Abstract
Purpose
Severe uncontained tibial bone defects occurring during total knee arthroplasty are challenging, and which treatment method is the best remains unknown. In this study, clinical and radiographic outcomes of double metal blocks augmentation were examined.
Methods
Between 2004 and 2012, double metal blocks augmentation was carried out in 17 patients with severe asymmetric uncontained tibial bone defects. The first block was attached to the tibial tray with screws, and then the second block was cemented to the first block. Out of 17 patients, 13 (8 primary, 5 revision) were available for final follow-up at a median of 69 months (range 24–99). For clinical assessment, range of motion and Knee Society score were evaluated preoperatively and annually thereafter. At the final follow-up, Western Ontario and McMaster Universities Osteoarthritis Index, Oxford knee, Short Form-36, Lower extremity functional scale, and Lower extremity activity scale scores were evaluated. Radiographic assessment for radiolucent lines at the block–cement–bone interfaces and signs of failure was performed annually using fluoroscopy and standard radiographs.
Results
Range of motion and Knee Society score were significantly improved post-operatively. Other clinical outcomes were favourable. Radiolucent lines were seen on fluoroscopy in three knees, but no sign of failure, such as loosening, collapse, or instability, was observed at the final follow-up.
Conclusions
Double metal blocks augmentation is a favourable and useful method, which does not cause mechanical failure or protrusion of the prosthetic because of its modularity, to manage severe asymmetric uncontained proximal tibial bone defects >15 mm in total knee arthroplasty.
Level of evidence
Case series, Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Proper management of severe bone defects is a challenge in total knee arthroplasty (TKA) [3, 10]. Most severe bone defects in primary TKA occur from severe preoperative angular deformity and commonly present as tibial bone defects [38]. Bone loss following TKA failure can occur by several factors, including implant and cement removal [45], mechanical loosening [15], wear debris-induced osteolysis [23], chronic infection [28], or delayed reimplantation of prosthesis [45]. Severe bony deficiencies can significantly influence factors such as stability, alignment, and soft tissue balancing; therefore, adequate restoration of bone stock is critical [25, 34, 37]. Reconstitution of severe bone defects, including single tibial plateau >25–40 % of the tibial support surface or >5–10 mm deep, is accepted to provide prosthetic support [13, 18, 40, 47]. Several options for the management of severe bone defects have been reported, including structural allograft, modular metal augmentation with a wedge or block, metaphyseal tantalum cones or sleeves, custom implants, or condyle-replacing hinged prosthesis [14, 39, 45]. Although several methods are available for treating bone defects, massive asymmetric uncontained tibial bone defects >15 mm remain difficult for surgeons. Each method has advantages and disadvantages as well as proper indications considering such defect characteristics as size, location, and type. For example, structural allograft carries risks of infection, non-union, and graft resorption. Modular metal augmentation has high availability and familiarity, but has limitations to its size and shape. Cones or sleeves are applicable to massive bone defects, but have limited indications to only cavitary defects [41].
Double rectangular metal blocks augmentation, which was previously introduced in a technical note [4], is a unique method that has the advantages of modular metal augmentation, while also overcoming the limitations of size and shape, for managing severe uncontained bone defects >15 mm. This technique can prevent protrusion of the prosthetic support, which can cause irritation to soft tissue and pain, by applying a smaller-size metal block. However, the results of this technique have not been reported, and there has been no evidence demonstrating its mechanical stability. The aim of this study was to evaluate whether double metal tibial blocks augmentation improves clinical results and provides favourable radiographic results in patients with severe asymmetric uncontained proximal tibial bone defects >15 mm after undergoing primary or revision TKA. The hypothesis was that double metal tibial blocks augmentation produces a stable and durable reconstruction and should be considered as an effective method.
Materials and methods
This retrospective study was approved by the Institutional Review Board of our hospital. The authors did not receive any financial aid from manufacturers mentioned in this study. Between 2004 and 2012, severe asymmetric uncontained tibial bone defects were managed by double metal blocks augmentation in 17 patients (17 cases) who underwent primary or revision TKA at a median age of 65 years (range 48–80 years). All operating procedures were carried out by one surgeon (CHC). Out of the 17 patients, 3 died <1 year after surgery for reasons not related to the operation, and one patient could not be followed up due to non-ambulatory status following myocardial infarction. Therefore, the remaining 13 patients (8 primary TKAs, 5 revision TKAs) were available for final follow-up at a median of 69 months (range 24–99 months). Demographic data of the patients and characteristics associated with the metal blocks are shown in Table 1.
