Abstract
Purpose
Several studies have confirmed that maltreatment and abuse in childhood are related to conduct problems. Less is known about such relationships with concurrent adversities in adolescence and, also, when compared with other severe adversities and possible multiple additive effects.
Methods
The study encompassed a community population of 4881 adolescents 15–16 years of age 50.1 % boys and 49.9 % girls. Youth with and without conduct problem scores within the deviant range on the Strength and Difficulties Questionnaire (SDQ) was compared on 12 concurrent adversities.
Results
Based on self-reports, 4.4 % of the adolescents had conduct problem scores within the deviant range and more girls (5.1 %) than boys (3.7 %). In the deviant conduct problem group, 65.1 % had experienced two or more concurrent adversities compared with 26.3 % of youths in the non-deviant group (OR 5.23, 95 % CI 3.91–7.01). Likewise, the deviant conduct problem group was from 1.71 to 8.43 times more at the risk of experiencing the different adversities. Parental mental health problems and experiences of violence were multivariately strongest associated with conduct problem scores within the deviant range on the SDQ. A strong multiple additive relationship with adversities was found.
Conclusions
Two-thirds of youth with SDQ conduct problem scores within the deviant range reported two or more concurrent adversities. Clinicians should seek information about kinds and amount of possible traumatic adversities in youth with conduct problems and offer evidence based treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Early adversities are common and have a strong co-occurrence. Several studies have found strong associations between adversities and adolescent psychiatric disorders. In a nationally representative, US study adversities were associated with more than one-fourth of all onsets of adolescent psychiatric disorders, and were found to be the strongest predictor of behavior disorders [1]. Similarly, Affi et al. [2] found maltreatment primarily to be associated with conduct disorder. Conduct problems constitute a considerable share of mental health problems among children and adolescents [3, 4]. In 2009–2010, conduct problems represented 12.4 % of all referrals to outpatient child and adolescent psychiatric services in Norway [5]. In a representative study from these services, more than half (60.2 %) of all youth patients reported sexual and physical abuse and neglect [6]. In a longitudinal study of the associations of sexual and physical abuse and neglect, official registered physical abuse cases were strongest related to a pattern of antisocial and impulsive behavior [7]. Mersky and Reynolds [8] found significant relationships between maltreatment and violent juvenile delinquency as well as lifetime violent arrests. Furthermore, the significance of a developmental course of influences has been discussed. Thornberry et al. [9] reported the outcome of childhood-limited maltreatment to be related to internalizing problems, whereas adolescent maltreatment had a stronger and more pervasive influence on later adjustment, and, with a broader range of outcomes as violence, a diversity of conflicts with the judicial system and addiction problems. Likewise, Kaplow and Widom [10] found later onset of maltreatment to be predictive of more behavioral problems in adulthood.
In a summary of review findings, Gilbert et al. [11] concluded that retrospective as well as prospective studies documented strong relationships between maltreatment and child and adolescent behavior problems as well as PTSD and criminal behaviors.
Traditionally, researchers have focused on single or just a few adversities, such as abuse and neglect, and their associations with mental health disorders [12–14]. However, according to Kessler et al. [15], results of single-adversity single-disorder studies should not be used as evidence of unique effect of specific adversities on specific disorders. Mersky et al. [16] found cumulative adversities to be associated with cumulative effects of poor health-related outcomes. Consistent evidence suggests a cumulative effect of different types of maltreatment on later behavior problems [17, 18]. In addition, high rates of comorbidity complicate the picture. More than half of referred youth with behavior disorders are found to have another psychiatric disorder [19].
The relationship between social factors and conduct problems is well known. Less than a half of children with conduct disorders live with married parents. Equally, they tend to live in poorer areas than other children do, and living in poverty makes it more than twice as likely to have a conduct disorder as living in non-poverty [3].
Many of the studies of adversities and conduct problems have investigated selected groups, such as maltreated children and youth in conflict with the judicial system, clients from the social and child protective services, and patients from pediatric wards or from child and adolescent psychiatry. Less is known about these relationships in an adolescent community population. In addition, most studies have focused on childhood adversities, while the association between concurrent adolescent adversities and adolescent conduct problems is less studied.
The aim of this study was to investigate the prevalence of critical conduct problems in a large adolescent community population and to explore the prevalence and amount of concurrent adversities among youth with critical conduct problems compared with youth without such problems. Furthermore, we wanted to look at the relationship between conduct problems and different kinds of concurrent adversities and to investigate the associations between critical conduct problems and multiple additive effects of adversities. Likewise, we intended to explore the influence of comorbidity. Finally, we wanted to examine the relationship with sociodemographic variables (gender, economy, divorce, family, peers, school, and service use).
