Abstract
Purpose
Unaffordable housing has a negative impact on mental health; however, little is known about the causal pathways through which it transmits this effect. We examine the role of financial hardship and social support as mediators of this relationship.
Methods
We identified households where housing costs changed from affordable to unaffordable across two waves of the Household, Income and Labour Dynamics in Australia (HILDA) Survey (2014–2015). The sequential causal mediation analysis was used to decompose the total effect of unaffordable housing on mental health into the portion attributable to financial hardship and social support [natural indirect effect (NIE)] and the portion not occurring through measured pathways [natural direct effect (NDE)]. Mental health was measured using the Mental Health Inventory (MHI) and Kessler psychological distress (KPD) scale. Baseline covariates included age, sex, household income, financial hardship, social support, marital status and employment status. Bootstrapping with 1000 replications was used to calculate 95% confidence intervals (CIs). Multiple imputations using chained equations were applied to account for missing data.
Results
Unaffordable housing led to a change in mean mental health score on the MHI scale (− 1.3, 95% CI: − 2.1, − 0.6) and KPDS scale (0.9, 95% CI: 0.4, 1.4). Financial hardship accounted for 54% of the total effect on MHI scale and 53% on KPD scale. Collectively, financial hardship and social support explained 68% of the total effect on MHI scale and 67% on KPD scale, respectively.
Conclusions
In conclusion, the negative mental health effect of unaffordable housing is largely mediated through increased financial hardship.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Housing is a key social determinant of mental health [1, 2]. Access to affordable and adequate housing is critical for mental and physical health as individuals spend a substantial amount of time in housing during their lives [1,2,3,4,5]. Associations between poor physical characteristics of housing and poor outcomes of physical health are well established [4, 6,7,8]. In high-income countries where the quality of housing stock is relatively high, physical characteristics of housing may be less important for health than economic aspects of housing such as housing affordability [9].
However, only in the last decade has evidence of the complex relationship between financial characteristics related to housing and mental health emerged [4, 10,11,12,13,14,15,16].
Affordable housing refers to housing costs, when considered in relation to income, that allows people at low and moderate incomes to meet other essential basic costs [17]. A systematic review found foreclosures and unaffordable housing to be associated with psychological health [18]. Considerably strong evidence from individual longitudinal studies from the UK, the USA and South Korea has found associations between unaffordable housing and outcomes of poor mental health (depression and low score on general health questionnaire) [15, 19, 20]. Within Australia, studies have suggested an association between unaffordable housing and overall mental health among low-to-moderate income households [12], and private renters [4]. Cumulative exposure to higher housing affordability stress is also reported to be negatively associated with poor overall mental health in Australia [11].
Pathways through which housing affordability impacts on mental health are seldom explicitly tested [21]. Material and psychosocial theories are advanced in the literature as explanations for the observed association between social disadvantage and poor health outcomes [22,23,24]. The material explanation stresses the role of economic and socio-structural factors. In this framework, financial hardship is central to the ‘social production’ of disease [23, 24]. Coherent with this theory, explanations for poor mental health effects of unaffordable housing include indirect trade-offs that may harm health, for example, reduced household resources for food, transportation and medical care [14, 21, 25], or financial insecurity, anxiety and stress related to a fear of foreclosure/eviction if housing costs are not met [19].
In contrast, psychosocial explanations assert that people’s perception of their position in a social hierarchy affects their health, along with lack of control experienced at lower levels of a social hierarchy leading to poor health and health damaging behaviours [22, 24]. Social support mitigates this process; therefore, low levels of social support accentuate the production of poor health through psychosocial processes [22,23,24]. It is postulated that sufficient social support and social cohesion buffer housing-related psychosocial stressors [26]. Housing is implicated in these social processes in more than one way. Housing is a base for social interaction [21]. Housing also shapes access to neighbourhood resources for gaining social support [21]. High housing costs particularly in neighbourhoods with adequate facilities and opportunities for social support pose limited opportunities of engagement for individuals with low socioeconomic resources. Socially disadvantaged individuals are more constrained on residential and neighbourhood choices, leading to socio-spatial sorting and residential segregation based on housing affordability [27]. Consequently, people in unaffordable housing may lack connections and opportunities outside their immediate neighbourhood [21].
