Abstract
Purpose
To evaluate the sonoelastographic features of Achilles tendon healing after percutaneous treatment using real-time sonoelastography, a new tool able to quantify deformation in biological tissues.
Methods
Patients with atraumatic Achilles tendon ruptures, treated with a percutaneous technique, were assessed. Sonoelastographic evaluations were performed at the myotendinous junction, tendon body/lesion site and osteotendinous junction, both for the operated and contralateral side, at 40 days, 6 months and 1 year after surgery. Using standard regions of interest, the “strain index” (SI) was calculated as an indicator of tendon elasticity. Clinical outcomes were assessed by the ATRS questionnaire at 6 months and 1 year post-operatively and correlated with sonoelastographic findings. Sixty healthy tendons from 30 volunteers were used to provide a healthy control range.
Results
Twenty-five patients were recruited for this study. The SI in treated tendons showed progressive stiffening over time, especially at myotendinous junction and at the site of the sutured lesion, resulting in significantly higher stiffness than both the contralateral tendon and healthy volunteers. Peak thickness of treated tendons occurred at 6 months, with a tendency to reduce at 1 year, while never achieving a normal physiological state. Greatest remodelling was seen at the lesion site. The contralateral tendon showed significant thickening at the myotendinous and osteotendinous junctions. The SI of the contralateral tendon was found to be stiffer than physiological values found in the control group. ATRS score improved significantly between 6 months and 1 year, being negatively correlated with the SI (p < 0.001).
Conclusion
RTSE showed that operatively treated Achilles tendons become progressively stiffer during follow-up, while the ATRS score improved. From a biomechanical point of view, at 1 year after surgery Achilles tendons did not show a “restitutio ad integrum”. Real-time sonoelastography provides more qualitative and quantitative details in the diagnostics and follow-up of Achilles tendon conditions as the post-operative evolution of the repairing tissue.
Level of evidence
Diagnostic and therapeutic study, Level III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Complete subcutaneous rupture of the Achilles tendon is estimated to account for approximately 35 % of all tendon tears. It most commonly occurs in an active population, particularly in those with specific risk factors such as diabetes, prolonged fluoroquinolone therapy or anti-tumoural drug therapy [13].
During the last decades, the pathophysiology of human tendon, and in particular its healing process, has been extensively studied. However, the biomechanical changes in tendon recovery have only partially been investigated in pre-clinical studies [26], or in clinical studies of the entire flexor functional unit rather than the tendon itself. It is well known that after a complete tendon rupture, the healing process normally requires approximately 1 year to restore a normal histological structure [5–7, 15]. In 2002, Palmes demonstrated in an experimental animal model the importance of early post-operative mobilization to achieve accelerated healing [26]. In their study, the histological structure of these specimen tendons was more mature and rich in elastic fibres than controls. It has not been clarified whether it is possible to fully restore biomechanical features and how long this may take.
B-mode ultrasonography (US) is a cost-effective diagnostic instrument used in tendon pathology: it converts a radiofrequency signal into a bidimensional black and white image showing morphological characteristics, but with poor qualitative and no direct quantitative assessment of the pathoanatomical and biomechanical condition of a tissue.
Recently, real-time sonoelastography (RTSE), or “elastosonography”, has become of interest as an ultrasound-based technique to assess structural and biomechanical features of biological tissues, such as “elasticity” [31]. Ophir et al. [24] first described the elastographic principles of strain imaging, and more recently, Pesavento [27] described the basis for its clinical applications. The reading of RTSE is based on the effects of an external compression force on the tissue under investigation, which produces displacement in its structure. The magnitude of such displacement is less in harder tissues than in softer tissues. Tissue displacement is calculated in real time by a modified ultrasound scanner, such that different grades of elasticity may be displayed over a common ultrasound image. An easy colour scale overlaps the conventional US images, giving an immediate portrait of the tissue. Furthermore, the software analyses shear waves and returns a mean value for tissue strain. For this reason, RTSE is considered as “virtual” palpation [10, 16].
To our knowledge, this new ultrasound-based method has been used to detect quantitative and qualitative information in the normal and pathologic Achilles tendon, but no systematic evolution of the repairing tissue after surgery has been reported yet to assess whether the “restitutio ad integrum” is myth or truth.
