Abstract
Purpose
Increasingly, very old patients are admitted to Intensive Care Units (ICUs). The objective of this study was to describe 12-month outcomes of these patients and determine which characteristics are associated with a return to baseline physical function 1 year later.
Methods
In this prospective cohort study in 22 Canadian hospitals, we recruited 610 patients aged 80 years or older who were admitted to ICU for at least 24 h. At baseline, we completed a comprehensive geriatric assessment and followed patients to determine 12-month survival and physical function. Our primary outcome was physical recovery from critical illness at 12 months, defined as being alive with Short Form-36 physical function score of at least 10 points, and not 10 or more points below baseline. We used regression analysis to examine factors associated with physical recovery.
Results
Patients were on average 84 years old (range 80–99). Mortality was 14 % in ICU, 26 % in hospital and 44 % at 12 months after admission. Of 505 patients evaluable at 12 months, 26 % achieved physical recovery. In the multivariable model, physical recovery was significantly associated with younger age, lower APACHE II score, lower Charlson comorbidity score, lower frailty index, lower baseline physical function score, and specific admission diagnoses.
Conclusions
One-quarter of patients aged 80 years or older who are admitted to ICU survived and returned to baseline levels of physical function at 1 year. Routine assessment of baseline physical function and frailty status could aid in prognostication and informed decision-making for very old critically ill patients. (ClinicalTrials.gov number NCT01293708).
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Purpose
An increasing number of very old (aged 80 or older) patients are being admitted to intensive care units (ICUs) [1, 2]. Uncertainty about outcomes after admission to ICU for these patients has prompted evaluation of their long-term mortality and health-related quality-of-life (HRQOL). Long-term mortality rates range from 55 to 90 % at 3 years [3–5], while in some studies, mortality is similar to old patients who are denied ICU admission [6, 7]. Longitudinal studies yielded mixed results, showing either acceptable [8–18] or poor long-term quality-of-life [19–22]. However, these investigations have been limited by single-center enrolment, small sample sizes, and use of non-validated functional outcome measures. The largest study of long-term HRQOL in old survivors of critical illness enrolled 299 patients [3]. No studies have comprehensively evaluated the determinants of long-term functional recovery after critical illness in these patients.
Other research has documented poor communication and decision-making regarding the use of life-sustaining treatments for these old, critically ill patients [23–25]. A major barrier to optimal decision-making is accurate prognostication in this group. Inadequately informed decision-making can have adverse clinical and psychological consequences for patients and families, and substantial economic consequences for healthcare systems [26, 27]. A clearer understanding of the determinants of long-term outcomes for critically ill patients aged 80 and older may lead to decision-making for these vulnerable individuals that is more consistent with their values.
Our primary objective was to determine the physical recovery of patients at least 80 years of age 1 year after their admission to Canadian ICUs. The secondary objective was to identify factors associated with return to baseline physical function 1 year after ICU admission. A priori, we hypothesized that baseline measures of frailty and physical function, and reason for admission to ICU, would be determinants of 12-month physical recovery, after adjusting for confounding variables, such as illness severity and comorbidities.
Methods
Study protocol
The primary purpose of this study was to develop a longitudinal cohort that we would follow for 12 months involving interviews with patients (if able) and their family members. Recognizing that the recruitment of such patients would reflect a select patient population, we collected ICU and hospital data from chart review on all consecutive patients admitted to the participating ICUs without requiring consent. For this analysis, we define 2 mutually exclusive cohorts: (1) the “longitudinal cohort” of consenting participants and their primary caregivers followed for 12 months, and (2) an unselected “hospital cohort” of consecutive patients not participating in the longitudinal cohort. In participating centers, all patients aged 80 years or older who were admitted to ICUs were eligible for the hospital cohort, but we excluded patients who remained in ICU for less than 24 h. Patients 80 years or older who were admitted to ICU for at least 24 h were eligible for the longitudinal cohort. From the longitudinal cohort, we excluded non-residents of Canada and patients who did not have available family members because we depended on family members for complete data collection. Family members (including partners, significant others, and friends) were eligible if they: (1) spoke English or French; (2) visited the patient at least once during the ICU admission; and (3) were at least 18 years old. For the longitudinal cohort, we obtained consent from the patient’s legal representative or participating family member before enrolment, and subsequently from competent, surviving patients.
