Abstract
Purpose
Condylar lift-off can induce excessive polyethylene wear after total knee arthroplasty (TKA). A computer simulation was used to evaluate the influence of femoral varus alignment and lateral collateral ligament (LCL) laxity on lift-off after single-design TKA. It was hypothesised that proper ligament balancing and coronal alignment would prevent lift-off.
Methods
The computer model in this study is a dynamic musculoskeletal program that simulates gait up to 60° of knee flexion. The lift-off phenomenon was defined as positive with an intercomponent distance of >2 mm. In neutrally aligned components in the coronal plane, the femoral and tibial components were set perpendicular to the femoral and tibial mechanical axis, respectively. The femoral coronal alignment was changed from neutral to 5° varus in 1° increments. Simultaneously, the LCL length was elongated from 0 to 5 mm in 1-mm increments to provide a model of pathological slack.
Results
Within 2° of femoral varus alignment, lift-off did not occur even if the LCL was elongated by up to 5 mm. However, lift-off occurred easily in the stance phase in femoral varus alignments of >3° with slight LCL slack. The contact forces of the tibiofemoral joint were influenced more by femoral varus alignment than by LCL laxity.
Conclusions
Aiming for neutral alignment in severely varus knees makes it difficult to achieve appropriate ligament balance. Our study suggests that no lift-off occurs with excessive LCL laxity alone in a neutrally aligned TKA and therefore that varus alignment should be avoided to decrease lift-off after TKA.
Level of evidence
Case series, Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Appropriate soft tissue balance and alignment are important factors for good knee function, component durability, and patient satisfaction after total knee arthroplasty (TKA) [11, 22, 34]. Fluoroscopic analysis has shown that the condylar lift-off phenomenon, defined as excessive joint space opening, can occur after TKA [4, 7, 8, 14, 30, 31]. Condylar lift-off can induce various complications such as excessive polyethylene wear [10, 20]. Proper ligament balancing is crucial for preventing postoperative condylar lift-off [7, 14, 27].
Achieving both proper balance and alignment of ligaments is sometimes difficult in knees with severe deformity. One study reported that medial–lateral soft tissue imbalance was larger in patients with greater preoperative varus deformity [32]. Aiming for neutral alignment in a severe varus knee may make it difficult to achieve equal medial and lateral gaps because of looseness on the lateral side. Ligamentous release is an effective surgical technique to solve this problem, but it is especially difficult for measured resection techniques to adjust the ligamentous tension throughout knee flexion in cases with significant ligamentous imbalance [28, 32]. The surgeon’s experience may thus be important in this procedure due to the difficulty in obtaining measurements in dynamic clinical situations.
Many authors have investigated the potential causes of condylar lift-off. Nilsson et al. [31] were the first to show that asymmetrical subsidence and tilting of the tibial component could cause condylar lift-off due to an imbalanced bearing load. Stiehl et al. [41] later reported that lateral condylar lift-off in midflexion reflected an abnormality in lateral joint laxity. Insall et al. [14] subsequently suggested the importance of coronal ligamentous stability in terms of lessening condylar lift-off during knee flexion after posterior cruciate ligament-substituted (PS) TKA. On the other hand, Hamai et al. [12] demonstrated that sufficient coronal stability and alignment did not cause more significant condylar lift-off during knee extension in a single-leg stance after posterior cruciate-retaining TKA. Thus, condylar lift-off remains unavoidable when only the implant design is modified, and it is not known precisely how much operative uncertainty is permitted, although it is accepted that the surgeon must allow some degree of ligamentous imbalance and coronal malalignment.
A musculoskeletal computer model was recently introduced as a potentially effective tool for simulating pathological conditions after TKA, such as the effects of malposition of the femoral and tibial components [23, 24] or implant-bone impingement in deep flexion [25, 26]. Cadaver and clinical studies subsequently validated the accuracy of such computer simulations [25, 26].
This study used a musculoskeletal computer simulation of level walking to evaluate the influence of collateral ligament balance and femoral coronal alignment on the occurrence of condylar lift-off under various pathological conditions after PS TKA. While malrotation of the femoral component might cause more lift-off in flexion, this study focused on lift-off in extension. It was hypothesised that proper ligamentous balancing and coronal alignment would prevent condylar lift-off during gait. In addition, the allowable ranges of ligamentous imbalance and malalignment on condylar lift-off were also evaluated.
