Abstract
Purpose
To assess the diagnostic test accuracy of magnetic resonance imaging (MRI), magnetic resonance arthrography (MRA) and computed tomography arthrography (CTA) for the detection of chondral lesions of the patellofemoral and tibiofemoral joints.
Methods
A review of published and unpublished literature sources was conducted on 22nd September 2011. All studies assessing the diagnostic test accuracy (sensitivity/specificity) of MRI or MRA or CTA for the assessment of adults with chondral (cartilage) lesions of the knee (tibiofemoral/patellofemoral joints) with surgical comparison (arthroscopic or open) as the reference test were included. Data were analysed through meta-analysis.
Results
Twenty-seven studies assessing 2,592 knees from 2,509 patients were included. The findings indicated that whilst presenting a high specificity (0.95–0.99), the sensitivity of MRA, MRI and CTA ranged from 0.70 to 0.80. MRA was superior to MRI and CTA for the detection of patellofemoral joint chondral lesions and that higher field-strength MRI scanner and grade four lesions were more accurately detected compared with lower field-strength and grade one lesions. There appeared no substantial difference in diagnostic accuracy between the interpretation from musculoskeletal and general radiologists when undertaking an MRI review of tibiofemoral and patellofemoral chondral lesions.
Conclusions
Specialist radiological imaging is specific for cartilage disease in the knee but has poorer sensitivity to determine the therapeutic options in this population. Due to this limitation, there remains little indication to replace the ‘gold-standard’ arthroscopic investigation with MRI, MRA or CTA for the assessment of adults with chondral lesions of the knee.
Level of evidence
II.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Chondral lesions are considered a common cause of knee pain and can be difficult to differentiate clinically from meniscal injury [9, 13, 46]. Chondral lesions can be a source of pain and subsequent disability limiting the occupational and social pursuits of people [13, 21]. Furthermore, they are progressive in nature as the articular cartilage degenerates resulting in increased contact pressures on underlying subchondral bone [12]. With a variety of non-operative and operative treatment options, an accurate diagnosis is required to ensure that the optimal treatment strategy is tailored to each individual.
Magnetic resonance imaging (MRI) has gained favour as a diagnostic tool for intra-articular knee pathology over the past 20 years [18, 19]. Previous studies have demonstrated the high diagnostic accuracy of MRI protocols for the detection of meniscal and anterior cruciate ligament (ACL) disruption [7, 32, 41]. However, the use of MRI in the detection of chondral lesions is less widely accepted because of limitations in contrast resolution [24]. Recent developments in pulse sequences and increasing magnetic field-strength have led to improvements in contrast resolution [11].
Controversy exists regarding the accuracy of different imaging techniques for different grades of chondral lesion. Generally, MRI is considered more sensitive for the detection of deeper rather than more superficial lesions [13, 14]. Magnetic resonance arthrography (MRA) and computed tomography arthrography (CTA) can also be used to investigate intra-articular pathology affecting the knee [6, 47]. Both techniques have been used to diagnose chondral delamination of the hip [34, 53]. The addition of contrast agent delineates the cartilage surface to provide greater discrimination of cartilaginous lesions [36]. However, both MRA and CTA are less frequently used than conventional MRI for the detection of chondral lesions in the knee, because they are invasive and more expensive. Overall, the value of an accurate radiological measurement is considerable given the alternative is arthroscopic investigation, a more invasive and more expensive procedure [36].
The purpose of this study was to undertake a meta-analysis of the literature to assess the diagnostic test accuracy of MRI, MRA and CTA for chondral lesions of the patellofemoral and tibiofemoral joints. Examination of the grade of chondral lesion, location of lesion and image interpreter was assessed in addition to determining the optimal modality for imaging chondral lesions. This was justified since it has not been previously undertaken, whilst continuing controversy exists regarding the optimal imaging technique for this population.
Materials and methods
Search strategy
The primary search was based on the electronic databases: the Cochrane Central Register of Controlled Trials (in The Cochrane Library), MEDLINE, EMBASE, AMED, Biomed Central, CINAHL and Zetoc reviewed from their inception to 22 September 2011.
The unpublished or grey literature was searched using the electronic databases: OpenSIGLE (System for Information on Grey Literature in Europe), the WHO International Clinical Trials Registry Platform, Current Controlled Trials, UKCRN Portfolio Database, National Technical Information Service and the UK National Research Register Archive. The Boolean operators and MeSH and keyword search terms used for the MEDLINE search are presented in Table 1. These were amended for each search platform.
The reference lists of all potentially relevant papers were examined for initially missed studies. The corresponding author for each included study was contacted. Each was asked to review the search results and to highlight any additional papers that may have been initially omitted.
Study identification
Titles and abstracts were initially screened by one reviewer (TS). The shortlisted studies were then reviewed by a second reviewer (BD) to determine their eligibility according to the inclusion/exclusion criteria. The full texts of each potentially eligible paper were retrieved and subsequently reviewed by the two reviewers independently.
