Abstract
Invasive candidiasis is the most common critical care-associated fungal infection with a crude mortality of ~ 40–55%. Important factors contributing to risk of invasive candidiasis in ICU include use of broad-spectrum antimicrobials, immunosuppressive drugs, and total parenteral nutrition alongside iatrogenic interventions which breach natural barriers to infection [vascular catheters, renal replacement therapy, extracorporeal membrane oxygenation (ECMO), surgery]. This review discusses three key challenges in this field. The first is the shift in Candida epidemiology across the globe to more resistant non-albicans species, in particular, the emergence of multi-resistant Candida glabrata and Candida auris, which pose significant treatment and infection control challenges in critical care. The second challenge lies in the timely and appropriate initiation and discontinuation of antifungal therapy. Early antifungal strategies (prophylaxis, empirical and pre-emptive) using tools such as the Candida colonisation index, clinical prediction rules and fungal non-culture-based tests have been developed: we review the evidence on implementation of these tools in critical care to aid clinical decision-making around the prescribing and cessation of antifungal therapy. The third challenge is selection of the most appropriate antifungal to use in critical care patients. While guidelines exist to aid choice, this heterogenous and complex patient group require a more tailored approach, particularly in cases of acute kidney injury, liver impairment and for patients supported by extracorporeal membrane oxygenation. We highlight key research priorities to overcome these challenges in the future.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Epidemiological shifts towards multi-resistant Candida requires enhanced surveillance and rigorous infection control to detect and prevent resistance emergence. The evidence around deployment of risk-scores and fungal non-culture-based tests in decision-making around starting and stopping antifungals in the ICU is lacking: adequately powered multi-site studies using a combination of tests linked to clinical and cost effectiveness outcomes are needed. Antifungal prescribing in special ICU populations, particularly acute kidney injury, liver impairment and ECMO requires a tailored approach and further PK evaluation. |
Introduction
‘Invasive candidiasis’ (IC) is an umbrella term for three clinical conditions: candidaemia; deep-seated candidiasis; and deep-seated candidiasis with associated candidaemia [1]. Cases are often hospital acquired, and critically ill patients are particularly vulnerable [2], with approximately one-third of all candidaemia occurring in this setting [3]. Despite expanded access to fungicidal agents, IC-related outcomes remain poor, with a crude mortality of ~ 40–55% in intensive care unit (ICU)-focused studies over the past decade [4,5,6,7].
The incidence of deep-seated candidiasis without concomitant candidaemia in ICU is less certain due to challenges in obtaining specimens for microbiological confirmation. Intra-abdominal candidiasis (IAC) accounts for most deep-seated cases, with ~ 30% occurring in critical care [8]. Perforation, anastomotic leaks, repeat laparotomies, necrotizing pancreatitis and abdominal organ transplants increase risk; therefore, incidence is higher in surgical ICUs [8]. Other forms of deep-seated candidiasis include haematogenously disseminated disease (hepatosplenic, ocular, cardiac, central nervous system, bone and renal), seen more frequently with prolonged candidaemia, and in immunosuppressed and neutropenic patients [9, 10]. Host genetics also influence IC susceptibility, with various single-nucleotide polymorphisms (SNPs) identified as increasing candidaemia risk [11].
Figure 1 illustrates key factors contributing to development of IC in ICU. IC risk factors have fluctuated with advances in intensive care medicine; while there is increased use of renal replacement therapy, extracorporeal membrane oxygenation (ECMO), and immunosuppression treatments, there has been improved vascular catheter management, more judicious use of total parenteral nutrition (TPN) and greater emphasis on antimicrobial stewardship [12,13,14]. The collective impact of this on IC incidence is unclear. Large multi-centre studies examining IC incidence in ICU have been conducted over the past decade [4,5,6,7, 15,16,17,18]. Rates of candidaemia reported vary significantly between 3.5 and 16.5 per 1000 admissions [4, 6, 7, 16,17,18]. However, due to inter-centre variability, the fact most studies focused on candidaemia only, and some encompassed cases likely to represent colonization rather than IC, evaluation of IC incidence trends in ICU over time is challenging.
Key factors in the development of invasive candidiasis in critical care. Key factors include: (1) Candida colonization; patients develop invasive candidiasis from their own colonizing Candida flora. Broad-spectrum antibiotic use selects for Candida in the gut and skin microbiome and patients can acquire new species through environmental or patient-to-patient transmission. (2) Breach in barrier defenses; Breaches due to disease (e.g. gut perforation) or critical care interventions (e.g. skin; line insertion), act as a portal for Candida entry into a sterile site (sterile-site cavity or bloodstream). (3) Predisposing host risk factors; these include genetics, drugs, and co-morbidities which influence the likelihood of developing localized candidiasis (e.g. abdominal candidiasis), candidaemia, and the chance of progression to disseminated disease. BMT bone marrow transplant, GI gastrointestinal, Haem haematological, IV intravenous, SNPs single-nucleotide polymorphisms, TPN total parenteral nutrition
In this narrative review, we sought to summarize key epidemiological, diagnostic and treatment challenges of managing IC in ICU and highlight future directions in this field. To ensure a broad coverage of relevant literature, we undertook a MEDLINE search for English language articles published before 1 July 2020, using the terms “candidiasis”, “candidaemia”, “critical care”, “resistance”, “biomarkers” and “antifungal”, including further relevant studies from reference lists of articles identified.
Challenge 1: changing epidemiology and emergence of antifungal resistance
Epidemiological shifts
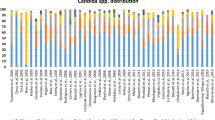
There is significant geographic and demographic variation in IC [19]. C. albicans remains the dominant species in Europe [5,6,7]; in a pan-European ICU cohort study (2015–16) [6], C. albicans represented 57% of cases, followed by C. glabrata and C. parapsilosis. Across India, C. tropicalis was the most common cause of ICU-acquired candidaemia [20], whereas C. albicans and C. parapsilosis predominate in Latin America [21]. The USA sees a higher proportion of non-albicans cases (approximately, two-thirds), with increasing C. glabrata incidence [22]. Echinocandin-resistant C. glabrata is reported; while European prevalence appears low (< 1%) [23], US studies report a prevalence of 6–12% [24,25,26], with azole cross-resistance in up to one-third of isolates [27]. This is concerning given echinocandins are recommended first-line treatment in IC, and azoles the most widely used antifungals globally. Moreover, the emergent multi-drug-resistant C. auris has caused outbreaks on ICUs worldwide [28]. It is the third most common cause of candidaemia in South Africa, with 88% of cases associated with ICU stays [29]. C. auris is usually fluconazole resistant, with variable amphotericin and echinocandin susceptibility, and pan-fungal resistance to all three classes reported [30].
Reservoirs of resistance in ICU: the patient and environment
The patient and the environment can be reservoirs of fungal resistance in ICU. Antibiotic use disrupts the skin and gut microbiome, increasing Candida colonization and risk of IC [31]. Antifungal exposure selects for less susceptible Candida species such as C. parapsilosis, C. krusei and C. glabrate [32] and fosters resistance; in a US study, echinocandin-resistant C. glabrata was associated with prior echinocandin exposure, fluconazole resistance, and prolonged hospitalization [26]. In Denmark, post-treatment (≥ 7 days) mouth swabs in candidaemic patients demonstrated acquired resistance to fluconazole and echinocandins in 29% and 22% of C. glabrata isolates, respectively [33]. Specifically, reduced echinocandin penetration into the gut may select for the emergence of echinocandin-resistant species [33, 34].