Materials and methods
The musculoskeletal computer simulation model used in this study (LifeMOD/KneeSIM 2010; LifeModeler Inc., San Clemente, CA) is a dynamic, musculoskeletal modelling program of the knee. The computer simulation was used to simulate the period-two gait cycle. This model included tibiofemoral and patellofemoral contact, lateral collateral ligament (LCL), medial collateral ligament (MCL), elements of the knee capsule, quadriceps muscle and tendon, patellar tendon, and hamstring muscles. The hamstrings in this model acted as single muscle, including all flexor functions, and were attached to the posterior centre of the proximal tibia. The LCL comprised a single bundle, and the MCL comprised anterior and posterior bundles [18, 42, 44]. All ligament bundles were modelled as nonlinear springs with material properties obtained from a published report [5]. The hip joint was modelled as a revolute joint parallel to the flexion axis of the knee and was allowed to slide vertically. The ankle joint was modelled as a combination of several joints that allowed free translation in the medial–lateral direction and free rotation in the flexion, axial, and varus–valgus directions.
The insertion point origins, stiffness, and length patterns for each ligament were based on the relevant anatomical literature [18, 21, 33, 45]. The proximal attachment points of the LCL and MCL were defined as the most prominent points of their respective femoral epicondyles. The distal attachment points of the LCL and MCL were adjusted to the tip of the fibular head and the midpoint between the tibial attachments of the anterior and posterior bundles, respectively. The stiffness coefficients of the LCL, anterior MCL, and posterior MCL were determined as 59, 63, and 63 N/mm, respectively, based on reported values [35, 42]. The attachments of and slack in each ligament were finely adjusted [3].
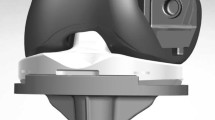
The KneeSIM program uses the Parasolid geometry of the femoral and tibial components, as well as tibial and patellar inserts for analysis. Parasolid models of a fixed-bearing flat design PS TKA (NexGen LPS-Flex; Zimmer, Warsaw, USA), including a patellar component, were imported into the program.
In aligning the components in the coronal plane, the femoral component was set perpendicular to the mechanical axis that connected the centre of the knee and the centre of the femoral head, and the tibial component was set perpendicular to the mechanical axis that connected the centre of the knee and the centre of the ankle joint. For the sagittal alignment, the femoral component was aligned to the distal anatomical axis of the femur, and the tibial component was aligned to the proximal anatomical axis of the tibia with a 7° posterior slope. The neutral rotational alignments of the femoral and tibial components were positioned in line with the femoral epicondylar axis and the tibial anteroposterior axis, respectively.
Previous studies have reported that the peak tibiofemoral contact force in TKA patients is about three times the body weight [9, 38]. In the testing conditions, a constant vertical force corresponding to a body weight of 80 kg was converted into about 2500 N (i.e. about three times the installed weight) loading on the bicondylar joint of the knee. This was applied at the hip. A closed-loop controller monitored knee flexion and compared it with the prescribed input. The quadriceps and hamstring loads were adjusted to obtain the prescribed flexion angle at each time point. Previous studies reported that the maximum quadriceps force in flexion reached 3.5 times the body weight [38, 39] and that the quadriceps force in flexion was similar to the patellofemoral contact forces. The peak quadriceps force in this study was 1753 N (i.e. double the installed weight) in a neutral alignment and was similar to the patellofemoral contact force (1311 N). The peak force of the hamstrings in this study was set at 178 N. It was confirmed that the collateral ligament tension during the ACL-deficient gait in this simulation was similar to that in a previous study [36].
The z axis (+: proximal, −: distal) of the simulation model was defined as the extension of the tibial axis. The plane normal to the z axis at the centre of the knee was defined as the xy plane. The x axis (+: lateral, −: medial) was defined as the extension of the femoral epicondylar axis, which was projected onto the xy plane along the z axis. The y axis (+: anterior, −: posterior) was defined as the extension of the tibial anteroposterior axis, which was perpendicular to the x axis and was projected onto the xy plane. The tibiofemoral contact force was a compressive joint reaction force perpendicular to the tibial insert against the femoral component. The anterior and posterior bundles of the MCL were modelled as two strands, each with identical characteristics, which split the total force at the start-up position. The modelled systems were subjected to the period-two gait cycle up to 60° knee flexion [17] (Fig. 1). Measured values in the second gait cycle were selected because the first gait cycle was slightly unstable for fitting the bounding conditions of each intercomponent joint. The tibiofemoral kinematics of the current study were very similar to those of a previous study that sought to validate a tibiofemoral kinematics simulation using fluoroscopic data [1].
