Abstract
Purpose
When housing is insufficient, or poor quality, or unaffordable there are well established health effects. Despite the pervasiveness of housing affordability problems (widely referred to as Housing Affordability Stress—HAS), little quantitative work has analysed long-term mental health effects. We examine the mental health effects of (prolonged and intermittent) patterns of exposure to housing affordability problems.
Methods
We analysed a large, nationally representative longitudinal population sample of individuals, following them over five-year periods to assess the relative mental health effects of different patterns of exposure to housing affordability problems. To maximise the number of observations and the robustness of findings, we used 15 years (2002–2016) of data, across three pooled exposure windows. Longitudinal regression analysis with Mundlak adjustment was used to estimate the association between prolonged (constant over a 5-year period) and intermittent exposure to HAS, and mental health (as measured using the SF-36 MCS).
Results
We found that, on average, both prolonged and intermittent exposure were associated with lower mental health (Beta = − 1.338 (95% CI − 2.178–0.488) and Beta = − 0.516 (95% CI − 0.868–0.164), respectively). When we additionally adjusted for baseline mental health, thereby accounting for initial mental health status, coefficients were attenuated but remained significant.
Conclusions
Both prolonged and intermittent exposure to HAS negatively impact mental health, irrespective of baseline mental health. Interventions that target affordable housing would benefit population mental health. Mental health interventions should be designed with people’s housing context in mind.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Housing affordability has emerged as an increasingly pressing social and policy issue across almost all post-Industrial nations [1, 2]. Housing affordability affects people in real and measureable ways. Insecure, unsuitable and/or poor condition housing have well-established negative health consequences [3,4,5], and there is evidence that housing affordability problems negatively influence health, especially mental health [6]. For most people, housing is their largest lifetime—and ongoing—expenditure. At a day-to-day level, high housing costs (either rent or mortgage payments) are a major influence on the amount of household budget available for food, transport, education, other life necessities and good health [7, 8]. Excessive housing costs also have a major impact on where people can afford to live, and the quality, appropriateness, and tenure of their dwelling [9,10,11,12].
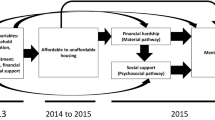
The influence of poor housing affordability on individuals and households is now well documented, across and beyond health [10, 13,14,15]. Increasingly, work within the field focusses on describing the likely causal pathways and mechanisms. In this vein, housing affordability has been shown to affect mental health, both via income, and independent of it [16], and interactions have been shown with tenure [6, 17] and employment [18]. Further, the health effects of poor affordability have been shown to accumulate [13]. As with similar research on housing affordability [19, 20], all these analyses have been based upon perhaps the most widely used measure of unaffordable housing, the 30/40 measure of housing affordability stress (HAS) [21, 22]. With this ratio measure, individuals who are paying more than 30% of their gross household income on housing, and are in the lowest 40% of the national income distribution are identified as being in HAS. Though the limitations of using a simple ratio measure are well acknowledged [23], the HAS measure consistently appears in research and policy because it is relatively easy to construct, allows comparison across jurisdictions, and can be based on nationally collected, robust population-wide data, for example [21, 24]. Importantly, the 30/40 measure assesses housing affordability at a specific point in time. Although point-in-time measurement provides methodological and conceptual convenience, it is increasingly recognised [25,26,27] that they poorly capture the ongoing (over time) experience of affordability problems in people’s lives. Previous investigation of the longitudinal measurement of housing affordability [25] showed that when affordability problems were measured over time (e.g. 5 years), rather than at a single point in time, a different (and potentially more accurate) classification of people with housing affordability problems was revealed.