The aim of this paper is to report the RTSE pattern of surgically repaired Achilles tendons, to provide new information regarding the biomechanics of tendon healing and to describe a feasible technical method that may be applicable in day-by-day clinical practice.
Materials and methods
This study was designed as a prospective study. As the technique is new and no gold standard exists for the purpose of evaluating in vivo tissue strain, no comparison with other images was performed. From January 2011 to January 2013, patients referred to our university hospital for spontaneous subcutaneous rupture of the Achilles tendon were enrolled. Patients aged over 65 years, or with a history of diabetes, familial hypercholesterolemia, fluoroquinolones therapy, glucocorticoid therapies within the last 12 months (either orally or locally administered), collagenopathies, seropositive or seronegative enthesopathies or anti-tumour drug administration were excluded. A control group of healthy volunteers were evaluated for comparison of the ultrasonographic and sonoelastographic findings. All enrolled patients underwent a percutaneous tenorrhaphy using a polyethylene terephthalate (PET) thread with two long, straight needles. Surgical interventions were performed as day surgery, under local anaesthesia with lidocaine hydrochloride 10 % at the entry and exit points of the device. The surgical technique is described in Gigante et al. [14].
Clinical follow-up
Post-operatively, patients were discharged a few hours after surgery with two crutches and an anterior splint, non-weight bearing indication on the operated side and subcutaneous low molecular weight heparin as DVT prophylaxis. At the first follow-up visit on day 20, the splint was removed and a loose elastic bandage was applied with the ankle in a neutral position. Protected weight bearing with crutches and active flexion–extension exercises of the ankle were then commenced.
At day 40, after US and sonoelastographic assessment, the PET device was removed, and progressive weight bearing and ankle rehabilitation were allowed.
At day 55, another clinical follow-up was performed. Full weight bearing was then permitted, and the rehabilitation program progressed [14].
At 6 months and at 1 year post-operatively, patients attended a follow-up visit to assess functional recovery through RTSE and administration of the Achilles Tendon Total Rupture Questionnaire (ATRS) [23]. This is a disease-specific, ten-item questionnaire (built on a Likert Scale from 0 to 10 points per question) and is currently considered the most reliable questionnaire to assess the functional recovery of the Achilles tendon after surgical treatment compared with previous scores such as the AOFAS or VISA-A [3, 18]. The highest score, 100 points, indicates a complete return to all activities, including sports. For each question, a score of 0 corresponds to maximum limitation and complaint, while a 10 signifies well-being and complete recovery. For our study, the questionnaire was translated into Italian by the first author and revised by a professional medical writer.
Real-time sonoelastography methods and endpoints
Sonoelastographic evaluation was performed 40 days post-operatively and repeated at 6 months and 1 year. Tendons were first evaluated using conventional US with a 5–12 MHz probe, followed by RTSE examination (Philips iU 22, Eindhoven, the Netherlands).
Patients were positioned in prone position with both the ankles over the extremity of the bed. A senior radiologist, expert in musculoskeletal disorders and blinded to clinical outcome and questionnaire scores, examined a longitudinal view of both Achilles tendons (the operated and non-operated sides). Image acquisition was performed, following the technical notes published by Palle [25].
Thirty healthy volunteers (25 males and 5 females) aged between 20 and 40 (mean 31.3) were recruited to identify an ultrasonographic and elastographic normal range. The same exclusion criteria were applied to this control group as to the study group. This healthy control group included smokers and non-smokers, non-diabetics and subjects reported occasional physical activity, but none participated in competitive sports.
Both volunteers’ tendons (60 tendons in total) were scanned using the same methodology. Informed consent was obtained from all patients. This study conforms to the Declaration of Helsinki and subsequent modifications. IRB of Department of Clinical and Molecular Sciences (DISCLIMO)—Università Politecnica delle Marche gave the approval (ref. no. 2011/01).
All assessments were carried out with tendons in a relaxed state. No acquisitions were made with contraction of the triceps surae, to avoid mechanical effects on the tendon related to muscle.
Prior to performing sonoelastographic analysis, conventional US was performed with the same machine, only using the B-mode function. Thickness of tendon was evaluated at the myotendinous junction (MTJ), the body of the tendon (ruptured site), and at the osteotendinous junction (OTJ).
