Abstract
Aims/hypothesis
In type 1 diabetes, cardiovascular disease (CVD) and diabetic nephropathy progress in parallel, thereby potentiating the risk of premature death during their development. Since urinary liver-type fatty acid binding protein (L-FABP) predicts the progression of diabetic nephropathy, the aim of this study was to investigate whether urinary L-FABP also predicts cardiovascular outcomes and mortality.
Methods
We tested our hypothesis in a Finnish cohort of 2329 individuals with type 1 diabetes and a median follow-up of 14.1 years. The L-FABP to creatinine ratio was determined from baseline urine samples. The predictive value of urinary L-FABP was evaluated using Cox regression models, while its added predictive benefit for cardiovascular outcomes and mortality was evaluated using a panel of statistical indexes.
Results
Urinary L-FABP predicted incident stroke independently of traditional risk factors (HR 1.33 [95% CI 1.20, 1.49]) and after further adjustment for eGFR (HR 1.28 [95% CI 1.14, 1.44]) or AER (HR 1.24 [95% CI 1.06, 1.44]). In addition, it predicted mortality independently of traditional risk factors (HR 1.34 [95% CI 1.24, 1.45]), and after adjustment for eGFR (HR 1.29 [95% CI 1.18, 1.39]) or AER (HR 1.22 [95% CI 1.09, 1.36]). Urinary L-FABP was as good a predictor as eGFR or AER, and improved the AUC for both outcomes on top of traditional risk factors, with no reclassification benefit (integrated discrimination improvement/net reclassification improvement) for stroke or mortality when AER or eGFR were added to traditional risk factors. However, urinary L-FABP was not a predictor of other cardiovascular endpoints (coronary artery disease, peripheral vascular disease and overall CVD events) when adjusted for the AER.
Conclusions/interpretation
Urinary L-FABP is an independent predictor of stroke and mortality in individuals with type 1 diabetes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Individuals with type 1 diabetes have a higher risk of cardiovascular disease (CVD) compared with the general population [1, 2]. In addition, the risk of death from cardiovascular causes is already higher by early adulthood [3]. Furthermore, diabetic nephropathy increases the risk of CVD and mortality along with the progression of kidney damage [4, 5]. Diabetic nephropathy and CVD thus progress in parallel and share many common risk factors such as hypertension, dyslipidaemia, hyperglycaemia and smoking [6]. Therefore, the use of biomarkers to identify kidney and vascular dysfunction at an early stage would be an attractive approach to detecting these complications.
AER is the most widely used predictor of diabetic nephropathy, mortality and CVD [7]. Its predictive power derives from the fact that it reflects glomerular damage and generalised endothelial dysfunction [8, 9].
Similar to AER, urinary L-FABP reflects proximal tubular damage and was shown to be as good a predictor of diabetic nephropathy progression as AER [10]. L-FABP is a member of the FABP family of intracellular lipid chaperones that coordinate lipid responses in cells and are strongly linked to metabolic and inflammatory pathways [11, 12]. L-FABP expression is highly increased in cells exposed to NEFAs or hypoxia, where it promotes fatty acid metabolism and acts as a powerful endogenous antioxidant that mitigates the effects of hypoxia and high lipid levels [13, 14]. In tubular cells, L-FABP responds to NEFA overload and to decreased peritubular capillary blood flow [13, 15]. However, these pathological changes reflect more than just tubular injury because NEFA overload depends on the serum NEFA concentrations, while peritubular capillary blood flow is an expression of the general microcirculation and hypoxia. Thus, urinary L-FABP may represent a surrogate marker of general lipid metabolism, microvascular injury and chronic hypoxia [11, 15]. Although there is some suggestion that urinary L-FABP may be related to CVD in individuals with type 2 diabetes and related to mortality in type 1 diabetes, no study has extensively evaluated the role of urinary L-FABP as a predictor of CVD outcomes and mortality in type 1 diabetes [16,17,18,19]. Therefore, the aim of our study was to investigate the prognostic value and potential added clinical benefit of urinary L-FABP for prediction of the most important cardiovascular outcomes and mortality in individuals with type 1 diabetes.