Possibly as a result of our increasing ability to longitudinally measure and analyse the effects of accumulated exposure to mental health stressors, there has been substantial recent interest in refining conceptual understanding of cumulative effects, for example across housing affordability stress [13], financial strain [28], poor quality housing [29] or poverty [30]. If we conceptualise housing affordability as something experienced over time, rather than more simply classified at a single point in time, we can contemplate additional hypotheses. Namely, that the mental health effects of housing affordability problems may accumulate (as in a dose-response model), and/or that different patterns of exposure may have different effects. Using causally focussed methods and a large nationally representative dataset, the recent study by Bentley et al. [13] examined the possibility of a simple dose-response accumulation of mental health effect of unaffordable housing over a five-year period. This study found no evidence of a dose effect. Subsequently, another longitudinal paper [25] examined patterns of exposure and distinguished between the characteristics and potential socioeconomic vulnerabilities of people who ‘slipped’ in and out of housing affordability problems, and people who were ‘stuck’ in unaffordable housing for extended periods. While not measuring health effects, the authors suggested that the pattern of exposure may be more important than the overall ‘dose’, and that people who slipped in and out of affordability problems intermittently would be much less affected than those who were stuck for prolonged periods. Hence, it may not be the dose of exposure per se, but the pattern of exposure which may make people vulnerable to negative mental health effects of time spent with housing affordability problems. Therefore, we investigated mental health effects of three patterns of exposure to unaffordable housing—Prolonged, Intermittent, and Unexposed.
Patterns of exposure
Within a whole population at any one point in time, there will be one group classified as having unaffordable housing, but if we conceptualise housing affordability problems as experienced over time instead of cross-sectionally, three key exposure groups can be identified. A cohort of people experiencing ongoing unaffordable housing (Prolonged) is distinct from a cohort who ‘churn’ in and out for shorter periods (Intermittent), and both are distinct from the cohort who has no exposure to housing affordability problems (Unexposed).
Seelig, O’Flaherty, Short et al. [31] highlighted a significant and largely unrecognised problem with traditional point-in-time approaches. At a point in time, people with intermittent housing affordability problems are indistinguishable from people with persistent ones. Earlier analysis in a large Australian sample [25] showed that the majority of people classified as being in unaffordable housing were only intermittently exposed over the five-year study period. This study highlighted a smaller minority of greater concern, comprising people who experienced prolonged exposure to unaffordable housing costs continuously over five years. This group was shown to be older, more likely to be women, to live alone, have disabilities and illnesses, as well as lower incomes, and lower educational attainment than those with intermittent exposure. The authors hypothesised that, independent of the socio-demographic differences between the groups, any effects on health and wellbeing of unaffordable housing were likely to be more pronounced among the cohort experiencing prolonged exposure than among the intermittently exposed group. This work strongly justified further research to examine the longitudinal rather than the point-in-time effects of housing affordability.
Therefore, the health outcomes of people with prolonged and intermittent housing affordability problems were compared to those with no exposure to housing affordability problems, to test the following two research questions:
- 1.
Compared to people with no exposure to HAS, do those who experience either continuous or intermittent housing affordability problems have worse mental health?
- 2.
How much of the association between pattern of exposure and mental health is explained by people’s pre-existing mental health status?
Methods
Data
Data from the Household, Income and Labour Dynamics in Australia (HILDA) survey were analysed using Stata/SE 16.0. Commencing in 2000/1, HILDA is the largest available annual panel survey of Australian households and individuals. It was based upon a nation-wide probability sample, collecting information about income, employment, health and wellbeing, and other individual attributes from a representative sample of Australian householders using face-to-face interviews and self-completion questionnaires [32].
This analysis focused on adult participants (aged 15 years or older at 2002) in Australian cities and towns reporting values for the variables of interest, who took part in the survey for five consecutive waves (during the period 2002–2016 inclusive). The maximum samples were 1008 observations for those subject to prolonged exposure to HAS and 2966 observations for those with intermittent exposure to HAS (compared with 44,472 not exposed to HAS). The sample size for the Intermittent and Prolonged models differ due to the patterns of missing data in both the dependent and independent variables (e.g. see Table 1). There was only a small amount of missing data for each exposure group (Unexposed = 2.26%; Intermittent = 2.16%; Prolonged = 0.89%). Given that the amount of missing data were negligible, complete case analysis was used.
Exposure variable
The exposure variable in each model described the pattern of exposure to unaffordable housing over time. Housing costs were measured as the amount spent on rent or mortgage repayments. Individuals were classified as being in unaffordable housing if their rent or mortgage exceeded 30% of their household income, and their income was in the bottom 40% of the distribution (lower income households). Income was defined as gross household income (from wages, salaries and government payments), equivalised to account for the number and age of individuals living in the household. In keeping with the 30/40 definition of housing affordability (described above), households were categorised as being in either the lower 40% or upper 60% of the national income distribution. This categorisation was performed separately for each year.