Eligibility criteria
Studies assessing the diagnostic test accuracy (sensitivity/specificity) of MRI or MRA or CTA for the assessment of adults with chondral (cartilage) lesions of the knee (tibiofemoral/patellofemoral joints) with surgical comparison (arthroscopic or open) as the reference test were included. Arthroscopy was included as a reference test since this has been suggested as the gold-standard in the diagnosis of cartilage lesions [1]. Studies assessing cadaveric knees or animal models were excluded. Studies that did not use surgery as the reference standard or did not aim to assess the diagnostic accuracy (sensitivity/specificity) were excluded.
Data collection/methodological quality assessment
Data from each eligible study were extracted by two reviewers independently (BD, TS). Data extracted included: sample size, cohort gender, average age, MRI, MRA, CTA, multi-detector computed tomography (MDCT) and surgical ‘reference’ procedure and the frequency of true positives, true negatives, false positives and false negatives for the index to reference test. If insufficient data were available, this was either calculated using summary estimates or the respective corresponding authors were contacted to obtain this.
The methodological quality of each paper was evaluated using the QUADAS (Quality Assessment of Diagnostic Accuracy Studies) criteria [50, 51]. Each reviewer (BD, TS) performed this independently. Any disagreements during the study identification, data extraction or methodological assessment processes were resolved through discussion between the two reviewers until consensus was met. Any unresolved disagreements were resolved by a third reviewer (AT) who acted as an adjudicator.
Analysis
Study heterogeneity was assessed by recording differences in study characteristics and methodological approaches using the data extraction tables. Data from studies that did not demonstrate substantial heterogeneity were pooled in meta-analyses.
The primary analysis was the assessment of sensitivity, specificity, likelihood ratios and diagnostic odds ratios for MRI, MRA and CTA using a random-effects meta-analysis. For each analysis, 95% confidence intervals (CI) were calculated. These were then compared with a summary Receiver Operating Characteristics plot (sROC) to determine the superior diagnostic test accuracy.
Secondary analyses included the assessment of diagnostic test accuracy for 0.5, 1.5 T compared with 3.0 T field-strength MRI; different grades of chondral lesions, and whether the diagnostic test accuracy differed dependent on the location of the chondral lesion, that is, patellofemoral or tibiofemoral. Finally, a comparison of the diagnostic test accuracy to image interpreter profession, that is, Radiologist versus Musculoskeletal (MSK) Radiologist versus Orthopaedic Surgeon, was planned.
All analyses were performed by one reviewer (TS) and conducted on Revman version 5.0 (The Nordic Cochrane Centre, The Cochrane Collaboration 2009, Copenhagen, Denmark) or Meta-Disc (Unit of Clinical Biostatistics, Ramón y Cajal Hospital, Madrid, Spain).
Results
Search results
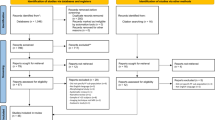
A total of 159 papers were identified from the search strategy. From these, 45 were considered of pertinent interest. After a review of the full texts, 27 were deemed eligible and included in the review. The results of the search strategy are summarised in a PRISMA flow-chart (Fig. 1).
Methodology appraisal
The results of the methodological assessment are presented in Table 2. Based on this, the methodological quality of the evidence appeared high. Strengths in the evidence included the recruitment of a clinically meaningful cohort by all studies, with 78% of studies clearly describing the subject selection process to recruit their cohorts. Furthermore, 85% of papers ensured that all eligible subjects received both reference and index tests, and in 89% of studies, subjects received the reference test irrespective of the result of the index test, indicating minimal risk of selection bias. Whilst the description of the conduct of each radiological investigation was clearly defined in 81% of studies, the surgical comparison was less frequently sufficiently defined (76%). Nonetheless, 81% of studies blinded the reviewer of the radiological examination to the surgical finding. However, blinding of the radiological findings to the surgeon was only ensured in 37% of studies. A recurrent limitation, noted in 89% of studies, was that limited clinical data were made available to the radiology reviewer, as would be expected in normal clinical practice.
Population characteristics
The cohort and radiological characteristics are summarised in Tables 3 and 4. The 27 studies reported the diagnostic test accuracy of 2,592 knees in 2,509 patients. Mean age of the cohort was 37.7 years, ranging from 19 years [28] to 57 years [49]. The duration between radiological assessment and surgical comparison was reported in 14 studies. This ranged from 1 day [35] to 12 months [12]. Only one study stated the size of chondral lesion, where the mean surface area for chondral lesions was reported as 1.992 cm2 [12].