Study procedures
Upon enrolment into the longitudinal cohort, trained research personnel administered the comprehensive geriatric assessment (CGA) questionnaire in-person to a family member [28]. For this questionnaire, family members were asked to consider the patient’s condition 2 weeks before hospitalization. The CGA questionnaire enabled calculation of the frailty index, which has been validated in population studies [29, 30]. The frailty index identifies 43 deficits at baseline (Supplementary Appendix 1 eTable 1), each coded as 0 (absent), 1 (present), or 0.5 (where intermediate values were possible). It was calculated as the cumulative proportion of deficits present (minimum score 0; maximum score 1.0), and then graded as mild (>0 and ≤0.2), moderate (>0.2 and <0.4) or severe frailty (≥0.4). Additional variables collected from family members and abstracted from hospital records are shown in Tables 1 and 2 and described in Supplementary Appendix 1.
In the longitudinal cohort, at 3, 6, 9 and 12 months after enrolment, hospital survivors (or family members) were contacted by telephone to record survival status and physical function using the Short Form (SF-36), a 36-item survey of general health status with summary physical component scale and mental component scales [31]. During follow-up, if patients were unable to participate in data collection, family members were asked to complete the SF-36 from the perspective of the patient. Surrogate assessment of the SF-36 has been shown to be reliable, particularly for assessment of physical function [32].
Statistical analysis
Patient characteristics and hospital outcomes were compared between the longitudinal cohort and the hospital cohort. Continuous variables were described by means, standard deviations (SD) and ranges, except for the skewed length of stay variables which were described by medians, quartiles and ranges. Categorical variables were described by counts and percentages. Differences between the hospital and longitudinal cohorts were tested by the Mann–Whitney U test for continuous variables and the chi-square test for categorical variables.
Our primary outcome was physical recovery from critical illness, defined as being alive with SF-36 physical function score of at least 10, and no more than 10 points below baseline. The SF-36 physical functioning domain ranges from 0 (worst score) to 100 (best score) and raw scores are reported for survivors and compared to Canadian age- and sex-matched community controls [33]. A 10-point change is considered small but clinically important; we required patients to have a score greater than 10 to avoid floor effects [34]. We combined survival with the physical function domain score to more comprehensively describe outcomes relevant to this population; for many older persons, quality-of-life and functional capacity are more important than just survival [35]. Patients who died were not considered to have recovered. When estimating physical recovery, we employed fully conditional multiple imputation to reduce potential bias due to loss to follow-up [36]. As described in the Supplementary Appendix 2, the imputation model utilized baseline patient characteristics as well as available 3-, 6- and 9-month SF-36 physical function scores. The estimates of the physical recovery rate and all regression models account for clustering by center by treating center as the primary sampling unit as implemented by the survey procedures of SAS [37].
Unadjusted associations between baseline characteristics and physical recovery at 12 months were estimated by odds ratios (OR) derived from single predictor logistic regression models. We then performed multivariable logistic regression including all baseline characteristics presented in Table 3. Continuous predictors were scaled so that one unit was approximately equal to the interquartile range. This analysis was repeated focusing on 12-month mortality and a separate linear regression model was developed for the 12-month physical recovery of survivors. We evaluated for multicollinearity among the independent variables using variance inflation factors; the largest was 2.6, indicating no such difficulties.
To assess representativeness of the longitudinal cohort, we re-estimated our models of 12-month survival and physical recovery using inverse probability weighting (IPW) so the weighted longitudinal cohort more closely reflected the unselected hospital cohort. Details of the IPW and treatment of missing data (including multiple imputation and sensitivity analyses) are provided in Supplementary Appendix 2.
Analyses were done using SAS Version 9.4 (SAS Inc., Cary, NC., USA).