To explore the pattern of exposure to unaffordable housing over time we examined individual’s patterns of exposure within five-year windows (2002–2006; 2007–2011; 2012–2016). Within each window ‘Prolonged’ unaffordability was defined as lower-income individuals whose housing costs exceeded 30% of their household income in each of the 5 years. Individuals who made at least one transition into unaffordable housing, and at least one transition out of unaffordable housing in a five-year window were defined as the ‘Intermittent’ unaffordability cohort. As previously noted this ‘slippage’ in and out of housing affordability may occur due to changed position in the national household income distribution (above and below the 40th percentile) or a change in the proportion of income spent on housing costs above or below the 30% cut-off. Individuals who were not classified as being in unaffordable housing in any of the five years formed the ‘Unexposed’ comparison. The classification (described in more detail [25]) aimed to derive three groups of interest within the whole population. Though the majority of the population were described by these three categories, they were not exhaustive—in the eligible sample, 6% of the total population had alternative patterns of affordability, such as people who entered affordability problems once, during the five-year study period, and remained there.
Outcome variables
The outcome variable was mental health, defined using the self-assessed health measures contained in the Short Form 36 (SF-36) assessment tool. The SF-36 is a widely used self-completion measure of health status [33] and has been validated for use in the Australian population [34]. The SF-36 provides a Mental health Component Summary score (MCS), which is standardised between 1 and 100 (with a mean of 50 and a standard deviation of 10). The MCS relates most directly to four subscales of the SF-36: vitality, social functioning, role limitations due to emotional problems (“role emotional”), and mental health. A higher score represents better mental health. Its psychometric properties (including internal consistency, discriminatory accuracy, test–retest reliability) are well established [35].
Analyses
We used regression to estimate the relative influence of housing affordability exposure pattern on mental health. We estimated models with and without baseline adjustment for mental health to assess how much people’s initial mental health status explained variation in their subsequent mental health (after exposure to prolonged or intermittent HAS). Because the exposure for the three cohorts was, by definition, time-invariant, we used a Mundlak regression model, a hybrid approach that has been shown to effectively capture both within and between-person differences [36]. The longitudinal regression with Mundlak adjustment and baseline (Initial condition/state dependence) is represented as:
where Y is the outcome (MCS), X is the set of (k) explanatory variables, α is the common intercept, β is the vector of coefficients to be estimated, \(\overset{\lower0.5em\hbox{$\smash{\scriptscriptstyle\leftrightarrow}$}} {Y}\) represents the initial condition/state dependence controls, \(\overline{Z}\) represents the Mundlak means, ui represents the individual specific effects that vary across individuals but are constant over time and v is the usual unobserved zero-mean constant variance, uncorrelated, random disturbance (representing the net effect of all other unobserved factors that may influence the outcome); i are individuals (i = 1,…,N), and t is time (or survey waves, t = 1,…,T).
The influence of potential confounders (including age, sex, income, number of adults in household, number of children in the household, years of unemployment, education, marital status, self-reported health, long-term disability) are accounted for. The produced coefficient indicates whether or not there was a mean change in the outcome variable between individuals in the exposed (Prolonged or Intermittent) and Unexposed cohorts, at the end of each five-year window, as expected. The Mundlak adjustment enabled a relaxation of the assumption that the individual-specific observed and unobserved variables were uncorrelated, providing more robust findings (leading to unbiased and consistent model estimates).
Results
Descriptive
Just over 8% of the pooled analytical sample were exposed to housing affordability stress, most being intermittently exposed; and just 2% were classified as having prolonged exposure. Note the lower average mental health scores for the Prolonged exposure cohort, indicating poorer mental health; and the highest average scores for the Unexposed group, indicating better mental health summarised by descriptive population characteristics in Table 1. The table highlights noticeably lower average mental health scores for the Prolonged exposure cohort. The Unexposed group have the highest average scores (mean for Prolonged = 45.0 compared to Unexposed = 49.4; p < 0.001). When different population characteristics were considered, there appeared to be a general worsening of mean mental health with additional exposure to unaffordable housing. A predictable gradient towards higher mean mental health with age held for the cohorts exposed to housing affordability problems, however, their scores were lower. Unsurprisingly, people with a disability or health condition had lower average mental health, but importantly, mean mental health was much lower for people with exposure to housing affordability stress. This pattern was replicated for labour force, household and education characteristics; note that private renters with prolonged exposure to housing affordability stress had very low (40.4) mean MCS scores. This is especially salient when previous studies have indicated that an MCS score of 42 or below may be of clinical importance in diagnosing depression [37, 38].