Methods
Study participants
This study is part of the Finnish Diabetic Nephropathy Study (FinnDiane)—a nationwide cohort of individuals with type 1 diabetes followed prospectively at more than 80 centres. The FinnDiane protocol, described in detail elsewhere, was approved by the local ethics committees at all centres [20]. Individuals recruited to the study provided written informed consent in accordance with the revised Declaration of Helsinki. Those with a previous history of CVD (stroke, coronary artery disease [CAD] or peripheral vascular disease [PVD]) or baseline end-stage renal disease (ESRD) were excluded from the study.
Baseline data and sample collection
All relevant medical history and data on cardiovascular endpoints, drug treatment and diabetes complications were collected at enrolment using a standard questionnaire. Anthropometric characteristics and BP were recorded. Blood samples were drawn at baseline. Glycated HbA1c and the following biochemical measurements were measured in fresh serum samples: total cholesterol, HDL-cholesterol, triacylglycerol, creatinine and C-reactive protein. The LDL-cholesterol level was calculated using the Friedewald formula [20]. Based on serum creatinine values, eGFR was calculated using the Chronic Kidney Disease Epidemiology Collaboration formula [21]. AER levels were measured in 24 h urine collections. [10]. Additional blood and urine samples were collected at baseline in 1998 and stored at −20°C. In 2008, these additional urine samples were used for L-FABP measurements.
Assays
Common biochemical tests were performed using standard laboratory methods [20]. Urinary L-FABP was evaluated in single 24 h urine samples using an Elecsys Immuno-assay Kit (Roche Diagnostics, Mannheim, Germany), with a coefficient of variation of <7% and a recovery in serial measurements of ~100 ± 10% [10]. Urinary L-FABP concentrations were normalised to urinary creatinine concentrations.
Follow-up data and ascertainment of outcomes
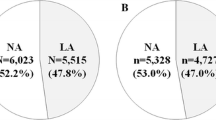
Participants were followed prospectively and information on cardiovascular outcomes and all-cause mortality were documented until the end of 2014 by linking the FinnDiane data with two high quality registries (the Finnish Hospital Discharge Registry and Finnish Cause of Death Registry), as previously described [22]. Cardiovascular outcomes were documented from the Hospital Discharge Registry using hospital admission, discharge diagnoses and treatment procedure data, based on ICD-8, ICD-9 (www.icd9data.com/2007/Volume1) and ICD-10 (www.who.int/classifications/icd/en/)., together with Nordic Classifications of Surgical Procedures (http://www.nordclass.se/ncsp_e.htm).
CAD was defined as a history of acute myocardial infarction (ICD8 or ICD9 code 410; ICD10 codes I21, I22) or of a coronary artery procedure (bypass grafting surgery or angioplasty). PVD was considered only when a limb amputation or peripheral artery procedure (bypass grafting surgery or angioplasty) was performed. Stroke (ischaemic or haemorrhagic) was considered if the corresponding ICD codes (ICD8 or ICD9 codes 430–434; ICD10 codes I60–I64) were documented in the Hospital Discharge Registry as a history of ischaemic, haemorrhagic or unspecified stroke. CVD events were defined as a composite outcome including all three endpoints (CAD, PVD and stroke). A full description of the cardiovascular outcomes used in the FinnDiane Study is presented elsewhere [23].
Statistical analysis
All continuous variables were tested for normal distribution. A generalised extreme Studentised deviate test (α = 0.05 and n outliers < 15) was used for outlier detection and exclusion. Normally distributed variables are presented as the mean ± SD, while non-normally distributed variables are presented as the median and interquartile range. Comparison between groups was performed using one-way ANOVA or the Kruskal–Wallis test, depending on the distribution of variables. Categorical variables are presented as percentage and compared using the χ 2 test.
