Abstract
Background
Penetrating cardiac injuries are uncommon and lethal. The objectives of this study are to examine the national profile of cardiac injuries, identify independent predictors of outcome, generate, compare and validate previous predictive models for outcomes. We hypothesized that National Trauma Data Bank (NTDB) given its large number of patients, would validate these models.
Methods
The NTDB was queried for data on cardiac injuries, using survival as the main outcome measure. Statistical analysis was performed utilizing univariate and stepwise logistic regression. The stepwise logistic regression model was then compared with other predictive models of outcome.
Results
There were 2016 patients with penetrating cardiac injuries identified from 1,310,720 patients. Incidence: 0.16%. Mechanism of injury: GSWs—1264 (63%), SWs—716 (36%), Shotgun/impalement—19/16 (1%). Mean RTS 1.75, mean ISS 27 ± 23. Overall survival 675 (33%). 830 patients (41%) underwent ED thoracotomy, 47 survived (6%). Survival stratified by mechanism: GSWs 114/1264 (10%), SWs 564/717 (76%). Predictors of outcome for mortality—univariate analysis: vital signs, RTS, ISS, GCS: Field CPR, ED intubation, ED thoracotomy and aortic cross-clamping (p < 0.001). Stepwise logistic regression identified cardiac GSW’s (p < 0.001; AOR 26.85; 95% CI 17.21–41.89), field CPR (p = 0.003; AOR 3.65; 95% CI 1.53–8.69), the absence of spontaneous ventilation (p = 0.008; AOR 1.08, 95% CI 1.02–1.14), the presence of an associated abdominal GSW (p = 0.009; AOR 2.58, 95% CI 1.26–5.26) need for ED airway (p = 0.0003 AOR 1386.30; 95% CI 126.0–15251.71) and aortic cross-clamping (p = 0.0003 AOR 0.18; 95% CI 0.11–0.28) as independent predictors for mortality. Overall predictive power of model—93%.
Conclusion
Predictors of outcome were identified. Overall survival rates are lower than prospective studies report. Predictive model from NTDB generated larger number of strong independent predictors of outcomes, correlated and validated previous predictive models.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Penetrating cardiac injuries are uncommon and lethal. The majority of these patients succumb at the scene of the traumatic incident. Those that survive to arrive at a Trauma Center present with impending or cardiopulmonary arrest; and incur high mortality. Evaluation of data in the literature reveals favorable outcomes in selected studies, for these injuries [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32]. Close scrutiny of these series reveal many to be retrospective and overlapping. Frequently, there is a lack of reported data describing the initial physiologic status upon arrival of these patients. No series have graded cardiac injuries utilizing the American Association for the Surgery of Trauma Organ Injury Scale (AAST-OIS). Similarly, there is a lack in reporting independent predictors of outcomes [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32]. To the best of our knowledge, there are only three prospective cardiac injury series in the literature providing statistical analysis of predictors of outcomes [33,34,35] and only one validating the AAST-OIS cardiac injury scale [35].
In a prospective 2-year study of 105 penetrating cardiac injuries, the authors prospectively analyzed parameters measuring the physiologic condition of these patients upon arrival at the Trauma Center along with the cardiovascular respiratory score (CVRS) of the Trauma score, mechanism and anatomic site of injury, the presence versus the absence of tamponade and other predictors of outcome upon opening the pericardium including bleeding, need for aortic cross-clamping, and restoration of blood pressure, amongst others by univariate and multivariate analysis. In this study, the stepwise logistic regression analysis identified gunshot wounds (GSW), exsanguination and restoration of blood pressure to be the most predictive variable for mortality. This model produced a Max-rescaled R 2 of 0.81 and a concordance of 95% [35].
Objectives of this study are to examine the national profile of cardiac injuries, identify and validate independent predictors of outcome, create a more robust predictive model, and compare and validate previous predictive models determining outcomes. We hypothesized that the NTDB, with its large number of patients would allow the creation of such predictive model and validate current models. Other objectives are to report the incidence of these injuries, and overall survival and mortality rates.
Methods
Data were obtained from the National Trauma Data Bank (NTDB) version 3.0. The NTDB is the largest repository of multi-institutional data collected prospectively from level I Trauma Centers and maintained by the American College of Surgeons (ACS). This version contains data from a total of 1,310,720 patients from all level I trauma centers reporting data to this registry. The NTDB was queried for pre-hospital and admissions data for all patients sustaining penetrating cardiac injuries. Data extracted included demographics. Pre-hospital data able to be extracted included pre-hospital procedures such as field CPR, field intubation and thoracic needle decompression. Other data extracted included initial admission, vital signs, GCS, RTS and ISS along with airway management whether FAST was performed or not. Patients pronounced dead upon arrival were noted. Data collected also included ED versus OR thoracotomy, need for aortic cross-clamping and outcomes.