Surgical technique
The knee joint was exposed using a medial parapatellar approach. Proper axial alignment of the tibia was confirmed by an extramedullary tibial alignment guide. Initial proximal tibial osteotomy was carried out at a depth of 10 mm from the unaffected tibial condyle. In the case of revision TKA, the proper level of proximal tibial osteotomy was set with consideration of the relationship between the patella and fibular head in order to restore the initial joint line [33]. Subsequently, the tibial bone defect was evaluated, and an appropriately sized tibial tray was selected. Matching bone resection was performed after assembling a block-cutting guide. If the tibial bone deficiency was >15 mm and the type of bony defect was uncontained, which has no bony support base after tibial bone resection, two rectangular metal blocks, 10- and 5-mm thick or 10- and 10-mm thick, were used to compensate for the bony defect. The first metal block was affixed to the tibial tray using screws, and then the second metal block was attached to the first block with polymethyl methacrylate (PMMA) cement (Fig. 1). If the metal block protruded over the natural cortical rim of the proximal tibia, downsized metal block augmentation was performed to maintain the natural tibial cortical shape (Fig. 1). The long intramedullary stem assembled to the tibial component was fixed in all cases using a diaphyseal dangling stem and cementation in the tibial tray and metaphysis. The size of the stem was determined by considering the length, depth, and width of the tibia, and whether the stem was fitted to or contacted the medullary canal. The implant used in this study was Scorpio TS prosthesis (Stryker Orthopedics, Mahwah, NJ, USA).
Real photograph showing double metal blocks assembled to tibial tray with intramedullary stem (a). The first metal block being affixed to the tibial tray using screws, and second down sized metal block being assembled to first metal block with polymethyl methacrylate (PMMA) cements (b). The downsized metal block of width being used to maintain the cortical shape, in case of second metal block protruding over the tibial cortical rim (b)
Outcome evaluations
For clinical assessment, range of motion (ROM) of the knee joint and Knee Society score (KSS; knee score, function score) [26] were evaluated preoperatively and annually thereafter. In addition, Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score [7], Oxford Knee Score (OKS) [20, 35], Short Form-36 (SF-36) score [46], Lower extremity functional scale (LEFS) score [8], and Lower extremity activity scale (LEAS) score [43] were recorded at the final follow-up. Preoperative values of ROM and KSS were compared with the final values.
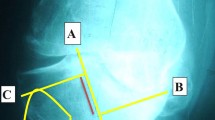
For radiographic assessment, standard anteroposterior (AP), posteroanterior (PA), and long-leg standing radiographs were obtained preoperatively at 3, 6, and 12 months post-operatively, and annually thereafter. Initial femorotibial anatomic alignment was compared with final anatomic alignment. Radiographic images involving component position, presence of radiolucent lines (RLLs) >1 mm in width, and osteolysis at the block–cement–bone interfaces were examined by one author (KSC) unrelated to the surgeons and procedures in this study using the Knee Society Roentgenographic evaluation system [21] with consultation to a single experienced musculoskeletal radiologist. Furthermore, supine AP and lateral fluoroscopic images, focused on the femoral and tibial components separately, were obtained annually to ensure clear views of the block–cement–bone interfaces. All radiographic measurements were documented three times with an interval of 2 weeks using a picture archiving and communication systems (Infinitti; Marotech, Seoul, Korea); the averages of the measurements were used for analysis.
Statistical analysis
The Wilcoxon signed rank test was used to compare the difference in values between preoperative and final follow-up results of ROM of the knee joint, femorotibial anatomic alignment, and KSS. The level of significance was set at p < 0.05. Statistical analysis was performed using SPSS 18.0 for Windows (SPSS Inc., Chicago, IL, USA). The sample size required to detect differences was calculated from the absolute difference knee score of KSS between preoperative and final results. Alpha was set at 0.05, and power was set at 0.80. If the null hypothesis was set at 45, a minimum sample size of eight cases was required based on the difference between initial and final values of 64.0 ± 16.6. The present study involved 13 cases, so the overall power of the study was 0.953.