Of the included studies, 26 studies assessed the accuracy of MRI, four assessed MRA whilst three assessed CTA. Of the 24 studies that used MRI and MRA, 19 reported the field-strength of their MR scanners. Investigations were conducted on 0.15 Tesla (T) magnetic resonance (MR) scanners in one study, 0.2 T in one, 0.3 T in one and 0.5 T in one study, respectively. Four studies reported using 1.0 T scanners, 10 studies used 1.5 T, whilst one paper reported using a 3.0 T MR scanner for their investigations (Table 3). Further information on radiological procedure and specific sequences and protocols used is presented in Tables 3 and 4.
The grading for chondral lesions was described as having been performed using two difference systems. Sixteen studies assessed chondral lesions using a 0–4 grading system as suggested by Shahriaree [43], where 0 equated homogenous intermediate signal intensity and cartilage normal; 1 focal thickening of cartilage with smooth surface or cartilage loss/softening of cartilage; 2 equating to focal bulging, fissuring, blister lesions or shallow ulceration with mild surface irregularities; grade 3 equates to surface irregularities with deep ulceration or fibrillation not extending to subchondral bone; and grade 4 equating to cartilage defect with exposure of subchondral bone [3, 4, 9, 10, 14, 15, 17, 21, 25, 28, 35, 42, 44, 48, 49, 52]. Nine studies assessed grade of lesion using a 0–3 point scale as recommended by Noyes and Stabler [31], where grade 0 was normal cartilage; grade 1 was assigned to cartilage with minor surface irregularities with early fissuring but no loss of thickness; grade 2 signified cartilage thinning with deep fissures but no full-thickness loss; and grade 3 equated to cartilage with at least one area of full-thickness loss [1, 16, 19, 22, 29, 37, 38, 45, 46]. Radiological assessment of grade of lesion was not assessed in two studies [14, 29].
The interpreter of each radiological image was stated in 23 studies. Images were reviewed by MSK radiologists in 12 studies, by general radiologists in 10 studies and by orthopaedic surgeons in one study.
Primary analysis: MRI versus MRA versus CTA
Overall, the specificity of radiological measurements was greater than their sensitivity for the detection of both patellofemoral and tibiofemoral joint lesions. The pooled meta-analysis indicated that MRA and CTA were superior in the detection of patellofemoral joint chondral lesions compared with MRI investigations (Table 5; Fig. 2). MRA reported a pooled sensitivity of 0.70 (95% CI: 0.57–0.81) and specificity of 0.99 (0.97–1.00), CTA sensitivity was 0.80 (95% CI: 0.70–0.88) and specificity 0.99 (95% CI: 0.95–1.00), whilst MRI reported a sensitivity of 0.74 (0.71–0.77) and a specificity of 0.95 (0.94–0.95).
There were insufficient data to compare the diagnostic test accuracy of the three investigations for the detection of tibiofemoral joint lesions. However, it was possible to assess the diagnostic test accuracy of MRI for patellofemoral compared with tibiofemoral lesions (Fig. 3). The sROC plot indicated superior diagnostic test accuracy for the detection of tibiofemoral over patellofemoral joint lesions (Fig. 3) with the tibiofemoral joint reported a sensitivity for 0.88 (95% CI: 0.86–0.89) and specificity of 0.82 (0.81–0.83), compared with 0.74 (95% CI: 0.71–0.77) and 0.95 (95% CI: 0.94–0.95) for patellofemoral joint sensitivity and specificity, respectively (Table 5).
Secondary analysis: MR field-strength
Whilst there were insufficient data to compare the effect of different field-strength MR scanners used for MRA investigations, the data permitted the comparison of 0.2–0.5 T, compared with 1.0 T, compared with 1.5 T MRI. The individual sensitivity, specificity and summary diagnostic odds ratio data indicated that there were superior sensitivity and specificity values for 1.0 T over 0.2–0.5 T or 1.5 T scanners (Table 6). There were insufficient data to compare these lower field-strength results with 3.0 T MRI findings using meta-analysis techniques.
Secondary analysis: grade of lesion
There was sufficient, homogenous data to analyse diagnostic test accuracy of MRI and MRA by grade of chondral lesion using the 0–4 point Shahriaree [43] system. The results of this analysis indicated that for the assessment of patellofemoral joint chondral lesions using MRI, grade I and II lesions reported the poorest diagnostic test accuracy, whilst grade IV reported the highest diagnostic test accuracy (Table 7). Whilst the sensitivity for all grades ranged from 0.66 to 0.68, specificity values ranged from 0.85 (95% CI: 0.81–0.89) for grade I lesions up to 0.99 (95% CI: 0.98–1.00) for grade IV lesions. Similarly, the trend for superior grade IV and inferior grade I lesion detection was reported for the MRA patellofemoral joint investigations (Table 7). However, this analysis indicated that the detection of grade III lesions was poorer with a sensitivity of 0.72 (95% CI: 0.51–0.88) and specificity of 0.98 (95% CI: 0.92–1.00) compared to grade II lesions with a sensitivity of 0.81 (95% CI: 0.58–0.95) and specificity of 0.98 (95% CI: 0.92–1.00).