Role of the funding source
The funding agency had no role in data collection, analysis, or interpretation, writing of the report or decision to submit the paper for publication.
Results
Of 3064 consecutive patients 80 years or older screened for eligibility, 2450 met the inclusion criterion of ICU admission for at least 24 h. From these, 610 patients comprise our longitudinal cohort and an additional 894 patients comprise our hospital chart review cohort (Figure e1a). By the 12-month assessment in the longitudinal cohort, 40 patients had withdrawn consent or refused to respond and 63 were missed or lost to follow-up, leaving 507 patients with known 12-month status. (eFigure 1b). The primary outcome of recovered physical function at 12 months was available in 505 patients (2 patients had missing baseline SF-36 scores). Tables 1 and 2 of Supplementary Appendix 2 compare the baseline characteristics and hospital outcomes between patients with a known versus unknown primary outcome.
Patients in the longitudinal cohort were on average 84 years old (range 80–99), 55 % were men, 62 % had a medical admission diagnosis, 87 % lived at home before hospital admission, 19 % were moderately to severely frail and the average (SD) baseline physical function score was 40 (30) (Table 1). Characteristics of the longitudinal cohort were similar to those of the unselected hospital cohort, but the longitudinal cohort had a higher proportion of patients who had CABG or valve replacement.
Compared to the hospital cohort, the longitudinal cohort had significantly longer ICU (median of 6 vs. 4 days) and hospital (median of 21 vs. 16 days) stays but significantly lower ICU (14 vs. 24 %) and hospital mortality (26 vs. 39 %) rates (Table 2). In patients in the longitudinal cohort, of 526 patients who lived at home before ICU admission, only 179 (34 %) were discharged home and the proportion of patients discharged home decreased with increasing frailty index (Table 2).
12-month follow up data
The 12-month survival rate in the longitudinal cohort sample was 56 %. Using inverse probability weighting (IPW) to reflect the unselected hospital cohort, 12-month survival was estimated to be 50 %.
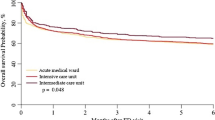
ICU survivors had significantly lower physical function and physical component SF-36 scores compared to age- and sex-matched community controls at all time points (eFigure 2). By 12 months, an estimated 26 % (95 % CI 21–31 %) of the longitudinal cohort had physically recovered (Fig. 1). Using inverse probability weighting to reflect the unselected hospital cohort, the 12-month physical recovery rate was estimated at 24 (18–30 %). Table 6 of the Supplementary Appendix 2 shows the minimal impact of IPW, multiple imputation and the method for accounting for site clustering on estimates of physical recovery. eFigure 3 shows the physical recovery rates for patients with low baseline PF (<40) and high baseline PF (≥40).
Combined outcomes of mortality and change of physical function from baseline at different time points in the longitudinal cohort. Each section of the bar graph represents the proportion of patients who died or returned to varying levels of baseline function as denoted by the legend (PF physical function)
In both the single predictor and multivariable models, younger age, lower APACHE II score, lower Charlson comorbidity index, lower frailty index, and admission diagnosis of CABG/valve replacement were significantly associated with a greater likelihood of physical recovery. Conversely, after adjustment for other covariates, patients admitted for stroke had one-ninth the odds of returning to baseline physical function compared to other patients (Table 3). After adjusting for all other patient characteristics, a higher baseline physical function score was associated with a lower probability of physical recovery.
In the multivariable model, independent associations with survival included lower APACHE II score, admission diagnosis of CABG/valve replacement, lower Charlson comorbidity index, lower frailty index, and family preferences for more than comfort measures (eTable 2). When considering 12-month physical function score as the dependent variable amongst survivors, lower APACHE II scores, admission diagnosis of CABG/valve replacement, higher baseline physical function, lower frailty index, and family preference for more than comfort care were significantly associated with better physical function, whereas admission diagnosis of stroke was associated with significantly worse physical function (eTable 3).