Results
Median ROM improved significantly from 110° ± 26° preoperatively to 125° ± 15° at the final follow-up (p = 0.019). All final clinical outcomes were favourable; in particular, final KSS improved significantly (p = 0.001; Table 2). To clarify midterm outcomes with a minimum 5-year follow-up (median, 92 months; range 60–99 months), ROM and KSS of cases improved significantly, while final results of other clinical scores were also satisfactory (Table 3).
Final anatomic alignment showed significant improvement compared with initial values (p = 0.005; Table 4). There was no failure, breakage, or sign of deterioration between the first and second metal blocks on radiography. On fluoroscopic images, RLLs at the block–cement–bone interfaces were observed on AP view in three knees (23 %) during the first post-operative year (zone 1, 2 cases; zones 1 and 2, 1 case). One patient (2.5 mm, zone 1) progressed at 5 years post-operatively, but no further progression existed at the final 92-month follow-up (Fig. 2). One case with RLLs on AP view demonstrated RLLs (2.0 mm, zone 1) on lateral view at 5 years post-operatively; however, progression was limited to 4 mm at the final 98-month follow-up. All RLLs did not cause any failure, component loosening, or instability.
Preoperative standing anteroposterior (AP) images (a) and intraoperative photographs after arthrotomy (b) showing severe uncontained proximal tibial bone defects, approximately 23 mm compared with unaffected lateral tibial condyle. AP view of fluoroscopy with medial double metal blocks (10 mm block + down sized 10 mm block) combined intramedullary stem at 60-month follow-up after primary total knee arthroplasty, demonstrating radiolucent line (white arrow) of 2.5 mm width bottom the block (c). AP view at 92-month follow-up indicating non-progressive stable radiolucent lines (white arrow) at same area without any radiographic failure signs and broken sign between first and second metal block (d)
Discussion
The most important finding of the present study was that double metal tibial blocks augmentation presented favourable clinical outcomes without any case of mechanical failure. Radiographically, there was no aseptic loosening or failure between the block–cement–bone interfaces. Only three cases showed RLLs, two of which showed progression. However, scoring by measuring the width of the RLLs [21] was not greater than a score of 4, which is probably not significant and stable. All RLLs did not cause evidence of mechanical failures. Therefore, the results of this study fully support the hypothesis that this technique produces a stable and durable reconstruction and should be considered as an effective method. The satisfactory clinical and radiographic results after a minimum 5-year follow-up demonstrate the favourable midterm durability and mechanical stability of this construct.
Management methods for severe bone defects >15 mm are limited. Structural allograft is suitable for younger patients who require further revision TKA in order to restore bone stock. Advantages of allograft include potential for biologic ingrowth and versatility [14, 16, 45]. However, allograft has concerns regarding disease transmission, as well as less osteoinductive power with regard to non-union, malunion, and late collapse [11, 22, 38]. The survival rate of allograft is not favourable: only 77.2 % at 5 years [6] and 72 % at 10 years [12]. Only surgeons with extensive experience demonstrate the best results [19]. Impaction bone graft which can be converted into contained defects by use of wire mesh may be used for uncontained defects. However, follow-up duration in previous studies has been limited to the short term. Impaction bone graft has the same disadvantages as bulk allograft [31, 32, 36].
Metaphyseal tantalum cones and sleeves are an alternative treatment for massive bone defects to restore metaphyseal stability [27, 45]. Tantalum surfaces present osteoblast expression for growth of native bone into the metal [9, 24]. Advantages of cones and sleeves include simplifying the surgical technique, shortening the operating time [40]. In the average 36-month follow-up results of 29 cases with trabecular cones, improved clinical outcomes and no RLLs were reported [42]. Another recent study reported similarly favourable results and no evidence of loosening [17, 29, 44]. In the 36 case of sleeves, no significant osteolysis or loosening was found at average follow-up of 38 months [5]. Other studies on sleeves have described similarly favourable results [1, 2]. However, weaknesses of the above studies include a short-term results and inclusion of only revision TKA cases. Potential concerns of them include removal difficulty, long-term durability, high cost, iatrogenic fracture during vigorous sleeve impaction, and epiphyseal stress shielding [24]. Most importantly, the primary indication of cones and sleeves is contained cavitary metaphyseal defects, meaning they are not suitable for severe asymmetric uncontained bone defects [14]. Additionally, the size of commercially available cones and sleeves is not suitable for Asian patients who commonly have much smaller tibial diameter compared with Caucasians.