Resistant isolates spread between patients, and within the ICU environment, with reports of genotype-linked clusters of azole-resistant C. parapsilosis [35], and inter-hospital spread of azole-resistant C. glabrate [36] in ICU. C. auris studies have described widespread contamination of environmental surfaces and equipment persisting for months, with patient acquisition of C. auris occurring after as little as 4 h of contact [37]. The limited efficacy of commonly used environmental disinfectants and absence of effective skin decolonization regimens for C. auris have made transmission difficult to interrupt [38]. A UK ICU C. auris outbreak was only stemmed when reusable temperature probes were removed from circulation [39]. For C. auris, infection control measures including screening, isolation, cohorting and environmental disinfection are advised in Public Health guidance [40, 41]. ICU interventions for tackling fungal resistance are summarized in Fig. 2.
Reservoirs of resistance in critical care: interventions to prevent, detect, and interrupt transmission of resistant Candida. (1) The ICU patient as a reservoir of resistance; antibiotic use alters the human microbiome and allows Candida to flourish in the gut and on the skin. Exposure to antifungal drugs can then select for less drug-susceptible and resistant species, transforming the host fungal ecology. Patients may also acquire resistant Candida species prior to admission, particularly those who have been exposed to other healthcare settings, with the potential of introducing new fungal pathogens to the ICU. Interventions to prevent, detect and interrupt transmission of resistant Candida in the ICU patient: antimicrobial and antifungal stewardship; screening for resistant Candida (e.g. C. auris) on admission and isolation of colonized patients; identification of yeasts in sterile and non-sterile specimens in ICU to monitor changes in fungal ecology. (2) The ICU environment as a reservoir of resistance; resistant Candida can be shed from patients’ skin and gastrointestinal tract, contaminating the surrounding ICU environment and healthcare workers, facilitating transmission to other patients. Interventions to prevent, detect and interrupt transmission of resistant Candida in the ICU environment: cleaning of equipment and the environment and introduction of single-use equipment during an outbreak; environmental screening; contact precautions for colonized patients; good hand hygiene
Many hospital laboratories do not identify yeasts in non-sterile specimens to species level; as a result, changes in ecology and resistance may go undetected. Misidentification of C. auris for other species, particularly C. haemulonii, when using common diagnostic platforms is recognized [42]. Matrix-assisted laser desorption/ionization time-of-flight (MALDI-TOF) allows quick, accurate identification, but is not universally available. Improving laboratory capacity for Candida speciation, particularly C. auris, and fungal susceptibility testing is important for surveillance and early detection of resistance emergence in ICU.
Challenge 2: when to start and when to stop antifungal therapy?
Timely delivery of effective AFT in proven IC is crucial, as delays are associated with increased mortality [43]. Conversely, over-prescription may be detrimental, exposing patients to drug toxicities and driving resistance emergence. A cross-sectional study of French and Belgian ICUs demonstrated that while 7.5% of patients were prescribed systemic AFT, two-thirds subsequently had no evidence of IFI [44], emphasising the challenge of achieving a balance between targeted, timely AFT whilst avoiding excessive and unnecessary use.
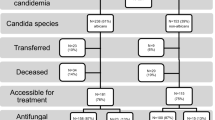
Earlier antifungal strategies have thus been developed (prophylactic, empiric, pre-emptive), (Table 1), although the optimal strategy in ICU remains controversial. To aid decision-making about stopping and starting antifungals, three key tools, for use alone or in combination, have been proposed: Candida colonization assessment, clinical prediction rules, and fungal non-culture-based tests (NCBT) (Table 2). Table 3 summarizes key studies using these tools to initiate or discontinue AFT; however, their impact on clinical practice remains hotly debated.
Role of candida colonization and clinical prediction rules
Candida colonization is considered a pre-requisite for the development of IC (Fig. 1) [62]; those with a higher Candida Colonization Index (CCI) are at greater risk [45]. However, although the proportion of ICU patients colonized with Candida increases over time (~ 50–80%), only 5–30% may develop IC [63]. While studies have proposed colonization can be used to guide prophylaxis and reduce IC [64,65,66], they have not shown a mortality benefit. A study found colonization-triggered caspofungin or azole use changed the ICU fungal ecology (increased C. glabrata), without reducing IC-associated mortality or incidence [67]. Hence, the moderate positive predictive value (PPV) of this approach (~ 66% for CCI [45]) could lead to excessive antifungal use that is neither appropriate nor cost-effective.
To improve the PPV, clinical prediction rules, incorporating host factors with or without Candida colonization, have been established. The UK FIRE Study reviewed ~ 60,000 ICU admissions and evaluated risk models for predicting IC. However, IC incidence was lower than expected (0.6%), and analysis suggested a strategy of no risk assessment or AFT prophylaxis was the most cost-effective [68].
RCTs have evaluated the impact of clinical prediction rules triggering early AFT on IC incidence and mortality in ICU. The MSG-01 trial [57] (n = 219) randomized to caspofungin prophylaxis or placebo based on the Ostrosky-Zeichner clinical prediction rule, demonstrating a non-significant reduction in IC (9.8% vs 16.7%, p = 0.14) and no difference in all-cause mortality (16.7% vs 14.3%, p = 0.78).
The similarly sized INTENSE trial [58] (n = 241) randomized ICU patients with intra-abdominal infection requiring emergency surgery to ‘pre-emptive’ micafungin or placebo. Given prescribing was not based on NCBTs or radiology, current definitions would consider this an antifungal prophylaxis trial. There was no reduction in IC incidence (micafungin 11.1% vs placebo 8.9%). AFT was possibly initiated too late (max. 120 h post-surgery) given many developed IC early in their admission. No details around source control were presented (e.g. drainage of collections/second laparotomies), which may play a more significant role than early AFT in patients with a surgical abdominal focus.
Both trials suggest early AFT based on risk factors alone does not reduce IC incidence or impact mortality. However, they also illustrate the challenges of powering studies adequately: in the MSG-01 trial, IC incidence in the control group was lower than expected, and the INTENSE trial highlighted the importance of selecting the right at-risk group and time point for intervention.
Empirical antifungal therapy in ICU
Given signs and symptoms of IC are non-specific, overlapping with many other infectious and non-infectious aetiologies, empirical AFT to cover the possibility of fungal infection in the septic ICU patient is common practice. A major factor driving empirical therapy are limitations of conventional culture-based methods. Although the gold standard for diagnosing IC, blood culture (BC) sensitivity is suboptimal (~ 75% in bloodstream infection, ~ 5–20% in abdominal candidiasis) [1, 69], sterile site sampling (e.g. abdominal pus) often difficult, and time to culture positivity prolonged (2–3 days) [1].
No survival benefit of early AFT in non-neutropenic ICU patients was demonstrated in a 2016 meta-analysis (> 2300 patients from 22 RCTs) [70], although criteria triggering antifungal prescribing in the analyzed studies were very heterogenous. Subsequently, the EMPIRICUS trial [59] (n = 261) randomized ventilated patients with evidence of ICU-acquired sepsis, Candida colonization, and multi-organ failure to empirical micafungin or placebo. No improvement in 28-day fungal-free survival was demonstrated (68% vs 60.2%, p = 0.18), despite significant reduction in proven IC in the micafungin arm (3% vs 12%, p = 0.008). Subgroup analysis suggested a trend towards better survival in those with SOFA score > 8 (HR, 1.69 [95% CI 0.96–2.94], p = 0.07); Demonstrating survival benefit in ICU patient groups, often with multiple co-morbidities and high baseline mortality, requires much larger trials to achieve adequate power. Identifying the subset of ICU patients who could benefit from early AFT remains a key challenge.
