Abstract
Purpose
The course of conduct disorder (CD) is heterogeneous. Moffitt proposed the heuristic of life course persistent (LCP) and adolescence limited (AL) to differentiate etiologically distinct forms of antisocial behavior (AB), each with distinct predictors and consequences, although a few studies have assessed this demarcation within the context of CD. The objective of this study was to apply Moffitt’s taxonomy in a nationally representative US sample to investigate the prevalence, predictors, and outcomes of LCP and AL CD.
Methods
Data come from the Collaborative Psychiatric Epidemiology Studies, a set of population-based nationally representative cross-sectional surveys (N = 20,130). Predictors included harsh discipline, maternal and paternal closeness, poverty in childhood, history of learning disability, parental deviance, and nativity. Outcomes included substance use, employment status, education attainment, marital status, income level, and self-rated mental and physical health.
Results
The prevalence of LCP and AL CD was 0.5 and 4.6%, respectively, for females, and 1.9 and 5.1%, respectively, for males. Low childhood SES [Odds Ratio (OR) = 3.49], lack of maternal closeness (OR = 2.50), and history of harsh discipline (OR = 2.17) increased odds of LCP group membership. The LCP group had higher odds of developing substance use disorders (OR = 2.00) relative to AL.
Conclusions
LCP CD is more strongly influenced by childhood environment and confers increased odds for substance use problems in adulthood relative to AL CD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Conduct disorder (CD) is characterized by pervasive patterns of hostile, aggressive, cruel, deceitful, and destructive behaviors [1]. CD typically develops in childhood or adolescence [2], and is associated with significantly increased risk for legal problems [3], poor physical health [4], co-morbid psychiatric conditions [5], and premature mortality [6]. The lifetime prevalence of CD is approximately 12% in males and 7% in females [7].
Patterns of heterogeneity within CD have long been observed [8] and various methods of sub-classifying CD have been proposed. Moffitt proposed one such method in her developmental taxonomy of antisocial behavior (AB) [9], which now constitutes the basis of the DSM-5 CD childhood- vs. adolescent-onset classification [1]. Within Moffitt’s classification system, two subgroups of AB were defined: life course persistent (LCP) and adolescence limited (AL) [9]. The LCP group is characterized by AB onset in childhood, with symptoms of AB persisting well into adulthood. In contrast, the AL group is characterized by AB onset in adolescence with symptoms desisting by the early adulthood. In large Oceanic and European samples, the prevalence of LCP and AL AB has been estimated at 5–10 and 10–26%, respectively, for males and 0.4–3 and 2–18%, respectively, for females [10–12]. In a population-based nationally representative US sample, the prevalence of LCP and AL AB was estimated at approximately 7.4 and 11.6%, respectively, for males and 6.9 and 11.4%, respectively, for females [13]. However, there are no well-established estimates of LCP and AL prevalence in the context of CD within the US population.
Over the last several decades, the LCP/AL distinction has continued to generate a wealth of theoretical and empirical literature. Theoretically, LCP AB is thought to be a more severe form of the condition, whereas AL AB is posited to be more akin to a heightened expression of normal adolescent behavior [9, 14]. In addition, LCP AB is thought to be influenced by genetic predisposition and/or neuropsychological deficits and exacerbated by risk factors relating to the childhood familial environment (e.g., poverty, inadequate parenting, and family conflict), whereas AL AB primarily stems from adolescent environmental factors, such as peer relationships [9, 14].
While the relationship between early childhood factors and CD in general has been well established [4, 15, 16], few studies have examined whether these factors differentially predict LCP vs. AL CD. Of the reports that have attempted to predict group membership, most have studied only male participants [17], or have been unable to accurately assign participants into LCP and AL groups due to a lack of data on adult AB/CD symptoms [18, 19]. In a recent study examining CD age of onset (one component of the LCP/AL distinction), both childhood- and adolescent-onset CD were similarly influenced by genetic factors; however, family dysfunction was more strongly associated with childhood-onset CD when compared to adolescent-onset CD [20]. Despite the problems with LCP/AL classification in extant studies, early life psychosocial adversity [e.g., low socioeconomic status (SES), parental conflict, harsh discipline, and low parental support/involvement] has generally emerged as the most salient predictor of early onset and enduring AB/CD [11, 18–20].
