Abstract
Objective
To describe triage decisions and subsequent outcomes in octogenarians referred to an ICU.
Design and setting
Prospective observational study in the medical ICU in a tertiary nonuniversity hospital.
Participants
Cohort of 180 patients aged 80 years or over who were triaged for admission.
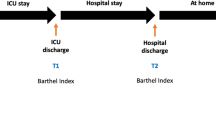
Measurements
Age, underlying diseases, admission diagnoses, Mortality Probability Model score, and mortality were recorded. Self-sufficiency (Katz Index of Activities of Daily Living) and quality of life (modified Perceived Quality of Life scale and Nottingham Health Profile) were measured 1 year after triage.
Results
In 132 patients (73.3%) ICU admission was refused, including 79 (43.8%) considered too sick to benefit. Factors independently associated with refusal were nonsurgical status, age older than 85 years, and full unit. Greater self-sufficiency was associated with ICU admission. Hospital mortality was 30/48 (62.5%), 56/79 (70.8%), 9/51 (17.6%), and 0/2 in the admitted, too sick to benefit, too well to benefit, and family/patient refusal groups, respectively; 1-year mortality was 34/48 (70.8%), 69/79 (87.3%), 24/51 (47%), and 0/2, respectively. Self-sufficiency was unchanged by ICU stay. Quality of life (known in only 28 patients) was significantly poorer for isolation, emotional, and mobility domains compared to the French general population matched on sex and age.
Conclusions
More than two-thirds of patients aged over 80 years referred to our ICU were denied admission. One year later self-sufficiency was not modified and quality of life was poorer than in the general population. These results indicate a need to discuss patient preferences before triage decisions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The demographic revolution that is sweeping across industrialized countries will dramatically increase the absolute number of elderly over the next 40 years. In France the population aged 85 years or more will expand from 1.6 to 6 million between now and 2050, according to data from the Institut National de Statistiques et de la Recherche Medicale (www.http//insee.fr). Therefore the number of elderly patients requiring critical care will grow substantially in the near future. Identifying the patients most likely to benefit from critical care is essential both to prevent suffering related to unnecessary treatments and to ensure optimal use of finite resources. Of the 1,266 patients older than 80 years in the Hospitalized Elderly Longitudinal Project [1], 5.7% died during the enrollment. Among these, 70% reported their baseline quality of life as fair or poor, and most wanted comfort care as opposed to life-prolonging care; nevertheless, 54% were admitted to ICUs. Many older adults were unwilling to trade time with their current quality of life for a shorter life in excellent health, in contradiction to the opinion of surrogates [2]. Because the elderly often have many acute and chronic diseases associated with physical impairments and psychological distress, their perceptions of quality of life may rest on different values from those important to younger individuals [3]. A prospective cohort study found that age was not independently associated with ICU mortality [4], but another study did find age to be associated with long-term mortality, presence of an underlying fatal condition, and severe functional limitation [5]. Three studies found that older age was an independent determinant of ICU refusal [6, 7, 8]. To our knowledge, no studies have focused on ICU triage for patients older than 80 years of age. Few studies [9, 10, 11] have investigated long-term survival, self-sufficiency, and quality of life after ICU admission in octogenarians.
The aim of this study (reported previously as an abstract [12]) was to describe triage to the ICU in patients older than 80 years of age and to determine 1-year survival, self-sufficiency, and quality of life.
Methods
Setting
The study was performed at the Saint Joseph Hospital, a 460-bed tertiary-care nonuniversity hospital for adults, located in Paris, France. The hospital provides services in all the medical specialties and in all the fields of surgery except neurosurgery. The ICU is a ten-bed medical unit that admits about 400 emergency cases per year (mean age, 62 years) including 70% of medical patients. In addition to the ICU, the hospital has 5 coronary beds for medical and postoperative cardiac patients, 15 intermediate beds for postoperative patients, and one room with 7 immediate recovery rooms, managed by non-ICU physicians. There is no geriatric unit.