Guidelines do not address de-escalation or discontinuation of empirical therapy for suspected infection in the absence of microbiological confirmation. In a post hoc analysis (n = 647) of the observational ARMCAND2 study including patients with suspected (57%) or proven IC (43%), de-escalation (defined as either switch to azole or antifungal discontinuation by day 5) only occurred in 22% (n = 142; 96 switched; 48 stopped), of which half had no microbiological evidence of IC [71]. De-escalation was associated with shorter total AFT duration, with no negative impact on mortality or length of ICU stay despite similar illness severity scores between those who did and did not de-escalate. A smaller observational study had similar findings [72]. Nevertheless, the low proportion switched or stopped highlights barriers to de-escalation in practice. This includes reluctance to modify empirical treatment in unstable patients with uncertain diagnoses, alongside a desire to use a fungicidal, well-tolerated agent to cover the possibility of azole-resistant Candida. Yet, for patients on empirical therapy where the clinical picture suggests low IC risk and BC are negative, discontinuing AFT appears a reasonable option and could be beneficial in preventing resistance emergence. For those where likelihood of IC is deemed moderate to high, non-culture-based diagnostics may have a role in informing decisions.
Role of non-culture-based tests
Non-culture-based tests (NCBTs) have been developed in an attempt to overcome the shortfalls of culture-based fungal diagnostics, given their quick turnaround time, the potential for earlier IC detection and given they may remain positive for longer while on AFT [1]. They include 1,3-β-d-glucan (BDG), T2 magnetic resonance Candida assay (T2Candida), multiplex candida real-time PCR, and the detection of mannan antigen (MAg) and anti-mannan IgG antibodies (Anti-Mn) (Table 2). Potential roles for NCBTs include aiding clinical decision-making to guide; 1) the initiation of pre-emptive AFT; 2) the discontinuation or withholding of empirical AFT; 3) monitoring clinical improvement in patients with IC.
NCBTs have been described as “Bayesian” [69]; i.e. they do not deliver a definitive result, but assess the likelihood of infection. IC prevalence varies between ICUs due to differences in case mix and interventions. With variation in the pre-test likelihood, the negative predictive value (NPV) and PPV of NCBTs changes; in higher-risk patients and settings (e.g. surgical ICU), the PPV will rise and the NPV will decrease, and vice-versa [69]. Hence, as recently outlined in Mycoses Study Group recommendations, NCBTs must be requested and interpreted in the context of the pre-test likelihood of IC [73]; they suggest that the clinical value of NCBTs is limited when this figure is less than 10%.
Non-culture-based tests to trigger antifungal initiation
The ideal NCBT for guiding early antifungal initiation needs a high sensitivity to identify IC, but reasonable specificity to avoid over-prescribing. The most widely used NCBT, BDG, has moderate specificity (~ 60–85% [48,49,50]), marred by false positivity which may occur due to haemodialysis, blood product administration, high-burden Candida colonization, and disturbed GI-mucosa, all common in ICU. This may result in antifungal overuse. Establishing diagnostic cutoff values which optimize test performance in ICU is crucial. BDG specificity improves with consecutive sampling and increasing the ‘positive’ cutoff value to ≥ 250 pg/ml (instead of 80 pg/ml [74]), which in one study increased specificity to 87% but reduced sensitivity to 52% [75]. NCBT combinations may also improve specificity; a positive BDG (≥ 80 pg/ml) alongside a negative PCT (< 2 ng/ml) had a 96% PPV for candidaemia, when distinguishing IC from bacteraemia in one study [76]. Additionally, a highly positive BDG (> 259 pg/ml) alongside a positive CAGTA better distinguished IC from Candida colonization in patients with severe gastrointestinal conditions, compared to either used alone [75]. A prospective Danish study (n = 126) in ICU patients at high risk of IC (particularly IAC) found a combination of T2Candida and BC compared to MAg and BC, or BC alone had a the greatest specificity (64%/53%/29% respectively) and a sensitivity of > 95%, for diagnosing proven/likely IC [77]. Additionally, a retrospective study assessing NCBTs performance for IAC (n = 48) found the sensitivity/specificity for T2Candida was 33%/93% and BDG 83%/67%; however, concordant positive results diagnosed IAC in 100% of cases, and concordant negative results excluded IAC in 90% of cases, suggesting combinations would be more useful clinically [78].
To date, few prospective studies have examined the impact of NCBT-driven pre-emptive AFT on outcomes [79]. A small pilot RCT (n = 64) administered pre-emptive anidulafungin to ICU patients with a BDG ≥ 60 pg/ml [56] during twice-weekly surveillance; while it demonstrated feasibility, enrolment difficulties meant it was not powered to assess a difference in IC or survival. In a sub-group analysis of the EMPIRICUS study, fungal-free survival was not significantly different in those with an elevated BDG who received micafungin versus placebo (BDG > 80 [HR 1.41, 95% CI 0.85–2.33], BDG > 200 [HR 1.51, 95% CI 0.47–5.00]), but the trend was in the direction of the micafungin arm [59].
Current evidence is not robust enough to support the use of NCBTs alone to trigger AFT. The moderate specificity of BDG hinders its use, but combination with other NCBTs, optimizing ‘cutoff’ values, and directing testing to ‘high risk’ patients using Candida risk scores, make it a more valuable tool. NCBT-driven pre-emptive therapy using NCBT combinations which maximize test performance (T2Candida plus BDG) alongside culture is the most promising early AFT strategy, which needs to be examined robustly in randomized multi-centre clinical trials. Outcomes should include IC, mortality, AFT consumption and cost-effectiveness, so benefits and risks of such a strategy can be holistically assessed. We eagerly await the results of the CandiSep trial (NCT02734550) comparing clinical outcomes of a BDG-driven versus culture-driven approach to AFT prescribing in septic ICU patients.
Non-culture-based tests to aid antifungal discontinuation
NCBTs with a high NPV may be better used to guide discontinuation or preventing initiation of AFT. A trial (n = 109) randomized patients with evidence of infection who fulfilled IC-risk criteria to 14-days’ empirical AFT or an NCBT-driven strategy, whereby AFT was stopped if BDG, MAg, Anti-Mn, and BC were negative [61]. Unsurprisingly, given comparison was to a 14-day standard, AFT duration was shorter in the NCBT arm, but importantly there was no deleterious impact on mortality or development of IC. A further study (n = 85) prescribed empirical AFT to patients with risk factors and signs of infection [60]; based on negative BC and serial negative BDGs, AFT was safely discontinued in 21/85 by day 4 and none developed candidaemia upon follow-up. Other retrospective studies demonstrated similar findings [80, 81]. An ICU study assessing the utility of BDG for therapeutic decision-making found that although introduced to target ‘high-risk’ patients of IC, in practice only 26% of patients in whom it was used were in this category [82]. Results influenced AFT prescribing in over half of the cases, deemed appropriate in three-quarters and inappropriate in a quarter of cases (AFT continued/started with no subsequent evidence of IFI). Thus paradoxically, in real-world deployment of ICU BDG testing, any reductions in antifungal consumption gained through earlier stopping of inappropriate therapy based on the test’s good NPV may be outweighed by an excess in prescribing due to the test’s poor PPV when used in an unselected population. Studies so far have been too small to assess the safety and clinical effectiveness of NCBT-driven AFT discontinuation algorithms. Multi-site studies comprising a range of low-to-high IC prevalence settings are needed for results to be generalizable.