In addition to differential predictors, Moffitt also argued that those in the LCP group have lower quality of life in adulthood due to their persistent antisocial behavior. Moffitt went further by arguing that AL AB is developmentally normative, and is due to “the widening gap between biological and social maturity” in today’s adolescent environment [9, p. 692]. Several studies have tested this hypothesis by examining whether LCP/AL subgroups differentially predict adult outcomes. Based on these studies, the early onset enduring AB (akin to the LCP distinction) appears to be more strongly associated with a diverse set of negative adult outcomes compared to adolescent-onset, including poorer mental health [21, 22], substance use problems [12, 21, 22], as well as problems with unemployment and family relationships [21].
It is important to note that a large percentage of research to date on the LCP/AL distinction has been conducted in European and Oceanic samples. Although several US birth cohorts have examined this distinction [23–25], to the authors’ knowledge, only two studies have used population-based US samples [13, 26], and neither of these examined LCP/AL in the context of CD. The overarching goal of the current study is to address this gap in the literature by investigating the prevalence, predictors, and outcomes of LCP and AL CD, as defined in Moffitt’s taxonomy, in a large, population-based, nationally representative, epidemiological US sample. The first aim of this study was to examine the prevalence of LCP and AL within the context of CD for the first time in a population-based nationally representative US sample. Because the prevalence of LCP/AL CD is not well established, we hypothesized that LCP CD would be less prevalent than AL CD in both males and females, and that female prevalence of both LCP and AL CD would be less than that of males. The second aim was to examine a range of early childhood familial factors to determine which differentially predict LCP vs. AL CD. Given that recent research shows that childhood- and adolescent-onset CD both appear to be influenced similarly by genetic factors [20], it was hypothesized that childhood familial factors (i.e., history of harsh discipline, lack of maternal closeness, lack of paternal closeness, low SES, and US nativity) would differentially predict LCP vs. AL group membership. The final aim was to examine a range of adult outcomes (i.e., educational attainment, employment, SES, perceived mental and physical health, substance use disorders, and romantic relationships) to determine if LCP vs. AL CD was differentially associated with outcomes in adulthood. Given that persistent AB appears to confer additional risk for a host of negative adult outcomes [12, 21, 22], it was hypothesized that LCP CD would be differentially associated with poorer adult outcomes relative to AL CD.
Methods
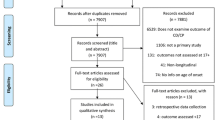
Sample
Data come from the Collaborative Psychiatric Epidemiology Studies (CPES) [27], a joint collaboration of three cross-sectional, population-based, nationally representative, epidemiological studies: the National Comorbidity Survey Replication (NCS-R) [28], the National Survey of American Life (NSAL) [29], and the National Latino and Asian American Study (NLAAS) [30]. Each of these studies used sampling techniques designed to obtain a nationally representative sample of their target populations: The entire US population for the NCS-R (N = 9282), African Americans and Americans of Caribbean decent for the NSAL (N = 6199), and Latino and Asian Americans for the NLAAS (N = 4649). The three samples were recruited from 252 geographic areas (“primary sampling units”) across the contiguous United States (plus Hawaii in the NLAAS sample). All eligible participants aged 18 or older were interviewed face-to-face in their home by a trained interviewer utilizing a computer-assisted interview technique. The weighted response rates were 70.9, 71.5, and 75.7% for NCS-R, NSAL, and NLAAS, respectively. The University of Michigan Institutional Review Board approved the CPES and all participants provided informed consent. Additional details regarding the design of the CPES and its included samples are described elsewhere [27–30].