Custom implants can provide the best fit for large bone defects. However, since accurate preoperative evaluation of bone loss is difficult, custom implants may not fit well. Other disadvantages include considerable time to produce, expansive costs, and a lack of reported results [47]. Condyle-replacing hinged prosthesis should be used for massive bone defects with loss of collateral ligamentous support, especially in low-demand, elderly patients. However, a potential disadvantage of hinged prosthesis is that there are few remaining reconstructive options if this method should fail [14].
Prosthetic augments are used for defects of 5–10 mm [47], or when 40 % or more of the projected implant–bone interface is unsupported by host bone [13]. Metal augments provide good load transmission to underlying bone as well as immediate support and stability [11]. They can be applied easily and quickly, allow for intraoperative custom fabrication, and require minimal bone resection [41]. Unlike allograft, there are no concerns about disease transmission, non-union, malunion, or augment collapse [14]. Lee and Choi [30] described the average 78.6-month follow-up results of 46 cases with tibial metal blocks and reported improved clinical outcomes and no radiographic failure. Considering these advantages, prosthetic metal augments were considered as suitable for severe asymmetric uncontained bone defects. Prosthetic augments are limited in size and shape, however. The Scorpio TS prosthesis used in this study has only two rectangular block size options, 5 or 10 mm. To compensate for bone defects >15 mm, a larger-size metal block was designed by attaching each block with cement. Because no screw system to attach each block has been developed, there was no choice but to use PMMA cement. The long intramedullary stem assembled to the tibial component was used not only to decrease the osseous strength of the defect base, but also to conserve the peripheral bone from stress [41].
This double blocks augmentation technique has several characteristics. First, this method is unique, simple, has no learning curve, and reduces operating time. Second, there are no concerns regarding disease transmission, bone healing, or graft resorption. Third, this technique is useful in cases of primary or revision TKA. Fourth, indications include defects with an intact cortical shell and uncontained asymmetric defects. Fifth, the double blocks augmentation technique can easily overcome the unsuitable size problem associated with cones and sleeves.
There are several limitations in this study. First, this was a retrospective study, and there was no comparative group. Second, sample size of 13 cases is small (as in most case series), and four out of 17 patients were lost to follow-up. However, the causes of loss were inevitable events in older patients. Third, the follow-up duration was not uniform, and the minimum follow-up of 24 months is short; however, the minimum 5-year follow-up cases showed a 100 % survival rate up to 99 months after surgery. In the future, a larger number of patients and longer-term follow-up results will be required to evaluate the fate of this technique.
The clinical relevance of this study is that double metal blocks augmentation is a useful method for managing severe asymmetric uncontained proximal tibial bone defects >15 mm. Second, this technique does not cause mechanical failure such as loosening, instability, or subsidence. Third, protrusion of the prosthetic support, which can cause irritation to soft tissue and pain, can be prevented by applying a smaller-size metal block, if necessary, in patients with a smaller tibia.
Conclusion
The author’s preferred technique of double metal blocks augmentation—attaching double blocks to the tibial tray with the use of cement and screws—is a favourable and useful method to manage severe asymmetric uncontained proximal tibial bone defects >15–20 mm based on clinical and radiographic results at a median of 69 months after primary or revision TKA.