Methods
Study design and sample
The Norwegian Arctic Adolescent Health Study (NAAHS) [20] was conducted among the tenth graders (15–16 years old) in all junior high schools in the three northernmost counties in Norway, in 2003–2005. All pupils (5877) in the tenth grade were invited to participate and those who agreed were asked to fill in two questionnaires during school hours. The data collection was conducted and funded by a joint collaboration between the Centre for Sami Health Research at the University of Tromsø and the Norwegian Institute of Public Health. The investigation was approved by the Regional Medical Ethical Committee, the Norwegian Data Inspectorate, and the school authorities.
A total number of 4881 of 5877 gave written consent to the use of data from the survey of whom 50.1 % were girls and 49.9 % were boys. The response rate was 83 %.
Mental health
The questionnaire in this study included the Strength and Difficulties Questionnaire (SDQ) as a measure of mental health [21]. SDQ has a parent, teacher, and youth version. In this study, only the SDQ self-report (SDQ-S) was used. The algorithms in SDQ generate problem scores for each of three broad-spectrum categories of problems—conduct problems, emotional symptoms, and hyperactivity/attention problems, as well as an impact score related to family, friends, learning situation, and leisure activities. Problem scores are grouped into four levels—“average”, “slightly raised”, “high”, or “very high” [22]. Deviant SDQ-S scores are reasonably consistent between Norway and the United Kingdom [23]. SDQ has proven suited for the registration of conduct problems [24–26]. Multi-informant SDQ scores above the 90th percentile predicts a clearly increased likelihood (OR 6.2) for the presence of independent diagnosed mental disorders [27]. Goodman et al. [22] reported that “very high” SDQ symptom scores predicted 81–91 % of children who had a defined clinical diagnosis with more positives than negatives, i.e., SDQ categories were overinclusive. Mathai et al. [25] found the sensitivity to be 93 % for ADHD (ICD-10), 81 % for emotional disorders and 100 % for conduct disorders when multi-informant SDQ was “high/very high” with combined symptom and impact scores. A review of Norwegian research on SDQ Kornør and Heyerdahl [23] concluded that the Norwegian version of SDQ-S was suitable for use in research. Diagnostic predictions from questionnaire data are likely to be more accurate if they draw both on impact and symptom scores, whereas both DSM-IV and the research version of ICD-10 define most of the common child and adolescent psychiatric disorders in terms of impact as well as symptoms [22]. In this study, symptom scores “very high” (above the 90th percentile—scores within the deviant range) combined with a “very high” impact score (above the 90th percentile) were used to define a conduct problem group with scores within the deviant range (deviant CP group) (4.4 %; n = 209). Likewise, the estimation of degree of comorbidity was based on SDQ deviant emotional problem and SDQ deviant hyperactivity/attention problem scores combined with impact scores within the deviant range. The control group in this study (n = 4524) included everyone who was not within the deviant conduct problem group (non-deviant CP group).
Concurrent adversities
Questions about 12 adversities were selected in line with the “Stressful life events” scheme from a UK study of mental health among children and adolescents [3] and the “Registration of trauma experiences in children” scheme (KATE-B) from the Norwegian Centre for Violence and Traumatic Stress Studies [28]. In addition, a question about “Parents with addiction problems” was used.
The 12 adversities were assessed through the following questions: “Have you during the past 12 months experienced”: “Sexual abuse”, “Serious illness or injury yourself”, “Serious illness or injury in someone who is close to you”—(“Yes”, “No”). Parental problems were registered through the question: ““Have you during the past 12 months had any of these problems”: “Mental health problems in parents/caretaker”,” Addiction problems in parents/caretaker (“No, never,” “Yes, sometimes,” “Several times,” “Very often”). Those who reported at least “Yes, sometimes” were defined to have a parent with mental health or addiction problems. Violence was surveyed through the question “Have you been a victim of violence (hit, kicked or similar) during the last 12 months”: “Yes, just by youth”, “Yes, just by adults”, “Yes, by both youths and adults”. Suicide was recorded through the question: “Do you know someone who has taken his own life?” “If yes”, was it (insert one or more marks)”: “Close family”; “Relatives”; “Someone in the neighborhood” (merged into one variable), “Pal”; “Boy/girlfriend”; “Fellow student” (merged into one variable). Bullying was registered through the question: “Have you during the past 12 months experienced bullying on your way to or from school?” (“Never”, “Sometimes”, “About once a week,” “Several times a week”). Those who reported at least “About once a week” were defined to have been bullied. Hospitalization was registered through the question: “Have you during the past 12 months ever used” (mentioned here several healthcare services) (“Never”, “1–3 times”, “4 times or more”). Those who reported at least “1–3 times” were registered as hospitalized.