In summary, whilst NCBT results interpreted in context remain a useful adjunct in stewardship, to date there is insufficient evidence to support antifungal discontinuation based on negative NCBT [48, 83]. The A-STOP trial (ISRCTN43895480), a large multi-site (35 hospital) UK diagnostic accuracy study prospectively assessing which NCBT (or combination thereof) can best rule out IC and facilitate AFT discontinuation in ICU patients, holds promise of delivering on this.
Non-culture-based tests for monitoring
Clinical response markers for monitoring and prognostication in IC are lacking. BC clearance of fungi is often used as a proxy for treatment effectiveness; however, this is less than ideal given their suboptimal sensitivity, particularly in deep-seated candidiasis.
Studies in ICU [77] and mixed ward/ICUs [84], found T2Candida remained detectable for longer than BC in candidaemia; in the latter study, 7.5% (4/31) had a positive surveillance BC, yet 41.9% (13/31) had a positive surveillance T2Candida. Hence, time-to-negative result with T2Candida was significantly longer, perhaps unsurprising given T2Candida also detects non-viable Candida cells. To assess its clinical relevance, larger studies correlating persistent T2Candida positivity with clinical outcomes are needed. While studies have examined BDG kinetics for monitoring treatment response in IC [85,86,87], few have done so in an ICU-specific population [88, 89]. In heterogenous patient groups, serial BDG decline has been associated with successful therapy, with a slower decrease in patients with deep-seated candidiasis [85, 86], and persistently negative BDGs in candidaemic patients are associated with a lower 30-day mortality [90, 91]. However, in ICU patients with intra-abdominal candidiasis [88] and candidaemia [89], BDG was slow to clear from circulation and remained positive beyond clinical resolution of infection. Hence, while the trajectory of decline, or persistent negativity may have some monitoring use, there is little evidence to support that transition from a positive to negative BDG is valuable in assessing treatment response and currently no evidence that it can be used to guide AFT duration.
Challenge 3: choosing the optimal antifungal drug for the ICU patient
The antifungal armamentarium is limited, with just four classes of drugs available for treatment of IC; azoles (fluconazole, voriconazole); echinocandins (caspofungin, anidulafungin, micafungin); polyenes (amphotericin B); and the pyrimidine analogue, flucytosine. Drug development is progressing, with several new agents undergoing trials (e.g. Ibrexafungerp, fosmanogepix, rezafungin) [92].
Several guidelines aid the appropriate selection of an antifungal [93, 94]. Echinocandins are recommended first-line treatment of proven [93, 94] and suspected [93] IC in non-neutropenic critically ill adults, due to their broader-spectrum compared to fluconazole, fungicidal activity, excellent tolerability and minimal drug interactions. In the only comparative RCT, anidulafungin was found to be non-inferior to fluconazole for the treatment of IC (global response 73.2% versus 61.1%, 95% CI − 1.1 to 25.3) [95]. A post hoc subgroup analysis in ICU patients demonstrated significantly better response rates for those receiving an echinocandin (70.8% versus 54.1%, p = 0.03), although this did not translate to a reduction in 28-day mortality (20.2% versus 24.3% p = 0.57) [96]. Other observational studies comparing mortality between those initiated on fluconazole or echinocandins, showed either no difference [97,98,99], or favoured echinocandins [100, 101]. However, adjusting for the multiple confounders influencing outcome in ICU in non-randomized studies is difficult. A recent large RCT failed to demonstrate non-inferiority of the newest triazole, isavuconazole, when compared to caspofungin for IC (end-of-IV-therapy treatment response, 60.3% versus 70.1%, 95% CI − 19.9 to − 1.8), consistent regardless of illness severity [102]. There is no evidence to suggest a difference in efficacy or mortality with amphotericin B compared to azoles and echinocandins [103]. Given the higher cost and association with greater toxicity, amphotericin B in IC treatment is usually reserved for situations with no suitable alternatives, e.g. MDR Candida, for drug penetration.
In candidaemia, de-escalation from echinocandins to fluconazole for azole-susceptible isolates, when repeat BCs are negative and the patient is clinically stable is recommended within 5–7 days in IDSA [93], and at 10 days in ESCMID guidelines [94]. A number of studies (albeit not RCTs) have demonstrated the safety of this approach at day 5 in proven IC [71, 100, 104] with no impact on clinical outcomes. The ESGCIP taskforce recently recommended considering de-escalation at day 5, dependent upon clinical response [105].
Antifungal drugs in special ICU populations
Alongside guidelines, patient-specific factors need to be considered when choosing the most appropriate drug, dose and duration for different clinical scenarios [106], summarized in Table 4.
Acute kidney injury (AKI) is common in ICU, sometimes requiring continuous renal replacement therapy (CRRT) which can significantly affect antifungal PK/PD. The kidneys excrete 60–80% of fluconazole unchanged [107]; dose reduction in AKI is thus required due to delayed elimination. Conversely, high elimination is seen with CRRT due to low protein binding and high water solubility; therefore, increased fluconazole doses are advised [107]. For voriconazole, no renal or CRRT dose adjustment is required, but frequent TDM is needed. Given the voriconazole IV solvent vehicle can accumulate in moderate-to-severe renal impairment, oral over IV therapy is recommended [107]. Amphotericin B, particularly the deoxycholate formulation, can be associated with nephrotoxicity and should be avoided in renal impairment if suitable alternatives are available. CRRT dose adjustment is not required. Echinocandins are highly protein bound with minimal renal excretion, therefore no dose adjustment is required in renal failure, and CRRT has no clinically significant effect on drug removal [108], making them an optimal choice.
Chronic and acute liver failure is frequently seen in ICU patients. Drug-induced liver injury (DILI) is a risk with all azoles; therefore, caution is required in pre-existing moderate or severe liver disease and alternatives considered. No dose adjustment is required for amphotericin [109]. Anidulafungin is the only echinocandin eliminated through extrahepatic metabolism [110] and therefore often the preferred agent in hepatic impairment.
ECMO is increasingly used for cardiorespiratory support in ICU; altered antifungal PK/PD may occur due to drug sequestration, increased volume of distribution, and drug clearance changes while on the ECMO circuit, but data are scarce [111]. Micafungin extraction by ECMO was demonstrated in an ex vivo study [112]; however, there are conflicting data with caspofungin [113, 114], the latter study demonstrating adequate levels at usual doses. Satisfactory liposomal amphotericin B levels at standard dosing on ECMO are reported [115], while others administering higher doses (10 mg/kg/day) found a ~ 50% reduction in Cmax [116]. Due to increased volume distribution, larger fluconazole loading doses were required in children; however, adult data are lacking [111, 117]. Voriconazole sequestration is reported, although the degree of sequestration changes with time, possibly due to saturation of ECMO circuit binding sites [114]. Hence frequent azole TDM is crucial yet rarely available in real time, highlighting a pressing need for development of point-of-care antifungal TDM in ICU patients. Given expanding ICU ECMO use and its association with higher IFI risk, further antifungal PK/PD studies are needed as current data are insufficient to adequately inform antifungal ECMO guidelines.
Conclusion
The diagnosis and management of IC poses many challenges in critical care; numerous unanswered questions remain as research priorities (Table 5). Improved identification of at-risk patients and the widening spectrum of diagnostics and therapeutics available for IC are promising. Personalized approaches to drug dosing and monitoring treatment response are needed. The key knowledge gap remaining is how tools such as risk scores and NCBTs can best be implemented in ICU practice to optimize clinical outcomes whilst exercising antifungal stewardship.
