Abstract
Purpose
One of the most important factors leading to revision of total knee arthroplasties (TKA) is malrotation of femoral and/or tibial component. Rotation measurements performed on radiographs are limited and less reliable compared to 2D computed tomography (CT). Nowadays, 2D-CT and 3D-CT can be distinguished in measuring rotation of the TKA components. The aim of this systematic review is to determine the most reliable CT techniques in measuring rotation of the TKA components and to investigate possible cut-off points that can be used in the clinician’s decision for a possible revision of the TKA.
Methods
A search of PubMed, Embase, the Cochrane Central Register of Controlled Trials and Web of Science was performed up to April 2015. Final selections of 12 articles were used in this systematic review.
Results
3D-CT, compared to 2D-CT, is more reliable and shows a high level of intra- and interobserver reliability. Femoral component rotation is measured using the component’s posterior condylar line or inner pegs in relation to the epicondylar axis. Five different techniques were used to measure tibial component rotation. The posterior border of the tibial component in relationship to the geometric centre and tibial tubercle was most frequently used.
Conclusion
This systematic review shows a strong preference for 3D-CT to determine the component’s rotation following a TKA. The literature shows consensus on the reference points of the femoral component. In measurements of the tibial component, various techniques are used with similar results. No clear cut-off point for revision of malrotated TKA components can be stated because of limited evidence.
Level of evidence
III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
About one in five patients are not satisfied after TKA [10, 24]. These patients often experience pain, instability, patellofemoral maltracking, stiffness or impaired function of the knee, 1 year after the TKA [2, 10, 13, 16, 31, 32, 36]. Malrotation of one or both components of the TKA may lead to aseptic loosening, instability, polyethylene wear or dislocation of the patella. It is therefore one of the most important factors leading to a revision of the TKA [4, 13, 34].
Roentgenographic measurements of the component’s position after TKA started with the knee evaluation system introduced by Ewald in 1989 [12]. Varus–valgus and flexion–extension alignment can be identified on (long-leg) radiographs, but is subject to rotation and magnification errors [1, 33]. Since the introduction of the CT scan, Berger et al. introduced a protocol on TKA component rotation measurements in 1993 [6–8, 25]. Post-operative sagittal, coronal and rotational alignment is routinely measured on two-dimensional (2D)-CT scans. Three-dimensional (3D) reconstructions, in which individual slices are accumulated to create a volume, are less frequently used in measuring the component’s rotation. In 3D-CT, measurements can be adjusted for the variability of the position of the patient’s leg in the scanner, which may lead to more reliable identification of the anatomical landmarks [18, 19].
Uncertainty exists nowadays about the most accurate technique to measure component rotation and what cut-off points must be applied. This is the first systematic review investigating which CT technique (2D or 3D) is most reliable in measuring rotation of the tibial and/or femoral component after TKA. Secondary outcome is the range of component rotation, from which a normal or deviating component rotation can be defined. Therefrom, we aim to define cut-off points that can be used in deciding for a revision of the TKA.
Materials and methods
Inclusion and exclusion criteria
This study included published full-text reports of randomized and non-randomized controlled trials, prospective and retrospective cohort studies and case–control studies.
Selection criteria consisted of patients (>18 years) with osteoarthritis of the knee, treated with primary or revision TKA and reporting post-operative measurements of TKA component rotation using a CT scan. Furthermore, studies were only selected if full description of the measurements was given, including reference points, for femoral and/or tibial component rotation. Studies were excluded when reporting on unicompartimental knee arthroplasties and studies based on pre- or peroperative measurements, instead of post-operative measurements.
Search strategy
A systematic search was conducted to identify all relevant reports using the scientific search engines Medline (PubMed), Embase, the Cochrane Library of Clinical Trials and Web of Science from their inception until April 2015. Languages were restricted to English, Dutch and German. The search strategy was designed based on the following controlled vocabulary (MeSH terms) and free text terms: (Arthroplasty, replacement, knee OR knee prosthesis OR knee joint prostheses, prosthesis, implants OR knee endoprosthesis OR TKA OR tibial component OR femoral component) AND (Tomography, X-ray computed OR computed tomography OR CT OR electron beam OR tomodensitometer) AND (Rotation OR bone malalignment OR malrotation OR alignment OR malalignment OR maltracking OR gap asymmetry OR torsion OR malposition).