References
Agarwal S, Azam A, Morgan-Jones R (2013) Metal metaphyseal sleeves in revision total knee replacement. Bone Joint J 95:1640–1644
Alexander GE, Bernasek TL, Crank RL, Haidukewych GJ (2013) Cementless metaphyseal sleeves used for large tibial defects in revision total knee arthroplasty. J Arthroplasty 28:604–607
Altchek D, Sculco TP, Rawlins B (1989) Autogenous bone grafting for severe angular deformity in total knee arthroplasty. J Arthroplasty 4:151–155
Baek SW, Choi CH (2011) Management of severe tibial bony defects with double metal blocks in knee arthroplasty—a technical note involving 9 cases. Acta Orthop 82:116–118
Barnett SL, Mayer RR, Gondusky JS, Choi L, Patel JJ, Gorab RS (2014) Use of stepped porous titanium metaphyseal sleeves for tibial defects in revision total knee arthroplasty: short term results. J Arthroplasty 29:1219–1224
Bauman RD, Lewallen DG, Hanssen AD (2009) Limitations of structural allograft in revision total knee arthroplasty. Clin Orthop Relat Res 467:818–824
Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW (1988) Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 15:1833–1840
Binkley JM, Stratford PW, Lott SA, Riddle DL (1999) The Lower Extremity Functional Scale (LEFS): scale development, measurement properties, and clinical application. North American Orthopaedic Rehabilitation Research Network. Phys Ther 79:371–383
Bobyn JD, Poggie RA, Krygier JJ, Lewallen DG, Hanssen AD, Lewis RJ, Unger AS, O’Keefe TJ, Christie MJ, Nasser S, Wood JE, Stulberg SD, Tanzer M (2004) Clinical validation of a structural porous tantalum biomaterial for adult reconstruction. J Bone Joint Surg Am 86(Suppl 2):123–129
Brand MG, Daley RJ, Ewald FC, Scott RD (1989) Tibial tray augmentation with modular metal wedges for tibial bone stock deficiency. Clin Orthop Relat Res 248:71–79
Brooks PJ, Walker PS, Scott RD (1984) Tibial component fixation in deficient tibial bone stock. Clin Orthop Relat Res 184:302–308
Clatworthy MG, Ballance J, Brick GW, Chandler HP, Gross AE (2001) The use of structural allograft for uncontained defects in revision total knee arthroplasty. A minimum five-year review. J Bone Joint Surg Am 83:404–411
Cuckler JM (2004) Bone loss in total knee arthroplasty: graft augment and options. J Arthroplasty 19:56–58
Daines BK, Dennis DA (2012) Management of bone defects in revision total knee arthroplasty. J Bone Joint Surg Am 94:1131–1139
Dalury DF, Pomeroy DL, Gorab RS, Adams MJ (2013) Why are total knee arthroplasties being revised? J Arthroplasty 28:120–121
Dennis DA (2002) The structural allograft composite in revision total knee arthroplasty. J Arthroplasty 17:90–93
Derome P, Sternheim A, Backstein D, Malo M (2014) Treatment of large bone defects with trabecular metal cones in revision total knee arthroplasty: short term clinical and radiographic outcomes. J Arthroplasty 29:122–126
Dorr LD, Ranawat CS, Sculco TA, McKaskill B, Orisek BS (1986) Bone graft for tibial defects in total knee arthroplasty. Clin Orthop Relat Res 205:153–165
Engh GA, Ammeen DJ (2007) Use of structural allograft in revision total knee arthroplasty in knees with severe tibial bone loss. J Bone Joint Surg Am 89:2640–2647
Eun IS, Kim OG, Kim CK, Lee HS, Lee JS (2013) Validation of the Korean version of the Oxford Knee Score in patients undergoing total knee arthroplasty. Clin Orthop Relat Res 471:600–605
Ewald FC (1989) The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res 248:9–12
Fehring TK, Peindl RD, Humble RS, Harrow ME, Frick SL (1996) Modular tibial augmentations in total knee arthroplasty. Clin Orthop Relat Res 327:207–217
Goldvasser D, Marchie A, Bragdon LK, Bragdon CR, Weidenhielm L, Malchau H (2013) Incidence of osteolysis in total knee arthroplasty: comparison between radiographic and retrieval analysis. J Arthroplasty 28:201–206