Lifetime history of CD was based on ICD-10 diagnostic criteria [31] and assessed using the Composite International Diagnostic Interview (CIDI) [32]. The CIDI is a fully structured diagnostic instrument modeled after a clinical psychiatric interview. LCP CD (N = 181) was defined as (a) onset of CD diagnosis prior to age 13 and (b) persistence of CD diagnosis at age 24 or older. AL CD (N = 795) was defined as (a) onset of CD diagnosis at age 13 or older and (b) desistence of CD diagnosis by age 24. Age 13 was used as the onset cutoff because using an earlier cutoff for CD diagnosis decreased the LCP sample size appreciably. Furthermore, age 13 corresponds to the developmental period when puberty has begun in most children and patterns of genetic influences have mostly stabilized [33]. Due to the age 24 cutoff for desistance, all respondents aged <24 at the time of interview were excluded from the analyses to ensure appropriate group assignment. Because of differences in missing information across variables and data sets, the analytic sample sizes varied from N = 353 to N = 15,447, depending on the specific analysis.
Measures
Early childhood predictors
A range of early childhood factors were examined as predictors of CD group membership: history of harsh discipline, lack of maternal closeness, lack of paternal closeness, having a learning disability, low childhood SES, and parental deviance. Due to the inclusion of a large number of immigrants in the NSAL and NLAAS surveys, country of origin was also assessed as a possible early childhood factor. All of these variables were retrospectively self-reported.
Harsh discipline
History of harsh discipline was assessed based on respondents’ answer to the question “How frequently did someone push, grab, shove, slap, hit, spank, or throw something at you when growing up?” Respondents who answered “often” or “sometimes” were classified as having a history of harsh discipline, whereas respondents who answered “rarely” or “never” were classified as having no history of harsh discipline.
Parental closeness
Maternal and paternal closeness were assessed based on the questions “How emotionally close to your maternal figure were you when growing up?” and “How emotionally close to your paternal figure were you when growing up?” Respondents who answered “not at all close” or “not very close” were classified as having a lack of closeness to that respective parental figure. Respondents who answered “very close” or “somewhat close” were classified as being close to that respective parental figure.
Parental deviance
Parental deviance was assessed based on respondents’ answers to six questions in which they were asked to indicate if, when growing up, their maternal figure “lied a lot,” “often got into physical fights” and/or “was involved in criminal activities.” The same questions were asked in regard to respondents’ paternal figures. Respondents who answered affirmatively to two or more of these six questions were classified as having a history of parental (maternal or paternal) deviance.
Childhood socioeconomic status
Low childhood SES was assessed based on a single question in which respondents were asked to indicate if their family received government assistance for six or more months during their childhood or adolescence. Respondents who answered this question affirmatively were classified as having low childhood SES.
Country of origin
Country of origin was based on a single question in which the respondents were asked to report the country they were born in. Participants were divided into two groups: US-born and foreign-born.
Learning disabilities
Presence of a learning disability was assessed based on a single self-report question in which respondents were asked to indicate if they “have a learning disability.” An affirmative response to this question was used to categorize participants as either having a learning disability or not.
Adult outcomes
A range of negative adult outcomes were examined as consequences of LCP vs. AL CD: not finishing high school, never being married, being currently unemployed, having a household income at or below the poverty level, having poor self-rated physical or mental health, and having a substance use disorder. All of these measures were assessed by self-report.
Educational attainment
Respondents who reported grade 11 or less as their highest grade completed were classified as never completing high school (low educational attainment) vs. high educational attainment.
Marital status
Respondents who reported their marital status as “married/cohabitating” or “divorced/separated/widowed” were classified as having a history of being married. Only those who answered “never married” were classified as never being married.
Employment status
Respondents were asked to classify their employment status as either (a) employed, (b) unemployed, or (c) not in the labor force (i.e., retired, disabled). Respondents who reported being “unemployed” or “not in the labor force” were classified as being currently unemployed. Only those who reported being “employed” were classified as employed.
Poverty
Poverty was assessed by the income-to-needs ratio, with a ratio below 1 indicating that the respective family is below the official definition of poverty [34]. Respondents with an income-to-needs ratio of one or below were classified as being at or below the poverty level, whereas those with an income-to-needs ratio greater than one were classified as being above the poverty level.
Mental and physical health
Respondents were asked to rate there perceived mental and physical health on a 5-point rating scale from poor to excellent. Those who answered “poor” or “fair” to either question were classified as having poor health in that particular category (mental or physical). Respondents who answered “excellent” or “very good” were classified as having good health in that particular category.