Prediction of cardiovascular outcomes and mortality was performed using Cox proportional hazard models only in individuals with first-ever cardiovascular events. When required for the Cox analysis, variables were loge transformed. All HRs were calculated per 1 log e unit change in L-FABP concentration.
We first tested urinary L-FABP in a simple Cox analysis, without any adjustment; then we adjusted the Cox analysis with a model comprising well-known traditional predictors of cardiovascular risk (sex, age, diabetes duration, BMI, ever smoking, HDL-cholesterol, triacylglycerol, systolic BP, HbA1c and proliferative retinopathy). Next, eGFR and AER were sequentially included in these models to further test the independence of urinary L-FABP. The Cox model fit was assessed by cumulative Cox–Snell residuals to (−log) Kaplan–Meier estimates and the validity of the model assumption was tested by checking the normal distribution of the residuals, using the D’Agostino–Pearson test [22]. Colinearity was estimated using the variance inflation factor, tolerance and R values. Variance inflation factor values of <10, tolerance values of >0.5 and R values of <0.7 were considered acceptable.
The discrimination ability of urinary L-FABP was compared with those of eGFR or AER was tested using Harrell’s C-index. In the statistical analysis, we used the estat concordance package in STATA (version 13, StataCorp, College Station, TX, USA) for postestimation after Cox regression. AUCs were compared using the Delong method [24]. We first compared the receiver operating characteristic (ROC) curves of urinary L-FABP, eGFR and AER alone, and then compared the ROC curve of the model formed by urinary L-FABP with either AER or eGFR with that of L-FABP, AER or eGFR alone. In addition, we compared the ROC curves of urinary L-FABP, LDL-cholesterol, HbA1c and systolic BP.
The added predictive (reclassification) benefit obtained by adding urinary L-FABP to the traditional risk factor models plus eGFR, AER or both was assessed by calculating the net reclassification improvement (NRI) and the integrated discrimination improvement (IDI) using the NRI3 and IDI packages implemented for STATA [25, 26]. For NRI calculation, we used three relevant thresholds (5%, 10% and 20%) for cardiovascular risk decision-making [27]. The same cut-offs were used also for the survival analysis. In addition, we calculated NRI3 and IDI generalised for survival data using the nricens and survIDINRI packages implemented in RStudio (version 1.0.136, Boston, MA, USA).
As we tested urinary L-FABP for predicting five outcomes, Bonferroni correction was applied and a p value for outcome prediction of <0.01 was considered significant (αBonferroni = α/m = 0.05/5, where m = the number of tested hypotheses). For all other tests, a p value of <0.05 was considered statistically significant.
Results
Cohort characteristics
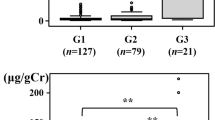
The clinical characteristics of all participants are presented in Table 1 and in electronic supplementary material (ESM) Tables 1–5. At baseline, there were 2329 individuals with type 1 diabetes without ESRD or a previous cardiovascular event for whom data on urinary L-FABP concentrations were available. The median follow-up time was 14.1 years (interquartile range 12.5–16.0). The percentages of incident macrovascular complications and mortality increased with the urinary L-FABP quartile at baseline.
Urinary L-FABP and incident CAD events
During follow-up, 240 participants developed CAD, and urinary L-FABP concentrations were higher in those who had a CAD event. Urinary L-FABP predicted incident CAD events in the unadjusted analysis and also when adjusted for traditional risk factors or eGFR, but not when it further adjusted for AER (Table 2).
Urinary L-FABP and incident PVD
Over the study duration, 116 participants developed PVD and L-FABP concentrations were higher in those who experienced a PVD event. Urinary L-FABP predicted an incident PVD event in the unadjusted analysis as well as after adjustment for traditional risk factors or eGFR, but after adjustment for AER (Table 2).