Triage study
All ICU admission requests between 1 March 2002 and 31 November 2003 were studied. For each request from the emergency unit or general wards of the hospital the triaging intensivist completed a questionnaire used in previous studies [13, 14] to collect the following data: date and time of the ICU triage decision, number of available beds, number and seniority of the ICU physicians involved in the decision (with senior intensivists being defined as having more than 2 years of ICU experience), patient age, and admission diagnosis. Comorbidities were assessed using the McCabe and Jackson [15] score and the Knaus et al. [16] classification system. The McCabe score defines underlying disease likely to cause death within 5 years (ultimately fatal disease), and underlying disease likely to cause death within 1 year (fatal disease). We defined severity of illness at ICU referral using the only model validated for this situation (the Mortality Prediction Model, MPM0) [17]. Self-sufficiency was evaluated using the Katz Index of Activities of Daily Living (ADL) [18] which uses three categories (no help, partial assistance, and complete assistance) for each of five activities (bathing, dressing, toileting, transferring, continence, and feeding). As proposed by Ridley and Wallace [19], we evaluated the need for special equipment to carry out each activity. When the patient was unable to answer questions, we interviewed the relatives to obtain information on self-sufficiency.
The reasons for refusal were categorized as follows: too well to benefit, too sick to benefit, and patient or family refusal. When the ICU was full, patients admitted by the triaging intensivists were transferred to other ICUs; we included these patients in the group of admitted patients. For patients considered too sick to benefit, the triaging physician indicated the main reasons for refusing admission among the following: advanced age, severe underlying disease, dependency, and severity of the acute illness. Preferences of patients or families were collected at triaging.
In the admitted patients we recorded the Simplified Acute Physiology Score (SAPS) II [20] to assess severity of illness at admission. It was computed using the worse physical and laboratory data during the first 24 h in the ICU. ICU stay length and ICU mortality were recorded, as well as the number of withholding and withdrawal decisions according to the recommendations of the Francophone Society for Critical Care (SRLF) [21].
Follow-up measures
To assess 1-year outcomes patients were contacted by telephone. Patients who failed to answer the first call were called again on different days, for a maximum of four calls. When we were unable to contact the patient by phone, we sought vital status information by calling the primary care physician and by looking for a death certificate at the appropriate registry office or, if the patient was not French, at the appropriate consulate. Self-sufficiency (ADL) [18] and quality of life (Perceived Quality of Life (PQoL) [22] scales and the Nottingham Health Profile (NHP) [23]) 1 year after ICU admission were evaluated during a telephone interview conducted by one of the investigators (M.G.O.). The PQoL and NHP scores are provided in Tables E1 and E2 of the Electronic Supplementary Material (ESM). Because quality of life is a subjective personal concept that cannot be readily evaluated by relatives, we interviewed patients only. Patients were interviewed about their current condition and asked to retrospectively evaluate their prehospitalization self-sufficiency regarding activities of daily living. A retrospective evaluation of quality of life was not sought: this would have increased the interview time.
This study was approved by the Institutional Review Board of the Saint Joseph Hospital, which waived the requirement for written informed consent at the time of triage but requested that patients or proxies be told they would receive a phone call 1 year later, and that they be asked for their consent at the time of the call. The study was explained again to the patient during the 1-year phone call, and the patient was then asked for consent to the interview.
Statistical analysis
Univariate analysis was performed using Fisher's exact test or the Mann–Whitney test. Variables associated with the dependent variable at the p ≤ 0.10 level were introduced into a stepwise logistic regression model. The variables entered in the logistic regression are listed in the ESM. Backward elimination was used to select variables for the final model. Differences below the level of p ≤ 0.05 were considered statistically significant. We calculated the Standard Mortality Ratio (SMR) for the admitted patients, which is the ratio of observed hospital mortality over mortality predicted by the SAPS II. Comparisons between self-sufficiency at triage and 1 year later were performed using the Wilcoxon rank sum test. The NHP of the survivors was compared to a random sample of the general French population (5:1) matched on age and sex using two-way analysis of variance by rank. SAS version 8.0 (SAS Institute, Cary, N.C., USA) and Medcalc 5.00 (Medcalc, Ghent, Belgium) were used for the statistical tests.