Demographics, family, and school
Parental involvement was measured by a four-item version of the Parental Involvement Scale (α = 0.78) [29] based on the questions: “My parents know where I am and what I do in the weekend,” “My parents know where I am and what I do on weekdays,” “My parents know who I spend my leisure time with”, “My parents like the friends I spend time with”. Parental support (α = 0.88) was measured by the following five statements: “I feel attached to my family,” My family takes me seriously”, “My family values my opinion”, “I mean a lot to my family”, and “I can count on my family when I need help.”
Peer support (α = 0.84) was measured by the following four statements: “I feel closely attached to my friends,” “My friends value my opinions,” “I can help/support my friends,” and “I can count on my friends when I need help”. Parental involvement and parental and peer support were all measured by a four point Likert scale from “completely agree” (1) to “completely disagree” (4).
School-related stress (α = 0.66) was measured by the following experiences: “Have you ever experienced any of the following:” “Heavy work pressure at school,” “Heavy pressure from others to succeed/do well at school,” “Find it very difficult to concentrate in class” and “Find it very difficult to understand the teacher when he/she is teaching?” Responses were measured on a three-point Likert scale from “no” (1) to “yes, often” (3).
Family economy was surveyed through the question: “I think our family compared with others in Norway, has”: “Poor economy”, “Medium economy”, “Good economy”, “Very good economy.” Those who reported “Poor economy” were recorded to have financial problems. Service use was surveyed through the question: “Have you during the past 12 months ever used: “School health services”; “Psychologist or psychiatrist (private or outpatient).” Those who reported at least “1–3 times” were registered as users of respectively school health and mental health specialist services.
Statistical analysis
The statistics program SPSS (Statistical Package for Social Sciences, version 21) was used for statistical analyses. Differences between the deviant CP group and the non-deviant CP group were analyzed with t test and odds ratio Chi-square test. To test for multivariate associations between deviant CPs and the 12 adversity items, data were entered into a logistic regression with deviant CPs as dependent variable. Adversity items correlated from −0.06 to 0.15 (except for 0.31 between the variables “Self serious illness/injury” and “Hospitalization”), indicating that multicollinearity was not a threat. Cohen’s d was used as a measure of effect size. A simple linear regression was calculated to predict CP scores based on the number of current adversities. In addition, conduct problems were analyzed categorically according to the 90th percentile cutoff related to each additional adversity.
Results
Totally, in the entire youth population boys had higher conduct problem symptom scores than girls measured with the SDQ, mean score = 2.23 vs. 2.01, t (4822) = 4.98, p < 0.001, but, totally, girls had higher impact scores, mean score = 0.66 vs. 0.33, t (4740) = 9.12, p < 0.001.
The deviant CP group (n = 209) accounted for 4.4 % of the adolescent population with a rate of 3.7 % among boys (n = 87) and 5.1 % among girls (n = 122) (OR 1.40, 95 % CI 1.06–1.86, p < 0.05). More than half of the youths with deviant CP scores (57.9 %) also had deviant hyperactivity/inattention problem scores vs. 2 % of adolescents in the non-deviant CP group (OR 50.90, 95 % CI 36.61–70.76, p < 0.001). Half of the deviant CP group (51.7 %) also had deviant SDQ emotional problem scores vs. 2.3 % of adolescents in the non-deviant CP group (OR 23.86, 95 % CI 17.55–32.44, p < 0.001).
Demographics, family, and school
One-third (35.4 %) of adolescents with deviant SDQ CP scores reported that their parents were divorced or separated compared with 27 % of youth with non-deviant CP scores (OR 1.48, 95 % CI 1.11–1.99, p < 0.01), and 7.8 % stated that their family was poor compared with 3.2 % of the adolescents with non-deviant CP scores (OR 2.51, 95 % CI 1.47–4.29, p < 0.01). Adolescents with deviant CP scores on the SDQ reported more parental and peer support than those with non-deviant CP scores, but they reported less parental involvement than youth with non-deviant CP scores (Table 1). Furthermore, they experienced more school-related stress (Table 1).