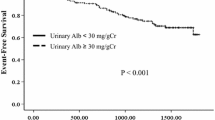
Urinary L-FABP and incident stroke
During follow-up, 133 participants suffered a stroke; urinary L-FABP was higher in individuals who suffered a stroke than in those who did not. Urinary L-FABP independently predicted stroke in the unadjusted analysis, as well as after adjustment for traditional risk factors and after further adjustment for eGFR and AER (Table 2). There was no difference between the AUC for L-FABP (AUCL-FABP) and the AUCeGFR (p = 0.94) or AUCAER (p = 0.96), but the AUC for L-FABP was superior to other well-known cardiovascular predictors for predicting incident stroke (ESM Table 6 and ESM Table 7). Notably, when urinary L-FABP was added to the model comprising the traditional risk factors, the increment in AUC was similar to that for AER but significantly different from that for the traditional risk factors (p = 0.04). However, there was no increment in the AUC compared with models comprising the AER or eGFR (Table 3). When the NRI and IDI generalised for survival data were calculated, the largest reclassification benefit on top of traditional risk factors was seen at 5 years (NRI3-S5 = 14.6%). However, there was no predictive benefit of adding urinary L-FABP on top of AER and/or eGFR (Table 4).
Urinary L-FABP and incident CVD
Throughout the study, a total of 343 individuals had an incident CVD event, and L-FABP concentrations were higher in those who experienced a CVD event. Urinary L-FABP was a predictor of incident CVD events in a univariate analysis and after adjustment for the traditional risk factors or eGFR, but not after adjustment for AER (p < 0.05 but not p < 0.01, as required by Bonferroni correction).
Urinary L-FABP and mortality
During follow-up, there were 269 deaths of any cause. In deceased individuals, the baseline L-FABP concentration was higher compared with survivors. Urinary L-FABP was an independent predictor of death in the unadjusted analysis and when adjusted for traditional risk factors as well as after adjustment for eGFR and AER (Table 2). The AUCL-FABP was not different from the AUCeGFR (p = 0.90) or the AUCAER (p = 0.72). After addition of urinary L-FABP to the model comprising traditional risk factors, the increment in AUC was significant (p = 0.001) and was similar to that for AER (p = 0.76; Table 3). Notably, the AUC for urinary L-FABP was again much better than that for other traditional cardiovascular risk factors (ESM Table 6 and ESM Table 8). When the NRI and IDI generalised for survival data were calculated, there was no added predictive benefit on top of AER or eGFR (Table 4).
Discussion
In this prospective study comprising 2329 individuals, urinary L-FABP was an independent predictor only for incident stroke and mortality. For these outcomes, urinary L-FABP was as good a predictor as AER or eGFR and improved the AUC for both outcomes on top of traditional risk factors, without a reclassification benefit (IDI/NRI) for stroke when AER or eGFR were added to traditional risk factors. However, urinary L-FABP was not an independent predictor of the other tested cardiovascular endpoints (CAD, PVD and overall CVD events) when adjusted for AER, while AER was a predictor for all outcomes except stroke, independently of L-FABP.
The novel finding that urinary L-FABP is an independent predictor of stroke is interesting because until now only a marginal association of a SNP in the FABP1 gene with stroke has been reported in a single study [28]. In our study, urinary L-FABP predicted stroke independently not only of known risk factors such as age, sex, BMI, diabetes duration, systolic BP, triacylglycerol, HDL-cholesterol, glycaemic control and proliferative diabetic retinopathy but also of eGFR and AER. The potential clinical value of this finding is emphasised by the finding that urinary L-FABP was as good a predictor of stroke as eGFR or AER and better than the traditional risk factors in the ROC curve analysis. When NRI and IDI were calculated, urinary L-FABP did not have an added reclassification benefit to the long-term prediction of stroke on top of eGFR and AER. However, when added to the model of traditional risk factors, urinary L-FABP correctly reclassified 17.9% of participants (compared with 6% or 10% provided by AER or eGFR) when NRI was calculated.