References
Clancy CJ, Nguyen MH (2013) Finding the missing 50% of invasive candidiasis: how nonculture diagnostics will improve understanding of disease spectrum and transform patient care. Clin Infect Dis 56:1284–1292. https://doi.org/10.1093/cid/cit006
Poissy J, Damonti L, Bignon A et al (2020) Risk factors for candidemia: a prospective matched case-control study. Crit Care. https://doi.org/10.1186/s13054-020-2766-1
Delaloye J, Calandra T (2014) Invasive candidiasis as a cause of sepsis in the critically ill patient. Virulence 5:161–169. https://doi.org/10.4161/viru.26187
Kett DH, Azoulay E, Echeverria PM, Vincent JL (2011) Candida bloodstream infections in intensive care units: analysis of the extended prevalence of infection in intensive care unit study. Crit Care Med 39:665–670. https://doi.org/10.1097/CCM.0b013e318206c1ca
Paiva JA, Pereira JM, Tabah A et al (2016) Characteristics and risk factors for 28-day mortality of hospital acquired fungemias in ICUs: data from the EUROBACT study. Crit Care 20:53. https://doi.org/10.1186/s13054-016-1229-1
Bassetti M, Giacobbe DR, Vena A et al (2019) Incidence and outcome of invasive candidiasis in intensive care units (ICUs) in Europe: results of the EUCANDICU project. Crit Care 23:219. https://doi.org/10.1186/s13054-019-2497-3
Koehler P, Stecher M, Cornely OA et al (2019) Morbidity and mortality of candidaemia in Europe: an epidemiologic meta-analysis. Clin Microbiol Infect 25:1200–1212. https://doi.org/10.1016/j.cmi.2019.04.024
Bassetti M, Righi E, Ansaldi F et al (2015) A multicenter multinational study of abdominal candidiasis: epidemiology, outcomes and predictors of mortality. Intensive Care Med 41:1601–1610. https://doi.org/10.1007/s00134-015-3866-2
Kullberg BJ, Arendrup MC (2015) Invasive candidiasis. N Engl J Med 373:1445–1456
Spellberg BJ, Filler SG, Edwards JE (2006) Current treatment strategies for disseminated Candidiasis. Clin Infect Dis 42:244–251. https://doi.org/10.1086/499057
Kumar V, Cheng S-C, Johnson MD et al (2014) Immunochip SNP array identifies novel genetic variants conferring susceptibility to candidaemia. Nat Commun 5:4675. https://doi.org/10.1038/ncomms5675
Vincent J-L, Lefrant J-Y, Kotfis K et al (2018) Comparison of European ICU patients in 2012 (ICON) versus 2002 (SOAP). Intensive Care Med 44:337–344. https://doi.org/10.1007/s00134-017-5043-2
Karagiannidis C, Brodie D, Strassmann S et al (2016) Extracorporeal membrane oxygenation: evolving epidemiology and mortality. Intensive Care Med 42:889–896. https://doi.org/10.1007/s00134-016-4273-z
Bell T, O’Grady NP (2017) Prevention of central line-associated bloodstream infections. Infect Dis Clin N Am 31:551–559
Vincent JL, Sakr Y, Singer M et al (2020) Prevalence and outcomes of infection among patients in intensive care units in 2017. J Am Med Assoc 323:1478–1487. https://doi.org/10.1001/jama.2020.2717
Tortorano AM, Dho G, Prigitano A et al (2012) Invasive fungal infections in the intensive care unit: a multicentre, prospective, observational study in Italy (2006–2008). Mycoses 55:73–79. https://doi.org/10.1111/j.1439-0507.2011.02044.x
Montagna MT, Caggiano G, Lovero G et al (2013) Epidemiology of invasive fungal infections in the intensive care unit: results of a multicenter Italian survey (AURORA project). Infection 41:645–653
Baldesi O, Bailly S, Ruckly S et al (2017) ICU-acquired candidaemia in France: epidemiology and temporal trends, 2004–2013—a study from the REA-RAISIN network. J Infect 75:59–67. https://doi.org/10.1016/j.jinf.2017.03.011
Lamoth F, Lockhart SR, Berkow EL, Calandra T (2018) Changes in the epidemiological landscape of invasive candidiasis. J Antimicrob Chemother 73:i4–i13. https://doi.org/10.1093/jac/dkx444
Chakrabarti A, Sood P, Rudramurthy SM et al (2015) Incidence, characteristics and outcome of ICU-acquired candidemia in India. Intensive Care Med 41:285–295. https://doi.org/10.1007/s00134-014-3603-2
Nucci M, Queiroz-Telles F, Alvarado-Matute T et al (2013) Epidemiology of candidemia in Latin America: a laboratory-based survey. PLoS ONE 8:e59373. https://doi.org/10.1371/journal.pone.0059373
Lockhart SR, Iqbal N, Cleveland AA et al (2012) Species identification and antifungal susceptibility testing of Candida bloodstream isolates from population-based surveillance studies in two US cities from 2008 to 2011. J Clin Microbiol 50:3435–3442. https://doi.org/10.1128/JCM.01283-12
Pfaller MA, Diekema DJ, Turnidge JD et al (2019) Twenty years of the SENTRY antifungal surveillance program: results for Candida species from 1997–2016. Open forum Infect Dis 6:S79–S94. https://doi.org/10.1093/ofid/ofy358
Alexander BD, Johnson MD, Pfeiffer CD et al (2013) Increasing echinocandin resistance in candida glabrata: clinical failure correlates with presence of FKS mutations and elevated minimum inhibitory concentrations. Clin Infect Dis 56:1724–1732. https://doi.org/10.1093/cid/cit136
Pfaller MA, Castanheira M, Lockhart SR et al (2012) Frequency of decreased susceptibility and resistance to echinocandins among fluconazole-resistant bloodstream isolates of Candida glabrata. J Clin Microbiol 50:1199–1203. https://doi.org/10.1128/JCM.06112-11
Vallabhaneni S, Cleveland AA, Farley MM et al (2015) Epidemiology and risk factors for echinocandin nonsusceptible Candida glabrata bloodstream infections: data from a large multisite population-based candidemia surveillance program, 2008–2014. Open Forum Infect Dis. https://doi.org/10.1093/ofid/ofv163
Pham CD, Iqbal N, Bolden CB et al (2014) Role of FKS mutations in Candida glabrata: MIC values, echinocandin resistance, and multidrug resistance. Antimicrob Agents Chemother 58:4690–4696. https://doi.org/10.1128/AAC.03255-14
Cortegiani A, Misseri G, Chowdhary A (2019) What’s new on emerging resistant Candida species. Intensive Care Med 45:512–515
Van Schalkwyk E, Mpembe RS, Thomas J et al (2019) Epidemiologic shift in Candidemia driven by Candida auris, South Africa, 2016–2017. Emerg Infect Dis 25:1698–1707. https://doi.org/10.3201/eid2509.190040
Ostrowsky B, Greenko J, Adams E et al (2020) Candida auris isolates resistant to three classes of antifungal medications—New York, 2019. MMWR Morb Mortal Wkly Rep 69:6–9. https://doi.org/10.15585/mmwr.mm6901a2
Eggimann P, Pittet D (2014) Candida colonization index and subsequent infection in critically ill surgical patients: 20 years later. Intensive Care Med 40:1429–1448. https://doi.org/10.1007/s00134-014-3355-z
Lortholary O, Desnos-Ollivier M, Sitbon K et al (2011) Recent exposure to caspofungin or fluconazole influences the epidemiology of candidemia: a prospective multicenter study involving 2441 patients. Antimicrob Agents Chemother 55:532–538. https://doi.org/10.1128/AAC.01128-10