One-third (36.2 %) with deviant CP scores reported contact with the school health services the last year compared with 23.6 % of youth with non-deviant CP scores (OR 1.84, 95 % CI 1.38–2.47, p < 0.001), while 24.2 % had been in contact with the specialist mental health services (psychologist or psychiatrist) compared with 4.8 % of youth with non-deviant CP scores (OR 6.31, 95 % CI 4.46–8.93, p < 0.001).
Concurrent adversities
A large effect size was found with respect to differences in the number of adversities. The deviant CP group reported in average more than twice as many adversities as the non-deviant CP group, mean score = 2.22 vs. 1.01, t (4731) = 15.20, p < 0.001, and Cohen’s d = 1.08.
Two-thirds of the adolescents (65.1 %) with SDQ deviant CP scores reported two or more adversities compared with 26.3 % of adolescents with non-deviant CP scores (OR 5.23, 95 % CI 3.91–7.01, p < 0.001). Likewise, two-thirds of the adolescents (67.8 %) with SDQ deviant CP scores and comorbid deviant SDQ hyperactivity/inattention scores had experienced two or more adversities vs. 26.9 % of adolescents with such non-deviant scores (OR 5.71, 95 % CI 3.88–8.40, p < 0.001). Similarly, more than twice as many youths (57.8 %) with deviant CP scores and comorbid deviant emotional problem scores had experienced two or more adversities compared with 25.2 % of adolescents with such non-deviant scores (OR 4.07, 95 % CI 3.30–5.02, p < 0.001).
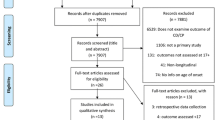
All 12 adversities occurred more frequently among adolescents with deviant CP scores compared with those with non-deviant scores (Fig. 1). Almost half of youth with deviant CP scores reported severe illness or injury in a closely related person, while a third reported suicide in the family, among relatives, or in the neighborhood.
Significant gender differences were found in the deviant CP group in three of the 12 adversities. Girls more often reported severe illness or injuries in a closely related person (OR 2.24, 95 % CI 1.27–3.96, p < 0.01) and sexual abuse (OR 3.16, 95 % CI 1.23–8.14, p < 0.05) Boys more often had experienced violence from other youths (OR 2.53, 95 % CI 1.41–4.55, p < 0.01). However, no significant gender differences were found related to the total number of adversities.
Deviant CP scores were significantly correlated with all 12 concurrent adversities (Table 2), and the risk of such events was from 1.7 to 8.4 times greater for adolescents in the deviant CP group than for those in the non-deviant CP group. The greatest risk was related to parents with mental or addiction problems and experiences of violence.
A multivariate linear regression analysis of the 12 adversities (Table 3) identified experiences of violence and parental mental health problems as adversities that increased the risk of SDQ deviant CP scores mostly.
A linear relationship between the number of adversities was reported, and severity of CP scores was investigated. A significant regression equation was found (F (1.48) = 664.95, p < 0.001), with an R 2 of 0.12. Adolescents’ predicted CP scores are equal to 1.89 + 0.67 (adversities) when adversities are measured in numbers. Adolescents’ CP scores increased 0.67 for each number of adversities. When conduct problems were analyzed categorically according to the 90th percentile cutoff, for each additional adversity, there was an almost twofold increased odds of such deviant range conduct problems, i.e., OR = 1.89, 95 % CI 1.72–2.08, p < 0.001. There was no non-linear effect in this relationship as indicated by a non-significant multiplicative term of adversities, OR = 0.96, 95 % CI 0.91–1.01, p = 0.08.
Discussion
The purpose of this community study was to investigate the amount and burden of concurrent adversities among adolescents with critical conduct problems compared with adolescents without such problems. Two-thirds of the youth with deviant CP scores on the SDQ had experienced two or more concurrent adversities. Parental mental health problems and experiences of violence were multivariately strongest related to deviant CP scores.
The group with deviant CP scores on the SDQ accounted for 4.4 % of the adolescent population, but, surprisingly, there were more girls than boys (5.1 vs. 3.7 %) in this group. Our findings suggest that girls with conduct problems to a larger extent than boys experience impairment related to family, school, and social functioning. Other studies as well have registered higher levels of stress and impairment in girls than in boys on SDQ self-reports [30, 31]. There may be less tolerance of conduct problems among girls with the subsequent negative social reactions. However, whereas the general literature indicates a higher prevalence of conduct disorder in boys, Kaplan et al. [32] found that physically abused girls were almost as likely as physically abused boys to receive a conduct disorder diagnosis. In the present study, the prevalence of deviant conduct problems was somewhat lower than the prevalence of conduct disorder diagnoses in a British mental health study of children and adolescents, where more boys (8.8 %) than girls (5.1 %) had such diagnoses [3]. In a literature review, Loeber et al. [33] estimated the conduct disorder gender difference to diminish from childhood to adolescence from a male dominance of 4:1 in childhood to 2:1 in adolescence.