Another important finding was that urinary L-FABP is an independent predictor of death. This was previously suggested by another study that was unfortunately not sufficiently powered to adjust for other risk factors, thus leaving the question open [18]. In our study, urinary L-FABP predicted mortality independently of the most important traditional risk factors and after additional adjustment for eGFR and AER. As in the case of stroke, urinary L-FABP was as good as eGFR or AER in predicting death. When added to the traditional risk factors, urinary L-FABP correctly reclassified about 7.5% of participants compared with 8.6% and 1.4% for eGFR and AER. Since urinary L-FABP predicted only stroke and mortality but not CAD, PVD or total CVD (i.e. two out of five outcomes tested), one can argue that these findings are just a statistical anomaly. However, the most rigorous statistical testing with Bonferroni correction was used for all outcomes. In addition, the results were obtained using the most extended statistical model for adjustment that contained all well-known risk factors for cardiovascular outcomes. Another potential reason for the differential association of CAD or PVD and stroke with urinary L-FABP may be related to how these two outcomes are defined. However, the same definition of outcomes was previously demonstrated to be reliable, while data collection relied on high quality registries and medical documents.
With regard to the other cardiovascular endpoints, it is notable that urinary L-FABP predicted CAD, PVD and CVD independently of the traditional risk factors model and eGFR, but not independently of AER. One interpretation of these results could be that the actions of urinary L-FABP on these cardiovascular endpoints are independent of kidney function but not of endothelial dysfunction. Previous reports suggested that urinary L-FABP is a good discriminator between patients with acute coronary syndrome and those with stable angina, as well as a good predictor of future coronary restenosis after a first acute coronary event [29, 30]. It is possible that the most important triggers of L-FABP expression (hypoxia and NEFA concentration) play smaller roles in the chronic processes that lead to CAD or PVD compared with acute coronary syndromes, while AER and endothelial dysfunction are more important in these chronic states [15].
From the biological point of view, these independent predictive abilities of urinary L-FABP for stroke but not for the other cardiovascular endpoints are very interesting because NEFAs are metabolised by FABP proteins in all organs and new data have linked NEFAs to BP regulation [31]. However, these results may suggest a new mechanism of L-FABP action on stroke because, when adjusted for AER or BP, urinary L-FABP still predicted stroke but not other cardiovascular outcomes. Since L-FABP is not expressed in the brain but is expressed in proximal tubular cells, increased urinary L-FABP in the case of stroke prediction may represent tubular injury. Mechanisms proposed to explain the increase in L-FABP expression in the proximal tubular cells are NEFA overload, oxidative stress or toxic insults [32]. Thus, NEFA overload of the proximal tubule could mimic the effect of fatty acids on the progression of atherosclerosis in the carotid arteries. Other possible mechanisms linking the brain or carotid atherosclerosis with L-FABP could be oxidised LDL-cholesterol or other modified lipoproteins. This possibility is supported by the role of these lipoproteins in stroke development and tubular dysfunction [33]. In addition, this is based on the similar behaviour of tubular and endothelial cells in response to oxidised LDL-cholesterol exposure as well as on the positive effect of statin therapy toward tubular dysfunction and urinary L-FABP concentrations [34, 35]. Furthermore, local expression of L-FABP in the kidney can be triggered by hypoxia due to decrease peritubular capillary blood flow, which could be a proxy for the brain microcirculation status [15]. Moreover, we cannot exclude the possibility of crosstalk between the brain and kidney through B-type natriuretic peptide, which also predicts stroke and is supposed to increase diuresis and to be cleared by the kidney. Alternatively, there may be a feedback mechanism between L-FABP and other FABPs or signalling molecules expressed in hypoxic areas of the brain [36, 37]. However, it is beyond the scope of this study to further explore these potential underlying mechanisms. Therefore, the possible existence of a specific brain–kidney axis must be elucidated in future studies.