Jensen RH, Johansen HK, Søes LM et al (2016) Posttreatment antifungal resistance among colonizing Candida isolates in candidemia patients: results from a systematic multicenter study. Antimicrob Agents Chemother 60:1500–1508. https://doi.org/10.1128/AAC.01763-15
Healey KR, Nagasaki Y, Zimmerman M et al (2017) The gastrointestinal tract is a major source of echinocandin drug resistance in a murine model of Candida glabrata colonization and systemic dissemination. Antimicrob Agents Chemother. https://doi.org/10.1128/AAC.01412-17
Thomaz DY, De Almeida JN, Lima GME et al (2018) An azole-resistant Candida parapsilosis outbreak: clonal persistence in the intensive care unit of a Brazilian teaching hospital. Front Microbiol. https://doi.org/10.3389/fmicb.2018.02997
Goemaere B, Lagrou K, Spriet I et al (2018) Clonal spread of Candida glabrata bloodstream isolates and fluconazole resistance affected by prolonged exposure: a 12-year single-center study in Belgium. Antimicrob Agents Chemother. https://doi.org/10.1128/AAC.00591-18
Schelenz S, Hagen F, Rhodes JL et al (2016) First hospital outbreak of the globally emerging Candida auris in a European hospital. Antimicrob Resist Infect Control 5:35. https://doi.org/10.1186/s13756-016-0132-5
Ku TSN, Walraven CJ, Lee SA (2018) Candida auris: disinfectants and implications for infection control. Front Microbiol 9:726
Eyre DW, Sheppard AE, Madder H et al (2018) A Candida auris outbreak and its control in an intensive care setting. N Engl J Med 379:1322–1331. https://doi.org/10.1056/NEJMoa1714373
Centers for Disease Control and Prevention (2020) Infection prevention and control for Candida auris. In: Fungal Dis. https://www.cdc.gov/fungal/candida-auris/c-auris-infection-control.html
Public Health England (2017) Candida auris: laboratory investigation, management and infection prevention and control. In: Public Health Engl. https://www.gov.uk/government/publications/candida-auris-laboratory-investigation-management-and-infection-prevention-and-control
Caceres DH, Forsberg K, Welsh RM et al (2019) Candida auris: a review of recommendations for detection and control in healthcare settings. J Fungi 5:111. https://doi.org/10.3390/jof5040111
Kollef M, Micek S, Hampton N et al (2012) Septic shock attributed to Candida infection: importance of empiric therapy and source control. Clin Infect Dis 54:1739–1746. https://doi.org/10.1093/cid/cis305
Azoulay E, Dupont H, Tabah A et al (2012) Systemic antifungal therapy in critically ill patients without invasive fungal infection*. Crit Care Med 40:813–822. https://doi.org/10.1097/CCM.0b013e318236f297
Pittet D, Monod M, Suter PM et al (1994) Candida colonization and subsequent infections in critically ill surgical patients. Ann Surg 220:751–758. https://doi.org/10.1097/00000658-199412000-00008
León C, Ruiz-Santana S, Saavedra P et al (2006) A bedside scoring system (“Candida score”) for early antifungal treatment in nonneutropenic critically ill patients with Candida colonization. Crit Care Med 34:730–737. https://doi.org/10.1097/01.CCM.0000202208.37364.7D
Ostrosky-Zeichner L, Pappas PG, Shoham S et al (2011) Improvement of a clinical prediction rule for clinical trials on prophylaxis for invasive candidiasis in the intensive care unit. Mycoses 54:46–51. https://doi.org/10.1111/j.1439-0507.2009.01756.x
Haydour Q, Hage CA, Carmona EM et al (2019) Diagnosis of fungal infections a systematic review and meta-analysis supporting American thoracic society practice guideline. Ann Am Thorac Soc 16:1179–1188
Karageorgopoulos DE, Vouloumanou EK, Ntziora F et al (2011) d-Glucan assay for the diagnosis of invasive fungal infections: a meta-analysis. Clin Infect Dis 52:750–770. https://doi.org/10.1093/cid/ciq206
He S, Hang JP, Zhang L et al (2015) A systematic review and meta-analysis of diagnostic accuracy of serum 1,3-β-d-glucan for invasive fungal infection: focus on cutoff levels. J Microbiol Immunol Infect 48:351–361
Mikulska M, Calandra T, Sanguinetti M et al (2010) The use of mannan antigen and anti-mannan antibodies in the diagnosis of invasive candidiasis: recommendations from the Third European conference on Infections in Leukemia. Crit Care. https://doi.org/10.1186/cc9365
Wei S, Wu T, Wu Y et al (2019) Diagnostic accuracy of Candida albicans germ tube antibody for invasive candidiasis: systematic review and meta-analysis. Diagn Microbiol Infect Dis 93:339–345. https://doi.org/10.1016/j.diagmicrobio.2018.10.017
Chang SS, Hsieh WH, Liu TS et al (2013) Multiplex PCR system for rapid detection of pathogens in patients with presumed sepsis—a systemic review and meta-analysis. PLoS ONE. https://doi.org/10.1371/journal.pone.0062323
Avni T, Leibovici L, Paul M (2011) PCR diagnosis of invasive candidiasis: systematic review and meta-analysis. J Clin Microbiol 49:665–670. https://doi.org/10.1128/JCM.01602-10
Tang DL, Chen X, Zhu CG et al (2019) Pooled analysis of T2 Candida for rapid diagnosis of candidiasis. BMC Infect Dis 19:798. https://doi.org/10.1186/s12879-019-4419-z
Hanson KE, Pfeiffer CD, Lease ED et al (2012) β-d-glucan surveillance with preemptive anidulafungin for invasive candidiasis in intensive care unit patients: a randomized pilot study. PLoS ONE 7:e42282. https://doi.org/10.1371/journal.pone.0042282
Ostrosky-Zeichner L, Shoham S, Vazquez J et al (2014) MSG-01: a randomized, double-blind, placebo-controlled trial of caspofungin prophylaxis followed by preemptive therapy for invasive candidiasis in high-risk adults in the critical care setting. Clin Infect Dis 58:1219–1226. https://doi.org/10.1093/cid/ciu074
Knitsch W, Vincent J-L, Utzolino S et al (2015) A randomized, placebo-controlled trial of preemptive antifungal therapy for the prevention of invasive candidiasis following gastrointestinal surgery for intra-abdominal infections. Clin Infect Dis 61:1671–1678. https://doi.org/10.1093/cid/civ707
Timsit JF, Azoulay E, Schwebel C et al (2016) Empirical micafungin treatment and survival without invasive fungal infection in adults with ICU-acquired sepsis, candida colonization, and multiple organ failure the empiricus randomized clinical trial. J Am Med Assoc 316:1555–1564. https://doi.org/10.1001/jama.2016.14655
Nucci M, Nouér SA, Esteves P et al (2016) Discontinuation of empirical antifungal therapy in ICU patients using 1,3-β-d-glucan. J Antimicrob Chemother 71:2628–2633. https://doi.org/10.1093/jac/dkw188
Rouzé A, Loridant S, Poissy J et al (2017) Biomarker-based strategy for early discontinuation of empirical antifungal treatment in critically ill patients: a randomized controlled trial. Intensive Care Med 43:1668–1677. https://doi.org/10.1007/s00134-017-4932-8
Pappas PG, Lionakis MS, Arendrup MC et al (2018) Invasive candidiasis. Nat Rev Dis Prim 4:18026. https://doi.org/10.1038/nrdp.2018.26