It was determined that condylar lift-off was positive when the measured intercomponent distance between the femoral and tibial components was >2 mm during the gait cycle. To investigate the relationships between condylar lift-off, coronal alignment, and excessive lateral joint laxity, the femoral coronal alignment and the LCL length were changed from this standard setting. The LCL length was elongated from 0 mm (free length) to 5 mm in 1-mm increments as pathological slack without changing the femoral and tibial attachments. Simultaneously, the femoral coronal alignment was also changed between 0° and 5° varus in 1° increments. The femoral varus alignment was changed at the centre of the femoral component in the coronal plane. Condylar lift-off was measured as the distance between the femoral component and the tibial insert projected onto the xz plane. The measurement results in this study are presented with one decimal place because our simulation system could calculate each value with at least this degree of accuracy. Tibiofemoral contact forces were measured under the same testing conditions, in which the vanishing point of the tibiofemoral contact force was the start of condylar lift-off.
Results
The incidence and peak amount of lift-off (mm) with changes in slack of the LCL and femoral varus alignment are shown Table 1. Within 2° of femoral varus alignment, condylar lift-off did not occur even if the LCL distance was elongated by up to 5 mm. By contrast, with 3° of femoral varus alignment, condylar lift-off occurred with 1 mm of slack in the LCL in the late stance phase of the gait cycle, and the distance was 2.8 mm (Fig. 2). With up to 4° of femoral varus alignment, condylar lift-off occurred easily and without slack in the LCL (Fig. 3). The combination of 5° of femoral varus alignment and 5 mm of slack in the LCL caused the maximum condylar lift-off from the early stance phase to the late stance phase.
Schemas showing the tibiofemoral contact forces under three different conditions: a standard condition, b 3° varus and 1-mm slack condition, and c 5° varus and 5-mm slack condition during gait. The black arrows represent the phase at which the tibiofemoral contact force of the lateral condyle disappears (i.e. lateral femoral condylar lift-off)
Peak contact forces (N) of the lateral and medial tibiofemoral joints were not affected by changes in LCL slack. By contrast, peak tibiofemoral contact forces of the lateral condyle decreased gradually (Table 2) and peak tibiofemoral contact forces of the medial condyle increased progressively with increases in femoral varus alignment (Table 3).
Discussion
The most important finding of this study was that condylar lift-off could be avoided with the use of precise surgical technique. In the computer simulation study, condylar lift-off was closely related to ligamentous balancing and coronal alignment. Previous studies have suggested that proper rotation of the femoral component seems to lessen the incidence of condylar lift-off because of better coronal stability [7, 14], but few studies have examined the influence of coronal malalignment on condylar lift-off. A cadaver study reported that a varus deformity of only 3° substantially unloaded the lateral compartment [6]. Bertin et al. [4] also reported that condylar lift-off occurred predominantly at the lateral condyle. Therefore, the amount of lateral condylar lift-off was measured with various amounts of lateral joint laxity and increased varus alignment. The effects of ligamentous balancing and coronal alignment on condylar lift-off have been evaluated separately in previous reports [6, 7, 14, 15]. However, it was expected that the combination of these factors would be important in influencing condylar lift-off. Musculoskeletal computer models are very useful for evaluating various factors because it is difficult to evaluate such combinations in a clinical study. Ours is the first study to evaluate the combined effect of ligamentous balancing and coronal alignment on condylar lift-off using a specific implant design.
The extent of condylar lift-off is an important issue. Sharma et al. [37] reported that the amount of condylar lift-off was larger in the midflexion range in a limited knee flexion group than in a high knee flexion group. Nakahara et al. [29] reported that about 1.5 mm of condylar lift-off did not affect clinical results measured by the new Knee Society Score questionnaire. Consequently, it was determined that condylar lift-off >2 mm was pathological, and the tibiofemoral contact forces were also measured as an estimate of patient discomfort.
