Abstract
Purpose
To compare clinical outcomes after high-flex versus conventional total knee arthroplasty (TKA).
Methods
A systematic review and meta-regression were performed to compare post-operative outcomes between the two types of prostheses. Relevant randomized controlled trials were identified from MEDLINE and Scopus up to November, 2014.
Results
Fourteen of 369 studies were eligible; 14, 7, 6, 5, 3, 12 and 7 studies were included in the pooling of maximum knee flexion, Knee Society Knee Score (KS), Knee Society Function Score (FS), Hospital for Special Surgery score (HSS), short-form (SF) physical activity score, post-operative complications (DVT, fractures, infection) and revision TKA, respectively. The high-flex TKA had 1.97° [95 % confidence interval (CI) 0.37, 3.57], −0.86 (95 % CI −1.65, 0.07) and −1.34 (−2.57, −0.11) higher mean maximum knee flexion, KS and FS when compared to conventional TKA. However, there were non-significant differences in HSS, SF-36 (physical), complications and revision TKA.
Conclusion
This study suggests that there are improvements in post-operative knee range of motion and knee scores in high-flex TKA implants when compared to conventional TKA implants; however, the difference was very small and therefore might not have any clinical impact. Therefore, conventional TKA can be used as a substitute. However, cost-effective analysis should be performed to make appropriate selections in the future. There are no statistically significant differences in terms of HSS, quality of life, complications and revisions between the groups.
Level of evidence
I.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Restoration of knee flexion is an important factor in determining the functional outcome after total knee arthroplasty (TKA) [20]. A recent study showed that while wearing a range of motion (ROM) monitor for 35 consecutive hours, patients flexed their knees >90° for <0.5 % of the time and >120° for <0.1 % of the time [17]. Many efforts have been made to improve ROM including new prostheses designs (e.g. high-flex prostheses designs). The use of the new prostheses requires an additional 2-mm bone cut from the posterior femoral condyles, which leads to a greater curvature of the posterior condyles (NexGen LPS-Flex implant, NexGen LPS-Flex gender implant and RP or RP-F implant [8, 19, 21]). The tibial insert has an anterior cut to avoid patellar tendon impingement during deep flexion (RP or RP-F implant [8] and Genesis II PS implant [12]). However, outcomes of the high-flex and standard posterior-stabilized prostheses are inconsistent. Some studies [12, 15, 19, 20] show benefits with the use of the high-flexion posterior-stabilized total knee prosthesis with regard to ROM and clinical and radiographic outcomes, as well as maximum knee flexion. However, other studies [8, 14, 22] do not. A previous meta-analysis [13] including five randomized controlled trials (RCTs) [10, 12, 15, 21, 22] found that no clinically relevant or statistically significant improvement was obtained in flexion with the “high-flex” prostheses, whereas another meta-analysis that included nine RCTs [1, 6, 9, 10, 14, 15, 19, 21, 22], in which there were pooled outcomes of only one prosthesis design, found that NexGen LPS-Flex had a greater ROM without severe complications when compared to the NexGen LPS implant. A more recent meta-analysis [5] including ten studies pooled outcomes of ROM, KSS, HSS and quality of life scores demonstrated that no obvious statistical difference was found between high-flex prosthesis and standard prosthesis groups in terms of post-operative range of flexion, clinical scores and quality of life outcomes. However, this meta-analysis did not consider other clinically relevant outcomes (e.g. complication and revision rates), risk of bias assessment was not performed, and sources of heterogeneity (e.g. age, sex and body mass index and use of different prostheses) were not explored and assessed. Moreover, four RCTs [1, 9, 14, 20] that have since been published were not included in this meta-analysis, making it necessary to perform a further analysis containing these latest RCTs. Therefore, this systematic review and meta-analysis of high-flex and conventional TKA were conducted with the aim to update the comparison of the two for ROM and functional outcomes and to add further comparisons for quality of life and revision rates.
Materials and methods
MEDLINE and Scopus databases were used for identifying relevant studies published in English since the date of inception to 12 November 2014. The PubMed and Scopus search engines were used to locate studies with the following search terms: total knee arthroplasty and high flex. Search strategies for MEDLINE and Scopus are described in detail in the “Appendix” section. References from the reference lists of included trials and previous systematic reviews were also explored.
Selection of studies
Identified studies were first selected based on titles and abstracts by two independent authors (J. K. and A. A.). Full papers were retrieved if a decision could not be made from the abstracts. Disagreements were resolved by consensus and discussion with a third party (P. P.). Reasons for ineligibility or exclusion of studies were recorded and described.