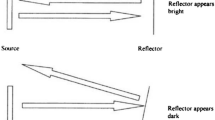
For the sonoelastographic assessment, first the examiner performed an auto-calibration of the pressure applied on the probe, using a pressure sensor that showed the pressure level on screen as a green bar. For reproducibility, tendon examination was performed at 50 % of the peak pressure (Fig. 1). The probe was placed perpendicular to the tendon in order to reduce any bias related to anisotropy. The examiner tapped the tendon in the same place four times with a small, regular pressure: this external pressure generates a change in the structural shape of tendon that the probe detects as elastographic information. Depending on tissue deformability, one of four colours appears on the screen superimposed on the B-mode image: blue for high stiffness, green for intermediate stiffness, yellow for low stiffness and red for very elastic tissue. This coloured picture is the so-called elastogram. The colour-coded images were analysed on a personal computer using QLAB software (Philips Medical Systems), which allowed selection of a 30-frame cine loop. To calculate the SI, two regions of interest (ROIs) or “windows” with the same area (4 × 1 mm) were identified on the screen (Fig. 2): the first localized on the tendon area being investigated and the second in Kager’s fat. Adipose tissue has been reported to show consistent sonoelastographic behaviour [12]. Each acquisition was performed continuously for 30 s. These technical methods allow the examiner to reach the best accuracy and reproducibility according to the current literature [12, 21, 25, 29].
Elastogram superimposed on the B-mode image. The colour scale indicates progressive stiffness from red (soft) to blue (hard). The upper colour bar is used as reference to compare the examined tissue. The lower red square marks the pressure bar that is used by the operator to calibrate the pressure applied to the tendon. The method is standardized such that the operator applies pressure at 50 % of the measurable peak
Two regions of interest (ROIs) of 4 × 1 mm are identified on the elastogram: the first belongs to the tendon (red area) to be investigated and the second is in the fat tissue of Kager’s triangle (green area). Fat tissue shows a poor response to pressure; thus on the elastogram, it does not modify its colour. We consider it a reference tissue to calculate the SI and the strain/time curve (shown here below the elastogram)
The SI is calculated as the mathematical ratio of the tendon and adipose strains within the selected window. Once the ROIs are placed, the RTSE software creates a curve showing the mean elasticity variations within the ROIs in the 30 s of continuous examination. Same size windows were identified in MTJ and OTJ of both tendons and in the tendon body on the contralateral side at a distance of 3–4 cm from the calcaneal insertion. All scans were recorded and the data saved to hard disk for statistical analyses. Images were obtained in the phase of compression as this provided the best contrast. Three cycles of compression/decompression were performed. Images were saved after every cycle.
Tendon thickness and SI in the three zones of the Achilles tendon were evaluated at each of the three follow-up appointments. Furthermore, a correlation between ATRS and SI at the lesion site was calculated, to determine how the measured biomechanical features related to patient recovery.
Statistical analysis
Group sample sizes of 25 patients and 30 healthy volunteers achieved 80 % power to detect a mean difference of at least 0.5 mm in tendon thickness between the two groups, with estimated group standard deviations of 0.8 mm, a significance level of 0.05, two-tailed test. Besides, a sample size of 25 patients achieved 82 % power to detect a difference of at least 0.6 mm in tendon thickness in the three time-points, considering a standard deviation of 1 and a significance level of 0.05, two-tailed test.
A nonparametric approach was used to compare the treated group with the healthy group, and treated tendons with contralateral untreated tendons, since variables were not found normally distributed. Qualitative variables were summarized by absolute and percentage frequencies, and comparisons between patients and healthy volunteers were made using Fisher’s exact test. Quantitative variables were summarized using the median and first and third quartiles as variability measures. Comparison between patients and healthy volunteers was made using Wilcoxon’s test (independent samples); variations in tendon thickness between day 40 and 1 year post-operatively, and between 6 months and 1 year, were calculated with Wilcoxon’s test for paired data. Correlation between the SI at the lesion site and ATRS at 1 year of follow-up was estimated through Spearman’s linear correlation with a 95 % confidence interval.
Results
Study population
During the period of investigation, to reach the sample size, 29 consecutive patients were diagnosed with subcutaneous rupture of Achilles tendon and underwent percutaneous repair. Four patients were excluded; two patients were excluded due to diabetes, one patient for anti-tumour treatment and one patient due to age. None of the enrolled patients were lost to follow-up. Of the enrolled 25 patients, 22 were male and three were female, with a mean age of 42.1 ± 9.0 years. In 80 % (20 tendons), the rupture was on the left side, while in 20 % (five tendons), it was on the right side. Patients were significantly older than healthy volunteers (p < 0.001); no significant differences were found in gender, smoke habits and physical activity distributions.