It was found in our study that no condylar lift-off occurred in neutral coronal alignment regardless of excessive collateral ligament laxity. A recent study [43] reported that mild varus alignment was associated with better clinical and functional outcomes compared with neutral alignment after TKA for varus deformity. The authors also suggested that undercorrection to an approximately pre-arthritic alignment as proposed by Bellemans et al. [2] might cause less release of knee ligaments. In the current study, however, condylar lift-off occurred easily in >3° varus alignment with slight slack in the LCL. More than 3° varus alignment should be avoided to prevent condylar lift-off. Our results are consistent with those reported by Hamai et al. [12], who examined the influence of varus–valgus laxity and coronal alignment on condylar lift-off during walking and found that lift-off hardly occurred in a well-aligned TKA. The force pattern during the gait cycle in our study is also consistent with that of a previous study by Stiehl et al. [40], who reported that 90 % of the 20 subjects after TKA demonstrated significant condylar lift-off during the single-leg stance of gait but not on heel strike. Our study also detected higher peak contact forces in the medial tibiofemoral joint on heel strike and lateral condylar lift-off during the single-leg stance. The contact forces at the tibiofemoral joint were influenced more by the degree of varus alignment than by the amount of LCL slack. A 5° varus alignment caused 1.5 times the medial tibiofemoral contact force as the neutral alignment.
Implant design is an important factor affecting the occurrence of condylar lift-off. A previous study reported that the incidence of condylar lift-off was greater using the PS design than using the posterior cruciate-retaining design with the restraining effect of the posterior cruciate ligament [19]. Other studies reported no statistically significant difference in the incidence of condylar lift-off between the two designs [8, 16].
There are important limitations to our study. First, a virtual and variable model with general knee joint was comprised in this simulation, and the material properties for soft tissues were obtained from relevant cadaver studies. Second, although fine adjustments were made to the stiffness, length patterns, and slack of each ligament based on the relevant anatomical literature, our model may not have strictly simulated TKA for various knee deformities because of the absence of definitive data for each material property in knees with severe osteoarthritis. Third, this computer simulation did not directly measure the adduction moment in each setting. A biomechanics study reported that varus knees had significantly greater peak knee adduction moments than neutral knees [13]. In our model, the ground reaction force was applied along the mechanical axis of the leg (the centre of the femoral head to the centre of the ankle). Therefore, it was considered that the adduction moment increased with greater femoral varus alignment. Further, this study evaluated only one representative model and could not detect the influence of various proximal offsets of the femur. The magnitude of this offset is an important factor causing condylar lift-off in the coronal plane because it affects the adduction moment. Finally, our analysis used component data with only one fixed-bearing flat design for PS TKA and did not consider a malrotation model of the femoral component.
The clinical relevance of this study is that excessive varus alignment should be avoided to prevent postoperative condylar lift-off, especially if LCL laxity remains during TKA.
Conclusions
These computer simulation findings suggest that no condylar lift-off occurred in neutral coronal alignment regardless of excessive collateral ligament laxity, and therefore, varus alignment should be avoided to decrease lift-off after TKA.
References
Banks SA, Hodge WA (2004) 2003 Hap Paul Award paper of the International Society for Technology in Arthroplasty. J Arthroplasty 19:809–816
Bellemans J, Colyn W, Vandenneucker H, Victor J (2012) The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res 470:45–53