Inclusion criteria
Randomized controlled trials that compared clinical outcomes between high-flex design and conventional design in primary TKA were eligible if they met following criteria:
-
Compared clinical outcomes between high-flex design and conventional design in primary TKA.
-
Compared at least one of the following outcomes: knee ROM in flexion and extension, Knee Society Knee Score (KS) and Knee Society Function Score (FS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score, Hospital for Special Surgery (HSS) score, short-form quality of life assessment (e.g. SF-12, SF 36), complications [infection, deep vein thrombosis (DVT), fracture] and revision rates.
-
Had sufficient data to extract and pool, i.e. the reported mean, standard deviation (SD), the number of subjects according to treatments for continuous outcomes and the number of patients according to treatment for dichotomous outcomes.
Data extraction
Two reviewers (J. K. and A. A.) independently performed data extraction using standardized data extraction forms. General characteristics of the study [i.e. mean age, gender, body mass index (BMI), mean follow-up time, ROM, functional scores (KS, FS, HSS), quality of life scores (SF-12, SF-36) at baseline] were extracted. The number of subjects, mean and SD of continuous outcomes [i.e. knee ROM, Knee Score (KS), Function Score (FS), HSS score and WOMAC score] between groups were extracted. Cross-tabulated frequencies between treatment and all dichotomous outcomes (complications and revisions) were also extracted. Any disagreements were resolved by discussion and consensus with a third party (P. P.).
Risk of bias assessment
Two authors (J. K. and A. A.) independently assessed risk of bias for each study following suggestions in the PRISMA guideline [11]. Six domains were assessed, including sequence generation, allocation concealment, blinding (participant, personnel and outcome assessors), incomplete outcome data, selective outcome reporting and other sources of bias. Disagreements between two authors were resolved by consensus and discussion with a third party (P. P.). Level of agreement for each domain and the overall domains were assessed using the Kappa statistics.
Outcomes
The outcomes of interests included knee ROM, knee function, quality of life, rates of complications and revision rates. These outcomes were measured as reported in the original studies, which were ROM for maximum knee flexion; Knee Score (KS), Function Score (FS) and HSS score for function. For knee ROM, higher values are equivalent to better outcomes. For the functional and quality of life scores including KS (0–100), FS (0–100), HSS (0–100) and SF physical activities (0–100) scores, higher scores reflect better functional and physical activities. Post-operative complications (infection, deep vein thrombosis, fracture) and revision rates were considered.
Statistical analysis
For continuous outcomes (i.e. knee ROM, KS, FS, HSS and SF), the mean difference between high-flex design and conventional design in TKA was estimated for each study. Unstandardized mean difference was applied for pooling outcomes across studies. Before pooling, intervention effects were assessed on whether they varied or were heterogeneous across included studies. Heterogeneity of mean differences was checked using the Q statistic, and the degree of heterogeneity was also quantified using the I 2 statistic. If heterogeneity was significant or I 2 > 25 %, the unstandardized mean difference was estimated using a random-effects model, and otherwise a fixed-effects model was applied.
For dichotomous outcomes, the odds ratio (OR) for complications (infection, deep vein thrombosis, fracture) and for revision was estimated for each study. Heterogeneity of ORs across studies was assessed using the same method as mentioned previously. If heterogeneity was present, the random-effects model by Dersimonian and Laird method was applied for pooling ORs, and otherwise the fixed-effects model by inverse variance method was applied.
Meta-regression was applied for exploring the cause of heterogeneity by fitting a co-variable [e.g. mean age, BMI, follow-up time, type of surgery (unilateral or bilateral), preoperative ROM and percentage of female] in the meta-regression model. Subgroup or sensitivity analysis was then performed according to the results of meta-regression. Publication bias was assessed using contour funnel plots [16, 17] and Egger’s tests [4]. Asymmetry of the funnel plot might be due to some missing studies where results that were negative might not have been published and thus could not be identified. The meta-trim and fill method was used to estimate the number of studies that might be missing and to adjust the pooled estimate [3]. All analyses were performed using STATA version 13.0. P value <0.05 was considered statistically significant, except for the test of heterogeneity where <0.10 was used.