We obtained similar estimates and the same conclusions for all three outcomes using inverse probability weighting so that the longitudinal cohort more closely represented the unselected hospital cohort (see Tables 4, 5, 6 of Supplementary Appendix 2).
Discussion
In this multicenter cohort study, we followed 610 very old patients admitted to 22 Canadian ICUs, and determined their survival and physical recovery 1 year after ICU admission. On average, patients spent just under 1 week in ICU and 3 weeks in hospital. Approximately 20 % died in the ICU, and an addition 12–15 % of patients discharged from ICU died prior to hospital discharge. At 1 year, 50 % had died, and survivors had reduced physical function compared to community controls, and only 26 % of patients were alive and had recovered back to, or near, their pre-hospital level of physical functioning. Only one-third of surviving patients who lived at home before ICU admission returned home; one-quarter of those who were moderately or severely frail at baseline returned home. In multivariable models, primary ICU diagnostic category, baseline physical function, pre-hospital frailty index and APACHE II score were the key predictors of recovery.
Prior studies have addressed long-term outcomes of very old people after critical illness, but most do not report an endpoint that meaningfully combined survival and return of physical function [4, 7, 9, 12, 15, 19]. In an observational study of 2646 patients aged 80 years or more, Boumendil and colleagues reported that 63 % either died or declined (defined as a one-point loss in at least one dimension of the Katz functional status scale) 6 months after enrollment [25]. Given our definition of recovery, this would translate to a recovery rate of approximately 35 % at 6 months.
Our most notable finding is that approximately one-quarter of patients returned to near their baseline physical state 1 year after ICU admission, and the determinants of recovery included variables related to both baseline function and acute illness. Higher baseline physical function was associated with higher 12-month survival, but not after adjusting for other baseline characteristics. Not surprisingly, higher baseline physical function was associated with significantly higher 12-month physical function both before and after covariate adjustment. It is important to note however, baseline physical function was not associated with our composite measure of physical recovery before adjustment and was negatively associated with physical recovery after controlling for the other baseline patient characteristics. This is because physical recovery required a return to within 10 points of baseline PF score which is more difficult to achieve for patients who start with a higher baseline score than a lower baseline score, especially after controlling for other characteristics. The clinical message here is that older patients with higher baseline physical function are more likely to survive, and, on average, if they survive will have a better PF long-term compared to patients with low baseline PF. This is the case even though their chances of returning to the prior level of physical function, after controlling for their other baseline characteristics, are reduced compared to patients who had low baseline PF prior to their critical illness.
Frailty was a more significant independent predictor than age, illness severity, or comorbidity, which are commonly considered important determinants of long-term outcomes (Table 3). Frailty is a multi-dimensional state characterized by loss of physiologic and cognitive reserves which accumulate in older patients and predict adverse events and unfavorable outcomes [29]. Frailty has only recently been recognized as an important determinant of mortality among older critically ill patients [38, 39], and was not included in previous longitudinal studies that examined functional recovery or quality-of-life outcomes of very old people who were admitted to ICU. The frailty index used in this study is based on an accumulation of deficits, reflecting that frailty (a multiply determined greater risk of adverse health outcomes compared with others of the same age [29]) will have different manifestations in different contexts. We measured more than 30 variables from the family and hospital record to determine this index. The frailty index is robust, such that many of the properties of the index are preserved despite differences in how the index is calculated across studies. In fact, within studies, it is possible to randomly select variables that make up an FI and get closely comparable results [40]. This property is a manifestation of the redundancy of biological systems. In short, not every item in a failing system need to be gathered to know that the system is failing [41]. Awareness of baseline frailty can inform discussions about the goals of care and expected outcomes of treatment.