Belvedere C, Ensini A, Feliciangeli A, Cenni F, D’Angeli V, Giannini S, Leardini A (2012) Geometrical changes of knee ligaments and patellar tendon during passive flexion. J Biomech 45:1886–1892
Bertin KC, Komistek RD, Dennis DA, Hoff WA, Anderson DT, Langer T (2002) In vivo determination of posterior femoral rollback for subjects having a NexGen posterior cruciate-retaining total knee arthroplasty. J Arthroplasty 17:1040–1048
Blankevoort L, Kuiper JH, Huiskes R, Grootenboer HJ (1991) Articular contact in a three-dimensional model of the knee. J Biomech 24:1019–1031
Bourne RB, Finlay JB, Papadopoulos P, Rorabeck CH, Andreae P (1984) In vitro strain distribution in the proximal tibia. Effect of varus-valgus loading in the normal and osteoarthritic knee. Clin Orthop Relat Res 188:285–292
Dennis DA, Komistek RD, Kim RH, Sharma A (2010) Gap balancing versus measured resection technique for total knee arthroplasty. Clin Orthop Relat Res 468:102–107
Dennis DA, Komistek RD, Walker SA, Cheal EJ, Stiehl JB (2001) Femoral condylar lift-off in vivo in total knee arthroplasty. J Bone Joint Surg Br 83:33–39
D’Lima DD, Patil S, Steklov N, Chien S, Colwell CW Jr (2007) In vivo knee moments and shear after total knee arthroplasty. J Biomech 40(Suppl):S11–S17
Feng EL, Stulberg SD, Wixson RL (1994) Progressive subluxation and polyethylene wear in total knee replacements with flat articular surfaces. Clin Orthop Relat Res 299:60–71
Halewood C, Risebury M, Thomas NP, Amis AA (2014) Kinematic behaviour and soft tissue management in guided motion total knee replacement. Knee Surg Sports Traumatol Arthrosc 22:3074–3082
Hamai S, Miura H, Okazaki K, Shimoto T, Higaki H, Iwamoto Y (2014) No influence of coronal laxity and alignment on lift-off after well-balanced and aligned total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22:1799–1804
Hunt MA, Birmingham TB, Giffin JR, Jenkyn TR (2006) Associations among knee adduction moment, frontal plane ground reaction force, and lever arm during walking in patients with knee osteoarthritis. J Biomech 39:2213–2220
Insall JN, Scuderi GR, Komistek RD, Math K, Dennis DA, Anderson DT (2002) Correlation between condylar lift-off and femoral component alignment. Clin Orthop Relat Res 403:143–152
Kim SH, Lee HJ, Jung HJ, Lee JS, Kim KS (2013) Less femoral lift-off and better femoral alignment in TKA using computer-assisted surgery. Knee Surg Sports Traumatol Arthrosc 21:2255–2262
Komistek RD, Scott RD, Dennis DA, Yasgur D, Anderson DT, Hajner ME (2002) In vivo comparison of femorotibial contact positions for Press-Fit posterior stabilized and posterior cruciate-retaining total knee arthroplasties. J Arthroplasty 17:209–216
Laassel EM, Loslever P, Angue JC (1992) Patterns of relations between lower limb angle excursions during normal gait. J Biomed Eng 14:313–320
LaPrade RF, Bollom TS, Wentorf FA, Wills NJ, Meister K (2005) Mechanical properties of the posterolateral structures of the knee. Am J Sports Med 33:1386–1391
Lee SY, Matsui N, Kurosaka M, Komistek RD, Mahfouz M, Dennis DA, Yoshiya S (2005) A posterior-stabilized total knee arthroplasty shows condylar lift-off during deep knee bends. Clin Orthop Relat Res 435:181–184
Lewis P, Rorabeck CH, Bourne RB, Devane P (1994) Posteromedial tibial polyethylene failure in total knee replacements. Clin Orthop Relat Res 299:11–17
Liu F, Gadikota HR, Kozanek M, Hosseini A, Yue B, Gill TJ, Rubash HE, Li G (2011) In vivo length patterns of the medial collateral ligament during the stance phase of gait. Knee Surg Sports Traumatol Arthrosc 19:719–727
Matsuzaki T, Matsumoto T, Kubo S, Muratsu H, Matsushita T, Kawakami Y, Ishida K, Oka S, Kuroda R, Kurosaka M (2014) Tibial internal rotation is affected by lateral laxity in cruciate-retaining total knee arthroplasty: an intraoperative kinematic study using a navigation system and offset-type tensor. Knee Surg Sports Traumatol Arthrosc 22:615–620
Mihalko WM, Conner DJ, Benner R, Williams JL (2012) How does TKA kinematics vary with transverse plane alignment changes in a contemporary implant? Clin Orthop Relat Res 470:186–192
Mihalko WM, Williams JL (2010) Computer modeling to predict effects of implant malpositioning during TKA. Orthopedics 33:71–75
Mizu-Uchi H, Colwell CW Jr, Fukagawa S, Matsuda S, Iwamoto Y, D’Lima DD (2012) The importance of bony impingement in restricting flexion after total knee arthroplasty: computer simulation model with clinical correlation. J Arthroplasty 27:1710–1716