Testing material and psychosocial theories as mediators in the association between unaffordable housing and poor mental health is necessary to determine the scope of interventions targeting each for two reasons. First, quantifying the scope of potential interventions directed to addressing financial hardship and social support and second informing a theoretical framework for studying mental health effects of housing affordability [28]. Using longitudinal data allowing for temporal ordering between housing affordability and mental health outcomes, this study quantifies major material and psychosocial pathways between unaffordable housing and mental health.
Methods
Data source
Longitudinal and nationally representative data from was obtained from the Household, Income and Labour Dynamics in Australia (HILDA) survey to address the aim of the study. HILDA is an annual household survey that has collected information on demographic, social, economic and health characteristics since 2001. In its first wave, the survey included 13,969 participants from 7682 randomly sampled households through national probability sample of private dwellings. An additional top-up sample was added in 2011 [29]. Data were collected through interviews and self-completion questionnaires.
The current analysis used a subsample of data from wave 13 (2013) to 15 (2015) to maintain the temporal sequence between changing exposure (housing costs shifting from affordable to unaffordable), mediators and the outcome of mental health. Wave 15 of HILDA was the most recent data available for analysis at the conceptualisation of study. Only individuals aged 15 and above were included in the analysis.
Exposure
Housing costs were designated as unaffordable when households were in the lowest 40% of the equivalised household income distribution and were paying 30% or more of their gross income in rent and mortgage costs [30]. The exposed group was comprised of households whose housing costs changed from being affordable to unaffordable between waves 14 and 15. The unexposed group comprised households whose housing costs remained affordable at each wave. Individuals within households with unaffordable housing in wave 14 were excluded from the analysis.
It should be noted that over time, change in housing affordability stress status is driven by change in either housing costs or income. Previous work has examined this using the HILDA dataset [31]. This work has shown that between two annual waves of the HILDA survey, there is an equal split in the proportion of households that change their housing affordability stress status for either reason.
Outcome
Mental health was assessed in wave 15 (2015) using the Mental Health Inventory (MHI) and Kessler Score (a measure of psychological distress). MHI is a subscale of SF-36, a widely applied general health questionnaire validated in the Australian context [32]. MHI measures symptoms of depression, anxiety and psychological well-being. Its psychometric properties including internal consistency, discriminatory accuracy, test–retest reliability are well established [33]. Five items related to mental health during the past 4 weeks are scored using five response categories. The total scores are transformed to a scale with a mean score of 74 ranging from 0 to 100. Higher scores on this scale reflect better mental health. Another tool, Kessler Psychological Distress Scale (K10) was used to measure psychological distress. The scale measures negative emotional states experienced in the past 30 days and higher scores on the scale ranging from 10 to 50 reflects increased distress [34].
Mediators
Material explanations place primary causal significance on the role of economic deprivation (direct influence of poverty/economic deprivation) in production of health inequalities [23, 24]. Individuals’ perceptions of financial hardship within the current needs and financial responsibilities subjectively capture the economic deprivation experienced by them. Therefore, consistent with the material explanation, financial hardship was included as a mediator. It was derived from the participants’ response to the following question: ‘Given your current needs and financial responsibilities, would you say that you and your family are:’. … (a) prosperous/very comfortable, (b) reasonably comfortable, (c) just getting along/poor/very poor. People selecting (c) were classified as being in financial hardship. For psychosocial theory, we used lack of social support as a mediator. Social support is well identified in the literature as a psychosocial asset that buffers the poor health effects of social inequalities among individuals and populations [35, 36]. We created a derived variable for social support using the average of ten questions addressing different aspects of emotional support rated on a seven-point Likert scale with a higher score reflecting more perceived social support. For ten different aspects, each participant was asked: How much do you agree or disagree with each? The statements were—I do not have anyone that I can confide in, there is someone who can always cheer me up when I am down, I seem to have a lot of friends, I have no one to lean on in times of trouble, I often need help from other people but ca not get it, I enjoy the time I spend with the people who are important to me, people do not come to visit me as often as I would like, when I need someone to help me out, I can usually find someone, when something is on my mind, just talking with the people I know can make me feel better, and, I often feel very lonely. Both mediators were measured in wave 15 (2015).