Analytical results
Results of the regression analyses (summarised in Table 2) showed a significant association with mental health for both the Prolonged (Beta − 1.338, LCI − 2.187 UCI − 0.488) and Intermittent (Beta − 0.515, LCI − 0.868 UCI − 0.164) exposure groups. The mental health of people experiencing prolonged exposure to housing affordability stress was 1.5 points lower, on average, compared to the group without experience of HAS. People who experienced intermittent exposure to HAS over the five-year window also had lower mental health on average, however, the coefficient was considerably smaller. After adjusting for baseline mental health, the coefficients were slightly reduced, suggesting that respondents’ baseline mental health may have explained some of the observed association.
Discussion
In this study, we sought to investigate whether, over time, different patterns of exposure to unaffordable housing would affect mental health. Results of the simple descriptive analysis (Table 1), suggested substantial socio-demographic and mental health differences between the three examined cohorts–the populations were distinct. Of particular interest, low average mental health scores within many sub-populations that comprised the Prolonged exposure cohort. The average mental health score for many of the sub-populations within the Prolonged exposure cohort was close to, or below 42. This means that many individuals who experience prolonged affordability problems are also close to, or already below the point at which depression may be diagnosed. For example, people with a disability and private renters on average have MCS scores of 41.7 and 40.4, respectively, making people within these groups especially vulnerable to any additional negative influences on their mental health. The analytical results further justify a deeper examination of this condition.
The analytical results showed that, even after controlling for a broad range of socio-demographic characteristics (described in Table 1), there was a statistically significant mental health effect of time spent in unaffordable housing. Our results suggest that the largest effect may be experienced by the Prolonged exposure group, a small cohort who our descriptive analysis characterises as having both low existing mental health, and additional vulnerability to many of the social determinants of poor mental health.
This has important consequences for policy and highlights the need to understand the factors that lead people into prolonged affordability problems. People’s initial mental health may also be a driver of these effects, with recent work, utilising a quantile regression approach [39], suggesting that good mental health is protective when people’s housing becomes unaffordable. This has implications for the design of mental health interventions suggesting that the provision of affordable housing could be a valuable component of public health prevention strategies that address the social environment.
There are limitations to our analysis. First, we focussed on the most commonly applied measure of housing affordability stress, the 30/40 approach. Although this may be the most commonly used measure, alternative definitions of housing affordability stress may yield different results. A valuable feature, as well as a potential limitation of this measure is that it acknowledges both housing costs and the ability to afford them (income level). As previous work has discussed [16], high income households may choose (and are often rewarded in the tax system) to spend more than 30 per cent of their income on housing costs, and have no negative health effects. Therefore, health effects and the inability to afford essentials post housing expenditure, tend to be concentrated in the lower income groups. This does present a difficulty, however, as both housing and (low) income may be driving the mental health effects we measure. To mitigate this as much as possible we have adjusted all models for income. Second, though a large nationally representative longitudinal dataset was utilised, and our overall observation sample is in excess of n = 54,000, the requirements of defining a five-year pattern of continuous or intermittent exposure limits the size of our exposure groups. Further, because individuals were only included in the analytical sample if they provided data in five consecutive waves of the survey, even though attrition in this dataset was low (for example just 3.8% in wave 9 [40]), our sample may underrepresent some less stable population groups. Additionally, exposure to HAS can potentially occur across a person’s lifetime. In the absence of lifetime data, five-year windows were chosen as the experimental exposure period, and the analysis, therefore, cannot reflect lifetime exposure patterns. Relatedly, this analysis has provided additional insight into the mental health effect of pattern of exposure, rather than point in time exposure. We note that future work might also apply this ‘longitudinal’ approach to the outcome variable, to better understand the role of mental health variations over time in shaping our findings. Although we measure change in mental health over the study period and adjust for baseline mental health, we cannot entirely exclude the possibility that some of the magnitude of estimated effect is due to reverse causation. It is plausible that people already on a trajectory of declining mental health (irrespective of their absolute level of mental health at baseline) may be more likely to fall into housing stress during the study period (and, therefore, potentially enter the Intermittent exposure category). We have quantified and measured people’s experiences of unaffordable housing from survey data. Substantial insight would come from in-depth qualitative interviews with people who have had long periods of exposure to unaffordable housing. Such qualitative work might also facilitate progress towards better understanding of the indirect pathways and social conditions through which housing affordability influences mental health outcomes. This, and any subsequent qualitative work could be complemented by the analysis of housing, income and mental health data collected directly from local councils, national taxation records and data linkage to health service records, enabling a wider catchment and deeper longitudinal description.