Substance use
Current (past 12 months) substance use disorders (SUDs) were assessed using the CIDI modules for licit (alcohol) and illicit (cannabis, cocaine, heroin, etc.) substances using ICD-10 criteria for abuse or dependence. Respondents were classified as having a SUD if they met criteria for any diagnoses (alcohol abuse or dependence, drug abuse or dependence). Respondents were classified as not having a SUD if they did not meet criteria for all four of these diagnoses. In addition to examining SUDs as a whole, each of the four SUD diagnoses was examined separately.
Analysis
Logistic regression was used to estimate odds ratios and 95% confidence intervals separately for each childhood predictor and negative adult outcome. For analyses of childhood predictors, the dependent variable was defined as LCP CD (vs. AL CD as reference). For analyses of negative adult outcomes, the independent variable was defined as LCP CD (vs. AL CD as reference). Adjusted regressions included sex, age, and race/ethnicity as covariates.
To account for the complex sampling design of the CPES and our subsetting of respondents with CD, models were fit using PROC Surveylogistic and the DOMAIN statement in SAS [35].
Results
Sample Demographics
Table 1 displays the demographic characteristics of the analytic sample, stratified by LCP CD and AL CD status, as well as individuals who never met criteria for ICD-10 CD. The LCP group consisted of 181 respondents (78.6% male, 21.4% female), with a mean age of approximately 37 years (range 24–70). The AL group consisted of 795 respondents (49.3% male, 50.7% female) with a mean age of approximately 35 years (range 24–81). The group who never met criteria for CD consisted of 6028 individuals (44.5% male, 55.5% female) with a mean age of approximately 51 years (range 24–98).
Prevalence of LCP and AL CD
Table 2 displays the prevalence of AL and LCP CD among the total sample and among the sample meeting criteria for lifetime ICD-10 CD. All estimates reflect weighted percentages. Among the total sample age 24 or older at the time of interview, 1.1% of respondents were classified as LCP CD and 4.8% were classified as AL CD. Among those who met criteria for lifetime ICD-10 CD (and were age 24 or older at the time of interview), 9.9% were classified as LCP, 42.1% were classified as AL, and 48.0% did not fit into either then LCP or AL categories.
For females, 0.5 and 4.6% of the total sample were classified as LCP and AL CD, respectively. For females who met criteria for lifetime ICD-10 CD, 5.2 and 53.9% were classified as LCP and AL, respectively, and 40.9% did not fit into either category. For males, 1.9 and 5.1% of the total sample were classified as LCP and AL CD, respectively. For males who met criteria for lifetime ICD-10 CD, 13.1 and 33.9% were classified as LCP and AL, respectively, and 53.0% did not fit into either category.
Predictors of LCP vs. AL CD
History of harsh discipline, lack of maternal closeness, and low childhood SES differentially increased odds of LCP vs. AL CD after controlling for race/ethnicity, sex, and age (Table 3). Those with a low childhood SES had approximately 3.5 times higher odds (OR = 3.49, 95% CIs 1.53–7.97, t = 3.06, df = 38, p = .004) of belonging to the LCP group relative to the AL group. Those who lacked closeness with their primary maternal figure had 2.5 times higher odds (OR = 2.50, 95% CIs 1.16–5.39, t = 2.42, df = 38, p = .021) of belonging to the LCP group relative to the AL group. In addition, those with a history of harsh discipline had approximately 2.2 times higher odds (OR = 2.17, 95% CIs 1.23–3.83, t = 2.77, df = 38, p = .009) of belonging to the LCP group relative to the AL group. Parental deviance was also associated with higher odds of LCP group membership, but this relationship was not significant after accounting for demographic characteristics. No significant relationship was found between CD group membership and lack of paternal closeness, US nativity, or history of learning disabilities.