The strength of this study was the large multicentre cohort representative of the Finnish population with type 1 diabetes recruited from 80 centres in Finland. In addition, the study benefited from well-characterised phenotypes, long follow-up and high quality registry data on outcomes [22]. One potential limitation of the study may be that only a single urinary L-FABP measurement was included, although large variability in urinary L-FABP concentrations has never been reported. Another potential limitation could be the lack of data regarding anaemia, since anaemia may influence L-FABP expression. However, this was not an issue in this study because all individuals with ESRD were excluded at baseline and no member of the cohort received treatment with erythropoietin.
In summary, this large prospective study of individuals with type 1 diabetes showed that urinary L-FABP is an independent predictor of stroke and mortality, but did not have an additional predictive benefit over AER and eGFR.
Abbreviations
- CAD:
-
Coronary artery disease
- CVD:
-
Cardiovascular disease
- ESRD:
-
End-stage renal disease
- IDI:
-
Integrated discrimination improvement
- L-FABP:
-
Liver-type fatty acid binding protein
- NRI:
-
Net reclassification improvement
- PVD:
-
Peripheral vascular disease
- ROC:
-
Receiver operating characteristic
References
Laing SP, Swerdlow AJ, Slater SD et al (2003) Mortality from heart disease in a cohort of 23,000 patients with insulin-treated diabetes. Diabetologia 46:760–765
Laing SP, Swerdlow AJ, Carpenter LM et al (2003) Mortality from cerebrovascular disease in a cohort of 23 000 patients with insulin-treated diabetes. Stroke 34:418–421
Maftei O, Pena AS, Sullivan T et al (2014) Early atherosclerosis relates to urinary albumin excretion and cardiovascular risk factors in adolescents with type 1 diabetes: Adolescent type 1 Diabetes cardio-renal Intervention Trial (AdDIT). Diabetes Care 37:3069–3075
Groop PH, Thomas MC, Moran JL et al (2009) The presence and severity of chronic kidney disease predicts all-cause mortality in type 1 diabetes. Diabetes 58:1651–1658
Forsblom C, Harjutsalo V, Thorn LM et al (2011) Competing-risk analysis of ESRD and death among patients with type 1 diabetes and macroalbuminuria. J Am Soc Nephrol 22:537–544
Thorn LM, Forsblom C, Waden J et al (2009) Metabolic syndrome as a risk factor for cardiovascular disease, mortality, and progression of diabetic nephropathy in type 1 diabetes. Diabetes Care 32:950–952
McKenna K, Thompson C (1997) Microalbuminuria: a marker to increased renal and cardiovascular risk in diabetes mellitus. Scott Med J 42:99–104
Viberti GC (1991) Diabetic renal disease in type 1 diabetes: aetiology and prevention. Diabet Med 8 Spec No:S38–S42
Deckert T, Feldt-Rasmussen B, Borch-Johnsen K, Jensen T, Kofoed-Enevoldsen A (1989) Albuminuria reflects widespread vascular damage. The Steno Hypothesis. Diabetologia 32:219–226
Panduru NM, Forsblom C, Saraheimo M et al (2013) Urinary liver-type fatty acid-binding protein and progression of diabetic nephropathy in type 1 diabetes. Diabetes Care 36:2077–2083
Makowski L, Hotamisligil GS (2005) The role of fatty acid binding proteins in metabolic syndrome and atherosclerosis. Curr Opin Lipidol 16:543–548
Furuhashi M, Hotamisligil GS (2008) Fatty acid-binding proteins: role in metabolic diseases and potential as drug targets. Nat Rev Drug Discov 7:489–503
Kamijo-Ikemori A, Sugaya T, Kimura K (2006) Urinary fatty acid binding protein in renal disease. Clin Chim Acta 374:1–7
Matsui K, Kamijo-Ikemorif A, Sugaya T, Yasuda T, Kimura K (2011) Renal liver-type fatty acid binding protein (L-FABP) attenuates acute kidney injury in aristolochic acid nephrotoxicity. Am J Pathol 178:1021–1032