Results
Factors associated with ICU refusal
During the 20-month study period a request for ICU admission was made for 180 patients older than 80 years (mean age 86 ± 5.09 years, range 80–99). The requests came from the emergency unit in 129 cases (71.6%), medical wards in 59 (32.7%), and surgical wards in 13 (7.2%). Of the 180 patients 48 were admitted (42 to our ICU and 6 to another ICU on the same day). Of the 132 refused patients (73.3%) 51 (28.3%) were considered too well to benefit, 79 (43.8%) too sick to benefit, and for two the family/patient refused. Most patients (n = 129, 71.6%) were not informed of the triage decision, about one-fourth (n = 49, 27.3%) agreed with the decision (directly at the time of triage in 44, via advance directives in 1, and via proxies in 4), and two families refused ICU admission.
In the 79 patients considered too sick to benefit the main reasons given by the ICU triage physician were advanced age (n = 72), presence of an underlying disease (n = 52), dependency before the current hospital admission (n = 52), and severity of the acute illness (n = 53). Parameters associated with ICU refusal are reported in Table 1. In the logistic regression analysis (Table 2) factors independently associated with ICU refusal were medical status, age older than 85 years, and full unit. Greater self-sufficiency was associated with ICU admission.
Mortality
Figure 1 shows the patient flow chart. Crude hospital mortality was 95 of 180 (52.7%). Vital status at hospital discharge was available for all study patients. Hospital mortality was 62.5% (30/48) in the admitted patients, 70.8% (56/79) in those too sick to benefit, and 17.6% (9/51) in those too well to benefit (0/2 in the patients whose families refused ICU admission). The mortality predicted by the MPM0 was, respectively, 22.8 ± 14.5%, 30.9 ± 16.5%, and 22.4 ± 10.5%. ICU mortality was 50% (20/48). SMR using SAPS II was 1.63 among admitted patients. Seventeen patients (70%) died after treatment limitation. The time from ICU admission to treatment limitation was 13.2 ± 20.8 days (median 6).
Eighty-five patients were discharged from the hospital. Of these, 32 (37.6%) died within the 1st year following the ICU triage decision. Mortality after 1 year was 70.8% (34/48) in the admitted patients, (87.3%) 69/79 in those too sick to benefit, and (47.0%) 24/51 in those too well to benefit and 0/2 in the patients whose families refused ICU admission.
Self-sufficiency and quality of life 1 year after the ICU triage decision
Forty-two patients were contacted by phone. Of these, 14 were not interviewed, for the following reasons: dementia (n = 3), aphasia (n = 3), unwillingness to be interviewed (n = 4), and deafness (n = 4). This left 28 patients for whom data on self-sufficiency and quality of life were obtained. The ADL score used to evaluate self-sufficiency was not significantly changed compared to the pretriage score assessed retrospectively by the patients (see Table E3 in the ESM). One year after the triage decision 11 patients lived at home and the remaining 17 in retirement homes (n = 5) or extended-care facilities (n = 12); regarding place of residence only 4 patients reported a change compared to the time of the triage decision.
The PQoL scale showed good levels of satisfaction regarding respect by others (6.78 ± 3.23), memory (6.75 ± 2.41), help from family and friends (6.57 ± 3.51), income (6.57 ± 2.64), and happiness (6.37 ± 2.62). Satisfaction was fair regarding physical health (5.39 ± 3.07), seeing friends (5.96 ± 3.22), and being retired (5.88 ± 3.28). Lower levels of satisfaction were noted regarding leisure (4.14 ± 3.33), contribution to the community (4.89 ± 3.14), and meaning and purpose of life (5.46 ± 3.16). The comparison of the quality of life as assessed by NHP compared to that in the general age- and sex-matched population is provided in Table E5 in the ESM. Our elderly survivors were significantly more depressed, more isolated, and less mobile. Of the 28 patients 16 (57%) said they did not want ICU admission should they experience a life-threatening health problem.
Discussion
The main findings from this single-center study are the very high ICU refusal rate in octogenarians and the high 1-year mortality rates both in admitted patients and in patients considered too sick to benefit from ICU admission. Self-sufficiency in survivors was unchanged compared to the pretriage estimate, and quality of life was poor. About one-half the survivors stated that they did not want further ICU admission.