Our longitudinal cohort study found lower short-term and 12-month mortality rates than those reported in other studies of old ICU patients [9, 10, 42, 43]. These findings may relate to enrollment of patients who were admitted to the ICU and who survived for at least 24 h. Therefore, our cohort may have a better prognosis than all old patients admitted to ICU. Furthermore, our longitudinal cohort required the presence of a caregiver, which may have been less likely for patients who were in the ICU very briefly; this hypothesis is supported by the higher mortality and shorter length of stay (ICU and hospital) in the hospital cohort compared to the longitudinal cohort. Also, differences in medical and surgical case-mix may explain differences in long-term outcomes between our study and other similar studies. Thus, compared to studies that enrolled consecutive, very old critically ill people, our study underestimates mortality and overestimates recovery of physical function. Our hospital cohort data gives us a sense of the magnitude of the potential differences in outcome between those enrolled and not enrolled in the longitudinal study. Using inverse probability weighting so that the longitudinal cohort would better reflect the unselected hospital cohort, we obtained 6 % higher 12-month mortality (from 44 to 50 %) and 2 % lower rate of physical recovery compared to the unweighted longitudinal cohort.
There are several strengths of this study. This is the largest longitudinal cohort study of very old patients admitted to ICU that evaluated 12-month outcomes and the determinants of those outcomes. Our study was unique in combining survival and physical recovery as a composite endpoint, recognizing the importance of function in these patients [35], and the utility of predicting future functional recovery for clinical decision-making in the ICU [44]. Our baseline evaluation of patients was comprehensive, and we used validated instruments including a structured assessment of frailty. Our results offer important insights about the role of frailty and other conditions and characteristics that are associated with 12-month outcomes in old critically ill patients. In contrast to previous single-center studies, our multicenter design enhances the generalizability of our findings to those old patients who survive more than 24 h after ICU admission.
Limitations of this study include the fact that a relatively large proportion of patients could not be followed, primarily due to withdrawal of consent and inability to track patients for 1 year after ICU admission. This may have influenced estimates of mortality and recovery, but should not have substantially affected the estimates of association between these outcomes and baseline patient characteristics. Multiple imputation and inverse probability weighting only minimally altered our estimate of 12-month physical recovery, and sensitivity analyses indicate that the estimated rate is fairly robust. We used a proxy family assessment for some baseline variables which is a limitation of most similar studies. This approach has been validated using a comprehensive geriatric assessment as the referent standard [28], which is unavoidable for such studies of critically ill participants, and is consistent with how these data will be used in ‘real-life’ practice. Most of the patients in our sample were Caucasian and are from a single health care system; this may limit the applicability of our results. Finally, we did not record complications, adverse events, or healthcare encounters after critical illness which may have influenced outcomes.
In conclusion, we observed that very old patients who are admitted to the ICU have a low probability of being alive and returning to baseline levels of physical function at 1 year after ICU admission. Clinicians should be aware of the determinants of these outcomes and consideration should be given to recording these measurements for older patients admitted to the ICU. Further research is needed to investigate strategies to systematically include this type of information for real-time decision-making, so that old patients, family members and clinicians become more familiar with the role of baseline frailty and physical function on the trajectory of critical illness.