There was a difference in the trend of results for the assessment of tibiofemoral lesions. Whilst grade IV lesions reported the highest diagnostic test accuracy with a sensitivity of 0.81 (95% CI: 0.76–0.84) and specificity of 0.99 (95% CI: 0.98–1.00), grade II and III lesions reported lower diagnostic test accuracy values compared to grade I lesion detection (Table 7).
Secondary analysis: image interpreter
There was insufficient data to compare the diagnostic test accuracy of musculoskeletal and conventional radiologists to orthopaedic surgeons. Furthermore, although there was insufficient data to compare the diagnostic test accuracy of MRA or CTA interpretation between musculoskeletal radiologists compared to general radiologists, it was possible to assess this domain with MRI. There was similar diagnostic accuracy between both groups of reviewers (Table 8). The sensitivity of MRI for assessing chondral lesions of the knee by a musculoskeletal radiologist was 0.64 (95% CI: 0.62–0.67) with a specificity of 0.96 (95% CI: 0.95–0.97) and a summary diagnostic odds ratio of 55.68 (95% CI: 24.47–126.67). The general radiologists reported comparable results with a sensitivity of 0.84 (95% CI: 0.82–0.85), specificity of 0.87 (95% CI: 0.86–0.88) and a summary diagnostic odds ratio value of 50.66 (95% CI: 30.60–83.85).
Discussion
The most important finding of the present study was that MRA is superior to MRI and CTA for the detection of chondral lesions in the patellofemoral joint, but that all three, whilst presenting with high specificity, have poorer sensitivity in diagnosing cartilage disease. Higher field-strength MRI machines are superior to lower field-strength and that higher-grade lesions are better detected than lower-grade ones. Finally, there is no difference in diagnostic accuracy between musculoskeletal and general radiologists when interpreting MRI to investigate tibiofemoral and patellofemoral chondral lesions.
Previous studies have cited sample size as a limiting factor to interpret radiological findings [21]. This meta-analysis aimed to address this limitation by appropriate pooling of data. However, due to the heterogeneity in methods of analysis and data presentation, it was only appropriate to undertake specific analyses by grade of lesion rather than more global grouped analyses of the diagnostic accuracy of a radiological examination for the detection of chondral lesions. Whilst large trials may still be warranted, this study provides some indication of the current limitations in the use of radiological imaging for the detection of tibiofemoral and patellofemoral chondral lesions.
A recurrent limitation to the studies was that the MRI results were available to the surgeons prior to the arthroscopic ‘reference standard’ procedure. A number of retrospective studies including Bredella et al. [3] and Disler et al. [9] reported that this was unavoidable since such imaging reports were part of routine clinical care at the time of the study. A second recurrent limitation was the lack of detail provided by papers regarding their arthroscopic technique. Broderick et al. [4] reported that they used a single arthroscopic portal. Using such a technique, the arthroscopic surgeon is unable to probe the cartilage to accurately assess chondromalacia or grade I lesions [4]. As a result studies that either adopted the single portal assessment technique or neglected to document this information may have either under or over diagnosed the presence of chondral lesions, questioning the appropriateness of their ‘gold-standard’ reference test. Bredella et al. [3] reported that because arthroscopy only visualises surfaces unless subchondral bone is exposed, estimating the depth of a lesions is inherently inaccurate [3, 23]. Finally, arthroscopy is operator-dependent and therefore the reliability of arthroscopy for the detection of chondral lesions may be affected by the training and experience of the orthopaedic surgeon who undertakes the reference standard [52].
The results indicated that lower-grade lesions had poorer diagnostic test accuracy than higher grade lesions for MRI and MRA. In addition, the pooled meta-analyses indicated that diagnostic test accuracy was greater for tibiofemoral compared with patellofemoral joint lesions on MRI (Fig. 3). Whilst the association of diagnostic accuracy with grade of chondral lesion concurred with Disler et al’s [9] results, they reported that the majority of their false negative chondral lesions were missed from the lateral tibial surface. Disler et al. [9] were unable to justify why lesions in this location were more difficult to detect. This may be attributed to the relatively low signal intensity of the cartilage in the tibial plateau because of the anisotropic arrangement of collagen [52]. The severity and depth of chondral changes is widely recognised as a limiting factor in the ability to detect these lesions with MRI [9, 15, 27, 30, 35]. Disler et al. [9] argued that the fat-suppressed 3D SPGR sequence they adopted allowed depiction of a trilaminar structural architecture of the hyaline cartilage which could facilitate the determination of lesion depth. Kawahara et al. [26] acknowledged that the reduced ability to detect lower-grade chondral lesions is primarily attributed to poor spatial resolution. They suggested that this could be improved by decreasing section thickness or intersectional gap, by increasing the matrix or by using 3D acquisition techniques [26]. However, given the overall limitation in the detection of grade I lesions, MRI can only be recommended for patients with suspected extensive chondral lesions and/or prolonged knee pain, and not for those with less severe lesions of a short duration [35].