Adult outcomes of LCP vs. AL CD
Relative to the AL group, respondents in the LCP group had two times higher odds of reporting a recent (i.e., past 12 month) SUD, but this relationship did not remain significant after accounting for demographic characteristics. Post-hoc analyses revealed that the association between LCP group membership and increased odds of a SUD was carried primarily by alcohol abuse and alcohol dependence, both of which remained significant in separate regressions after controlling for race/ethnicity, sex, and age (alcohol abuse OR = 2.66, 95% CI = 1.26–5.61, t = 2.60, df = 107, p = .011; alcohol dependence OR = 3.65, 95% CI = 1.42–9.37, t = 2.72, df = 107, p = .008). There was no significant association between CD group membership and past 12-month drug abuse or drug dependence. LCP CD was not associated with the odds of being unemployed, educational attainment, household income, marital status, or self-rated mental or physical health relative to AL CD. Table 4 displays the odds ratios and 95% confidence intervals for all adult outcomes.
Discussion
To our knowledge, this study provides the first prevalence estimates and comprehensive assessment of the predictors and outcomes of LCP and AL AB in the context of CD in a population-based nationally representative sample of US adults. Our findings indicate that approximately 1.1 and 9.9% of US adults have a history of LCP CD and AL CD, respectively. In addition, early life familial factors differentially predict CD group membership, and those with LCP CD are more likely than those with AL CD to have alcohol problems in adulthood. However, these two groups are similar in other adult outcomes.
The initial hypotheses regarding prevalence within the US population were supported. That is, LCP CD was found to be less prevalent than AL CD in both males and females, and the female prevalence was lower than males for both LCP and AL CD. Interestingly, the prevalence of both LCP and AL CD in males and females was at the bottom of the reported range in the previous studies [10–13]. However, this is unsurprising given that the results reported here use a more severe definition of AB than other studies (i.e., diagnosable CD) are the first of their kind within a population-based nationally representative US sample. Furthermore, it is also possible that our strict definition of LCP persistence (i.e., age 24) may have resulted in lower estimates than previously reported.
It is important to note that most CD cases in this data set were neither LCP nor AL (e.g., CD with either onset prior to the AL cut-off but desisted early, onset later than LCP cut-off but persisted, or there was insufficient information to determine AL or LCP status because of missing data on onset or remission). The previous research has shown that about half of those with childhood-onset CD do not display antisocial behavior in adult life [22, 36, 37]. The results reported here, taken together with the previous research, support Moffitt’s suggestion that the recognition of a childhood-limited classification may help refine the original taxonomy [38].
The hypothesis that the early familial factors would differentially increase odds of LCP as compared to AL CD was supported. That is, the majority of familial factors examined (low SES, lack of maternal closeness, and history of harsh discipline) differentially increased odds of LCP CD group membership. Taken together with the previous research (11, 18–20), this supports the hypothesis that LCP AB is, indeed, more strongly influenced by early childhood familial factors relative to AL AB. While Moffitt proposed that LCP AB was influenced by a genetic propensity to AB, adverse early childhood environmental factors were also included in her proposal as factors exacerbating LCP AB [9]. Recent research indicates that childhood- and adolescent-onset CD are both influenced by relatively similar amounts of genetic factors, but that only childhood-onset CD shares common genetic underpinnings with other childhood psychiatric disorders (e.g., ADHD) [20], suggesting distinct genetic etiologies for LCP and AL CD.
Taken together with this previous research, we propose two possible explanations for the association between LCP CD and the early familial factors found in the current study. First, LCP CD may be due to an underlying genetic predisposition to AB/CD, and an inadequate childhood environment may further exacerbate this predisposition (i.e., synergistic gene-environment interaction) [39]. An alternate explanation is that specific childhood familial factors (e.g., inadequate parenting as indexed by harsh discipline and lack of maternal closeness) reflect a parental genetic predisposition to antisocial behavior, which is passed on to children in the form of LCP CD. In other words, early childhood familial factors influencing LCP CD may be genetically mediated [39].
Finally, our results indicate that LCP CD differentially increases odds of recent SUD, specifically alcohol abuse and dependence, relative to AL CD, but that these two groups are otherwise similar in adult outcomes. These results are in line with the previous studies showing that individuals with LCP AB are at an increased risk for substance use problems in adulthood [12, 21, 22]. However, the previous reports of LCP AB conferring increased risk for a broad range of negative adult outcomes (including poorer mental health, unemployment, adult antisocial behavior, and impaired social relationships [12, 20–22]) were not supported. The lack of differentiation in many of these outcomes may be due to (a) the use of a more severe type of AB (diagnosable CD) in the current study rather than more normative AL antisocial individuals, or (b) the fact that both AL and LCP AB confer increased odds of negative adult outcomes. For example, Odgers and colleagues found that those with AL AB and LCP AB both experienced more adverse adult outcomes than those with low levels of AB symptomatology [22]. Taken together, these results call into question the utility of using the LCP/AL distinction in predicting a broad range of impaired adult psychosocial functioning.