Study selection
The initial search strategy, after eliminating 379 duplicates, resulted in a total of 847 hits.
Two reviewers (E.V. and E.M.) independently applied the selection criteria on the titles (788) and abstracts (59) from which 23 potentially relevant studies were selected. The full texts of these 23 studies were once more reviewed, and a final selection was made based on the above-mentioned criteria. Reference lists of all included articles were then searched to retrieve additional published studies not identified by the computerized database search (0). Disagreements were resolved through a consensus meeting. Twelve articles were finally included in the systematic review. The selection procedure is summarized in Fig. 1.
Levels of evidence
The Oxford Levels of Evidence as produced by the Oxford Centre for Evidence-Based Medicine was used to categorize methodological quality [28]. This tool classifies systematic randomized clinical trials and inception cohort studies as Level II evidence, cohort studies or control arm of randomized trials as Level III evidence, and case series or case–control studies or poor-quality prognostic cohort studies as Level IV evidence.
Quality assessment
Quality assessment was performed according to the Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies drafted by the National Institutes of Health [27]. This tool is designed to evaluate the internal validity of a study considering the risk of potential bias and confounders. For each included study, 14 questions were answered, concerning the methodologically quality of each study. An overview is given in Table 1.
Data extraction
Two reviewers (E.V. and E.M.) extracted data independently. The collected data consisted of year of publication, type of study, CT technique (2D- or 3D-CT), population, component of interest, (anatomical) reference points, results (intraclass correlation coefficient) and level of evidence. Disagreements were resolved through a consensus meeting.
Results
Description of included studies
The final selection of 12 studies contained six prospective cohort studies, five retrospective cohort studies and one human cadaver specimen cohort study, published between 2000 and 2014. According to The Oxford Levels of Evidence as produced by the Oxford Centre for Evidence-Based Medicine [28], all studies are considered as Level III evidence. An overview of the 12 included studies is shown in Table 2.
Measuring rotation of the femoral component
Femoral component rotation is defined by the epicondylar axis relative to the posterior condylar line or the inner pegs of the femoral component. Nine studies [2, 3, 5, 18, 19, 21–23, 29] used CT scan at the level of the femoral epicondyles to determine the angle between the component posterior condylar line and the epicondylar axis (Fig. 2). Two other studies [20, 26] used the inner pegs of the femoral component to determine femoral component rotation (Fig. 3). When 3D-CT was used, the component’s posterior condylar line and the epicondylar axis were used as well (Fig. 4) [18, 19, 29].
Femur was aligned to the mechanical axis in coronal, the anatomical in sagittal and the femoral epicondylar axis in the transverse plane (a + e). The piriformis fossa was selected as the proximal point of the anatomical axis (b). A plane was fitted to the posterior surface of the anterior flange. Flexion/extension alignment of the femoral component was measured as the angle between this plane and the femoral anatomical axis (c). Femoral component rotation was measured as the angle between the epicondylar axis and posterior condylar axis (d). Varus–valgus alignment was measured as the angle between femoral distal surface and the mechanical axis (e) [18, 19]
Four studies reported levels of accuracy using intraclass correlation coefficients (ICC) [18, 19, 23, 29]. An ICC value of 1 indicates perfect reliability, 0.81–1.0 very good reliability, 0.61–0.80 good reliability, 0.41–0.6 is moderate and less than or 0.4 is poor [19].
Konigsberg et al. found a poor interobserver ICC for the femoral component of 0.386 and a good intraobserver ICC of 0.606 [23] measured with 2D-CT.
High levels of intra- and interobserver reliability were found in 3D measurements of femoral component rotation. Hirschmann et al. [18] reported a very good intraobserver (ICC of 0.93) and interobserver reliability (ICC 0.88). This corresponds with a variation of 2° (range 0°–5°) and 3° (range 0°–6°) for the intra- and interobserver reliability, respectively. These findings were comparable to Rasch et al. [29], who found a very good intraobserver reliability (ICC 0.84–0.99) and interobserver reliability (ICC 0.85–0.99) as well.