Results
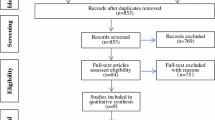
Sixty-nine and 373 studies were identified from MEDLINE and Scopus, respectively (Fig. 1); 73 studies were duplicates, leaving 369 studies to review titles and abstracts. Of these, 13 full papers [1, 2, 6, 8–10, 12, 14, 15, 18–20, 22] plus one study [21] identified from reference list were reviewed, leaving a total of 14 studies for data extraction. Characteristics of the 14 studies [1, 2, 6, 8–10, 12, 14, 15, 18–22] are described in Table 1. All 14 studies were RCTs that reported post-operative ROM for maximum knee flexion. Knee function was reported using the Knee Society Knee Score in seven studies [2, 6, 9, 10, 14, 19, 21], the Knee Society Function Score in six studies [2, 6, 9, 14, 15, 19], HSS score in five studies [2, 6, 10, 19, 22] and short-form physical activity score in three studies [6, 12, 15]. Post-operative complications included DVT, fractures and infection in 12 studies [2, 6, 8–10, 12, 14, 15, 19–22] and revision after TKA in seven studies [6, 8, 9, 14, 19, 20, 22]. Mean age (SD), BMI (SD), median (range) follow-up of participants and percentages of female gender were 67.3 (2.6) years, 28.9 (2.9), 2 (1–10.3) years and 58 (25–100) %, respectively. Mean preoperative ROM of maximum knee flexion was 114.7 (7.5)°. One study [14] compared mobile-bearing high-flex TKA implants versus mobile-bearing conventional TKA implants and fixed-bearing high-flex TKA implants versus fixed-bearing conventional TKA implants. Most studies [1, 2, 6, 8–10, 12, 14, 15, 18, 19, 21, 22] were posterior-stabilized TKA implants with only one study [20] comparing posterior-stabilized and cruciate-retaining TKA implants. Nine studies [1, 6, 9, 10, 14, 15, 19, 21, 22] compared the NexGen LPS-Flex implant and NexGen LPS implants, whereas five other studies [2, 8, 12, 18, 20] compared NexGen LPS-Flex and CR ACG implants, RP flex and RP, Genesis II flex and Genesis II implants, NexGen LPS-Flex implants and PFC sigma implants, respectively. Ten studies [1, 6, 8, 12, 14, 15, 18, 21, 22] performed unilateral TKA, four studies [9, 10, 19, 20] performed bilateral TKA, and one study [2] performed both unilateral and bilateral TKA.
Risk of bias in included studies
Risk of bias is described in Table 2.
Outcome
Post-operative knee range of motion for maximum knee flexion
Fourteen studies [1, 2, 6, 8–10, 12, 14, 15, 18–22] compared the mean values of maximum knee flexion between high-flex and conventional TKA (Table 3). The pooled UMD varied moderately across studies (I 2 = 55.5 %) and was 2.0 (95 % CI 0.37, 3.57), i.e. mean maximum knee flexion had a 2.0° statistically significant difference between two implants (Fig. 2). Separately fitting co-variables in a meta-regression analysis and none of the co-variables could explain the heterogeneity. Subgroup analysis (Fig. 3) was performed for the two studies [8, 12] with the RP flex implant compared with RP, and Genesis II flex compared with Genesis II; both showing no heterogeneity (I 2 = 0 %). It was also done for the 12 studies [1, 2, 6, 9, 10, 14, 15, 18–22] with NexGen LPS-Flex implants (I 2 = 61.4 %). The corresponding means for maximum knee flexion were 0.9 (95 % CI −1.63, 3.35) and 2.3 (95 % CI 0.40, 4.15).
Knee Society Knee Score
Seven studies [2, 6, 9, 10, 14, 19, 21] reported mean KSs between high-flex and conventional TKA groups (Table 3). Mean difference was similar across studies with an UMD of −0.9 (95 % CI −1.65, −0.06), indicating that the high-flex TKA group had statistically significant difference in KS when compared to conventional TKA group (Fig. 4).
Knee Society Function Score
Six studies [2, 6, 9, 14, 15, 19] compared mean FS between high-flex and conventional TKA groups (Table 3). The pooled UMD was −1.3 (95 % CI −2.57, −0.11) with statistically significant difference in functional score in high-flex TKA when compared to conventional TKA with mild heterogeneity (I 2 = 30.3 %, Fig. 4).
Hospital for Special Surgery score
Five studies [2, 6, 10, 19, 22] reported mean HSS scores between high-flex and conventional TKA groups (Table 3). Mean difference was similar across studies (I 2 = 0 %) with an UMD of −0.04 (95 % CI −1.02, 0.94), indicating that the high-flex TKA group had similar HSS scores to the conventional TKA group (Fig. 4).