More than half of the youth with a deviant CP score on the SDQ also had comorbid emotional problem and hyperactivity/inattention scores within the deviant range. However, Green et al. [3] registered a considerably lower comorbidity among British youth with conduct disorders, though Greene et al. [19] found more than half of referred youth with conduct disorders to have comorbid ADHD or major depression disorder.
Concurrent adversities
The deviant CP group reported in average more than twice as many concurrent adversities as the non-deviant CP group. Two-thirds of the youth with deviant CP scores on the SDQ had experienced two or more adversities compared with only one-fourth of youth without such scores. All 12 adversities were reported significantly more often by youth with deviant CP scores. Comorbidity with deviant hyperactivity/inattention scores or with deviant emotional scores made just a little increase in the share of those who had experienced two or more adversities in this study.
The findings that youth with deviant CP scores had experienced more adversities than peers with non-deviant scores are in line with reports from Green et al. [3], where children with conduct disorders were twice as likely as other children (50 vs. 25 %) to have experienced two or more stressful life events. Sexual abuse, suicide by a pal, girl/boyfriend, or fellow student, and the youth him/herself had been seriously ill or injured were reported more than twice as often by youths in the deviant CP group. All three adversities of violence gave a risk from 3.6 to 6.8 times of deviant CP scores. Many studies have identified physical abuse as a critical factor in the development of conduct disorders [2, 7, 32, 34]. However, reverse causation may be a particular problem for behavior disorders. Youth with conduct problems may often be impulsive and aggressive themselves, and thus, more easily could be involved in or exposed to violence from others. Disruptive behaviors are also known to increase the likelihood of harsh parenting [35]. Loeber et al. [33] found physical fighting to be the best predictor of onset of conduct disorders in boys, while physical abuse has been found to be most strongly related to youth violence in girls [36].
Significant gender differences were found for three of the adversities. Girls with deviant CP scores more often reported sexually abuse (p < 0.05), and had a close person who were seriously ill or injured (p < 0.01). Boys with deviant CP scores more often reported violence from other youths (p < 0.01). However, no significant gender differences were related to the total number of adversities.
When the deviant CP group was compared with the non-deviant CP group on the total number of adversities, the effect size of the difference was large (Cohen’s d = 1.08). We thus found a strong cumulative effect of adversities. Likewise, we found a significant linear relationship between the number of adversities reported and severity of CP scores. Each adversity increased the CP scores with more than a half point (0.67). There was an almost twofold increased risk of deviant range CP scores for each additional adversity.
However, the question of the cumulative adversity effect has been disputed. On one hand, Turner et al. [37] stated that focus on particular kinds of victimization was likely to underestimate the full burden of victimization that children and youth experience. Likewise, Mersky et al. [16] also found cumulative adversity to be associated with cumulative effects of poor health-related outcomes. On the other hand, Schilling et al. [38] reported higher cumulative adversity to be related to unduly poorer mental health; because of the severity of the adversities, they were exposed to, not the cumulative number of different kinds of adversities experienced. Thus, a critical issue may be the traumatic impact of adversities. In the present study, we have no knowledge of the frequency or severity of the current adversities or of possible earlier adversities. However, in the multivariate analysis, we found a strong relationship between the adversities of violence, parental mental health problems, and deviant CP scores. Many studies have documented relationships between maltreatment and conduct problems and delinquency [2, 17, 34, 39, 40]. Kaplow and Widom [10] found later onset of maltreatment to be connected with more conduct problems in adulthood. Parental mental health problems were registered somewhat more often among British children with conduct disorders [3] compared with the deviant CP group in the present study (17 vs. 13 %).
McLaughlin et al. [1] concluded from a US national study of trauma exposed adolescents that interventions designed to prevent PTSD in youths should be targeted at victims of violence. The impact of major adversities seems to persist well into adulthood [41].