One study, by Hirschmann et al. [19], compared the inter- and intraobserver reliability for axial 2D- and 3D-CT images. These results show a poor interobserver reliability (ICC 0.29) when using 2D-CT in measuring the rotation of the femoral component. However, using 3D-CT significantly (p < 0.001) improves the interobserver reliability to a very good reliability (ICC 0.91) [19].
Four studies reported a reference range for femoral component rotation [2, 3, 5, 22].
To determine whether the femoral component is in excessive internal or external rotation, the original posterior condylar angle is generally used [5]. A native value of 3.5° (±1.2°) internal rotation of the posterior condylar angle in males and of 0.3° (±1.2°) in females, relative to the surgical epicondylar axis, is accepted [2, 3, 5].
Kim et al. [22] determined the neutral (optimal) alignment using an algorithm that examined the range of angles associated with the lowest failure rate and selected the narrowest range that had the greatest significance in their model using Cox regression analysis. Based on their retrospective cohort of 3048 TKA’s, no TKA required revision in the group with 2°–5° external rotation [22].
Measuring rotation of the tibial component
Seven 2D-CT studies [2, 3, 5, 20, 22, 23, 26] used five different techniques to measure tibial component rotation; four other studies used 3D-CT [18, 19, 29, 30].
In 2D-CT the most frequently used measurements are the posterior border of the tibial component in relationship to the geometric centre and tibial tubercle (Fig. 5) [3, 5, 23, 26].
Three cuts of the CT scan are required to define the rotational position of the tibial component relative to the tibial tubercle. a The most proximal cut of the CT scan passes through the component and defines the tibial component angle (TCA). b Immediately distal to the component a second cut is used to establish the geometric centre of the proximal tibia. c The most distal cut is performed through the tibial tubercle. Data from the preceding two images are superimposed on this image: (1) the geometric centre and (2) the TCA. One line is drawn from the apex of the tubercle to the geometric centre. The angle subtended by this line and the TCA is the rotational position of the tibial component [3, 5, 23, 26]
Bédard et al. [2] developed a modification of this technique (Fig. 6) to assess the rotational position of asymmetric tibial components.
Lines AB and DE cross the lateral and medial hemiplateau, respectively. Both are bisected. A third line, CF, connects the centres of each hemiplateau and defines the flexion axis for an asymmetric component. The line at right angles to the flexion axis (g), defines the TCA for an asymmetric component. The TCA is corrected for the angle formed by line g (flexion axis) and the line perpendicular to the posterior condylar axis [2]
Jazrawi et al. [20] determined tibial rotation using the angle formed between the posterior aspect of the tibial component and a line 2 cm below the joint line along the posterior condyles of the tibial specimens. Kim et al. [22] believed that the true rotational alignment of the tibial component may be affected by the mobile nature of the tibial bearing. They calculated tibial component rotation as the angle between the posterior margins of the proximal tibia and the tibial bearing [22].
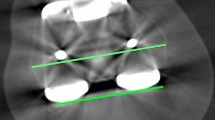
Prior to measurements, the tibia was aligned to the anatomical axis in the coronal and sagittal planes and posterior condylar axis (PCA) in the transverse plane (a, b). The tibial component rotation was measured as an angle between the PCA (black line) and the posterior tibial prosthesis (dotted red line) axes (b). A plane was fitted to the inferior surface of the tibial component (c). Image (d) shows the centre of the talus, which is the distal point of the tibial anatomical axis. The tibial varus/valgus and slope alignments were measured as angles between this plane (red dotted line) and the tibial anatomical axis (black line) (a, e) [18, 19]
The posterior condylar axis and the posterior border of the tibial prosthesis were also used in three studies using 3D-CT (Fig. 7) [18, 19, 29]. Roper et al. [30] used a different technique; they identified the centre of the tibial tray and the junction between the medial and middle thirds of the tibial tuberosity to define tibial component rotation.
The overall measurements for intraobserver and interobserver reliability were good (ICC 0.809 and ICC 0.67) according to Konigsberg et al. [23] for 2D-CT measurements.