Strengths and limitations
This study is the first, to our knowledge, to examine the LCP/AL distinction within the context of CD in a population-based nationally representative US sample. This allows for broader generalizability of LCP/AL findings within the US population. In addition, the breadth of the participant interviews allowed for a large range of predictors and outcomes of CD to be examined. Finally, this study used data on CD age of onset as well as last CD episode to more precisely assign members into LCP and AL groups, bypassing a common drawback found in many LCP/AL studies that use only age of onset or do not have data for participants past early adulthood.
Despite the study’s substantial strengths, the results should also be interpreted in light of several limitations. First, the data regarding CD and associated childhood factors were retrospectively self-reported, and several measures were comprised of only one or two indicators. This may have impacted the reliability of measurement, particularly concerning dating CD age of onset [40]. Furthermore, due to the cross-sectional nature of this study, these findings cannot be interpreted as causal, especially considering that the childhood factors examined could have had temporal overlap with childhood CD symptoms. Another limitation common to most nationally representative epidemiological samples is that a percentage of cases may have been unreachable (e.g., incarcerated). Given the higher rates of CD, AB, and recidivism among incarcerated individuals [41, 42], rates of incarceration may have decreased the overall severity of CD symptoms in the current study.
Although our combined LCP and AL sample was large (N = 976), the cell sizes for individual analyses were much smaller. Due to these small samples, there was limited power to detect factors that may be salient in the LCP/AL distinction. These limited sample sizes also required that males and females be analyzed together, and therefore, sex differences for predictors and outcomes were not examined. The previous research has indicated that similar factors predict LCP AB in males and females, but adulthood consequences of LCP AB are most severe for females [22]. Therefore, future analyses of predictors and outcomes of LCP and AL CD should continue to examine sex-specific relationships.
Finally, examining the LCP/AL distinction in terms of an extreme AB phenotype (i.e., diagnosable CD) represents both strength and a limitation of the current study. While this phenotype limits the generalizability of findings to more normative AB samples, it is important to examine this distinction within the context of CD due to the LCP/AL taxonomy serving as the theoretical basis for the age-of-onset CD subtyping used by clinicians [1].
Conclusion
The results of this study, taken together with the previous research [11, 18–20, 22], support the hypothesis that LCP and AL CD represent etiologically distinct groups, with LCP CD being more heavily influenced by early familial factors. This familial influence on LCP CD suggests that psychosocial interventions relating to the caregiving environment (e.g., improving parent–child relationships) may be especially effective in reducing the early onset symptomatology. However, despite the differences in risk factors, the outcomes of both LCP and AL CD appear relatively similar. Therefore, efforts should be made by relevant professionals (e.g., clinicians, social workers, and school personnel) to target children and adolescents with both sub-types of CD equally.
References
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5th edn. American Psychiatric Publishing, Arlington
Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE (2005) Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiat 62:593–602.
Simonoff E, Elander J, Holmshaw J, Pickles A, Murray R, Rutter M (2004) Predictors of antisocial personality: Continuities from childhood to adult life. Brit J Psychiat 184:118–127.
Bardone AM, Moffitt TE, Caspi A, Dickson N, Stanton WR, Silva PA (1998) Adult physical health outcomes of adolescent girls with conduct disorder, depression, and anxiety. J Am Acad Child Psy 37:594–601
Kim-Cohen J, Caspi A, Moffitt TE, Harrington H, Milne BJ, Poulton R (2003) Prior juvenile diagnoses in adults with mental disorder: Developmental follow-back of a prospective-longitudinal cohort. Arch Gen Psychiat 60:709–717.