Ultrasonographic findings
Tendon thickness, on a sagittal view in healthy volunteers and evaluated using conventional B-mode US, was 3.9 ± 0.4 mm at the osteotendinous junction (OTJ), 4.6 ± 0.5 mm in the body and 2.1 ± 0.4 mm at the MTJ, respectively.
Considering the treated tendons, for each of the three examined areas and particularly at the lesion site, thickness was significantly increased at 6 months post-operatively and reduced after 1 year. Despite this reduction, after 1 year, the thickness remained greater than that observed in the control group. The contralateral, untreated tendons, during all evaluations, also demonstrated a significant increase in thickness in all examined areas, by 0.5 mm (Table 1).
Real-time sonoelastography findings
The sonoelastographic method revealed a significant modification in SI values for all areas of the surgically treated and untreated tendons compared with the control group. Values were lower than those found in normal samples. In particular, a significant decrease was observed when comparing the values at 40 days and at 1 year (Table 1). In addition, a significant decrease was found when comparing the results between 6 months and 1 year for the treated side (Table 1). Note that similar values for SI were found at 40 days and 6 months, while the tendon thickness was significantly different. When compared to the control group, both the treated and untreated sides showed increased thickness and SI differences. Treated tendons appeared to be thicker than normal at 1 year, but also the untreated side had a significant increase in thickness at the OTJ and MTJ (Table 2). The SI for treated tendons was lower (i.e. the tendons were stiffer) than healthy tendons at 1 year, and interestingly, the contralateral tendons also became stiffer over time, as shown by a reduced SI (Table 3).
Clinical outcomes
At 6 months post-operatively, the median ATRS score was 91 (78–97), and at 1 year, the score was 95 (80–100). During the follow-up period, a significant improvement (p < 0.001) was observed.
An inverse correlation was found between the ATRS score and SI value at the lesion site (Spearman’s coefficient −0.42, 95 % confidence interval −0.70 to −0.30, p = 0.03). The wide confidence interval demonstrates low accuracy in the estimation, due to the small number of cases.
Discussion
The most important findings of the present study were the identification of an elastographic pattern of the Achilles tendon after surgery and the relationship between these data and clinical outcomes.
Despite the abundant literature on the Achilles tendon, few data are available regarding the biomechanical recovery of the tendon after surgical repair. Mc Nair and co-workers [22] compared the effects of a weight bearing and non-weight bearing protocol on energy stored, stiffness and shock absorption in the plantar flexor muscle–tendon unit of patients managed non-operatively following an Achilles tendon rupture. They found that weight bearing generally gave superior results; however, these results were still well below the normal values seen in unaffected legs at 6 months follow-up.
Type III collagen is observed during scar formation, prior to the neo-synthesis of type I collagen [11], leading to a change in Achilles tendon biomechanics. This abnormal collagen composition is recognized as a cause of intrinsic tissue weakness [20].
RTSE is mainly used for the diagnostics of soft tissues neoplasms; however, it has recently been proposed as a novel and non-invasive instrument for the evaluation of tissue elasticity in response to external pressure. This field of application is new, and few papers have been published reporting such methods in relation to tendons [8, 9, 12, 28]. The diagnostic estimation of tissue hardness or elasticity has been used since the earliest origins of medicine. The simplest example is palpation, as reported first by Hippocrates [17]. Today, palpation of the Achilles tendon is a valid and reliable instrument for diagnosis and follow-up, although it is subjective, not quantifiable and related to the extemporaneity of the examination. RTSE has been described as “virtual palpation” [16], which adds qualitative and quantitative details to the conventional clinical examination.
In this context, the present study aimed to investigate the potential role of RTSE in the follow-up of repaired Achilles tendons and verify the described steps in the physiology of tendon healing. The Achilles tendon is superficial and has little soft tissue coverage, making it the ideal candidate for these first investigations.