Covariates
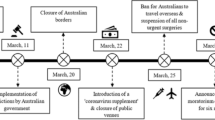
Figure 1 presents the theorised causal relationship between exposure, mediators and the outcome which is presented using a directed acyclic graph (DAG). Potential confounding factors included variables that were deemed to be common causes of the exposure, mediators and outcome. Age and household income are identified in the literature as confounding factors for the relationship between housing affordability and mental health. Consequently, they were included in our analysis as continuous measures [12]. In addition, we included sex, educational attainment (categories), marital status (categories) and employment status (categories) as potential confounding factors. Housing tenure was not included in the analysis, as it has been shown to be an effect modifier in the relationship between housing affordability and mental health [4]. Baseline levels of mental health, financial hardship and social support were also included as covariates in our analysis. All covariates were measured in wave 13 (2013).
Statistical analysis
A sequential approach to mediation analysis was applied to examine the extent to which the causal association between housing costs becoming unaffordable and poorer mental health occurs directly, and the extent to which it occurs through financial hardship and lack of social support [24, 37]. This approach partitions the total causal effect (TCE) of the exposure on outcome, into an indirect effect (effect that acts through the mediator) and the direct effect (pathways other than those that involve mediator). The TCE of housing costs becoming unaffordable on mental health was decomposed into natural direct effects (NDE) and natural indirect effects (NIE) through financial hardship and social support. This approach has key advantages over traditional approaches for testing mediation, as it allows consideration of multiple causally related mediators (with strong assumptions of causal ordering), and accounts for exposure–mediator interactions. The exposure–mediator interaction is a key source of potential bias in traditional approaches to mediation [37, 38]. The NIE through financial hardship (and its causal descendants) was estimated in Model 1, which estimated the pathway operating through financial hardship and the pathways operating through financial hardship and social support (see Fig. 1). Model 2 additionally estimated the NIE through social support independent of financial hardship.
The marginal TCE, NDE and NIE were estimated by applying a weighting approach [24, 37, 38]. Inverse probability weighting (IPW) was used to maximise exchangeability of the comparison groups. IPW can account for potential confounding of exposure–mediator and exposure–outcome associations by measured covariates. Multilevel multivariable linear regression models (individuals nested within households) including baseline covariates were applied to estimate the association between the exposure and mental health outcomes, without mediators to estimate the TCE and with mediators to estimate the NDE and NIE. Interaction terms were included between exposure and each of the mediator variables. Bootstrapping with 1000 replications was used to calculate 95% confidence intervals (CIs). Complete case analyses were conducted in Stata v15.
To quantify any potential effect of missing data, we examined the differences in baseline characteristics of respondents and non-respondents (Appendix Table 1). We also imputed missing data using multivariate imputation using chained equations (MICE) in Stata v15. Continuous variables (mental health outcomes and social support) were imputed using linear regression and categorical variables (education, employment, marital status and financial hardship) using multinomial logistic regression models. To combine the estimates from multiple imputations and bootstrapping, we first created 50 imputed datasets. Next, using user-written program with ‘mim: prefix’, coefficients from the imputed datasets were retrieved and bootstrapped with 50 replications to calculate 95% confidence intervals (CIs). This approach was consistent with the MI-Boot method suggested to integrate estimates from multiple imputation and bootstrapped standard errors [39].
Results
The analytical sample comprised 10,654 individuals, and around 4% (n = 421) had housing costs (relative to income) that became unaffordable between 2014 and 2015. A flowchart of eligible sample is presented in Appendix 1. Individuals whose housing costs changed were younger (mean 37.5 years) with low monthly income (mean $AUD732) compared to those whose housing costs remained affordable across two waves (mean age 46.1 years, mean income $AUD1035). Individuals whose housing became unaffordable were more likely to have not completed post-secondary education, be unemployed, experience financial hardship, and be unmarried, compared to those for whom housing remained affordable (Table 1).
TCE of housing costs becoming unaffordable was found to be associated with a mean score reduction of 1.3 (95% CI: − 2.6, − 0.4) on the MHI scale. When financial hardship was modelled as a mediator, the NIE was estimated at − 0.7 (95% CI: − 1.1, 0.04), corresponding to 54% of the total effect (Model 1). Collectively, financial hardship and social support explained 68% of the total mental health effect of housing costs becoming unaffordable (NIE: − 0.9, 95% CI: − 1.4, − 0.1). On the Kessler psychological distress scale, the TCE of housing costs becoming unaffordable was a mean increase of 0.9 (95% CI: 0.4, 1.4). The NIE through financial hardship was 0.5 (95% CI: 0.1, 0.8) amounting to 53% of the total effect. Further addition of social support as a mediator in the sequential approach led to the NIE estimated at 0.6 (95% CI: 0.2, 1.0), explaining 67% of the total effect (Table 2).