Social factors
Several studies have documented associations between conduct disorder diagnoses and social factors, such as income, education, and single parent status [3, 42]. Likewise, in the present study, we found significant associations between deviant CP scores and divorce (p < 0.01) and poverty (p < 0.01). The relationship between poverty and conduct disorders is well known, but the question of a possible causal link has been unanswered. However, Costello et al. [43] found support for a hypothesis of social causation for conduct and oppositional disorder, but not for anxiety or depression.
In the present study, youths in the deviant CP group reported more support from family and peers compared with youths without deviant CP scores, but, also, less parental involvement in monitoring the youth. These reports of more family support and less parental involvement may seem contradictive. One interpretation could be that a parental “laissez-faire” attitude with few conflicts at home may be misinterpreted by the youth as family support. On the other side, mothers of referred youth with oppositional defiant disorder report high levels of family conflict [19]. In addition to family, peers play a major role in the development of self-concept, social roles, and norms in the youth’s lives. However, not all peer relationships are positive. Youth with conduct problems tend to have friends who may be involved in negative and disruptive activities. Parents of children with conduct disorders are more likely than other parents to disapprove their child’s friends who often get into trouble [3]. In the present study, when youths in the deviant CP group reported more support from peers than those outside the deviant group, this support could as well contribute to maintenance of disruptive behaviors.
Youths with deviant CP scores also experienced more school-related stress than those without such scores. This may be related to a high comorbidity between deviant CP scores and deviant hyperactivity/inattention scores when two of the four questions on the School-related stress scale were associated with inattention problems. In addition, inattention problems may as well be indicators of traumatic experiences when concentration problems are part of the diagnostic criteria of PTSD. It is well known that youth with conduct problems struggle at school. About half of children with conduct disorders have been considered by their teachers to have special educational needs [3]. Tramontina et al. [44] found significantly more conduct disorders among school dropouts than among controls in the school.
In this study, more than one-third of adolescents with deviant CP scores reported contact with the school health services compared with a little less than one-fourth of youth without such scores. A quarter of the youth with SDQ deviant CP scores had been in contact with the specialist mental health services (psychologist or psychiatrist) last year vs. 4.8 % of youth without such scores. British youth with conduct disorders was found to have about the same rates of contact with helping services [3].
Strengths and weaknesses of the study
In this study of a large youth population from Northern Norway, there are no diagnoses. Definitions of deviant conduct problems are only based on SDQ scores from self-reports of young people themselves. In addition, SDQ categories are shown to be overinclusive with a risk of “false positives” [27]. It is important to affirm that CP scores within the deviant range of SDQ cannot be equated with an ODD/CD diagnosis, but only can be considered as indicative. Likewise, the 12 selected concurrent adversities are only partially comparable events compared with Green et al. [3] and KATE-B [28]. In the present study, the concurrent adversities asked for covered a limited period of last 12 months. Comparisons are thus only indicative. Similarly, both the SDQ and reports of concurrent adversities were obtained from the adolescents at the same time. Thus, the dependent and independent variables could share a reporting bias.
The strength of the study is that it includes a representative sample of an entire youth population (n = 5877) with a significant number of adolescents with CP scores within the deviant range of the SDQ (n = 209). Likewise, the memory of the last year’s adversities was likely to be fresh and less at the risk of memory errors than a backward memory span of several years. Equally, the self-reports were anonymous. This is important when disclosure of adversities and negative self-descriptions on the SDQ may be very sensitive. Research shows that sensitive information more easily is reported anonymously than by a clinical interview [45, 46]. The present study is a cross-sectional study from which one can say nothing about causality or predictability.
Conclusions
Two-thirds of youth with CP scores within the deviant range on the SDQ reported two or more concurrent adversities. Experiences of physical violence and parental mental health problems were multivariately strongest related to deviant CP scores. In addition, a strong multiple additive effect of adversities was found. We suggest that trauma contributes to the development and persistence of conduct problems, and thus should be addressed. Clinicians should seek information about possible traumatic experiences in children and youth with critical conduct problems. Such information may be of vital importance diagnostically as well as therapeutically.