De Zordo [9] observed a 94–96 % occurrence of stiffness (blue-green colour) in the proximal section and a 95–100 % rate in the distal section of the Achilles tendon, although these data were not compared to other images. Drakonaki [12] in 2009 reported data from healthy Achilles tendons with SI evaluation. Data are similar to our normal control findings; however, a different machine was used and data are not suitable for direct comparison. Tan [29] evaluated 19 Achilles tendons in amateur soccer players after surgical repair versus 40 tendons from 20 healthy players at an average follow-up of 38.6 months. The treated tendons appeared to be less elastic than normal controls on a graduated colour scale from red (very soft tissue) to blue (very hard tissue). Furthermore, the proximal section was found to be more rigid than the central and distal parts, which did not differ in terms of sonoelastographic properties.
Aubry et al. investigated 18 healthy Achilles tendons in three different examination positions, using shear wave imaging of the mid-portion of the tendon [1, 2]. They observed that maintaining the probe parallel to the collagen fibres was important, as if the transducer is not correctly placed, significant modifications to the results may occur.
The conventional US data from our investigation are consistent with those reported by Gigante et al. [14] in 2008, in which the treated tendons were observed to gradually approach native tendon diameter. They also reported a peak in thickness at 6 months post-operatively. Moreover, while it is understandable that the treated tendon has a thicker diameter due to scar maturation and remodelling, we also observed thickening of the contralateral tendon, likely due to an overload during the rehabilitation period. Among the several values we provided, thickening of the untreated osteotendinous junction is significant, while the myotendinous junction and tendon body were comparable to normal findings.
The main focus was on the SI and not the colour pattern classification, since this depends on the machine used. Here, it is reported that a non-homogeneous chromatic pattern was found in each of the three groups, confirming that the colour is not a marker of pathology, but only of structural variability.
The modifications of sonoelastographic findings during our study, and its trend to decrease after an initial phase (the hypertrophic scar formation phase), surely complement the “heterogenous echogenicity pattern” found in simple B-mode US; however, we are not yet able to give a clear association with pathoanatomical findings. Healing Achilles tendon tends to become stiffer at 6 months and stiffer at 1 year of follow-up, confirming that it is still undergoing maturation. It is noteworthy that the contralateral, untreated tendons also undergo a parallel modification into a stiffer tissue. This was statistically significant in the osteotendinous and myotendinous junction, but not in the tendon body. It remains unclear what is behind this contralateral stiffening, but it might be consequence of overload during the rehabilitation period, although it may also be an indication of a predisposition to tendinopathy.
Clinically, ATRS confirmed again that percutaneous Achilles repair provides excellent outcomes. Surprisingly, these outcomes demonstrate a slight inverse correlation with sonoelastographic findings. We hypothesize a compensation phenomenon across the tibiotalar joint involving the flexor tendons of the foot.
It should be noted from the present study that the Achilles tendon, in contrast with past histopathological and isokinetic findings [5, 14], cannot be considered biomechanically healed at 1 year after surgery.
Recently, Tudisco et al. [30] reported his findings for the supraspinatus tendon, assessing RTSE as a feasible method for clinical practice in the diagnosis of small insertional rotator cuff tears. The quantitative outcomes were correlated with the several shoulder scores. Similarly to what has been found with this study, the author found an inverse correlation between stiffness and clinical outcome. They used bone as a reference tissue as opposed to fat in our study. For this reason, the results of the two studies cannot be directly compared.
Chen et al. in 2013 [4] characterized 36 normal Achilles tendons and 14 torn tendons with shear wave elastography. They found a significant elasticity pattern, which was obviously expected, but quantified at 291.91 ± 4.38 kPa for normal tendons compared with an elasticity value of 56.48 ± 68.59 kPa for torn tendons. Like our study, this study was preliminary and involved a small sample size, but provides interesting new data about the tendon behaviour.
Contemporarily, Klauser et al. [19] provided a comparison between US and RTSE with an histological agreement: they found that the elastography was able to depict the 100 % of tendon high grade degeneration histologically demonstrated, while conventional US depicted only in 86 % of cases.
Although it is not yet known whether RTSE can really identify tendon conditions earlier than MRI or B-mode US, this method might be greatly useful for the orthopaedic surgeon for intraoperative monitoring and for follow-up of the repaired tendon.
RTSE does have some limitations, such as the lack of an MRI double-check and potential intrinsic operator error, although this may be lower than US if a reproducible method and auto-calibration are used [21]. The diagnostic value of the SI is better than an absolute value of tissue strain. The technique can be standardized, so that operator dependency is reduced and it might be useful for assessing whether a tendon is healing normally or whether there is a delay in the healing process.