Whilst not assessed directly in this study, the examination of associated damage to the subchondral bone may be of diagnostic use in the detection of chondral lesions. Friemert et al. [14] suggested that fat-suppressed MRI sequences might be superior to un-suppressed sequences because they are better able to demonstrate subchondral bone marrow oedema. Sclerosis or hyperaemia of the subchondral bone may also be associated with articular cartilage changes such as chondromalacia and fissuring [21]. Therefore, the ability to assess accurately for subchondral bone marrow signal changes may be an essential indicator of the degree of chondral damage, irrespective of the cartilage signal.
The accuracy of radiological imaging is paramount if such tools are used to plan definitive treatment. With the advent of microfracture or drilling, osteochondral grafting, autologous chondrocyte implantation and ultimately arthroplasty, the size and severity of chondral lesions needs to be accurately determined to decide whether an operative or non-operative management strategy is adopted [24]. Given the limitations in the diagnostic accuracy of conventional MR, based on fast spin echo and gradient echo pulse sequences, particularly for grade I and II lesions (Table 7), basing such decisions on radiological investigation rather than arthroscopy may not be advisable. However, this may change with the development of newer pulse sequences [52]. Furthermore, only one study reported the size of chondral lesion [12]. Consequently, it was not possible to determine whether this variable had an important effect on diagnostic test accuracy. Diagnostic accuracy is required to ensure the optimal treatment strategy for patients with chondral lesions [6, 36, 47]. Therefore, grading lesion size may be as important as the grading of severity in the decision-making about the treatment. Further reporting on the size of lesion is therefore important to evaluate this hypothesis.
The available literature assessing the use of MRA and CTA was limited. Only four studies have assessed the diagnostic test accuracy of MRA and three assessed CTA for the detection of knee chondral lesions. Given this, the analysis of such a small number of subjects may have been underpowered committing a type II statistical error [2]. This suggestion is supported by the wide confidence intervals demonstrated in Tables 5 and 7. However, the results of the pooled analysis indicated that MRA provided superior diagnostic test accuracy compared to CTA or MRI (Fig. 2). This was reflected in Gagliardi et al’s [15] study which reported that MRA and CTA were superior to conventional MR imaging, except for T2-weighted sequences, for detecting all grades of chondromalacia patellae. This difference was most obvious with grade I retropatellar chondral lesions [15]. This finding has been supported by cadaveric studies. Gylys-Morin et al. [20] reported that MRA was more sensitive than conventional MRI for the detection of defects which were 2 mm in diameter or larger. Furthermore Harman et al’s [21] supported this finding citing that MRA provides more accurate diagnosis of intermediate grades of chondromalacia patella compared to conventional MRI (P < 0.05). These findings were also reflected in the meta-analysis where higher grades of patellofemoral joint chondral lesion provided superior diagnostic test accuracy for MRA (Table 7).
The results indicated that there was similar diagnostic accuracy between musculoskeletal radiologists and general radiologists for MRI of knee chondral lesions (Table 8). However, this result may be confounded by the fact that there are no generally accepted criteria for distinguishing one from the other. None of the studies explicitly stated what qualifications their musculoskeletal radiologist had over and above a ‘general radiologists’. Furthermore, the sub-specialty of musculoskeletal radiology may not exist in all hospitals. Therefore, it may be that many ‘general radiologists’ have substantial specialist musculoskeletal experience if not the formal job title. This should be considered when interpreting these findings and when designing future trials on this area.
Pihlajamaki et al. [35] examined the clinical importance of MRI findings with patients with suspected chondromalacia patellae. They reported that there was no correlation between the presence of chondromalacia patellae and clinical symptoms. They also reported that severity of anterior knee pain did not correlate with the presence or severity of retropatellar chondral lesions, in contrast to previous literature [25]. Given this, and the low diagnostic test accuracy of grade I lesions, identifying which patients will be most appropriate for radiological imaging is therefore confusing [33, 39]. Further study to assess the appropriateness of imaging for these patients is therefore warranted.
The results of this study indicated that higher field-strength MR scanners provided greater diagnostic test accuracy compared to 0.2–0.5 T MR scanners (Table 6). It remains unclear whether higher field-strength machines such as 3.0 or 7.0 T MR scanners could provide greater accuracy and a more reliable diagnosis of chondral lesions of the tibiofemoral or patellofemoral joints. The advances of shorter acquisition times, improved signal-to-noise ratio and improved spatial resolution suggest that these higher field-strength MR machines may provide improved diagnostic capabilities [11]. Further studies examining this potential with 3.0 T field-strengths are anticipated.
An unexpected finding from these results was that 1.0 T MR scanners provided greater diagnostic test accuracy that 1.5 T machines. However, as Table 6 demonstrates, these findings were based on a small number of studies. Accordingly, these findings should be viewed with caution since its results may be underpowered for this subgroup analysis. Further investigation of the effects of field-strength on chondral lesion detection is therefore warranted particularly as extremity MR machines, with typical field-strengths in the order of 1.0 T, are becoming financially viable for many practices.