Mizu-uchi H, Colwell CW Jr, Matsuda S, Flores-Hernandez C, Iwamoto Y, D’Lima DD (2011) Effect of total knee arthroplasty implant position on flexion angle before implant-bone impingement. J Arthroplasty 26:721–727
Moro-oka TA, Shiraishi H, Iwamoto Y, Banks SA (2010) Modified gap-balancing technique in total knee arthroplasty: evaluation of the post-operative coronal laxity. Knee Surg Sports Traumatol Arthrosc 18:375–380
Mullaji AB, Shetty GM (2013) Surgical technique: computer-assisted sliding medial condylar osteotomy to achieve gap balance in varus knees during TKA. Clin Orthop Relat Res 471:1484–1491
Nakahara H, Okazaki K, Hamai S, Okamoto S, Kuwashima U, Higaki H, Iwamoto Y (2014) Does knee stability in the coronal plane in extension affect function and outcome after total knee arthroplasty? Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-014-3122-2
Nakamura S, Sharma A, Kobayashi M, Ito H, Nakamura K, Zingde SM, Nakamura T, Komistek RD (2014) 3D in vivo femoro-tibial kinematics of tri-condylar total knee arthroplasty during kneeling activities. Knee 21:162–167
Nilsson KG, Karrholm J (1993) Increased varus-valgus tilting of screw-fixated knee prostheses. Stereoradiographic study of uncemented versus cemented tibial components. J Arthroplasty 8:529–540
Okamoto S, Okazaki K, Mitsuyasu H, Matsuda S, Iwamoto Y (2013) Lateral soft tissue laxity increases but medial laxity does not contract with varus deformity in total knee arthroplasty. Clin Orthop Relat Res 471:1334–1342
Park SE, DeFrate LE, Suggs JF, Gill TJ, Rubash HE, Li G (2005) The change in length of the medial and lateral collateral ligaments during in vivo knee flexion. Knee 12:377–382
Paternostre F, Schwab PE, Thienpont E (2014) The difference between weight-bearing and non-weight-bearing alignment in patient-specific instrumentation planning. Knee Surg Sports Traumatol Arthrosc 22:674–679
Robinson JR, Bull AM, Amis AA (2005) Structural properties of the medial collateral ligament complex of the human knee. J Biomech 38:1067–1074
Shao Q, MacLeod TD, Manal K, Buchanan TS (2011) Estimation of ligament loading and anterior tibial translation in healthy and ACL-deficient knees during gait and the influence of increasing tibial slope using EMG-driven approach. Ann Biomed Eng 39:110–121
Sharma A, Dennis DA, Zingde SM, Mahfouz MR, Komistek RD (2014) Femoral condylar contact points start and remain posterior in high flexing patients. J Arthroplasty 29:945–949
Sharma A, Komistek RD, Ranawat CS, Dennis DA, Mahfouz MR (2007) In vivo contact pressures in total knee arthroplasty. J Arthroplasty 22:404–416
Sharma A, Leszko F, Komistek RD, Scuderi GR, Cates HE Jr, Liu F (2008) In vivo patellofemoral forces in high flexion total knee arthroplasty. J Biomech 41:642–648
Stiehl JB, Dennis DA, Komistek RD, Crane HS (1999) In vivo determination of condylar lift-off and screw-home in a mobile-bearing total knee arthroplasty. J Arthroplasty 14:293–299
Stiehl JB, Komistek RD, Dennis DA, Paxson RD, Hoff WA (1995) Fluoroscopic analysis of kinematics after posterior-cruciate-retaining knee arthroplasty. J Bone Joint Surg Br 77:884–889
Sugita T, Amis AA (2001) Anatomic and biomechanical study of the lateral collateral and popliteofibular ligaments. Am J Sports Med 29:466–472
Vanlommel L, Vanlommel J, Claes S, Bellemans J (2013) Slight undercorrection following total knee arthroplasty results in superior clinical outcomes in varus knees. Knee Surg Sports Traumatol Arthrosc 21:2325–2330
Warren LFMJ, Girgis F (1974) The prime static stabilizer of the medial side of the knee. J Bone Joint Surg Am 56:665–674
Wijdicks CA, Ewart DT, Nuckley DJ, Johansen S, Engebretsen L, Laprade RF (2010) Structural properties of the primary medial knee ligaments. Am J Sports Med 38:1638–1646
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Kuriyama, S., Ishikawa, M., Nakamura, S. et al. No condylar lift-off occurs because of excessive lateral soft tissue laxity in neutrally aligned total knee arthroplasty: a computer simulation study. Knee Surg Sports Traumatol Arthrosc 24, 2517–2524 (2016). https://doi.org/10.1007/s00167-015-3687-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3687-4