The present study was of prospective design, with the radiologist blinded to clinical examination results, which had strict inclusion and exclusion criteria and included a correlation between clinical and radiological findings. Here, we report a very reliable method considering the operator’s calibration, in the ROI window sizing and image acquisition method, as well as the post-processing phases. The study would require a longer follow-up period and a larger sample size to determine “if and when” the Achilles tendon has complete “restitutio ad integrum”. As in other studies on this subject, the lack of a direct comparison between RTSE and histological specimens from the examined tendons is a limitation. Despite that, RTSE application in Achilles tendon has clinical implications in detecting the evolution of the repairing scar tissue after surgery as in the correlation with the outcomes, providing a novel diagnostic and prognostic device in the hands of the clinician.
Conclusion
RTSE is interesting novel method in the follow-up of surgically repaired Achilles tendons, showing that 1 year after surgery the scar tissue is stiffer than the contralateral, untreated side and healthy control tendons. Validity and reliability of RTSE need to be further investigated, and it should be compared with existing methods for biomechanical evaluation.
References
Aubry S, Risson JR, Barbier-Brion B, Tatu L, Vidal C, Kastler B (2011) Transient elastography of calcaneal tendon: preliminary results and future prospects. J Radiol 92(5):421–427
Aubry S, Risson JR, Kastler A, Barbier-Brion B, Siliman G, Runge M, Kastler B (2013) Biomechanical properties of the calcaneal tendon in vivo assessed by transient shear wave elastography. Skelet Radiol 42(8):1143–1150
Carmont MR, Silbernagel KG, Nilsson-Helander K, Mei-Dan O, Karlsson J, Maffulli N (2013) Cross cultural adaptation of the Achilles tendon total rupture score with reliability, validity and responsiveness evaluation. Knee Surg Sports Traumatol Arthrosc 21(6):1356–1360
Chen XM, Cui LG, He P, Shen WW, Qian YJ, Wang JR (2013) Shear wave elastographic characterization of normal and torn achilles tendons: a pilot study. J Ultrasound Med 32(3):449–455
de Palma L, Gigante A, Rapali S (1998) I processi riparativi delle lesioni tendinee. In: “Progressi in Medicina e Chirurgia del piede” -Il piede nello sport-, vol 7. Aulo Gaggi Editor, Bologna, pp 13–23
de Palma L, Marinelli M, Meme L, Pavan M (2004) Immunohistochemistry of the enthesis organ of the human Achilles tendon. Foot Ankle Int 25(6):414–418
de Palma L, Santucci A, Sabetta SP (1994) Anatomia della regione calcaneare, vol 3. Progressi in Medicina e Chirurgia del piede - Fratture del Calcagno
De Zordo T, Chhem R, Smekal V, Feuchtner G, Reindl M, Fink C, Faschingbauer R, Jaschke W, Klauser AS (2010) Real-time sonoelastography: findings in patients with symptomatic achilles tendons and comparison to healthy volunteers. U Ultraschall Med 31(4):394–400
De Zordo T, Fink C, Feuchtner GM, Smekal V, Reindl M, Klauser AS (2009) Real-time sonoelastography findings in healthy Achilles tendons. AJR Am J Roentgenol 193(2):W134–W138
Dewall RJ (2013) Ultrasound elastography: principles, techniques, and clinical applications. Crit Rev Biomed Eng 41(1):1–19
Doral MN, Alam M, Bozkurt M, Turhan E, Atay OA, Donmez G, Maffulli N (2010) Functional anatomy of the Achilles tendon. Knee Surg Sports Traumatol Arthrosc 18(5):638–643
Drakonaki EE, Allen GM, Wilson DJ (2009) Real-time ultrasound elastography of the normal Achilles tendon: reproducibility and pattern description. Clin Radiol 64(12):1196–1202
Filippucci E, Farina A, Bartolucci F, Spallacci C, Busilacchi P, Grassi W (2003) Levofloxacin-induced bilateral rupture of the Achilles tendon: clinical and sonographic findings. Reumatismo 55(4):267–269