No studies were identified which compared a surgical reference standard to delayed gadolinium-enhanced MRI (DGEMRIC) [8]. This approach is gaining increasing attention with its potential ability to identify changes in the glycosaminoglycan content of articular cartilage before macroscopic changes in cartilage contours or signal changes on more conventional pulse sequences [5, 12, 38]. However, examination of the accuracy and clinical cost-effectiveness of DGEMRIC is in its infancy. Furthermore, as demonstrated in Table 3, a number of different sequences and protocols were used. The subgroup analyses were performed to minimise the risk of these providing inaccurate results in relation to the effects of field-strength, reviewer experience, and grade of lesion. However, there was insufficient data to be able to specifically examine the difference between different protocols within each imaging technique. It was therefore not possible to determine the optimal MRI, MRA or CTA procedure to detect these lesions, merely possible to identify the overall accuracy of these techniques. Given this, further prospective studies are required, based on these results, to determine the optimal sequence and imaging protocol for detection of chondral lesions of the knees.
Given the limited sensitivity of the radiological investigations assessed, there remains little indication to replace the use of arthroscopic investigations to diagnose chondral lesions. Surgical interventions may pose a greater risk of complications and at a higher financial cost to radiological examinations. However, the findings of this study do not support their substitution with MRI, MRA or CTA through a potentially greater risk of obtaining a false negative result to incorrectly inform clinical decision-making. Until the technology advances in imaging techniques, surgical intervention remains the ‘gold-standard’ to assess adults with possible chondral lesions of the tibiofemoral or patellofemoral joints.
Conclusions
Currently MRA, CTA and MRI can only be considered to be accurate for detecting the more advanced chondral lesions. The sensitivity for less severe lesions is limited. Further study to assess the diagnostic test accuracy of newer MR pulse sequences may be indicated to as the technology advances. Until then, there is little indication to replace the ‘gold-standard’ arthroscopic investigation with any of these radiological investigations.
References
Adams ME, Li DK, McConkey JP, Davidson RG, Day B, Duncan CP et al (1991) Evaluation of cartilage lesions by magnetic resonance imaging at 0.15 T: comparison with anatomy and concordance with arthroscopy. J Rheumatol 18:1573–1580
Bland M (2000) Introduction to medical statistics, 3rd edn. Oxford University Press, Oxford
Bredella MA, Tirman PF, Peterfy CG, Zarlingo M, Feller JF, Bost FW et al (1999) Accuracy of T2-weighted fast spin-echo MR imaging with fat saturation in detecting cartilage defects in the knee: comparison with arthroscopy in 130 patients. AJR Am J Roentgenol 172:1073–1080
Broderick LS, Turner DA, Renfrew DL, Schnitzer TJ, Huff JP, Harris C (1994) Severity of articular cartilage abnormality in patients with osteoarthritis: evaluation with fast spin-echo MR vs arthroscopy. AJR Am J Roentgenol 162:99–103
Burstein D, Gray M (2003) New MRI techniques for imaging cartilage. J Bone Joint Surg 85-A(Suppl 2):70–77
Cardello P, Gigli C, Ricci A, Chiatti L, Voglino N, Pofi E (2009) Retears of postoperative knee meniscus: findings on magnetic resonance imaging (MRI) and magnetic resonance arthrography (MRA) by using low and high field magnets. Skeletal Radiol 38:149–156
Crawford R, Walley G, Bridgman S, Maffulli N (2007) Magnetic resonance imaging versus arthroscopy in the diagnosis of knee pathology, concentrating on meniscal lesions and ACL tears: a systematic review. Br Med Bull 84:5–23
Crema MD, Roemer FW, Marra MD, Burstein D, Gold GE, Eckstein F et al (2011) Articular cartilage in the knee: current MR imaging techniques and applications in clinical practice and research. Radiographics 31:37–61
Disler DG, McCauley TR, Kelman CG, Fuchs MD, Ratner LM, Wirth CR et al (1996) Fat-suppressed three-dimensional spoiled gradient-echo MR imaging of hyaline cartilage defects in the knee: comparison with standard MR imaging and arthroscopy. AJR Am J Roentgenol 167:127–132