References
Wunsch H, Linde-Zwirble WT, Harrison DA, Barnato AE, Rowan KM, Angus DC (2009) Use of intensive care services during terminal hospitalizations in England and the United States. Am J Respir Crit Care Med 180:875–880. doi:10.1164/rccm.200902-0201OC
Bagshaw SM, Webb SA, Delaney A, George C, Pilcher D, Hart GK, Bellomo R (2009) Very old patients admitted to intensive care in Australia and New Zealand: a multi-centre cohort analysis. Crit Care 13:R45. doi:10.1186/cc7768
Kaarlola A, Tallgren M, Pettilä V (2006) Long-term survival, quality of life, and quality-adjusted life-years among critically ill elderly patients. Crit Care Med 34:2120–2126
Boumendil A, Maury E, Reinhard I, Luquel L, Offenstadt G, Guidet B (2004) Prognosis of patients aged 80 years and over admitted in medical intensive care unit. Intensive Care Med 30:647–654
Broslawski GE, Elkins M, Algus M (1995) Functional abilities of elderly survivors of intensive care. J Am Osteopath Assoc 95:712–717
Boumendil A, Latouche A, Guidet B, ICE-CUB Study Group (2011) On the benefit of intensive care for very old patients. Arch Intern Med 171:1116–1117. doi:10.1001/archinternmed.2011.102
Garrouste-Orgeas M, Timsit JF, Montuclard L, Colvez A, Gattolliat O, Philippart F, Rigal G, Misset B, Carlet J (2006) Decision-making process, outcome, and 1 year quality of life of octogenarians referred for intensive care unit admission. Intensive Care Med 32:1045–1051
Hofhuis JG, van Stel HF, Schrijvers AJ, Rommes JH, Spronk PE (2011) Changes of health-related quality of life in critically ill octogenarians: a follow-up study. Chest 140:1473–1483. doi:10.1378/chest.10-0803
Tabah A, Philippart F, Timsit JF, Willems V, Français A, Leplège A, Carlet J, Bruel C, Misset B, Garrouste-Orgeas M (2010) Quality of life in patients aged 80 or over after ICU discharge. Crit Care 14:R2. doi:10.1186/cc8231
Montuclard L, Garrouste-Orgeas M, Timsit JF, Misset B, De Jonge B, Carlet J (2000) Outcome, functional autonomy, and quality of life of elderly patients with a long-term intensive care unit stay. Crit Care Med 28:3389–3395
Chelluri L, Pinsky MR, Donahoe MP, Grenvik A (1993) Long-term outcome of critically ill elderly patients requiring intensive care. JAMA 269:3119–3123
de Rooij SE, Govers AC, Korevaar JC, Giesbers AW, Levi M, de Jonge E (2008) Cognitive, functional, and quality-of-life outcomes of patients aged 80 and older who survived at least 1 year after planned or unplanned surgery or medical intensive care treatment. J Am Geriatr Soc 56:816–822. doi:10.1111/j.1532-5415.2008.01671.x
Merlani P, Chenaud C, Mariotti N, Ricou B (2007) Long-term outcome of elderly patients requiring intensive care admission for abdominal pathologies: survival and quality of life. Acta Anaesthesiol Scand 51:530–537
Chelluri L, Pinsky MR, Grenvik AN (1992) Outcome of intensive care of the “oldest-old” critically ill patients. Crit Care Med 20:757–761
Sjögren J, Thulin LI (2004) Quality of life in the very elderly after cardiac surgery: a comparison of SF-36 between long-term survivors and an age-matched population. Gerontology 50:407–410
Mahul P, Perrot D, Tempelhoff G, Gaussorgues P, Jospe R, Ducreux JC, Dumont A, Motin J, Auboyer C, Robert D (1991) Short- and long-term prognosis, functional outcome following ICU for elderly. Intensive Care Med 17:7–10
Udekwu P, Gurkin B, Oller D, Lapio L, Bourbina J (2001) Quality of life and functional level in elderly patients surviving surgical intensive care. J Am Coll Surg 193:245–249
Andersen FH, Flaatten H, Klepstad P, Romild U, Kvåle R (2015) Long-term survival and quality of life after intensive care for patients 80 years of age or older. Ann Intensive Care 5:53. doi:10.1186/s13613-015-0053-0