Results from the multiple imputations showed attenuation in magnitude of both TCE and NIE on MHI scale and Kessler Psychological Distress Scale. However, findings of substantial mediation by financial hardship in the relationship between unaffordable housing and mental health were consistent. A total of 47% and 58% (with social support) effect on MHI scale, and 47% and 60% (with social support) on Kessler Psychological Distress Scale were explained by financial hardship, respectively (Table 3).
Discussion
This study is the first to confirm that a substantial proportion of the effect of unaffordable housing on mental health is transmitted through financial hardship and its descendent pathways. These findings suggest that the mental health of people affected by housing affordability problems should focus primarily on alleviating the material circumstances of lower income households when their housing costs become unaffordable. That said, social support is also shown to be additionally beneficial in protecting their mental health. We note that this study intentionally aimed to derive this evidence at the population average level. We hypothesise that the relative importance of social support and financial hardship may indeed vary for key sub-populations who may be especially vulnerable to unaffordable housing, such as people living with an existing mental illness. For these groups, the potential protective role of social support may be heightened, and this may be a valuable focus for future work.
This study has several strengths and some limitations. To our knowledge, previous work has proposed that there is a logical link between housing costs and broader poverty in driving mental health outcomes, but there has to date been little understanding of the pathways of effect [21, 25]. Applying advanced and robust methods for causal modelling and assessment of mediation, the current study addresses a significant gap regarding the role of financial hardship and social support in the relationship between housing affordability and mental health. Using data from a longitudinal national sample permitted to account for the temporal ordering where the exposure to unaffordable housing precedes the outcome, and also to address prior circumstances that act as confounding factors for the association between unaffordable housing and poor mental health. Additionally, by adjusting for mediators and mental health status at baseline, we were able to quantify the effect of unaffordable housing on change in mediator and change in outcome which makes the analysis more robust and strengthens our ability to draw causal conclusions. Robustness of current findings was confirmed on two different mental health screening tools—MHI and Kessler psychological distress scale. Both tools are validated in Australian context and are worded in opposite directions—higher score on MHI reflects better mental health, while a higher score on Kessler psychological distress scale reflects poorer mental health [32,33,34]. It is likely that pathways through which housing affordability leads to poor mental health vary across different life stages. We lacked statistical power to examine mediation by financial hardship and social support in this relationship within age groups and, therefore, future studies should address this gap in knowledge. Findings on the effect of unaffordable housing and mental health and mediation by financial hardship and social support were similar despite excluding younger adults (< 25 years old) who may not contribute financially to households in a sensitivity analysis (Appendix Table 2). Finally, we were able to quantify the contribution of missing data in our observed estimates using a multiple imputation technique, a challenge with most longitudinal studies.
This study has some limitations. Causal inference and methods applied in this study rely on the strong assumption that there is no confounding factor between unaffordable housing, mediators and mental health. Based on the existing literature, most potential confounding factors measured in the survey were accounted for using IPW. However, some residual confounding factors due to unmeasured confounders cannot be ruled out. All variables in HILDA are self-reported and therefore may be measured with error. Particularly problematic is the measurement of financial hardship, social support (mediators) and mental health (outcome) which are subjective measures and obtained from the same individual and recorded in the same wave, therefore may lead to dependent measurement error, where the measurement error of one variable is correlated with the measurement error of another variable in the analysis [40].
Findings on the causal association between housing costs becoming unaffordable and poor mental health substantiate the existing evidence from Australia, the US, South Korea and the UK [4, 11, 12, 15, 19, 20]. This current analysis, however, does not examine the role of tenure as an effect modifier of the relationship between housing affordability stress and mental health that has been previously observed in Australia [41]. Future research could consider if the pathways identified in this paper are tenure specific.
The relatively high degree of mediation by financial hardship substantiates the hypothesis that when housing costs become unaffordable, there are indirect trade-offs related to health resources, and financial insecurities, that lead to poor mental health [14, 19, 21, 25]. Perhaps unsurprisingly, given the substantial importance of housing costs to total household expenditure [14, 19, 21, 25], financial hardship dominates the explanation of the mental health effect of poor housing affordability. Increased financial hardship may also lead to housing insecurity. Households with financial hardship are more likely to doubt their ability to avoid house eviction or repossession further negatively impacting on mental health. Finally, evidence has established that self-perceived financial hardship is associated with stress and poor mental health outcomes including depression [42, 43], and our findings highlight its role in the relationship between housing affordability and mental health. This notion is consistent with the idea of social conditions as the fundamental causes of disease and health inequalities [44, 45].