Yamamoto T, Noiri E, Ono Y et al (2007) Renal L-type fatty acid-binding protein in acute ischemic injury. J Am Soc Nephrol 18:2894–2902
Matsui K, Kamijo-Ikemori A, Imai N et al (2016) Clinical significance of urinary liver-type fatty acid-binding protein as a predictor of ESRD and CVD in patients with CKD. Clin Exp Nephrol 20:195–203
Ishimitsu T, Ohta S, Saito M et al (2005) Urinary excretion of liver fatty acid-binding protein in health-check participants. Clin Exp Nephrol 9:34–39
Nielsen SE, Sugaya T, Hovind P, Baba T, Parving HH, Rossing P (2010) Urinary liver-type fatty acid-binding protein predicts progression to nephropathy in type 1 diabetic patients. Diabetes Care 33:1320–1324
Araki S, Haneda M, Koya D et al (2013) Predictive effects of urinary liver-type fatty acid-binding protein for deteriorating renal function and incidence of cardiovascular disease in type 2 diabetic patients without advanced nephropathy. Diabetes Care 36:1248–1253
Thorn LM, Forsblom C, Fagerudd J et al (2005) Metabolic syndrome in type 1 diabetes: association with diabetic nephropathy and glycemic control (the FinnDiane study). Diabetes Care 28:2019–2024
Stevens LA, Coresh J, Schmid CH et al (2008) Estimating GFR using serum cystatin C alone and in combination with serum creatinine: a pooled analysis of 3,418 individuals with CKD. Am J Kidney Dis 51:395–406
Sund R (2012) Quality of the Finnish Hospital Discharge Register: a systematic review. Scand J Public Health 40:505–515
Gordin D, Forsblom C, Panduru NM et al (2014) Osteopontin is a strong predictor of incipient diabetic nephropathy, cardiovascular disease, and all-cause mortality in patients with type 1 diabetes. Diabetes Care 37:2593–2600
Delong ER, Delong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44:837–845
Pencina MJ, D’Agostino RB Sr, D’Agostino R Jr, Vasan RS (2008) Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med 27:157–172 discussion 207–212
Pencina MJ, D’Agostino RB Sr, Steyerberg EW (2011) Extensions of net reclassification improvement calculations to measure usefulness of new biomarkers. Stat Med 30:11–21
Greenland P, Smith SC Jr, Grundy SM (2001) Improving coronary heart disease risk assessment in asymptomatic people: role of traditional risk factors and noninvasive cardiovascular tests. Circulation 104:1863–1867
Yamada Y, Kato K, Oguri M et al (2008) Association of genetic variants with atherothrombotic cerebral infarction in Japanese individuals with metabolic syndrome. Int J Mol Med 21:801–808
Fukuda Y, Miura S, Zhang B et al (2009) Significance of urinary liver-fatty acid-binding protein in cardiac catheterization in patients with coronary artery disease. Intern Med 48:1731–1737
Matsumori R, Shimada K, Kiyanagi T et al (2012) Clinical significance of the measurements of urinary liver-type fatty acid binding protein levels in patients with acute coronary syndrome. J Cardiol 60:168–173
Pluznick J (2014) A novel SCFA receptor, the microbiota, and blood pressure regulation. Gut Microbes 5:202–207
Kamijo A, Sugaya T, Hikawa A et al (2004) Urinary excretion of fatty acid-binding protein reflects stress overload on the proximal tubules. Am J Pathol 165:1243–1255
Nosadini R, Tonolo G (2011) Role of oxidized low density lipoproteins and free fatty acids in the pathogenesis of glomerulopathy and tubulointerstitial lesions in type 2 diabetes. Nutr Metab Cardiovasc Dis 21:79–85
Inoue T, Ikeda H, Nakamura T et al (2011) Potential benefit of statin therapy for dyslipidemia with chronic kidney disease: Fluvastatin Renal Evaluation Trial (FRET). Intern Med 50:1273–1278
