascher DC, Becker JR, Dexter JG, Blevins FT (1999) Reconstruction of the anterior and posterior cruciate ligaments after knee dislocation results using fresh-frozen nonirradiated allografts. Am J Sports Med 27(2):189–196
Yeh WL, Tu YK, Su JY, Hsu RW (1999) Knee dislocation: treatment of high-velocity knee dislocation. J Trauma 46(4):693–701
Conflict of interest
All authors report no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jiang, W., Yao, J., He, Y. et al. The timing of surgical treatment of knee dislocations: a systematic review. Knee Surg Sports Traumatol Arthrosc 23, 3108–3113 (2015). https://doi.org/10.1007/s00167-014-3435-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3435-1