Short form (physical activities)
Three studies [6, 12, 15] reported mean SF scores between high-flex and conventional TKA groups. Mean difference was similar across studies (I 2 = 27 %) with an UMD of 0.9 (95 % CI −0.37, 2.23), indicating that the high-flex TKA group had similar HSS scores to the conventional TKA group (Table 3; Fig. 4).
Complications and revision
Twelve studies [2, 6, 8–10, 12, 14, 15, 19–22] reported occurrences of fracture and DVT within the high-flex and conventional TKA groups (Table 4). Risk of fracture infection and DVT between two groups was similar (I 2 = 0 %, Fig. 5) with a pooled RR of 1.00 (0.29, 3.42), indicating that the chance of having a fracture infection and DVT between the two groups was not significantly different (Table 4; Fig. 5).
Seven studies [6, 8, 9, 14, 19, 20, 22] reported revision TKA after the high-flex and conventional TKA groups (Table 4). Risk of revision TKA between the two groups was similar (I 2 = 0 %, Fig. 5) with a pooled OR of 1.0 (0.29, 3.42), indicating that the chance of requiring a revision TKA and having post-operative infection between the two groups was not significantly different (Table 4; Fig. 5).
Neither contour funnel nor Egger’s test suggested evidence of publication bias for all outcomes (Fig. 6).
Discussion
The most important finding of the present study was high-flex TKA implants have about 2° of significant difference in outcomes of ROM when compared to conventional TKA implants. However, these reviews include three different high-flex implant designs. After subgroup analysis, the results show that patients who received NexGen LPS-Flex TKA implants had approximately 2.3° significantly higher post-operative knee flexion than those who had conventional TKA implants. However, the two implants showed no statistically significant difference in post-operative knee flexion ROM in patients who received RP flex and Genesis II flex TKA implants. In terms of function, quality of life, complication and revision outcomes, the high-flex TKA implants have approximately one point more of a significant difference in outcomes of Knee Society Knee Score, Knee Society Function Score than do conventional TKA implants, whereas the HSS score, short-form physical activities score, complications and revision after operation showed no statistical differences. After all outcomes were pooled and the sources of heterogeneity were explored by meta-regression analysis, the differences in implant designs were shown to have no effect on all outcomes.
Post-operative ROM and function were assessed by maximum knee flexion, Knee Society Knee Score and Knee Society Function Score, demonstrating that high-flex TKA had better outcomes than conventional TKA. These differences were not detected in the previous meta-analysis [5]. This review included four additional studies with 771 subjects and reached a power of 90 % for detecting the two-point difference in ROM between the two groups, with a type I error of 1 %. Although this study detected a statistically significant difference in maximum knee flexion, Knee Society Knee Score and Knee Society Function Score, the difference was very small and therefore might not have any clinical impact. Therefore, conventional TKA can be used as a substitute if the price of high-flex TKA is very high or if it is not available. However, cost-effective analysis should be performed to make appropriate selections in the future.
This study has several strengths. First of all, 14 studies were included for pooling relevant clinical outcomes (i.e. post-operative range of motion, functional scores, quality of life score, complications and revision) after total knee arthroplasty. The power to detect differences or equivalences between the two implants is 90 % or higher with false-positive results of only 1 %. Secondly, possible causes of heterogeneity were explored if covariate data at baseline (e.g. mean age, percentage of female, BMI, follow-up times, unilateral or bilateral TKA, preoperative ROM and implants design) were available. Third, publication bias for each outcome was also assessed. Most studies had a mean follow-up time of about 1–10 years; thus, long-term effects of TKA are still in question. Quality of evidence was also assessed for each outcome [7]. The quality of evidence was intermediate strength for all outcomes but may be capable of upgrading to high strength for the post-operative ROM if the range of estimation is more precise without heterogeneity and publication bias.
Conclusion
This meta-analysis indicated a higher post-operative knee ROM and function for high-flex prostheses that was not detected in the previous meta-analysis. However, the difference is very small and might not have any clinical impact. In terms of implants with different designs, quality of life, complication and revision TKA, this review demonstrated that only NexGen LPS-Flex can improve post-operative range of motion, whereas other designs cannot. There were no statistically significant differences in SF physical activities score and risk of having complications and revision TKA in both groups. These results are generally homogeneous and robust to publication bias and thus should be generalizable.