Conclusion
Our findings suggest the population exposed to housing affordability problems fares worse in terms of their mental health and wellbeing than their counterparts who are free of HAS over a 5-year window. While baseline mental health explains some of this association, it fails to explain all of it, suggesting a possible causal pathway that warrants further investigation. The population with prolonged experience of living in unaffordable housing is relatively small, identifiable, and a somewhat homogeneous group, who are also likely to occupy ‘niches’ [41] of other disadvantage. Assistance and intervention geared towards improving mental health and wellbeing might be very effectively targeted to this small cohort.
References
Desmond M (2018) Heavy is the house: rent burden among the American urban poor. Int J Urban Reg Res 42(1):160–170
Wetzstein S (2017) The global urban housing affordability crisis. Urban Stud 54(14):3159–3177
Snow J (1855) On the mode of communication of cholera: John Churchill.
Taylor MP, Pevalin DJ, Todd J (2007) The psychological costs of unsustainable housing commitments. Psychol Med 37:1027–1036
Free S, Howden-Chapman P, Pierse N, Viggers H (2010) More effective home heating reduces school absences for children with asthma. J Epidemiol Community Health 64:379–386
Mason KE, Baker E, Blakely T, Bentley RJ (2013) Housing affordability and mental health: does the relationship differ for renters and home purchasers? Soc Sci Med 94:91–97
Pollack CE, Griffin BA, Lynch J (2010) Housing affordability and health among homeowners and renters. Am J Prev Med 39:515–521
Waldron R, Redmond D (2017) “We’re just existing, not living!” Mortgage stress and the concealed costs of coping with crisis. Hous Stud 32:584–612
Baker E, Bentley R, Lester L, Beer A (2016) Housing affordability and residential mobility as drivers of locational inequality. Appl Geogr 72:65–75
Meltzer R, Schwartz A (2016) Housing affordability and health: evidence From New York city. Hous Policy Deb 26:80–104
Boymal J, de Silva A, Pomeroy J (2013) Quantity and quality estimates of changes in dwelling affordability in metropolitan Melbourne. Aust J Reg Stud 19:4
Cai W, Lu X (2015) Housing affordability: beyond the income and price terms, using China as a case study. Habit Int 47:169–175
Bentley R, Baker E, Mason K (2012) Measuring the dose-dependent mental health effect of poor housing affordability for men and women. J Epidemiol Community Health 66:761–766
Clair A, Loopstra R, Reeves A, McKee M, Dorling D, Stuckler D (2016) The impact of housing payment problems on health status during economic recession: A comparative analysis of longitudinal EU SILC data of 27 European states, 2008–2010. SSM-Popul Health 2:306–316
Bentley RJ, Pevalin D, Baker E, Mason K, Reeves A, Beer A (2016) Housing affordability, tenure and mental health in Australia and the United Kingdom: a comparative panel analysis. Hous Stud 31:208–222
Bentley R, Baker E, Mason K, Subramanian S, Kavanagh AM (2011) Association between housing affordability and mental health: a longitudinal analysis of a nationally representative household survey in Australia. Am J Epidemiol 174:753–760
Baker E, Mason K, Bentley R, Mallett S (2014) Exploring the bi-directional relationship between health and housing in Australia. Urban Policy Res 32(1):71–84
Bentley R, Baker E, Aitken Z (2019) The ‘double precarity’of employment insecurity and unaffordable housing and its impact on mental health. Soc Sci Med 225:9–16
Yates J, Gabriel M. Housing Affordability in Australia; National Research Venture 3: Housing Affordability for Lower Income Australians, Research Paper 3. AHURI Melbourne 2006.