3D-CT resulted in a higher ICC’s for both intra- and interobserver reliabilities. Hirschmann et al. [18, 19] reported a very good intraobserver reliability (ICC of 0.97 and 0.99) and interobserver reliability (ICC 0.95 and 0.99) in two studies. This corresponds with a variation of 1° (range 0°–4°) and 2° (range 0°–5°) for the intra- and interobserver reliability, respectively [18, 19]. These findings are in line with Roper et al. [30] who reported a very good intra- and interobserver reliability for the posterior angle (ICC 0.949 and 0.943) and for the centre angle (ICC 0.941 and 0.936) measurements.
Four included studies reported a reference range for tibial component rotation [2, 3, 5, 22]. The normal relationship between the orientation of the tibial tubercle and the tibial articular surface is used to determine whether the tibial component is in excessive internal or external rotation [5]. In general, a normal rotation value for the tibial component is 18° (±2.6°) of internal rotation from the tip of the tubercle, which corresponds to the native articular surface [2, 3, 5].
Kim et al. [22] determined neutral (optimal) alignment using an algorithm that examined the range of angles associated with the lowest failure rate. They selected the narrowest range with the greatest significance in their model using Cox regression analysis. In the group that showed an external rotation of 2°–5°, revision rate was only 0.04 %, based on their retrospective cohort of 3048 TKA’s [22].
Discussion
The most important finding of the present study is that 3D-CT provides the most accurately measurements, and no clear cut-off points for revision of TKA components can be given because of limited evidence. Besides, 3D-CT has very good intra- and interobserver reliabilities for both the femoral and tibial component. The femoral component rotation is merely assessed with respect to the epicondylar axis in both 2D- and 3D-CT protocols. Rotation measurements of the tibial component have been done in various ways. The majority of the studies used multiple transposed axial CT images of the tibia with different landmarks.
Component rotation, as introduced by Berger et al. [4], is performed on 2D axial slices of an unaligned CT scan. This method is considered to be less accurate as the position of the leg during scanning may influence the appearance of the epicondylar axis [17, 19]. Using 3D reconstructed images solves this problem. Moreover, 2D-CT only scans the distal femur and proximal tibia. We believe that functioning of the TKA depends on kinematics involving the upper and lower leg. Therefore, the entire leg should be taken into account in order to correctly measure the tibial and femoral component alignment, as being done in 3D-CT. Furthermore, knee kinematic can be affected by anatomical variations or femoral or tibial torsion. This can only be determined with total leg 3D-CT measurements [11, 37].
Following these thoughts, the study performed by Kim et al. [22] seems limited compared to the others because they do not refer to any anatomical landmarks. They used mobile-bearing rotation platform prosthesis in all cases. Tibial component rotation was defined as the angle formed by one line along the posterior margin of the tibial plateau and another line along the posterior margin of the tibial bearing [22]. They stated that the mobile nature of the tibial bearing may affect the true rotational alignment of the tibial component.
Unfortunately, only a few of the included studies described cut-off points for malrotation of the TKA components. Hence, no reliable conclusions can be drawn that substantiate revision of malrotated TKA components. This is in line with a recent study by Valkering et al. [35], who investigated the correlation between rotational alignment and functional outcome.
The normal posterior femoral condylar angle and the normal relationship between the orientation of the tibial tubercle and the tibial articular surface, as introduced by Berger et al. in 1993, are used as reference ever since. They distinguished gender differences for the native posterior condylar angle, based on a small cadaveric study [6]. Other studies could not confirm gender difference for the posterior condylar line, which makes decisions based on these measurements doubtful [9, 14, 15].
A limitation of this review is the quality of studies. All included studies were Level III evidence. Randomized controlled trials would have substantiated our conclusion with more certainty. However, to our knowledge, there were no randomized controlled trials available. Another limitation is the variety of methods for measuring tibial component rotation in 2D-CT, which could negatively influence a comparison with 3D-CT.
The findings arising from this systematic review show that 3D-CT provides the most accurate determination of TKA component rotation. The included studies are inconclusive regarding normative values on TKA component rotation because the cut-off points are still unclear. Thereby, anatomical reference points for measuring tibial component rotation still vary, and gender difference as introduced in the commonly used Berger protocol seem to be refuted. Based on this systematic review, one should be careful in drawing conclusions from CT rotation measurements. If rotational errors are suspected, after ruling out other causes for malfunctioning after TKA, 3D-CT should be used preferably.
Future research should focus on the ranges of normal component rotation after TKA and its anatomical landmarks.