Disler DG, McCauley TR, Wirth CR, Fuchs MD (1995) Detection of knee hyaline cartilage defects using fat-suppressed three-dimensional spoiled gradient-echo MR imaging: comparison with standard MR imaging and correlation with arthroscopy. AJR Am J Roentgenol 165:377–382
Eckstein F, Charles HC, Buck RJ, Kraus VB, Remmers AE, Hudelmaier M et al (2005) Accuracy and precision of quantitative assessment of cartilage morphology by magnetic resonance imaging at 3.0 T. Arthritis Rheum 52:3132–3136
Figueroa D, Calvo R, Vaisman A, Carrasco MA, Moraga C, Delgado I (2007) Knee chondral lesions: incidence and correlation between arthroscopic and magnetic resonance findings. Arthroscopy 23:312–315
Flanigan DC, Harris JD, Trinh TQ, Siston RA, Brophy RH (2010) Prevalence of chondral defects in athletes’ knees: a systematic review. Med Sci Sports Exerc 42:1795–1801
Friemert B, Oberländer Y, Schwarz W, Häberle HJ, Bähren W, Gerngross H et al (2004) Diagnosis of chondral lesions of the knee joint: can MRI replace arthroscopy? A prospective study. Knee Surg Sports Traumatol Arthrosc 12:58–64
Gagliardi JA, Chung EM, Chandnani VP, Kesling KL, Christensen KP, Null RN et al (1994) Detection and staging of chondromalacia patellae: relative efficacies of conventional MR imaging, MR arthrography, and CT arthrography. AJR Am J Roentgenol 163:629–636
Ghanem I, Abou Jaoude S, Kharrat K, Dagher F (2002) Is MRI effective in detecting intraarticular abnormalities of the injured knee? J Med Liban 50:168–174
Giovagnoni A, Valeri G, Ercolani P, Paci E, Carloni S, Soccetti A (1995) Magnetic resonance arthrography in chondral disease of the knee. Radiol Med 90:219–225
Gold GE, Bergman AC, Pauly JM, Lang P, Butts RK, Beaulieu CF et al (1998) Magnetic resonance imaging of knee cartilage repair. Top Magn Imaging 9:377–392
Gückel C, Jundt G, Schnabel K, Gächter A (1995) Spin-echo and 3D gradient-echo imaging of the knee joint: a clinical and histopathological comparison. Eur J Radiol 21:25–33
Gylys-Morin VM, Hajek PC, Sartoris DJ, Resnick D (1987) Articular cartilage defects: detectability in cadaver knees with MR. AJR Am J Roentgenol 45:1153–1157
Harman M, Ipeksoy U, Dogan A, Arslan H, Etlik O (2003) MR arthrography in chondromalacia patellae diagnosis on a low-field open magnet system. Clin Imaging 27:194–199
Heron CW, Calvert PT (1992) Three-dimensional gradient-echo MR imaging of the knee: comparison with arthroscopy in 100 patients. Radiology 183:839–844
Hodler J, Resnick D (1992) Chondromalacia patellae. AJR Am J Roentgenol 158:106–107
Hughes RJ, Houlihan-Burne DG (2011) Clinical and MRI considerations in sports-related knee joint cartilage injury and cartilage repair. Semin Musculoskelet Radiol 15:69–88
Kawahara Y, Uetani M, Nakahara N, Doiguchi Y, Nishiguchi M, Futagawa S, Kinoshita Y et al (1998) Fast spin-echo MR of the articular cartilage in the osteoarthritic knee. Correlation of MR and arthroscopic findings. Acta Radiol 39:120–125
Kettunen JA, Visuri T, Harilainen A, Sandelin J, Kujala UM (2005) Primary cartilage lesions and outcome among subjects with patellofemoral pain syndrome. Knee Surg Sports Traumatol Arthrosc 13:131–134
Lee SH, Suh JS, Cho J, Kim SJ (2001) Evaluation of chondromalacia of the patella with axial inversion recovery-fast spin-echo imaging. J Magn Reson Imaging 13:412–416
Macarini L, Perrone A, Murrone M, Marini S, Stefanelli M (2004) Evaluation of patellar chondromalacia with MR: comparison between T2-weighted FSE SPIR and GE MTC. Radiol Med 108:159–171
Magee T, Shapiro M, Williams D (2004) Usefulness of simultaneous acquisition of spatial harmonics technique for MRI of the knee. AJR Am J Roentgenol 182:1411–1415
Murphy BJ (2001) Evaluation of grades 3 and 4 chondromalacia of the knee using T2* weighted 3D gradient echo articular cartilage images. Skeletal Radiol 30:305–311
Noyes FR, Stabler CL (1989) A system for grading articular cartilage lesions at arthroscopy. Am J Sports Med 17:505–513
Oei EH, Nikken JJ, Verstijnen AC, Ginai AZ, Hunink MGM (2003) MR imaging of the menisci and cruciate ligaments: a systematic review. Radiology 226:837–848
Outerbridge RE (1961) The etiology of chondromalacia patellae. J Bone Joint Surg 43-B:752–757
Perdikakis E, Karachalios T, Katonis P, Karantanas A (2011) Comparison of MR-arthrography and MDCT-arthrography for detection of labral and articular cartilage hip pathology. Skeletal Radiol 40:1441–1447