Several groups have investigated the factors associated with refusal of ICU admission [6, 7, 8, 13, 14]. Patient-related factors and organizational factors were found to be independently related to ICU refusal. Several studies [6, 7, 13, 14] found a strong effect of bed availability; the only exception is a study that failed to evaluate the admission process when the unit was full [8]. Older age was independently associated with refusal [6, 7, 8, 13, 14], particularly in patients with greater disease severity [8, 13]. None of these studies focused on specific age groups. In our study age was related to ICU admission. Age older than 85 years and dependency were associated with refusal of ICU admission. The higher hospital mortality in dependent patients reported in several studies [6, 7, 8, 24] is consonant with the reluctance of ICU physicians in our study to admit strongly dependent patients.
Hospital mortality in admitted patients, those too sick to benefit, and those too well to benefit was 62.5%, 70.8%, and 17.6%, respectively. In admitted patients ICU mortality was 50% higher than in recent studies of similar-age patients conducted in France (26.7% [4], 16.3% [5], and 28% [25]) and in other countries (26% [8], 5.6% [1], and 10% [26]). It was also higher than in another French study with similar severity of illness at admission [5]. The high ICU mortality rate may be due to several factors: the large proportion of medical patients in our cohort, the 50% rate of patients transferred from wards, and the large proportion (70%) of patients with treatment withholding or withdrawing decisions, which have been found to independently predict ICU mortality [27]. The relationship between age and mortality warrants further comment. Although age per se is a major determinant of hospital mortality [28, 29], the most important determinant of ICU mortality is severity of illness, as shown by studies taking this confounding factor into account [4, 5]. However, in a study of about 150,000 ICU patients older than 80 years Rosenthal et al. [30] showed that the odds ratio for death increased at each 5-year interval after adjustment on severity of illness (Acute Physiology and Chronic Health Evaluation III score), gender, comorbidities, admission diagnosis, and place of stay before ICU admission. Although age was reliable for predicting benefits from ICU admission, the reported impact of age on mortality after ICU discharge [4, 5, 30, 31] influenced the triage decisions made by our ICU physicians.
There is general agreement that quality-of-life parameters such as self-sufficiency and psychological well-being are important patient outcomes, particularly in older patients [10]. Measuring these outcomes provides crucial information for determining whether aggressive therapy is warranted. Patients older than 80 years have been reported to receive less aggressive treatment than younger patients with similar disease severity [25]. Quality of life after ICU discharge is a dynamic process that depends on several factors including advanced age, severity of illness at admission, and diagnostic category [31, 32, 33]. Preadmission status and specific events in the ICU [26, 34] are associated with discharge to healthcare facilities. In our study self-sufficiency was not changed by the hospital stay. Most survivors (17/28, 60.7%) were discharged to an extended-care facility. Quality of life in our cohort was poorer than in our previous study of patients older than 70 years [35] and differed significantly in the emotional, isolation, and mobility domains compared to the general population matched on age and sex. One-half the survivors said that they did not want further ICU admission. This finding contrasts with that of previous studies [9, 35]. This discrepancy indicates that older patients must think about their wishes should they experience a life-threatening condition, and that they must communicate those wishes to their relatives or physicians.
This study has several limitations. First, because it was conducted in a single medical ICU, the results may not apply to all populations of octogenarians for whom ICU admission is requested. The large proportion of referred medical patients may have introduced a bias in the triage process. Second, we did not measure quality of life at the time of triage, and consequently we were unable to determine whether the poor quality of life after 1 year indicated deterioration after the hospital stay or merely reflected the baseline status. The time constraints that surround ICU admissions and the limited reliability of surrogates in this area are major obstacles to quality-of-life evaluation at the time of triage to the ICU. Third, 11 patients could not be contacted for the 1-year evaluation. We were unable to obtain outcome data from their physicians or families. Thus quality of life was reported in only 28 patients.
In conclusion, decisions to admit patients older than 80 years to our ICU were influenced only by preadmission patient-related factors and by bed availability. More than two-thirds of ICU admission requests for patients older than 80 years were denied. Among the few survivors in this age group 1-year survival was low, and quality of life was poor. These results invite physicians in all fields of clinical care to discuss preferences about ICU admission with their elderly patients.