Haidukewych GJ, Hanssen A, Jones RD (2011) Metaphyseal fixation in revision total knee arthroplasty: indications and techniques. J Am Acad Orthop Surg 19:311–318
Hoeffel DP, Rubash HE (2000) Revision total knee arthroplasty: current rationale and techniques for femoral component revision. Clin Orthop Relat Res 380:116–132
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Jones RE (2004) Modular revision stems in total hip arthroplasty. Clin Orthop Relat Res 420:142–147
Kasahara Y, Majima T, Kimura S, Nishiike O, Uchida J (2013) What are the causes of revision total knee arthroplasty in Japan? Clin Orthop Relat Res 471:1533–1538
Lachiewicz PF, Bolognesi MP, Henderson RA, Soileau ES, Vail TP (2012) Can tantalum cones provide fixation in complex revision knee arthroplasty? Clin Orthop Relat Res 470:199–204
Lee JK, Choi CH (2011) Management of tibial bone defects with metal augmentation in primary total knee replacement: a minimum five-year review. J Bone Joint Surg Br 93:1493–1496
Lonner JH, Lotke PA, Kim J, Nelson C (2002) Impaction grafting and wire mesh for uncontained defects in revision knee arthroplasty. Clin Orthop Relat Res 404:145–151
Lotke PA, Carolan GF, Puri N (2006) Impaction grafting for bone defects in revision total knee arthroplasty. Clin Orthop Relat Res 446:99–103
Mason M, Belisle A, Bonutti P, Kolisek FR, Malkani A, Masini M (2006) An accurate and reproducible method for locating the joint line during a revision total knee arthroplasty. J Arthroplasty 21:1147–1153
Mihalko WM, Krackow KA (2006) Flexion and extension gap balancing in revision total knee arthroplasty. Clin Orthop Relat Res 446:121–126
Murray DW, Fitzpatrick R, Rogers K, Pandit H, Beard DJ, Carr AJ, Dawson J (2007) The use of the Oxford hip and knee scores. J Bone Joint Surg Br 89:1010–1014
Naim S, Toms AD (2013) Impaction bone grafting for tibial defects in knee replacement surgery. Results at two years. Acta Orthop Belg 79:205–210
Nam D, Cross MB, Plaskos C, Sherman S, Mayman DJ, Pearle AD (2012) The effect of medial condylar bone loss of the knee on coronal plane stability—a cadaveric study. Knee 19:640–643
Pagnano MW, Trousdale RT, Rand JA (1995) Tibial wedge augmentation for bone deficiency in total knee arthroplasty. A followup study. Clin Orthop Relat Res 321:151–155
Panegrossi G, Ceretti M, Papalia M, Casella F, Favetti F, Falez F (2014) Bone loss management in total knee revision surgery. Int Orthop 38:419–427
Panni AS, Vasso M, Cerciello S (2013) Modular augmentation in revision total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 21:2837–2843
Radnay CS, Scuderi GR (2006) Management of bone loss: augments, cones, offset stems. Clin Orthop Relat Res 446:83–92
Rao BM, Kamal TT, Vafaye J, Moss M (2013) Tantalum cones for major osteolysis in revision knee replacement. Bone Joint J 95:1069–1074
Saleh KJ, Mulhall KJ, Bershadsky B, Ghomrawi HM, White LE, Buyea CM, Krackow KA (2005) Development and validation of a lower-extremity activity scale. Use for patients treated with revision total knee arthroplasty. J Bone Joint Surg Am 87:1985–1994
Schmitz HC, Klauser W, Citak M, Al-Khateeb H, Gehrke T, Kendoff D (2013) Three-year follow up utilizing tantal cones in revision total knee arthroplasty. J Arthroplasty 28:1556–1560
Vasso M, Beaufils P, Cerciello S, Schiavone Panni A (2014) Bone loss following knee arthroplasty: potential treatment options. Arch Orthop Trauma Surg 134:543–553
Ware JE Jr, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30:473–483
Whittaker JP, Dharmarajan R, Toms AD (2008) The management of bone loss in revision total knee replacement. J Bone Joint Surg Br 90:981–987
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chung, K.S., Lee, J.K., Lee, H.J. et al. Double metal tibial blocks augmentation in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 24, 214–220 (2016). https://doi.org/10.1007/s00167-014-3368-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3368-8