References
McLaughlin KA, Greif Green J, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC (2012) Childhood adversities and first onset of psychiatric disorders in a national sample of US adolescents. Arch Gen Psychiatry 69:1151–1160
Afifi TO, McMillan KA, Asmundson GJ, Pietrzak RH, Sareen J (2011) An examination of the relation between conduct disorder, childhood and adulthood traumatic events, and posttraumatic stress disorder in a nationally representative sample. J Psychiatr Res 45:1564–1572
Green H, McGinnity A, Meltzer H, Ford T, Goodman R (2005) Mental health of children and young people in Great Britain, 2004. Palgrave, Macmillan, Houndmills, Basingstoke, Hampshire RG21 6XS and 175 Fifth Avenue, New York
Nock MK, Kazdin AE, Hiripi E, Kessler RC (2006) Prevalence, subtypes, and correlates of DSM-IV conduct disorder in the National Comorbidity Survey Replication. Psychol Med 36:699–710
Sitter M (2012) Barn og unge i det psykiske helsevernet 2009–2010—kjennetegn og behandlingstid for utvalgte pasientgrupper. Helsedirektoratet, Oslo
Reigstad B, Jørgensen K, Wichstrøm L (2006) Diagnosed and self-reported childhood abuse in national and regional samples of child and adolescent psychiatric patients: prevalences and correlates. Nord J Psychiatry 60:58–66
Cohen P, Brown J, Smaile E (2001) Child abuse and neglect and the development of mental disorders in the general population. Dev Psychopathol 13:981–999
Mersky JP, Reynolds AJ (2007) Child maltreatment and violent delinquency: disentangling main effects and subgroup effects. Child Maltreat 12:246–258
Thornberry TP, Henry KL, Ireland TO, Smith CA (2010) The causal impact of childhood-limited maltreatment and adolescent maltreatment on early adult adjustment. J Adolesc Health 46:359–365
Kaplow JB, Widom CS (2007) Age of onset of child maltreatment predicts long-term mental health outcomes. J Abnorm Psychol 116:176–187
Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, Janson S (2009) Burden and consequences of child maltreatment in high-income countries. Lancet 373:68–81
Mullen PE, Martin JL, Anderson JC, Romans SE, Herbison GP (1993) Childhood sexual abuse and mental health in adult life. Br J Psychiatry 163:721–732
Brown J, Cohen P, Johnson JG, Smailes EM (1999) Childhood abuse and neglect: specificity of effects on adolescent and young adult depression and suicidality. J Am Acad Child Adolesc Psychiatry 38:1490–1496
Putnam FW (2003) Ten-year research update review: child sexual abuse. J Am Acad Child Adolesc Psychiatry 42:269–278
Kessler RC, Davis CG, Kendler KS (1997) Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey. Psychol Med 27:1101–1119
Mersky JP, Topitzes J, Reynolds AJ (2013) Impacts of adverse childhood experiences on health, mental health, and substance use in early adulthood: a cohort study of an urban, minority sample in the US. Child Abuse Negl 37:917–925
Thornberry TP, Ireland TO, Smith CA (2001) The importance of timing: the varying impact of childhood and adolescent maltreatment on multiple problem outcomes. Dev Psychopathol 13:957–979
Appleyard K, Egeland B, van Dulmen MH, Sroufe LA (2005) When more is not better: the role of cumulative risk in child behavior outcomes. J Child Psychol Psychiatry 46:235–245
Greene RW, Biederman J, Zerwas S, Monuteaux MC, Goring JC, Faraone SV (2002) Psychiatric comorbidity, family dysfunction, and social impairment in referred youth with oppositional defiant disorder. Am J Psychiatry 159:1214–1224
The Norwegian Institute of Public Health (2013) Youth studies, Oslo. http://www.fhi.no/artikler/?id=105586. Accessed 12 Sept 2008
Goodman R, Ford T, Simmons H, Gatward R, Meltzer H (2000) Using the Strengths and Difficulties Questionnaire (SDQ) to screen for child psychiatric disorders in a community sample. Br J Psychiatry 177:534–539
Goodman R, Renfrew D, Mullick M (2000) Predicting type of psychiatric disorder from Strengths and Difficulties Questionnaire (SDQ) scores in child mental health clinics in London and Dhaka. Eur Child Adolesc Psychiatry 9:129–134
Kornør H, Heyerdahl S (2013) Måleegenskaper ved den norske versjonen av Strengths and Difficulties Questionnaire, selvrapport (SDQ-S). PsykTestBarn 2, Oslo
Goodman R, Scott S (1999) Comparing the Strengths and Difficulties Questionnaire and the child behavior checklist: is small beautiful? J Abnorm Child Psychol 27:17–24