Therefore, policy interventions directed to address financial hardship can substantially reduce ill effects of unaffordable housing on mental health.
Additionally, this study shows that all aspects (material and psychosocial) pertaining to housing disadvantage must be considered when housing is examined as a determinant of health [5].
Research and policy implications
Grounded in existing theories proposed to explain health inequalities [22,23,24], this study addressed an important gap in theoretical framework for the mechanisms driving the causal relationship between one key social determinant—unaffordable housing—and poor mental health [28]. It must be noted that housing affordability varies across different social, political and economic contexts [46]. Comparisons of our findings with similar investigations in the future from other countries will shed light on the potential role of contexts which may strengthen our understanding of the pathways by which the effect operates. It is likely that depending on underlying social and political context, mechanisms are likely to vary with different context, so proportion mediated could also differ as well as the TCE. As highlighted in study limitations, the current study used a self-assessed subjective measure of financial hardship as a proxy measure of material disadvantage. Future studies may use objective measures of material and financial circumstances that can help in decomposing components of overall financial hardship related to unaffordable housing.
From a policy perspective, the fact that there are (at least) two pathways by which the mental health effect of unaffordable housing may be mediated is helpful. Moreover, current findings implicate multiple choices of policy interventions. First, reducing unaffordable housing can lead to increased mental health at the population level. Alternatively, addressing financial hardship through welfare policies can reduce the detrimental mental health effects of unaffordable housing by half of its magnitude. Finally, the results also show that only addressing social support may have limited impact in reducing ill effects of unaffordable housing on mental health. For some groups, social support may be an important addition to wider interventions. This is interesting in the context of recent Australian government mental health policy direction [47], which prioritises both packages of social support, and affordable accommodation, in the Roadmap for Mental Health Reform (2012–2022).
It is widely evidenced that socially disadvantaged individuals often move between unaffordable and affordable housing [11], and the current study showed that such change is associated with poor mental health. Housing and mental health promotion policies must consider the dynamicity related to unaffordable housing and should be directed to reducing exposures to unaffordable housing over the life course.
Conclusion
The study strengthens the evidence that housing affordability is associated with mental health among Australians. More than half of the effect is mediated through material factors. Elucidation of the pathways between housing affordability and mental health using mediation analysis provides new insight into the mechanisms driving the mental health effects of unaffordable housing and provides evidence with which to design appropriate interventions.
References
WHO (2014) Social determinants of mental health. WHO and the Calouste Gulbenkian Foundation, Geneva
Lund C, Brooke-Sumner C, Baingana F, Baron EC, Breuer E, Chandra P, Haushofer J, Herrman H, Jordans M, Kieling C, Medina-Mora ME, Morgan E, Omigbodun O, Tol W, Patel V, Saxena S (2018) Social determinants of mental disorders and the Sustainable Development Goals: a systematic review of reviews. Lancet Psychiatry 5(4):357–369. https://doi.org/10.1016/S2215-0366(18)30060-9
Braubach M (2011) Key challenges of housing and health from WHO perspective. Int J Public Health 56(6):579–580. https://doi.org/10.1007/s00038-011-0296-y
Mason KE, Baker E, Blakely T, Bentley RJ (2013) Housing affordability and mental health: does the relationship differ for renters and home purchasers? Soc Sci Med 94:91–97. https://doi.org/10.1016/j.socscimed.2013.06.023
Baker E, Beer A, Lester L, Pevalin D, Whitehead C, Bentley R (2017) Is housing a health insult? Int J Environ Res Public Health 14(6):1–8. https://doi.org/10.3390/ijerph14060567