Pihlajamäki HK, Kuikka PI, Leppänen VV, Kiuru MJ, Mattila VM (2010) Reliability of clinical findings and magnetic resonance imaging for the diagnosis of chondromalacia patellae. J Bone Joint Surg 92-A:927–934
Rand T, Brossmann J, Pedowitz R, Ahn JM, Haghigi P, Resnick D (2000) Analysis of patellar cartilage. Comparison of conventional MR imaging and MR and CT arthrography in cadavers. Acta Radiol 41:492–497
Recht MP, Piraino DW, Paletta GA, Schils JP, Belhobek GH (1996) Accuracy of fat-suppressed three-dimensional spoiled gradient-echo FLASH MR imaging in the detection of patellofemoral articular cartilage abnormalities. Radiology 198:209–212
Recht M, Bobic V, Burstein D, Disler D, Gold G, Gray M (2001) Magnetic resonance imaging of articular cartilage. Clin Orthop Relat Res 391:S379–S396
Reiser M, Karpf PM, Bernett P (1982) Diagnosis of chondromalacia patellae using CT arthrography. Eur J Radiol 2:181–186
Riel KA, Reinisch M, Kersting-Sommerhoff B, Hof N, Merl T (1999) 0.2-Tesla magnetic resonance imaging of internal lesions of the knee joint: a prospective arthroscopically controlled clinical study. Knee Surg Sports Traumatol Arthrosc 7:37–41
Rosas HG, De Smet AA (2009) Magnetic resonance imaging of the meniscus. Top Magn Reson Imaging 20:151–173
Russell GGQ, Johnson M, Johnston DWC, Arnett G, Swersky J (1994) Imaging studies in surgically proven chondromalacia patellae. Clin J Sport Med 4:11–13
Shahriaree H (1985) Chondromalacia. Contemp Orthop 11:27–39
Spahn G, Wittig R, Kahl E, Klinger HM, Mückley T, Hofmann GO (2007) Evaluation of cartilage defects in the knee: validity of clinical, magnetic-resonance-imaging and radiological findings compared with arthroscopy. Unfallchirurg 110:414–424
Tyrrell RL, Gluckert K, Pathria M, Modic MT (1988) Fast three-dimensional MR imaging of the knee: comparison with arthroscopy. Radiology 166:865–872
Vallotton JA, Meuli RA, Leyvraz PF, Landry M (1995) Comparison between magnetic resonance imaging and arthroscopy in the diagnosis of patellar cartilage lesions: a prospective study. Knee Surg Sports Traumatol Arthrosc 3:157–162
Vande Berg BC, Lecouvet FE, Poilvache P, Maldague B, Malghem J (2002) Spiral CT arthrography of the knee: technique and value in the assessment of internal derangement of the knee. Eur Radiol 12:1800–1810
von Engelhardt LV, Lahner M, Klussmann A, Bouillon B, Dàvid A, Haage P et al (2010) Arthroscopy vs. MRI for a detailed assessment of cartilage disease in osteoarthritis: diagnostic value of MRI in clinical practice. BMC Musculoskelet Disord 20:75
von Engelhardt LV, Schmitz A, Burian B, Pennekamp PH, Schild HH, Kraft CN (2008) 3-Tesla MRI vs. arthroscopy for diagnostics of degenerative knee cartilage diseases: preliminary clinical results. Orthopade 37:914–922
Whiting P, Rutjes AW, Dinnes J, Reitsma J, Bossuyt PM, Kleijnen J (2004) Development and validation of methods for assessing the quality of diagnostic accuracy studies. Health Technol Assess 8:1–234
Whiting PF, Weswood ME, Rutjes AW, Reitsma JB, Bossuyt PN, Kleijnen J (2006) Evaluation of QUADAS, a tool for the quality assessment of diagnostic accuracy studies. BMC Med Res Methodol 6:9
Yoshioka H, Stevens K, Hargreaves BA, Steines D, Genovese M, Dillingham MF et al (2004) Magnetic resonance imaging of articular cartilage of the knee: comparison between fat-suppressed three-dimensional SPGR imaging, fat-suppressed FSE imaging, and fat-suppressed three-dimensional DEFT imaging, and correlation with arthroscopy. J Magn Reson Imaging 20:857–864
Zaragoza E, Lattanzio PJ, Beaule PE (2009) Magnetic resonance imaging with gadolinium arthrography to assess acetabular cartilage delamination. Hip Int 19:18–23
Acknowledgments
We would like to thank the Information Services at the University of East Anglia, UK, for their assistance in gathering the papers required for this study.
Conflict of interest
No author declares a competing interest to this paper.
Author information
Authors and Affiliations
Corresponding author
Additional information
Registration: CRD42011001342.
Rights and permissions
About this article
Cite this article
Smith, T.O., Drew, B.T., Toms, A.P. et al. Accuracy of magnetic resonance imaging, magnetic resonance arthrography and computed tomography for the detection of chondral lesions of the knee. Knee Surg Sports Traumatol Arthrosc 20, 2367–2379 (2012). https://doi.org/10.1007/s00167-012-1905-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-012-1905-x