Mathai J, Anderson P, Bourne A (2004) Comparing psychiatric diagnoses generated by the Strengths and Difficulties Questionnaire with diagnoses made by clinicians. Aust N Z J Psychiatry 38:639–643
Achenbach TM, Becker A, Dopfner M, Heiervang E, Roessner V, Steinhausen HC, Rothenberger A (2008) Multicultural assessment of child and adolescent psychopathology with ASEBA and SDQ instruments: research findings, applications, and future directions. J Child Psychol Psychiatry 49:251–275
Goodman R (2001) Psychometric properties of the Strengths and Difficulties Questionnaire. J Am Acad Child Adolesc Psychiatry 40:1337–1345
Myhre MC, Borchgrevink C, Sommerfeldt MB (2015) Oversikt over rutineguider og kartleggingsverktøy for avdekking av vold i nære relasjoner. Rapport 4, Oslo. ISBN 978-82-8122-087-4, ISSN 0809-9103. http://www.nkvts.no. Accessed June 2015
Alsaker FD, Olweus D (1991) A growth curve approach to the study of parental relations and depression in child hood. In: Paper presented at the Biannual meetings of the Society for Research in Child development, Seattle
Van Roy B, Grøholt B, Heyerdahl S, Clench-Aas J (2006) Self-reported strengths and difficulties in a large Norwegian population 10–19 years: age and gender specific results of the extended SDQ-questionnaire. Eur Child Adolesc Psychiatry 15:189–198
Wille N, Bettge S, Wittchen HU, Ravens-Sieberer U (2008) How impaired are children and adolescents by mental health problems? Results of the BELLA study. Eur Child Adolesc Psychiatry 17(Suppl 1):42–51
Kaplan SJ, Pelcovitz D, Salzinger S, Weiner M, Mandel FS, Lesser ML, Labruna VE (1998) Adolescent physical abuse: risk for adolescent psychiatric disorders. Am J Psychiatry 155:954–959
Loeber R, Burke JD, Lahey BB, Winters A, Zera M (2000) Oppositional defiant and conduct disorder: a review of the past 10 years, part I. J Am Acad Child Adolesc Psychiatry 39:1468–1484
McCabe KM, Lucchini SE, Hough RL, Yeh M, Hazen A (2005) The relation between violence exposure and conduct problems among adolescents: a prospective study. Am J Orthopsychiatry 75:575–584
Jaffee SR, Caspi A, Moffitt TE, Polo-Tomas M, Price TS, Taylor A (2004) The limits of child effects: evidence for genetically mediated child effects on corporal punishment but not on physical maltreatment. Dev Psychol 40:1047–1058
Maas C, Herrenkohl TI, Sousa C (2008) Review of research on child maltreatment and violence in youth. Trauma Violence Abuse 9:56–67
Turner HA, Finkelhor D, Ormrod R (2010) Poly-victimization in a national sample of children and youth. Am J Prev Med 38:323–330
Schilling EA, Aseltine RH, Gore S (2008) The impact of cumulative childhood adversity on young adult mental health: measures, models, and interpretations. Soc Sci Med 66:1140–1151
Smith CA, Ireland TO, Thornberry TP (2005) Adolescent maltreatment and its impact on young adult antisocial behavior. Child Abuse Negl 29:1099–1119
Topitzes J, Mersky JP, Reynolds AJ (2012) From child maltreatment to violent offending: an examination of mixed-gender and gender-specific models. J Interpers Violence 27:2322–2347
Schilling EA, Aseltine RH Jr, Gore S (2007) Adverse childhood experiences and mental health in young adults: a longitudinal survey. BMC Public Health 7:30
McLaughlin KA, Costello EJ, Leblanc W, Sampson NA, Kessler RC (2012) Socioeconomic status and adolescent mental disorders. Am J Public Health 102:1742–1750
Costello EJ, Compton SN, Keeler G, Angold A (2003) Relationships between poverty and psychopathology: a natural experiment. JAMA 290:2023–2029
Tramontina S, Martins S, Michalowski MB, Ketzer CR, Eizirik M, Biederman J, Rohde LA (2001) School dropout and conduct disorder in Brazilian elementary school students. Can J Psychiatry 46:941–947
Safer DJ (1997) Self-reported suicide attempts by adolescents. Ann Clin Psychiatry 9:263–269
Evans E, Hawton K, Rodham K, Deeks J (2005) The prevalence of suicidal phenomena in adolescents: a systematic review of population-based studies. Suicide Life Threat Behav 35:239–250
Acknowledgments
Lars Wichstrøm contributed to the analyses of the present data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of both authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Reigstad, B., Kvernmo, S. Concurrent adversities among adolescents with conduct problems: the NAAHS study. Soc Psychiatry Psychiatr Epidemiol 51, 1429–1438 (2016). https://doi.org/10.1007/s00127-016-1258-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-016-1258-8