Roch A, Wiramus S, Pauly V, Forel JM, Guervilly C, Gainnier M, Papazian L (2011) Long-term outcome in medical patients aged 80 or over following admission to an intensive care unit. Crit Care 15:R36. doi:10.1186/cc9984
Sacanella E, Pérez-Castejón JM, Nicolás JM, Masanés F, Navarro M, Castro P, López-Soto A (2011) Functional status and quality of life 12 months after discharge from a medical ICU in healthy elderly patients: a prospective observational study. Crit Care 15:R105. doi:10.1186/cc10121
Khouli H, Astua A, Dombrowski W, Ahmad F, Homel P, Shapiro J, Singh J, Nallamothu R, Mahbub H, Eden E, Delfiner J (2011) Changes in health-related quality of life and factors predicting long-term outcomes in older adults admitted to intensive care units. Crit Care Med 39:731–737. doi:10.1097/CCM.0b013e318208edf8
Lieberman D, Nachshon L, Miloslavsky O, Dvorkin V, Shimoni A, Lieberman D (2009) How do older ventilated patients fare? A survival/functional analysis of 641 ventilations. J Crit Care 24:340–346. doi:10.1016/j.jcrc.2009.01.015
Heyland DK, Barwich D, Pichora D, Dodek P, Lamontagne F, You JJ, Tayler C, Porterfield P, Sinuff T, Simon J, ACCEPT (Advance Care Planning Evaluation in Elderly Patients) Study Team; Canadian Researchers at the End of Life Network (CARENET) (2013) Failure to engage hospitalized elderly patients and their families in advance care planning. JAMA Intern Med 173:778–787. doi:10.1001/jamainternmed.2013.180
Garrouste-Orgeas M, Tabah A, Vesin A, Philippart F, Kpodji A, Bruel C, Grégoire C, Max A, Timsit JF, Misset B (2013) The ETHICA study (part II): simulation study of determinants and variability of ICU physician decisions in patients aged 80 or over. Intensive Care Med 39:1574–1583. doi:10.1007/s00134-013-2977-x
Boumendil A, Angus DC, Guitonneau AL, Menn AM, Ginsburg C, Takun K, Davido A, Masmoudi R, Doumenc B, Pateron D, Garrouste-Orgeas M, Somme D, Simon T, Aegerter P, Guidet B, ICE-CUB study group (2012) Variability of intensive care admission decisions for the very elderly. PLoS ONE 7:e34387. doi:10.1371/journal.pone.0034387
Huynh TN, Kleerup EC, Wiley JF, Savitsky TD, Guse D, Garber BJ, Wenger NS (2013) The frequency and cost of treatment perceived to be futile in critical care. JAMA Intern Med 173:1887–1894. doi:10.1001/jamainternmed.2013.10261
Wright AA, Zhang B, Ray A, Mack JW, Trice E, Balboni T, Mitchell SL, Jackson VA, Block SD, Maciejewski PK, Prigerson HG (2008) Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA 300:1665–1673. doi:10.1001/jama.300.14.1665
Goldstein J, Hubbard RE, Moorhouse P, Andrew MK, Mitnitski A, Rockwood K (2015) The validation of a care partner-derived frailty index based upon comprehensive geriatric assessment (CP-FI-CGA) in emergency medical services and geriatric ambulatory care. Age Ageing 44:327–330. doi:10.1093/ageing/afu161
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K (2013) Frailty in elderly people. Lancet 381:752–762. doi:10.1016/S0140-6736(12)62167-9
Evans SJ, Sayers M, Mitnitski A, Rockwood K (2014) The risk of adverse outcomes in hospitalized older patients in relation to a frailty index based on a comprehensive geriatric assessment. Age Ageing 43:127–132. doi:10.1093/ageing/aft156
Ware JE (1996) The SF-36 health survey. In: Spilker B (ed) Quality of life and pharmacoeconomics in clinical trials, 2nd edn. Lippincott-Raven, Philadelphia, pp 337–345
Rogers J, Ridley S, Chrispin P, Scotton H, Lloyd D (1997) Reliability of the next of kin’s estimates of critically ill patient’s quality of life. Anaesthesia 52:1137–1143
Hopman WM, Towheed T, Anastassiades T, Tenenhouse A, Poliquin S, Berger C, Joseph L, Brown JP, Murray TM, Murray TM, Adachi JD, Hanley DA, Papadimitropoulos E, The Canadian Multicentre Osteoporosis Study Research Group (2000) Canadian normative data for the SF-36 health survey. CMAJ 163:265–271
Wyrwich KW, Metz SM, Kroenke K, Tierney WM, Babu AN, Wolinsky FD (2007) Measuring patient and clinician perspectives to evaluate change in health-related quality of life among patients with chronic obstructive pulmonary disease. J Gen Intern Med 22:161–170