Eggimann P, Bille J, Marchetti O (2011) Diagnosis of invasive candidiasis in the ICU. Ann Intensive Care 1:37. https://doi.org/10.1186/2110-5820-1-37
Garbino J, Lew DP, Romand JA et al (2002) Prevention of severe Candida infections in nonneutropenic, high-risk, critically ill patients: a randomized, double-blind, placebo-controlled trial in patients treated by selective digestive decontamination. Intensive Care Med 28:1708–1717. https://doi.org/10.1007/s00134-002-1540-y
Piarroux R, Grenouillet F, Balvay P et al (2004) Assessment of preemptive treatment to prevent severe candidiasis in critically ill surgical patients. Crit Care Med 32:2443–2449. https://doi.org/10.1097/01.ccm.0000147726.62304.7f
Senn L, Eggimann P, Ksontini R et al (2009) Caspofungin for prevention of intra-abdominal candidiasis in high-risk surgical patients. Intensive Care Med 35:903–908. https://doi.org/10.1007/s00134-009-1405-8
Ferreira D, Grenouillet F, Blasco G et al (2015) Outcomes associated with routine systemic antifungal therapy in critically ill patients with Candida colonization. Intensive Care Med 41:1077–1088. https://doi.org/10.1007/s00134-015-3791-4
Harrison D, Muskett H, Harvey S et al (2013) Development and validation of a risk model for identification of non-neutropenic, critically-ill, adult patients at high risk of invasive Candida infection. Health Technol Assess (Rockv) 17:1–30. https://doi.org/10.3310/hta17030
Clancy CJ, Nguyen MH (2018) Non-culture diagnostics for invasive candidiasis: promise and unintended consequences. J Fungi 4:27
Cortegiani A, Russotto V, Maggiore A et al (2016) Antifungal agents for preventing fungal infections in non-neutropenic critically ill patients. Cochrane Database Syst Rev 1:CD004920
Bailly S, Leroy O, Montravers P et al (2015) Antifungal de-escalation was not associated with adverse outcome in critically ill patients treated for invasive candidiasis: post hoc analyses of the AmarCAND2 study data. Intensive Care Med 41:1931–1940. https://doi.org/10.1007/s00134-015-4053-1
Jaffal K, Poissy J, Rouze A et al (2018) De-escalation of antifungal treatment in critically ill patients with suspected invasive Candida infection: incidence, associated factors, and safety. Ann Intensive Care 8:49. https://doi.org/10.1186/s13613-018-0392-8
Johnson MD, Lewis RE, Dodds Ashley ES et al (2020) Core recommendations for antifungal stewardship: a statement of the mycoses study group education and research consortium. J Infect Dis 222:S175–S198. https://doi.org/10.1093/infdis/jiaa394
Martin-Loeches I, Antonelli M, Cuenca-Estrella M et al (2019) ESICM/ESCMID task force on practical management of invasive candidiasis in critically ill patients. Intensive Care Med 45:789–805. https://doi.org/10.1007/s00134-019-05599-w
León C, Ruiz-Santana S, Saavedra P et al (2012) Value of β-d-glucan and Candida albicans germ tube antibody for discriminating between Candida colonization and invasive candidiasis in patients with severe abdominal conditions. Intensive Care Med 38:1315–1325. https://doi.org/10.1007/s00134-012-2616-y
Giacobbe DR, Mikulska M, Tumbarello M et al (2017) Combined use of serum (1,3)-β-d-glucan and procalcitonin for the early differential diagnosis between candidaemia and bacteraemia in intensive care units. Crit Care 21:176. https://doi.org/10.1186/s13054-017-1763-5
Arendrup MC, Andersen JS, Holten MK et al (2019) Diagnostic performance of T2Candida among ICU patients with risk factors for invasive candidiasis. Open forum Infect Dis 6:ofz136. https://doi.org/10.1093/ofid/ofz136
Lamoth F, Clancy CJ, Tissot F et al (2020) Performance of the T2Candida panel for the diagnosis of intra-abdominal candidiasis. Open Forum Infect Dis. https://doi.org/10.1093/ofid/ofaa075
Rouze A, Poissy J, Sendid B, Nseir S (2018) Biomarkers in early treatment of invasive candidiasis. Hosp Pract 46:239–242. https://doi.org/10.1080/21548331.2018.1516105
Gill CM, Kenney RM, Hencken L et al (2019) T2 Candida versus beta-d-glucan to facilitate antifungal discontinuation in the intensive care unit. Diagn Microbiol Infect Dis 95:162–165. https://doi.org/10.1016/J.DIAGMICROBIO.2019.04.016
Rautemaa-Richardson R, Rautemaa V, Al-Wathiqi F et al (2018) Impact of a diagnostics-driven antifungal stewardship programme in a UK tertiary referral teaching hospital. J Antimicrob Chemother 73:3488–3495. https://doi.org/10.1093/jac/dky360
Kritikos A, Poissy J, Poissy J et al (2020) Impact of the beta-glucan test on management of intensive care unit patients at risk for invasive candidiasis. J Clin Microbiol. https://doi.org/10.1128/JCM.01996-19
Hage CA, Carmona EM, Epelbaum O et al (2019) Microbiological laboratory testing in the diagnosis of fungal infections in pulmonary and critical care practice: an official American thoracic society clinical practice guideline. Am J Respir Crit Care Med 200:535–550
Mylonakis E, Zacharioudakis IM, Clancy CJ et al (2018) Efficacy of T2 magnetic resonance assay in monitoring candidemia after initiation of antifungal therapy: the serial therapeutic and antifungal monitoring protocol (STAMP) trial. J Clin Microbiol 56:e01756–e1817. https://doi.org/10.1128/JCM.01756-17
Jaijakul S, Vazquez JA, Swanson RN, Ostrosky-Zeichner L (2012) (1,3)-d-Glucan as a prognostic marker of treatment response in invasive candidiasis. Clin Infect Dis 55:521–526. https://doi.org/10.1093/cid/cis456
Angebault C, Lanternier F, Dalle F, et al (2016) Prospective Evaluation of Serum β-Glucan Testing in Patients With Probable or Proven Fungal Diseases. Open Forum Infect Dis 3:ofw128. https://doi.org/10.1093/ofid/ofw128
Koo S, Baden LR, Marty FM (2012) Post-diagnostic kinetics of the (1 → 3)-β-d-glucan assay in invasive aspergillosis, invasive candidiasis and Pneumocystis jirovecii pneumonia. Clin Microbiol Infect 18:E122–E127. https://doi.org/10.1111/j.1469-0691.2012.03777.x
Tissot F, Lamoth F, Hauser PM et al (2013) β-Glucan antigenemia anticipates diagnosis of blood culture-negative intraabdominal candidiasis. Am J Respir Crit Care Med 188:1100–1109. https://doi.org/10.1164/rccm.201211-2069OC
Poissy J, Sendid B, Damiens S et al (2014) Presence of Candida cell wall derived polysaccharides in the sera of intensive care unit patients: relation with candidaemia and Candida colonisation. Crit Care 18:R135. https://doi.org/10.1186/cc13953
Giacobbe DR, Berruti M, Mikulska M (2019) Prognostic impact of negative serum (1,3)-β-d-glucan in patients with candidemia. Clin Infect Dis. https://doi.org/10.1093/cid/ciz1051
Agnelli C, Bouza E, Martínez-Jiménez MDC et al (2020) Clinical relevance and prognostic value of persistently negative (1,3)-β-d-glucan in adults with candidemia: a 5-year experience in a tertiary hospital. Clin Infect Dis 70:1925–1932. https://doi.org/10.1093/cid/ciz555