Conclusions
Based on our systematic review, determination of component rotation after total knee arthroplasty should be performed by 3D reconstructed computed tomography. These images will help to define component position with high reliability. Although, only few studies investigated the use of 3D-CT. Consensus about the femoral component and its reference points seems to be present. Yet, for the tibial component, different techniques are used with similar results. No clear cut-off points for revision of malrotated TKA components can be given because of limited evidence. Therefore, future research must focus on anatomical landmarks and cut-off points of component rotation in TKA using 3D-CT.
Abbreviations
- TKA:
-
Total knee arthroplasty
- CENTRAL:
-
Cochrane Central Register of Controlled Trials
- CT:
-
Computed tomography
- ICC:
-
Intraclass correlation coefficients
- TCA:
-
Tibial component angle
References
Bäthis H, Perlick L, Tingart M et al (2004) Alignment in total knee arthroplasty: a comparison of computer-assisted surgery with the conventional technique. J Bone Jt Surg 86-B:682–687
Bédard M, Vince KG, Redfern J et al (2011) Internal rotation of the tibial component is frequent in stiff total knee arthroplasty. Clin Orthop Relat Res 469(8):2346–2355
Bell SW, Young P, Drury C et al (2014) Component rotational alignment in unexplained painful primary total knee arthroplasty. Knee 21:272–277
Berger RA, Crossett LS, Jacobs JJ et al (1998) Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res 356:144–153
Berger RA, Rubash HE (2001) Rotational instability and malrotation after total knee arthroplasty. Orthop Clin North Am 32(4):639–647
Berger RA, Rubash HE, Seel MJ et al (1993) Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res 286(1):40–47
Berger RA, Seel MJ, Schleiden M (1993) Computerized tomographic determination of the normal tibiofemoral rotational angle: a guide to tibial component alignment in TKA. Orthop Trans 17:1174
Berger RA, Seel MJ, Schleiden M (1993) Determination of femoral component rotation in total knee arthroplasty using computer tomography. Orthop Trans 17:427
Boisgard S, Moreau PE, Descamps S et al (2003) Computed tomographic study of the posterior condylar angle in arthritic knees: its use in the rotational positioning of the femoral implant of total knee prostheses. Surg Radiol Anat 25(3–4):330–334
Bourne RB, Chesworth BM, Davis AM et al (2010) Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 468(1):57–63
Buck FM, Guggenberger R, Koch PP et al (2003) Femoral and tibial torsion measurements with 3D models based on low-dose biplanar radiographs in comparison with standard CT measurements. AJR Am J Roentgenol 199(5):W607–W612
Ewald FC (1989) The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res 248:9–12
Fosco M, Rimondi E, Amendola L et al (2010) Revision of knee prostheses with components malrotation: treatment algorithm using a computed tomographic analysis. Eur Orthop Traumatol 1:61–68
Griffin FM, Insall JN, Scuderi GR (1998) The posterior condylar angle in osteoarthritic knees. J Arhtroplasty 13(7):812–815
Griffin FM, Math K, Scuderi GR et al (2000) Anatomy of the epicondyles of the distal femur: MRI analysis of normal knees. J Arhtroplasty 15(3):354–359
Harvie P, Larkin J, Scaddan M et al (2013) Stiffness after total knee arthroplasty: does component alignment differ in knees requiring manipulation? J Arhtroplasty 28(1):14–19
Henckel J, Richards R, Lozhkin K et al (2006) Very low-dose computed tomography for planning and outcome measurement in knee replacement. The imperial knee protocol. J Bone Jt Surg 88:1513–1518
Hirschmann MT, Iranpour F, Konala P et al (2010) A novel standardized algorith for evaluating patients with painful total knee arthroplasty using combined single photon emission tomography and conventional computerized tomography. Knee Surg Sports Traumatol Arthrosc 18:939–944
Hirschmann MT, Konala P, Amsler F et al (2011) The position and orientation of total knee replacement components: A comparison of conventional radiographs, transverse 2D-CT slices and 3D-CT reconstruction. J Bone Joint Surg 93-B(5):629–633
Jazrawi LM, Birdzell L, Kummer FJ et al (2000) The accuracy of computed tomography for determining femoral and tibial total knee artroplasty component rotation. J Arhtroplasty 15(6):761–766