References
Somogyi-Zalud E, Zhong Z, Hamel MB, Lynn J (2002) The use of life-sustaining treatments in hospitalized persons aged 80 and older. J Am Geriatr Soc 50:930–934
Tsevat J, Dawson NV, Wu AW, Lynn J, Soukup JR, Cook F, Vidaillet H, Phillips RS for the HELP investigators (1998) Health values of hospitalized patients 80 years or older. JAMA 279:371–375
Nilsson M, Eckman S, Ericsson K, Winblad B (1996) Some characteristics of the quality of life in old age illustrated by mean's of Allardt's concept. Scand J Caring Sci 116–121
Somme D, Maillet JM, Gisselbrecht M, Novara A, Ract C, Fagon JY (2003) Critically ill old and the oldest-old patients in intensive care: short and long term outcomes. Intensive Care Med 29:2137–2143
Boumendil A, Maury E, Reinhard I, Luquet L, Offenstadt G, Guidet B (2004) Prognosis of patients aged 80 years and over admitted in medical intensive care unit. Intensive Care Med 30:647–654
Azoulay E, Pochard F, Chevret S, Vinsonneau C, Garrouste-Orgeas M, Cohen Y, Thuong M, Paugam C, Appere C, De Cagny B, Brun F, Borstein C, Parrot A, Tamion F, Lacherade JC, Bouffard Y, Le Gall JR, Herve C, Grassin M, Zittoun R, Schlemmer B, Dhainaut JF (2001) Compliance with triage to intensive care recommendations. Crit Care Med 29:2132–2139
Sprung CL, Geber D, Eidelman LA, Baras M, Pizov R, Nimrod A (1999) Evaluation of triage decisions for intensive care admission. Crit Care Med 27:1073–1079
Joynt GM, Gomersall CD, Tan P, Lee A, Ai YU Chen C, Lai Yi Wong E (2001) Prospective evaluation of patients refused admission to intensive care unit: triage, futility and outcome. Intensive Care Med 27:1459–1465
Chelluri L, Pinski MR, Grenvik A (1992) Outcome of intensive care of the oldest-old critically ill patients. Crit Care Med 20:757–761
Covinski KE, Wu AW, Landefeld S, Connors AF, Phillips RS, Tsevat J, Dawson NV, Lynn J, Fortinsky RH (1999) Health status versus quality of life in older patients: does the distinction matter? Am J Med 106:435–440
Kass JE, Castriotta BJ, Malakoff F (1992) Intensive care unit outcome in the very elderly. Crit Care Med 20:1666–1671
Garrouste-Orgeas M, Timsit JF, Montuclard L, Gattolliat O, Philippart F, Rigal G, Misset B, Carlet J (2004) Preliminary study of ICU admission procedures in patients over 80 years and one-year outcome, functional capacity and quality of life. Intensive Care Med 30:S101
Garrouste-Orgeas M, Montuclard L, Timsit JF, Misset B, Christias M, Carlet J (2003) Triaging patients to the ICU: a pilot study of factors influencing admission decision and outcome. Intensive Care Med 29:774–781
Garrouste-Orgeas M, Montuclard L, Reignier J, Desmettre T, Karoubi P, Moreau D, Montesino L, Duguet A, Boussat S, Ede C, Monseau Y, Paule T, Misset B, Carlet J (2005) Predictors of ICU refusal in French ICUs. Crit Care Med 33:750–755
McCabe WR, Jackson GG (1962) Gram negative bacteremia: etiology and ecology. Arch Intern Med 110:847–855
Knaus WA, Zimmerman JE, Wagner DP, Draper EA, Lawrence DE (1981) APACHE acute physiology and chronic health evaluation: a physiologically based classification system. Crit Care Med 9:591–597
Lemeshow S, Teres D, Klar J, Avrunin JS, Gehlbach SH, Rapoport J (1993) Mortality Probability Models (MPM II) based on an interpretation cohort of intensive care unit patients. JAMA 270:2478–2486
Katz S (1983) Assessing self maintenance: activities of daily living, mobility and instrumental activities of daily living. J Am Geriatr Soc 31:721–727
Ridley SA, Wallace PGM (1990) Quality of life after intensive care. Anesthesia 45:808–813
Le Gall JR, Lemeshow S, Saulnier F (1993) A new Simplified Acute Physiology Score (SAPS II) based on a European/North American Multicenter study. JAMA 270:2957–2963