Durand CP, Andalib M, Dunton GF, Wolch J, Pentz MA (2011) A systematic review of built environment factors related to physical activity and obesity risk: implications for smart growth urban planning. Obesity Rev 12(5):e173–e182. https://doi.org/10.1111/j.1467-789X.2010.00826.x
Thomson H, Petticrew M, Morrison D (2001) Health effects of housing improvement: systematic review of intervention studies. BMJ 323(7306):187–190
Thomson H, Thomas S, Sellstrom E, Petticrew M (2009) The health impacts of housing improvement: a systematic review of intervention studies from 1887 to 2007. Am J Public Health 99(Suppl 3):S681–S692. https://doi.org/10.2105/AJPH.2008.143909
Cohen DA, Farley TA, Mason K (2003) Why is poverty unhealthy? Social and physical mediators. Soc Sci Med 57(9):1631–1641. https://doi.org/10.1016/s0277-9536(03)00015-7
Bentley R, Baker E, LaMontagne A, King T, Mason K, Kavanagh A (2016) Does employment security modify the effect of housing affordability on mental health? SSM Popul Health 2:778–783. https://doi.org/10.1016/j.ssmph.2016.09.003
Bentley R, Baker E, Mason K (2012) Cumulative exposure to poor housing affordability and its association with mental health in men and women. J Epidemiol Community Health 66(9):761–766. https://doi.org/10.1136/jech-2011-200291
Bentley R, Baker E, Mason K, Subramanian SV, Kavanagh AM (2011) Association between housing affordability and mental health: a longitudinal analysis of a nationally representative household survey in Australia. Am J Epidemiol 174(7):753–760. https://doi.org/10.1093/aje/kwr161
Kavanagh AM, Aitken Z, Baker E, LaMontagne AD, Milner A, Bentley R (2016) Housing tenure and affordability and mental health following disability acquisition in adulthood. Soc Sci Med 151:225–232. https://doi.org/10.1016/j.socscimed.2016.01.010
Pollack CE, Griffin BA, Lynch J (2010) Housing affordability and health among homeowners and renters. Am J Prev Med 39(6):515–521. https://doi.org/10.1016/j.amepre.2010.08.002
Pevalin DJ, Taylor MP, Todd J (2008) The dynamics of unhealthy housing in the UK: A panel data analysis. Hous Stud 23(5):679–695. https://doi.org/10.1080/02673030802253848
Taylor MP, Pevalin DJ, Todd J (2007) The psychological costs of unsustainable housing commitments. Psychol Med 37(7):1027–1036. https://doi.org/10.1017/S0033291706009767
Milligan V, Phibbs P, Gurran N, KF (2007) Approaches to evaluation of affordable housing initiatives in Australia. Australian Housing and Urban Research Institute Limited, Melbourne:AHURI Research Paper No. NRV3-7
Downing J (2016) The health effects of the foreclosure crisis and unaffordable housing: a systematic review and explanation of evidence. Soc Sci Med 162:88–96. https://doi.org/10.1016/j.socscimed.2016.06.014
Lee TH, Park EC, Kim W, Kim J, Shin J, Kim TH (2016) Depressive symptoms of house-poor persons: Korean panel data evidence. Int J Soc Psychiatry 62(6):569–577. https://doi.org/10.1177/0020764016653773
Alley DE, Lloyd J, Pagan JA, Pollack CE, Shardell M, Cannuscio C (2011) Mortgage delinquency and changes in access to health resources and depressive symptoms in a nationally representative cohort of Americans older than 50 years. Am J Public Health 101(12):2293–2298. https://doi.org/10.2105/ajph.2011.300245
Dunn JR (2000) Housing and health inequalities: review and prospects for research. Hous Stud 15(3):341–366. https://doi.org/10.1080/02673030050009221
Bartley M (2004) Health inequality: an introduction to theories, concepts, and methods. Polity Press, Cambridge
Townsend P, Davidson N, Black DS (1982) Inequalities in health: the Black report. Penguin, Harmondsworth
Aitken Z, Simpson JA, Gurrin L, Bentley R, Kavanagh AM (2018) Do material, psychosocial and behavioural factors mediate the relationship between disability acquisition and mental health? A sequential causal mediation analysis. Int J Epidemiol. https://doi.org/10.1093/ije/dyx277
Dunn JR, Hayes MV (1999) Identifying social pathways for health inequalities. The role of housing. Ann N Y Acad Sci 896:399–402
Smith CA, Smith CJ, Kearns RA, Abbott MW (1993) Housing stressors, social support and psychological distress. Soc Sci Med 37(5):603–612. https://doi.org/10.1016/0277-9536(93)90099-P
Anderson LM, Charles JS, Fullilove MT, Scrimshaw SC, Fielding JE, Normand J, Task Force on Community Preventive S (2003) Providing affordable family housing and reducing residential segregation by income. A systematic review. Am J Prev Med 24(3 Suppl):47–67