Statistical analyses included univariate and stepwise logistic regression. Pearson’s Chi-square test or Fisher’s exact test was used for categorical variables and the Mann–Whitney test for continuous variables. Odds ratio with 95% confidence intervals were calculated from contingency tables and statistical significance set at a p value <0.05. Multivariate analysis was performed to identify a set of patient characteristics that best predict mortality outcome utilizing binary logistic regression. Based on the findings of univariate analysis, variables showing at least a moderate level of association (p < 0.20) were entered into stepwise logistic regression analysis to select the highest model performance and to calculate the predictive power of the model. All statistical analyses were performed utilizing the SAS statistical packages (SAS Systems for Windows, Version 9.4 SAS Institute Inc., Cary NC).
Results
In this version of the NTDB, there were 2016 patients identified from a total of 1,310,720 patients. The national incidence of penetrating cardiac injuries is estimated as 0.16%. This does not take into account that many patients sustaining cardiac injuries succumb at the scene of the traumatic incident prior to transport. This data does not reflect penetrating cardiac injury deaths in non-trauma centers that do not submit data to the NTDB. Breakdown according to gender include 1203 males (59.4%) and 813 females (40.8%). Mean age for this patient population is 38 ± 23. Pre-hospital procedures performed include administration of intravenous fluids in 1689 (83.8%) and thoracic needle decompression in 267 (13.3%) (see Table 1).
There were a total 1264 (63%) gunshot wounds (GSWs), 717 (36%) stab wounds (SWs), and 19 (0.9%) patients with impalement injuries, while 16 (0.8%) sustained shotgun wounds (SGWs). The mean RTS was 1.75 ± 3.22 (range 0–7.84), mean ISS 27.19 ± 23 (range 1–75), mean admission systolic blood pressure (SBP) (mmHg) 42.72 ± 5.03 (range 0–150), mean admission diastolic blood pressure (DBP) (mmHg) 29.26 ± 34.29 (range 0–88), ED heart rate (HR) 58.71 ± 71.82 (range 0–238) beats/min and mean respiratory rate (RR) was 8.53 ± 10.69 (range 0–68), mean Temperature was 35.4 ± 0.09 °C (range 33.1–36.4), while the mean GCS was 5.7 ± 4.89 (range 3–15) (see Table 2).
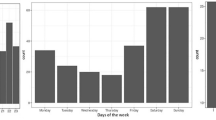
Of the 2016 patients, 212 (10.5%) were pronounced dead upon arrival, 1804 (89.5%) survived to receive further management. Of these, 830 patients underwent ED thoracotomy with 47 (5.7%) survivors. The remaining patients succumbed in the ED immediately post-resuscitative thoracotomy; while the remaining 974 (54%) survived to reach an operating room (OR) to undergo OR thoracotomy (ORT) 628 (64.5%) survived (see Fig. 1). There were 675 (33%) survivors. Survival stratified by mechanism of injury: GSWs 114/1264 (10%), SWs 564/717 (76%) (see Table 3).
The mortality rate of patients with RTS = 0 was 94% versus those with RTS ≥1–38.6%. The mortality for GSWs was 90.6% versus SWs—23.8%. Those requiring EDT had a mortality rate of 94.3% versus reaching the OR to undergo ORT—35.6%. For patients requiring aortic cross-clamping, the mortality rate was 94.3% (see Table 3).
There were statistically significant differences between survivors and non-survivors including initial vital signs, GCS, RTS and ISS (p < 0.0001) (see Table 4). Other statistically significant predictors of outcome for mortality included need for pre-hospital cardiopulmonary resuscitation (CPR), need for emergency department intubation, ED thoracotomy (EDT) and aortic cross-clamping (p < 0.001) (see Table 5).
Stepwise logistic regression identified GSW (p < 0.001; AOR 26.85; 95% CI 17.21–41.89), field CPR (p = 0.003; AOR 3.65; 95% CI 1.53–8.69), absent spontaneous ventilation (p = 0.008; AOR 1.0, 95% CI 1.02–1.14), need for an ED airway (p = 0.0003 AOR 1386.30; 95% CI 126.0–15251.71) and need for aortic cross-clamping (p = 0.0003 AOR 0.18; 95% CI 0.11–0.28) as independent predictors of outcome for mortality (see Table 6). Overall predictive power of model: 93%. Complications amongst the survivors ranged from 1.4 to 6.5%.