Gintjee TJ, Donnelley MA, Thompson GR (2020) Aspiring antifungals: review of current antifungal pipeline developments. J Fungi 6:28. https://doi.org/10.3390/jof6010028
Pappas PG, Kauffman CA, Andes DR et al (2015) Clinical practice guideline for the management of candidiasis: 2016 update by the infectious diseases society of America. Clin Infect Dis 62:e1–e50
Cornely OA, Bassetti M, Calandra T et al (2012) ESCMID guideline for the diagnosis and management of Candida diseases 2012: non-neutropenic adult patients. Clin Microbiol Infect 18:19–37. https://doi.org/10.1111/1469-0691.12039
Reboli AC, Rotstein C, Pappas PG et al (2007) Anidulafungin versus fluconazole for invasive candidiasis. N Engl J Med 356:2472–2482. https://doi.org/10.1056/NEJMoa066906
Kett DH, Shorr AF, Reboli AC et al (2011) Anidulafungin compared with fluconazole in severely ill patients with candidemia and other forms of invasive candidiasis: support for the 2009 IDSA treatment guidelines for candidiasis. Crit Care 15:R253. https://doi.org/10.1186/cc10514
López-Cortés LE, Almirante B, Cuenca-Estrella M et al (2016) Empirical and targeted therapy of candidemia with fluconazole versus echinocandins: a propensity score–derived analysis of a population-based, multicentre prospective cohort. Clin Microbiol Infect 22:733.e1–733.e8. https://doi.org/10.1016/j.cmi.2016.05.008
Murri R, Scoppettuolo G, Ventura G et al (2016) Initial antifungal strategy does not correlate with mortality in patients with candidemia. Eur J Clin Microbiol Infect Dis 35:187–193. https://doi.org/10.1007/s10096-015-2527-2
Bassetti M, Righi E, Ansaldi F et al (2014) A multicenter study of septic shock due to candidemia: outcomes and predictors of mortality. Intensive Care Med 40:839–845. https://doi.org/10.1007/s00134-014-3310-z
Garnacho-Montero J, Díaz-Martín A, Cantón-Bulnes L et al (2018) Initial antifungal strategy reduces mortality in critically ill patients with candidemia: a propensity score-adjusted analysis of a multicenter study. Crit Care Med 46:384–393. https://doi.org/10.1097/CCM.0000000000002867
Colombo AL, Guimarães T, Sukienik T et al (2014) Prognostic factors and historical trends in the epidemiology of candidemia in critically ill patients: an analysis of five multicenter studies sequentially conducted over a 9-year period. Intensive Care Med 40:1489–1498. https://doi.org/10.1007/s00134-014-3400-y
Kullberg BJ, Viscoli C, Pappas PG et al (2019) Isavuconazole versus caspofungin in the treatment of candidemia and other invasive Candida infections: the ACTIVE trial. Clin Infect Dis 68:1981–1989. https://doi.org/10.1093/cid/ciy827
Keane S, Geoghegan P, Povoa P et al (2018) Systematic review on the first line treatment of amphotericin B in critically ill adults with candidemia or invasive candidiasis. Expert Rev Anti Infect Ther 16:839–847
Vazquez J, Reboli AC, Pappas PG et al (2014) Evaluation of an early step-down strategy from intravenous anidulafungin to oral azole therapy for the treatment of candidemia and other forms of invasive candidiasis: results from an open-label trial. BMC Infect Dis. https://doi.org/10.1186/1471-2334-14-97
Tabah A, Bassetti M, Kollef MH et al (2020) Antimicrobial de-escalation in critically ill patients: a position statement from a task force of the European Society of Intensive Care Medicine (ESICM) and European Society of Clinical Microbiology and Infectious Diseases (ESCMID) Critically Ill Patients Study Group (ESGCIP). Intensive Care Med 46:245–265. https://doi.org/10.1007/s00134-019-05866-w
Chatelon J, Cortegiani A, Hammad E et al (2019) Choosing the right antifungal agent in ICU patients. Adv Ther 36:3308–3320
Bellmann R, Smuszkiewicz P (2017) Pharmacokinetics of antifungal drugs: practical implications for optimized treatment of patients. Infection 45:737–779
González de Molina FJ, de Martínez-Alberici MLA, Ferrer R (2014) Treatment with echinocandins during continuous renal replacement therapy. Crit Care 18:218
Tverdek FP, Kofteridis D, Kontoyiannis DP (2016) Antifungal agents and liver toxicity: a complex interaction. Expert Rev Anti Infect Ther 14:765–776
Aguilar G, Azanza JR, Carbonell JA et al (2014) Anidulafungin dosing in critically ill patients with continuous venovenous haemodiafiltration. J Antimicrob Chemother 69:1620–1623. https://doi.org/10.1093/jac/dkt542
Sherwin J, Heath T, Watt K (2016) Pharmacokinetics and dosing of anti-infective drugs in patients on extracorporeal membrane oxygenation: a review of the current literature. Clin Ther 38:1976–1994
Watt KM, Cohen-Wolkowiez M, Williams DC et al (2017) Antifungal extraction by the extracorporeal membrane oxygenation circuit. J Extra Corpor Technol 49:150–159
Ruiz S, Papy E, Da Silva D et al (2009) Potential voriconazole and caspofungin sequestration during extracorporeal membrane oxygenation. Intensive Care Med 35:183–184
Spriet I, Annaert P, Meersseman P et al (2009) Pharmacokinetics of caspofungin and voriconazole in critically ill patients during extracorporeal membrane oxygenation. J Antimicrob Chemother 63:767–770. https://doi.org/10.1093/jac/dkp026
Foulquier JB, Berneau P, Frérou A et al (2019) Liposomal amphotericin B pharmacokinetics in a patient treated with extracorporeal membrane oxygenation. Med Mal Infect 49:69–71. https://doi.org/10.1016/j.medmal.2018.10.011
Zhao Y, Seelhammer TG, Barreto EF, Wilson JW (2020) Altered pharmacokinetics and dosing of liposomal amphotericin B and isavuconazole during extracorporeal membrane oxygenation. Pharmacotherapy 40:89–95. https://doi.org/10.1002/phar.2348
Watt KM, Gonzalez D, Benjamin DK et al (2015) Fluconazole population pharmacokinetics and dosing for prevention and treatment of invasive candidiasis in children supported with extracorporeal membrane oxygenation. Antimicrob Agents Chemother 59:3935–3943. https://doi.org/10.1128/AAC.00102-15
Funding
None.
Author information
Authors and Affiliations
Contributions
CL, TB and IML conceived the idea; CL performed the literature search and drafted the manuscript, which was critically reviewed and revised by IML and TB.
Corresponding author
Ethics declarations
Conflicts of interest
IML has received speaking and advisory board fees from Merck and Gilead Sciences. TB has received speaking fees from Pfizer and speaking, advisory board fees and research support from Gilead Sciences. CL has received research support from Gilead Sciences.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Logan, C., Martin-Loeches, I. & Bicanic, T. Invasive candidiasis in critical care: challenges and future directions. Intensive Care Med 46, 2001–2014 (2020). https://doi.org/10.1007/s00134-020-06240-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-020-06240-x