Thompson BT, Cox PN, Antonelli M, Carlet J, Cassel J, Hill NS, Hinds CJ, Pimentel JM, Reinhart K, Thijs LG (2004) Challenges in end-of-life care in the ICU: statement of the 5th International Consensus Conference in Critical Care: Brussels, Belgium, April 2003: executive summary. American Thoracic Society, European Respiratory Society; European Society of Intensive Care Medicine, Society of Critical Care Medicine, Societé de Réanimation de Langue Française Crit Care Med 32:1781–1784
Patrick DL, Danis M, Southerland LI, Hong G (1988) Quality of life after intensive care. J Gen Intern Med 3:218–223
Bucquet D, Condon S, Ritchie K (1990) The French version of the Nottingham Health Profile: a comparison of items weights with those of the source version. Soc Sci Med 30:829–837
Davis RB, Iezzoni Li, Phillips RS, Reiley P, Coffman GA, Safran C (1995) Predicting in-hospital mortality. The importance of functional status information. Med Care 33:906–921
Boumendil A, Aegerter P, Guidet B. Cub-Rea Network (2005) Treatment intensity and outcome of patients aged 80 and older in intensive care units: a matched-cohort study. J Am Geriatr Soc 53:88–93
Rady MY, Johnson DJ (2004) Hospital discharge to care facility. A patient-centered outcome for the evaluation of intensive care for octogenarians. Chest 126:1583–1591
Azoulay E, Pochard F, Garrouste-Orgeas M, Moreau D, Montesino L, Adrie C, De Lassence A, Cohen Y, Timsit JF for the Outcomerea group (2003) Decisions to forgo life-sustaining therapy in ICU patients independently predicts hospital death. Intensive Care Med 29:1895–1901
Cohen L, Lambrinos J (1995) Investigating the impact of age of mechanical ventilation using a population of 41848 patients from a statewide database. Chest 107:1673–1680
Mayer-Oakes S, Oye R, Leake B (1991) Predictors of mortality in older patients following medical intensive care. J Am Geriatr Soc 39:862–868
Rosenthal GE, Kaboli PJ, Barnett MJ, Sirio CA (2002) Age and risk of in-hospital death: insights from a multihospital study of intensive care patients. J Am Geriatr Soc 50:1205–1212
Wright JC, Plenderleith L, Ridley SA (2003) Long term survival following intensive care: subgroup analysis and comparison with the general population. Anaesthesia 58:637–642
Niskanen M, Ruokonen E, Takala J, Rissanen P, Kari A (1999) Quality of care after prolonged intensive care. Crit Care Med 27:1132–1138
Graf J, Koch M, Dujardin R, Kersten A, Janssens U (2003) Health-related quality of life before, 1 month after, and 9 months after intensive care in medical cardiovascular and pulmonary patients. Crit Care Med 31:2163–2169
Nierman DM, Schechter CB, Cannon LM, Meier DE (2001) Outcome prediction model for very elderly critically ill patients. Crit Care Med 29:1853–1859
Montuclard L, Garrouste-Orgeas M, Timsit JF, Misset B, De Jonghe B, Carlet J (2000) Outcome, functional autonomy, and quality of life of elderly patients with a long term intensive care unit stay. Crit Care Med 28:3389–3395
Acknowledgements
We thank A. Wolfe, MD, for helping to prepare this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is discussed in the editorial available at: http://dx.doi.org/10.1007/s00134-006-0172-z
Electronic Supplementary Material
Rights and permissions
About this article
Cite this article
Garrouste-Orgeas, M., Timsit, JF., Montuclard, L. et al. Decision-making process, outcome, and 1-year quality of life of octogenarians referred for intensive care unit admission. Intensive Care Med 32, 1045–1051 (2006). https://doi.org/10.1007/s00134-006-0169-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-006-0169-7