Gigante A, Moschini A, Verdenelli A, Del Torto M, Ulisse S, de Palma L (2008) Open versus percutaneous repair in the treatment of acute Achilles tendon rupture: a randomized prospective study. Knee Surg Sports Traumatol Arthrosc 16(2):204–209
Gigante A, Specchia N, Rapali S, Ventura A, de Palma L (1996) Fibrillogenesis in tendon healing: an experimental study. Boll Soc Ital Biol Sper 72(7–8):203–210
Hamamoto K (2006) Investigation on virtual palpation system using ultrasonic elasticity imaging. Conf Proc IEEE Eng Med Biol Soc 1:4873–4876
Hippocrates: (400 B.C.) The books of prognostics. In: eBooks@Adelaide, The University of Adelaide Library, University of Adelaide, South Australia
Kearney RS, Achten J, Lamb SE, Parsons N, Costa ML (2012) The Achilles tendon total rupture score: a study of responsiveness, internal consistency and convergent validity on patients with acute Achilles tendon ruptures. Health Qual Life Outcomes 29:10–24
Klauser AS, Miyamoto H, Tamegger M, Faschingbauer R, Moriggl B, Klima G, Feuchtner GM, Kastlunger M, Jaschke WR (2013) Achilles tendon assessed with sonoelastography: histologic agreement. Radiology 267(3):837–842
Leadbetter WB (1992) Cell-matrix response in tendon injury. Clin Sports Med 11(3):533–578
Magarelli N, Carducci C, Bucalo C, Filograna L, Rapisarda S, De Waure C, Dell’Atti C, Maccauro G, Leone A, Bonomo L (2014) Sonoelastography for qualitative and quantitative evaluation of superficial soft tissue lesions: a feasibility study. Eur Radiol 24(3):566–573
McNair P, Nordez A, Olds M, Young SW, Cornu C (2013) Biomechanical properties of the plantar flexor muscle-tendon complex 6 months post-rupture of the Achilles tendon. J Orthop Res 31(9):1469–1474
Nilsson-Helander K, Thomee R, Silbernagel KG, Thomee P, Faxen E, Eriksson BI, Karlsson J (2007) The Achilles tendon Total rupture score (ATRS): development and validation. Am J Sports Med 35(3):421–426
Ophir J, Alam SK, Garra B, Kallel F, Konofagou E, Krouskop T, Varghese T (1999) Elastography: ultrasonic estimation and imaging of the elastic properties of tissues. Proc Inst Mech Eng H 213(3):203–233
Palle L, Reddy MB, Reddy KJ, Kumari MV (2011) Technical note: real-time sonoelastography evaluation of Achilles tendon. Indian J Radiol Imaging 21(4):267–269
Palmes D, Spiegel HU, Schneider TO, Langer M, Stratmann U, Budny T, Probst A (2002) Achilles tendon healing: long-term biomechanical effects of postoperative mobilization and immobilization in a new mouse model. J Orthop Res 20(5):939–946
Pesavento A, Perrey C, Krueger M, Ermert H (1999) A time-efficient and accurate strain estimation concept for ultrasonic elastography using iterative phase zero estimation. IEEE Trans Ultrason Ferroelectr Freq Control 46(5):1057–1067
Sconfienza LM, Silvestri E, Cimmino MA (2010) Sonoelastography in the evaluation of painful Achilles tendon in amateur athletes. Clin Exp Rheumatol 28(3):373–378
Tan S, Kudas S, Ozcan AS, Ipek A, Karaoglanoglu M, Arslan H, Bozkurt M (2012) Real-time sonoelastography of the Achilles tendon: pattern description in healthy subjects and patients with surgically repaired complete ruptures. Skeletal Radiol 41(9):1067–1072
Tudisco C, Bisicchia S, Stefanini M, Antonicoli M, Masala S, Simonetti G (2013) Tendon quality in small unilateral supraspinatus tendon tears. Real-time sonoelastography correlates with clinical findings. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-013-2551-7
Varghese T, Ophir J, Konofagou E, Kallel F, Righetti R (2001) Tradeoffs in elastographic imaging. Ultrason Imaging 23(4):216–248
Conflict of interest
The authors declare that no competing interests exist.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Busilacchi, A., Olivieri, M., Ulisse, S. et al. Real-time sonoelastography as novel follow-up method in Achilles tendon surgery. Knee Surg Sports Traumatol Arthrosc 24, 2124–2132 (2016). https://doi.org/10.1007/s00167-014-3484-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3484-5