Kanekasu K, Kondo M, Kadoya Y (2005) Axial radiograph of the distal femur to assess rotational alignment in total knee arthroplasty. Clin Orthop Relat Res 434:193–197
Kim YH, Park JW, Kim JS et al (2014) The relationship between the survival of total knee arthroplasty and postoperative coronal, sagittal and rotational alignment of knee prosthesis. Int Orthop 38:379–385
Konigsberg B, Hess R, Hartman C et al (2014) Inter- and intraobserver reliability of two-dimensional CT scan for total knee arthroplasty component malrotation. Clin Orthop Relat Res 472(1):212–217
Lakstein D, Zarrabian M, Kosashvili Y et al (2010) Revision total knee arthroplasty for component malrotation is highly beneficial: a case control study. J Arthroplasty 25(7):1047–1052
Longstaff LM, Sloan K, Stamp N et al (2009) Good alignment after total knee arthroplasty leads to faster rehabilitation and better function. J Arhtroplasty 24(4):570–578
Lützner J, Krummenauer F, Wolf C et al (2008) Computer-assisted and conventional total knee replacement. A comparative, prospective, randomised study with radiological and ct evaluation. J Bone Jt Surg 90-B(8):1039–1044
National Institutes of Health—Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies, 2014
OCEBM Levels of Evidence Working Group. The Oxford levels of evidence 2. Oxford Centre for Evidence-Based Medicine. http://www.cebm.net/ocebm-levels-of-evidence/
Rasch H, Falkowski AL, Forrer F et al (2013) 4D-SPECT/CT in orthopaedics: a new method of combined quantitative volumetric 3D analysis of SPECT/CT tracer uptake and component position measurements in patients after total knee arthroplasty. Skeletal Radiol 42:1215–1223
Roper GE, Bloemke AD, Roberts CC et al (2013) Analysis of tibial component rotation following total knee arthroplasty using 3D high definition computed tomography. J Arhtroplasty 28(8 Suppl):106–111
Scott CE, Howie CR, MacDonald D et al (2010) Predicting dissatisfaction following total knee replacement. J Bone Jt Surg 92:1253–1258
Sharkley PF, Hozack WJ, Rothman RH et al (2002) Why are total knee arthroplasties failing today? Clin Orthop Relat Res 404:7–13
Skyttä ET, Lohman M, Tallroth K et al (2009) Comparison of standard anteroposterior knee and hip-to-ankle radiographs in determining the lower limb and implant alignment after total knee arthroplasty. Scand J Surg 98:250–253
Sternheim A, Lochab J, Drexler M et al (2012) The benefit of revision knee arthroplasty for component malrotation after primary total knee replacement. Int Orthop 36(12):2473–2478
Valkering KP, Breugem SJ, van den Bekerom MP et al (2015) Effect of rotational alignment on outcome of total knee arthroplasty. Acta Orthop 86(4):432–439
Vanbiervliet J, Bellemans J, Verlinden C et al (2011) The influence of malrotation and femoral component material on patellofemoral wear during gait. J Bone Joint Surg 93-B(10):1348–1354
Yan M, Wang J, Wang Y et al (2014) Gender-based differences in the dimensions of the femoral trochlea and condyles in the Chinese population: correlation to the risk of femoral component overhang. Knee 21(1):252–256
Acknowledgments
We thank Chantal den Haan, medical librarian, for composing a complete and thorough search strategy based on our research questions.
Authors’ contributions
E.V. carried out the initial search with help of a medical librarian. E.V. and E.M. performed article selection independently and were responsible for composing the manuscript in the form of design, acquisition of data, analysis of data and interpretation. J.N. was mainly responsible for drafting the manuscript and critically evaluating the content. All authors have been involved in drafting the manuscript and revising it critically from time to time. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that they have no conflict of interest.
Funding
There is no funding source.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
None.
Rights and permissions
About this article
Cite this article
De Valk, E.J., Noorduyn, J.C.A. & Mutsaerts, E.L.A.R. How to assess femoral and tibial component rotation after total knee arthroplasty with computed tomography: a systematic review. Knee Surg Sports Traumatol Arthrosc 24, 3517–3528 (2016). https://doi.org/10.1007/s00167-016-4325-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-4325-5