References
Ahmed I, Gray AC, Van Der Linden M, Nutton R (2009) Range of flexion after primary TKA: The effect of soft tissue release and implant design. Orthopedics 32(11):811
Choi WC, Lee S, Seong SC, Jung JH, Lee MC (2010) Comparison between standard and high-flexion posterior-stabilized rotating-platform mobile-bearing total knee arthroplasties: a randomized controlled study. J Bone Joint Surg Am 92(16):2634–2642
Duval S, Tweedie R (2000) Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56(2):455–463
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634
Fu H, Wang J, Zhang W, Cheng T, Zhang X (2014) No clinical benefit of high-flex total knee arthroplasty. A meta-analysis of randomized controlled trials. J Arthroplasty. doi:10.1016/j.arth.2014.10.032
Guild GN, Labib SA (2014) Clinical outcomes in high flexion total knee arthroplasty were not superior to standard posterior stabilized total knee arthroplasty. A multicenter, prospective, randomized study. J Arthroplasty 29(3):530–534
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schunemann HJ, Group GW (2008) GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336(7650):924–926
Hamilton WG, Sritulanondha S, Engh CA (2011) Prospective randomized comparison of high-flex and standard rotating platform total knee arthroplasty. J Arthroplasty 26(Suppl 6):28–34
Kim YH, Park JW, Kim JS (2012) High-flexion total knee arthroplasty: survivorship and prevalence of osteolysis: results after a minimum of ten years of follow-up. J Bone Joint Surg Am 94(15):1378–1384
Kim YH, Sohn KS, Kim JS (2005) Range of motion of standard and high-flexion posterior stabilized total knee prostheses: a prospective, randomized study. J Bone Joint Surg Am 87(7):1470–1475
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6(7):e1000100
McCalden RW, MacDonald SJ, Bourne RB, Marr JT (2009) A randomized controlled trial comparing “high-flex” vs “standard” posterior cruciate substituting polyethylene tibial inserts in total knee arthroplasty. J Arthroplasty 24(6 Suppl):33–38
Mehin R, Burnett RS, Brasher PMA (2010) Does the new generation of high-flex knee prostheses improve the post-operative range of movement? A meta-analysis. J Bone Joint Surg Br 92(10):1429–1434
Nieuwenhuijse MJ, van der Voort P, Kaptein BL, van der Linden, van der Zwaag HM, Valstar ER, Nelissen RG (2013) Fixation of high-flexion total knee prostheses: five-year follow-up results of a four-arm randomized controlled clinical and roentgen stereophotogrammetric analysis study. J Bone Joint Surg Am 95(19):e1411–e14111
Nutton RW, Van Der Linden ML, Rowe PJ, Gaston P, Wade FA (2008) A prospective randomised double-blind study of functional outcome and range of flexion following total knee replacement with the NexGen standard and high flexion components. J Bone Joint Surg Br 90(1):37–42
Palmer TM, Peter JL, Sutton AJ, Moreno SG (2008) Contour-enhanced funnel plots for meta-analysis. Stata J 8(2):242–254
Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L (2008) Contour-enhanced meta-analysis funnel plots help distinguish publication bias from other causes of asymmetry. J Clin Epidemiol 61(10):991–996
Seng C, Yeo SJ, Wee JL, Subanesh S, Chong HC, Lo NN (2011) improved clinical outcomes after high-flexion total knee arthroplasty. A 5-year follow-up study. J Arthroplasty 26(7):1025–1030
Singh H, Mittal V, Nadkarni B, Agarwal S, Gulati D (2012) Gender-specific high-flexion knee prosthesis in Indian women: a prospective randomised study. J Orthop Surg (Hong Kong) 20(2):153–156
Thomsen MG, Husted H, Otte KS, Holm G, Troelsen A (2013) Do patients care about higher flexion in total knee arthroplasty? A randomized, controlled, double-blinded trial. BMC Musculoskelet Disord 14:127
Weeden SH, Schmidt R (2007) A randomized, prospective study of primary total knee components designed for increased flexion. J Arthroplasty 22(3):349–352
Wohlrab D, Hube R, Zeh A, Hein W (2009) Clinical and radiological results of high flex total knee arthroplasty: a 5 year follow-up. Arch Orthop Trauma Surg 129(1):21–24
Acknowledgments
All authors declare no funding source or sponsor involvement in the study design, collection, analysis and interpretation of the data, in writing the manuscript and in submission of the manuscript for publication.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Search Strategies
MEDLINE
-
((total knee arthroplasty) AND (high flex))
Scopus
#1 total knee arthroplasty
#2 high flex
#3 #1 and #2
Rights and permissions
About this article
Cite this article
Arirachakaran, A., Wande, T., Pituckhanotai, K. et al. Clinical outcomes after high-flex versus conventional total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 23, 1610–1621 (2015). https://doi.org/10.1007/s00167-015-3557-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3557-0