Thomson H, Thomas S (2015) Developing empirically supported theories of change for housing investment and health. Soc Sci Med 124(Supplement C):205–214. https://doi.org/10.1016/j.socscimed.2014.11.043
Summerfield M, Freidin S, Hahn M, Ittak P, Li N, Macalalad N, Watson N, Wilkins R, Wooden M (2011) HILDA user manual–release 10. Melbourne Institute of Applied Economic and Social Research, University of Melbourne, Melbourne
Yates J, Milligan V (2007) Housing affordability: a 21st century problem. AHURI Final Report No. 105. Australian Housing and Urban Research Institute Limited, Melbourne
Baker E, Mason K, Bentley R (2015) Measuring housing affordability: a longitudinal approach. Urban Policy Res 33(3):275–290. https://doi.org/10.1080/08111146.2015.1034853
Butterworth P, Crosier T (2004) The validity of the SF-36 in an Australian National Household Survey: demonstrating the applicability of the Household Income and Labour Dynamics in Australia (HILDA) Survey to examination of health inequalities. BMC Public Health 4:44. https://doi.org/10.1186/1471-2458-4-44
Pirkis J, Burgess P, Kirk P, Dodson S, Coombs T (2005) Review of standardised measures used in the National Outcomes and Casemix Collection (NOCC). NSW, Sydney
Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SL, Walters EE, Zaslavsky AM (2002) Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med 32(6):959–976
Kawachi I (1999) Social capital and community effects on population and individual health. Ann N Y Acad Sci 896:120–130
Wilkinson RG (1999) Health, hierarchy, and social anxiety. Ann N Y Acad Sci 896:48–63
VanderWeele TJ, Vansteelandt S (2014) Mediation analysis with multiple mediators. Epidemiol Methods 2(1):95–115. https://doi.org/10.1515/em-2012-0010
VanderWeele TJ (2015) Explanation in causal inference: methods for mediation and interaction. Oxford University Press, New York
Schomaker M, Heumann C (2018) Bootstrap inference when using multiple imputation. Stat Med 37(14):2252–2266. https://doi.org/10.1002/sim.7654
VanderWeele TJ, Hernán MA (2012) Results on differential and dependent measurement error of the exposure and the outcome using signed directed acyclic graphs. Am J Epidemiol 175(12):1303–1310. https://doi.org/10.1093/aje/kwr458
Bentley RJ, Pevalin D, Baker E, Mason K, Reeves A, Beer A (2016) Housing affordability, tenure and mental health in Australia and the United Kingdom: a comparative panel analysis. Hous Stud 31(2):208–222. https://doi.org/10.1080/02673037.2015.1070796
Dunn N, Inskip H, Kendrick T, Oestmann A, Barnett J, Godfrey K, Cooper C (2008) Does perceived financial strain predict depression among young women? Longitudinal findings from the Southampton Women’s Survey. Ment Health Fam Med 5(1):15–21
Handley TE, Rich J, Lewin TJ, Kelly BJ (2019) The predictors of depression in a longitudinal cohort of community dwelling rural adults in Australia. Soc Psychiatry Psychiatr Epidemiol 54(2):171–180. https://doi.org/10.1007/s00127-018-1591-1
Link BG, Phelan J (1995) Social conditions as fundamental causes of disease. J Health Soc Behav 35:80–94. https://doi.org/10.2307/2626958
Phelan JC, Link BG, Tehranifar P (2010) Social conditions as fundamental causes of health inequalities: theory, evidence, and policy implications. J Health Soc Behav 51(1_suppl):S28–40. https://doi.org/10.1177/0022146510383498
Beer A, Kearins B, Pieters H (2006) Housing affordability and planning in australia: the challenge of policy under neo-liberalism. Hous Stud 22(1):11–24. https://doi.org/10.1080/02673030601024572
COAG (2012) The roadmap for national mental health reform 2012–2022. Council of Australian Governments, Canberra
Acknowledgements
Rebecca Bentley and Emma Baker are supported by Australian Research Council’s Future Fellowship program (FT150100131 and FT1401100872, respectively). We are grateful to Dr Koen Simons for his statistical guidance on combining estimates from multiple imputation and bootstraps.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Singh, A., Aitken, Z., Baker, E. et al. Do financial hardship and social support mediate the effect of unaffordable housing on mental health?. Soc Psychiatry Psychiatr Epidemiol 55, 705–713 (2020). https://doi.org/10.1007/s00127-019-01773-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-019-01773-z