Laub JH, Vaillant GE (2000) Delinquency and mortality: A 50-year follow-up study of 1,000 delinquent and nondelinquent boys. Am J Psychiat 157:96–102
Nock MK, Kazdin AE, Hiripi E, Kessler RC (2006) Prevalence, subtypes, and correlates of DSM-IV conduct disorder in the national comorbidity survey replication. Psychol Med 36:699–710
Hindelang MJ, Hirschi T, Weis JG (1981) Measuring delinquency. Sage Publications, Beverly Hills
Moffitt TE (1993) Adolescence-limited and life-course-persistent antisocial behavior: A developmental taxonomy. Psychol Rev 100:674–701
Kratzer L, Hodgins S (1999) A typology of offenders: A test of Moffitt’s theory among males and females from childhood to age 30. Crim Behav Ment Health 9:57–73
Moffitt TE, Caspi A (2001) Childhood predictors differentiate life-course-persistent and adolescence-limited antisocial pathways among males and females. Dev Psychopathol 13:355–375
Bor W, McGee TR, Hayatbakhsh R, Dean A, Najman JM (2010) Do antisocial females exhibit poor outcomes in adulthood? An Australian cohort study. Aust NZ J Psychiat 44:648–657.
Lahey BB, Van Hulle CA, Waldman ID, Rodgers JL, D’Onofrio BM, Pedlow S, Rathouz P, Keenan K (2006) Testing descriptive hypotheses regarding sex differences in the development of conduct problems and delinquency. J Abnorm Child Psychol 24:737–755
Moffitt TE (2003) Life-course-persistent and adolescent-limited antisocial behavior: A 10-year research review and a research agenda. In: Lahey BB, Moffitt TE, Caspi A (eds) Causes of conduct disorder and juvenile delinquency. The Guilford Press, New York, pp 49–75
Jaffee SR, Caspi A, Moffitt TE, Dodge KA, Rutter M, Taylor A, Tully LA (2005) Nature x nurture: Genetic vulnerabilities interact with physical maltreatment to promote conduct problems. Dev Psychopathol 17:67–84
Silberg JL, Maes H, Eaves LJ (2012) Unraveling the effect of genes and environment in the transmission of parental antisocial behavior to children’s conduct disturbance, depression, and hyperactivity. J Child Psychol Psych 53:668–677
Burt SA, Donnellan MB, Iacono WG, McGue M (2011) Age-of-onset or behavioral sub-types? A prospective comparison of two approaches to characterizing the heterogeneity within antisocial behavior. J Abnorm Child Psych 39:633–644
Aguilar B, Sroufe LA, Egeland B, Carlson E (2000) Distinguishing the early-onset/persistent and adolescent-onset antisocial behavior types: From birth to 16 years. Dev Psychopathol 12:109–132
Roisman GI, Monahan KC, Campbell SB, Steinberg L, Cauffman E, The National Institute of Child Health and Human Development Early Child Care Research Network (2010). Is adolescence-onset antisocial behavior developmentally normative?. Dev Psychopathol 22:295–311
Silberg J, Moore AA, Rutter M (2015) Age of onset and the subclassification of conduct/dissocial disorder. J Child Psychol Psych 56:826–833
Moffitt TE, Caspi A, Harrington H, Milne BJ (2002) Males on the life-course-persistent and adolescence-limited antisocial pathways: Follow-up at age 26 years. Dev Psychopathol 14:179–207
Odgers CL, Moffitt TE, Broadbent JM et al (2008) Female and male antisocial trajectories: from childhood origins to adult outcomes. Dev Psychopathol 20:673–716
Huesmann LR, Dubow EF, Boxer P (2009) Continuity of aggression from childhood to early adulthood as predictor of life outcomes: Implications for the adolescent-limited and life-course-persistent models. Agress Behav 35:136–149.
Piquero AR, White NA (2003) On the relationship between cognitive abilities and life-course-persistent offending among a sample of African Americans: a longitudinal test of Moffitt’s hypothesis. J Crim Justice 31:399–409
Loeber R, Stouthamer-Loeber M, Van Kammen W, Farrington DP (1991) Initiation, escalation and desistance in juvenile offending and their correlates. J Crim Law Criminol 82:36–82
Barnes JC, Beaver KM, Boutwell BB (2011) Examining the genetic underpinnings of Moffitt’s developmental taxonomy: A behavioral genetic analysis. Criminology 49:923–954.