Lloyd CB, Nietert PJ, Silvestri GA (2004) Intensive care decision making in the seriously ill and elderly. Crit Care Med 32:649–654
van Buuren S (2007) Multiple imputation of discrete and continuous data by fully conditional specification. Stat Methods Med Res 16:219–242
SAS Institute Inc (2014) SAS/STAT® 13.2 User’s Guide. SAS Institute, Cary
Bagshaw SM, Stelfox HT, McDermid RC, Rolfson DB, Tsuyuki RT, Baig N, Artiuch B, Ibrahim Q, Stollery DE, Rokosh E, Majumdar SR (2014) Association between frailty and short- and long-term outcomes among critically ill patients: a multicentre prospective cohort study. CMAJ 186:E95–E102. doi:10.1503/cmaj.130639
Le Maguet P, Roquilly A, Lasocki S, Asehnoune K, Carise E, Saint Martin M, Mimoz O, Le Gac G, Somme D, Cattenoz C, Feuillet F, Malledant Y, Seguin P (2014) Prevalence and impact of frailty on mortality in elderly ICU patients: a prospective, multicenter, observational study. Intensive Care Med 40:674–682. doi:10.1007/s00134-014-3253-4
Rockwood K, Mitnitski A, Song X, Steen B, Skoog I (2006) Long-term risks of death and institutionalization of elderly people in relation to deficit accumulation at age 70. J Am Geriatr Soc 54:975–979
Taneja S, Rutenberg A, Mitnitski A, Rockwood K (2014) A dynamical network model for frailty-induced mortality. Bull Am Phys Soc 59(1):J11–J17
de Rooij SE, Abu-Hanna A, Levi M, de Jonge E (2007) Identification of high-risk subgroups in very elderly intensive care unit patients. Crit Care 11:R33
Lown DJ, Knott J, Rechnitzer T, MacIsaac C (2013) Predicting short-term and long-term mortality in elderly emergency patients admitted for intensive care. Crit Care Resusc 15:49–55
Turnbull AE, Krall JR, Ruhl AP, Curtis JR, Halpern SD, Lau BM, Needham DM (2014) A scenario-based, randomized trial of patient values and functional prognosis on intensivist intent to discuss withdrawing life support. Crit Care Med 42:1455–1462. doi:10.1097/CCM.0000000000000227
Acknowledgments
Funded by the Canadian Institutes of Health Research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The protocol was endorsed and conducted in collaboration with the Canadian Critical Care Trials Group (www.ccctg.ca) and the Canadian Researchers at the End of Life Network (www.thecarenet.ca). The study was funded by the Canadian Institutes of Health Research which played no role in the design, conduct, analysis, interpretation of results or decision to publish. Dr Heyland and Mr. Day have had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Dr. Cook is a Canada Research Chair of the Canadian Institutes of Health Research. Kenneth Rockwood is supported by the Dalhousie Medical Research Foundation as the Kathryn Allen Weldon Professor of Alzheimer Research. Dr. Turgeon is a Clinician Scientist of the Fonds de Recherche du Québec-Santé (FRQ-S). Dr. Bagshaw holds a Canada Research Chair in Critical Care Nephrology and is supported by a Clinical Investigator Award from Alberta Innovates-Health Solutions (AI-HS). Dr. Fowler is a Clinician Scientist of the Heart and Stroke Foundation (Ontario). Dr Burns holds a CIHR Clinician Scientist Award and a Ministry of Research and Innovation Early Researcher Award. No investigators report financial or other conflicts of interest.
Additional information
On behalf of the Canadian Critical Care Trials Group and the Canadian Researchers at the End of Life Network (CARENET).
Take-home message: One-quarter of patients aged 80 years or older admitted to ICU survived and returned to baseline levels of physical function at one year. Routine assessment of baseline physical function and frailty status could aid in prognostication and informed decision-making for very old critically ill patients.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Heyland, D.K., Garland, A., Bagshaw, S.M. et al. Recovery after critical illness in patients aged 80 years or older: a multi-center prospective observational cohort study. Intensive Care Med 41, 1911–1920 (2015). https://doi.org/10.1007/s00134-015-4028-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-015-4028-2