Yates J, Milligan V, Berry M, et al. Housing affordability: a 21st century problem. National research venture 2007; 3.
Nepal B, Tanton R, Harding A (2010) Measuring housing stress: how much do definitions matter? Urban Policy Res 28:211–224
Daniel, L., Baker, E. and Lester, L., 2018. Measuring Housing Affordability Stress: Can Deprivation Capture Risk Made Real?. Urban Policy and Research, pp.1–16.
Rowley S, Ong R, Haffner M (2015) Bridging the gap between housing stress and financial stress: the case of Australia. Hous Stud 30:473–490
Commonwealth of Australia (1991) The affordability of Australian housing. National Housing Strategy, Issues papers 2.
Baker E, Mason K, Bentley R (2015) Measuring housing affordability: a longitudinal approach. Urban Policy Res 33:275–290
Seelig T, Phibbs P (2006) Beyond the normative: low income private renters’ perspectives of housing affordability and need for housing assistance. Urban Policy Res 24:53–66
Borrowman L, Kazakevitch G, Frost L. How long do households remain in housing affordability stress? Housing Studies 2017: 1–18.
Kahn JR, Pearlin LI (2006) Financial strain over the life course and health among older adults. J Health Soc Behav 47(1):17–31
Pevalin DJ, Reeves A, Baker E, Bentley R (2017) The impact of persistent poor housing conditions on mental health: a longitudinal population-based study. Prev Med 105:304–310
Evans GW, Cassells RC (2014) Childhood poverty, cumulative risk exposure, and mental health in emerging adults. Clin Psychol Sci 2(3):287–296
Seelig HJ, O'Flaherty M, Short P, Haynes MA, Baum SW, Western MC, Jones A (2005) Housing consumption patterns and earnings behaviour of income support recipients over time. Australian Housing and Urban Research Institute (AHURI), Melbourne
Summerfield M, Freidin S, Hahn M et al (2011) HILDA user manual–release 10. University of Melbourne Melbourne Institute of Applied Economic and Social Research, Melbourne
Coons SJ, Rao S, Keininger DL, Hays RD (2000) A comparative review of generic quality-of-life instruments. Pharmacoeconomics 17:13–35
McCallum J (1995) The SF-36 in an Australian sample: validating a new, generic health status measure. Aust N Z J Public Health 19:160–166
Pirkis J, Burgess P, Kirk P, Dodson S, Coombs T (2005) Review of standardised measures used in the National Outcomes and Casemix Collection (NOCC). Sydney, NSW
Allison PD (2009) Fixed effects regression models. SAGE publications, Thousand Oaks
Ware JE, Gandek B (1998) Overview of the SF-36 health survey and the international quality of life assessment (IQOLA) project. J Clin Epidemiol 51:903–912
Ware JE, Keller SD, Kosinski M (1994) SF-36: Physical and mental health summary scales: a user’s manual: Health Assessment Lab.
Baker E, Pham NTA, Daniel L, Bentley R (2020) New evidence on mental health and housing affordability in cities: a quantile regression approach. Cities 96:102455
Watson N, Wooden M (2010) Data survey: the HILDA survey: progress and future developments. Australian Econ Rev 43(3):326–336
Baker E, Lester L (2017) Multiple housing problems: a view through the housing niche lens. Cities 62:146–151
Acknowledgements
This paper uses unit record data from the Household, Income and Labour Dynamics in Australia (HILDA) Survey. The HILDA Project was initiated and is funded by the Australian Government Department of Social Services (DSS) and is managed by the Melbourne Institute of Applied Economic and Social Research (Melbourne Institute). The findings and views reported in this paper, however, are those of the author and should not be attributed to either DSS or the Melbourne Institute
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Baker, E., Lester, L., Mason, K. et al. Mental health and prolonged exposure to unaffordable housing: a longitudinal analysis. Soc Psychiatry Psychiatr Epidemiol 55, 715–721 (2020). https://doi.org/10.1007/s00127-020-01849-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-020-01849-1