Agarwal A, Balla J, Balla G, Croatt AJ, Vercellotti GM, Nath KA (1996) Renal tubular epithelial cells mimic endothelial cells upon exposure to oxidized LDL. Am J Phys 271:F814–F823
Pelsers MM, Hanhoff T, Van Der Voort D et al (2004) Brain- and heart-type fatty acid-binding proteins in the brain: tissue distribution and clinical utility. Clin Chem 50:1568–1575
Wunderlich MT, Hanhoff T, Goertler M et al (2005) Release of brain-type and heart-type fatty acid-binding proteins in serum after acute ischaemic stroke. J Neurol 252:718–724
Acknowledgements
We thank our skilled laboratory technicians M. Parkkonen, A.-R. Salonen, A. Sandelin, T. Soppela, J. Tuomikangas (Helsinki University Central Hospital), R. Sedlmaier-Prasselsperger and K. Jaensch (Roche Germany) for their excellent organisation and measurement of urine samples on the Elecsys system. Finally, we acknowledge all physicians and nurses at each centre who participated in the recruiting participants. (The complete list of physicians and nurses is provided in ESM Table 9.)
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Data availability
The dataset is not publicly available for reasons of patient confidentiality. Please contact the authors for more information.
Funding
The study was supported by grants from Folkhälsan Research Foundation, Wilhelm and Else Stockmann Foundation, Liv och Hälsa Foundation, Novo Nordisk Foundation, Academy of Finland, Päivikki and Sakari Sohlberg Foundation and the Finnish Medical Society (Finska Läkaresällskapet). Measurements and assays for L-FABP were partly sponsored by Roche Diagnostics. However, the sponsors were not involved in the conduct of the study. PMN was supported by an Albert Renold Fellowship from the EASD. DG was supported by the Waldemar von Frenckell Foundation, the Paulo Foundation, the Paavo Nurmi Foundation, the Finnish Medical Foundation, the Swedish Cultural Foundation in Finland, and the Dorothea Olivia, Karl Walter och Jarl Walter Perkléns Foundation.
Duality of interest
MS is an advisory board member for Medtronic in Scandinavia, and has received lecture fees from Eli Lilly, Medtronic Finland, Novartis, Novo Nordisk, Roche, Sanofi Aventis and Merck Sharp & Dohme. P-HG has received investigator-initiated research grants from Eli Lilly and Roche; is an advisory board member for Abbvie, Astra-Zeneca, Boehringer-Ingelheim, Cebix, Eli Lilly, Janssen, Medscape, Merck Sharp & Dohme, Novartis, Novo Nordisk and Sanofi; and has received lecture fees from Astra-Zeneca, Boehringer-Ingelheim, Eli Lilly, Elo Water, Genzyme, Merck Sharp & Dohme, Novartis, Novo Nordisk and Sanofi. No other potential conflicts of interest relevant to this article were reported. NMP has received lecture fees from Eli Lilly.
Contribution statement
P-HG, CF, AB, PMH, MS and NMP conceived and designed the study and designed the data analysis; CF, MS, LMT, DG, NE, VH and P-HG collected and followed up the data; NMP researched data, performed statistical analyses and wrote the manuscript; and CF, MS, LMT, DG, NE, VH, PMH and P-HG researched data, contributed to discussions, and reviewed and edited the manuscript. P-HG is the guarantor of this work and gave final approval for the decision to publish.
Additional information
Angelika Bierhaus died during the course of this work.
Electronic supplementary material
ESM
(PDF 340 kb)
Rights and permissions
About this article
Cite this article
Panduru, N.M., Forsblom, C., Saraheimo, M. et al. Urinary liver-type fatty acid binding protein is an independent predictor of stroke and mortality in individuals with type 1 diabetes. Diabetologia 60, 1782–1790 (2017). https://doi.org/10.1007/s00125-017-4328-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-017-4328-x