Heeringa SG, Wagner J, Torres M, Duan N, Adams T, Berglund P (2004) Sample designs and sampling methods for the Collaborative Psychiatric Epidemiology Studies (CPES). Int J Meth Psych Res 13:221–240
Kessler RC, Berglund P, Chiu WT et al (2004) The US National Comorbidity Survey Replication (NCS-R): design and field procedures. Int J Meth Psych Res 13:69–92
Jackson JS, Torres M, Caldwell CH et al (2004) The National Survey of American Life: A study of racial, ethnic and cultural influences on mental disorders and mental health. Int J Meth Psych Res 13:196–207
Alegria M, Takeuchi D, Canino G et al (2004) Considering context, place and culture: the National Latino and Asian American Study. Int J Meth Psych Res 13:208–220
World Health Organization (1992) The ICD-10 classification of mental and behavioural disorders: Clinical descriptions and diagnostic guidelines. World Health Organization, Geneva
World Health Organization (1990) Composite International Diagnostic Interview (CIDI). World Health Organization, Geneva
Silberg JL, Rutter M, Eaves L (2001) Genetic and environmental influences on the temporal association between earlier anxiety and later depression in girls. Psych Med 49:1040–1049.
United States Census Bureau (2004) Current population survey: Subject definitions. http://www.census.gov/programs-surveys/cps.html. Accessed 29 Mar 2016
SAS Institute Inc (2000) SAS (Version 9.4) [Software]. SAS Institute, Cary
Robins LN (1966) Deviant children grown up: A sociological and psychiatric study of sociopathic personality. Williams & Wilkins, Baltimore
Robins L (1978) Sturdy childhood predictors of adult antisocial behavior: Replications from longitudinal studies. Psychol Med 8:295–311
Moffitt TE (2006) Life-course persistent versus adolescence-limited antisocial behavior. In: Cicchetti D, Cohen DJ (eds) Developmental psychopathology, 2nd edition, vol 3: Risk, disorder, and adaptation. Wiley, New York, pp 570–598
Rutter M, Moffitt TE, Caspi A (2006) Gene-environment interplay and psychopathology: multiple varieties but real effects. J Child Psychol Pych 47:226–261
Henry B, Moffitt TE, Caspi A, Langley J, Silva PA (1994) On the “remembrance of things past”: a longitudinal evaluation of the retrospective method. Psychol Assess 6:92–101
Eppright TD, Kashani JH, Robison BD, Reid JC (1993) Comorbidity of conduct disorder and personality disorders in an incarcerated juvenile population. Am J Psychiat 150:1233–1236
Black DW, Gunter T, Loveless P et al (2010) Antisocial personality disorder in incarcerated offenders: Psychiatric comorbidity and quality of life. Ann Clin Psychiat 22:113–120
Acknowledgements
AAM, RRN, and BM are supported by the National Institute of Mental Health (MH020030, MH101518, and MH093642, respectively). JLS is supported by the National Center for Advancing Translational Science (TR000058). The National Comorbidity Survey Replication is sponsored by the National Institute of Mental Health (MH60220), the National Institute of Drug Abuse, the Substance Abuse and Mental Health Services Administration, the Robert Wood Johnson Foundation (044708), and the John W. Alden Trust. The National Survey of American Life is sponsored by the National Institute of Mental Health (MH57716). The National Latino and Asian American Survey is sponsored by the National Institute of Mental Health (MH62209), the Substance Abuse and Mental Health Services Administration Center for Mental Health Services, and the Office of Behavioral and Social Sciences Research. The sponsors had no role in the design, interpretation, analysis, or presentation of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Moore, A.A., Silberg, J.L., Roberson-Nay, R. et al. Life course persistent and adolescence limited conduct disorder in a nationally representative US sample: prevalence, predictors, and outcomes. Soc Psychiatry Psychiatr Epidemiol 52, 435–443 (2017). https://doi.org/10.1007/s00127-017-1337-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-017-1337-5