Discussion
Penetrating cardiac injuries are uncommon and highly lethal. The majority of patients succumb at the scene of the traumatic incident. Because of rapid transport, many generally arrive at urban Trauma Centers either in impending or cardiopulmonary arrest.
There are currently three prospective cardiac injuries series in the literature [33,34,35]. The first reported by Buckman [33], analyzed factors influencing their initial resuscitation. This 27-month study included 66 patients evaluated with the cardiovascular respiratory score (CVRS) component of the trauma score (TS), 70% sustained GSWs and 71% of the patients required an Emergency Department Thoracotomy (EDT) and for the first time validated the CVRS as a physiologic predictor of outcome with reported survival rates of 20% for GSWs and 80% for SW’s, respectively.
Cardiac injuries are uncommon, and thus few trauma centers and trauma surgeons have significant experience with these injuries. This is validated by the paucity of series reported in the recent literature. A PubMed search of studies on penetrating cardiac injuries for the past 20 years; including search terms such as cardiac, heart, penetrating cardiac and penetrating heart injuries; yielded 323 publications. This search revealed that the last large series were published between 1998 and 2000, while the remaining series consisted of small studies and single case reports describing unusual wounding agents. Since 2004 there have been at least three series, reporting between 64 and 82 patients whose injury mechanism was mostly stab wounds [36,37,38].
The most recent retrospective study was published by Soto [39] in 2015, reporting 135 patients from a level II Trauma Center over the span of 15 years, from an institution receiving approximately nine cardiac injuries per year. Of these 135 patients, 96 (71%) did not survive past the ED; and 89 of these 96 (93%) patients were considered DOA (dead on arrival), thus leaving 39 patients to undergo thoracotomy. This small series reports similar survival data reported in only three prospective cardiac injury series in the literature [33,34,35].
Difficulties exist in evaluating the results of series reported over the past three decades. Over 30 series have been reported in the English language literature [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32]. Close scrutiny reveals that most series are retrospective, reporting small volumes with many serial and overlapping studies from selected institutions [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32]. Although some of these selected studies have reported favorable outcomes, many provide no data on the physiologic conditions of these patients upon presentation, nor do they report statistically validated predictors of outcome. Unfortunately, none of these series have graded these injuries utilizing the AAST-OIS cardiac injury scale.
We hypothesized that the NTDB, with its large number of patients would help us determine the outcomes for penetrating cardiac injuries. We thus reviewed the national profile of these injuries from the NTDB, for their incidence and to determine mortality and survival rates, and identify predictors of outcome for these highly lethal injuries. These enabled us to generate what we determined to be a more robust predictive model, to compare and validate current predictive models.
Subsequently, the second prospective study in the literature [34] consisting of 60 patients admitted in a 1 year period, validating the CVRS score, and statistically validating the physiologic conditions of these patients in the field, during transport and upon arrival; reported a 68% incidence of GSWs; and an overall survival rate of 36.6%. Stratified to mechanism of injury the survival rate for GSWs was 14% and SW’s was 68%, respectively; with an EDT survival rate of 16%. This study did not accumulate sufficient number of patients to perform stepwise logistic regression to generate a predictive model.
In the third prospective series in the literature, Asensio [35] reported a 2-year study consisting of 105 patients with an incidence of 65% GSWs and a survival rate of 33%. In this series, 71 (68%) of the patients required EDT with a survival rate of 14%. Survival stratified to mechanism of injury was 16% for GSWs and 65% for SWs. This study also prospectively validated the CVRS score and the physiologic condition of patients in the field, during transport and upon arrival as predictors of outcome. It graded cardiac injuries utilizing the AAST-OIS for cardiac injuries; stratifying mortality rates for each injury grade and per cardiac chamber injured. Of the 105 patients 99 (94%) of the patients sustained grade IV–VI injuries. Stepwise logistic regression identified GSWs, exsanguination and restoration of blood pressure to be the most independent predictive variables for mortality. This model had an overall predictive power of 95%.
In this analysis of 2016 patients from the NTDB, we have estimated the incidence of penetrating cardiac injuries at 0.16%. Stratified to mechanism of injury, GSWs account for 63%. This is consistent with series [33,34,35] which range from 65 to 70% and also with the study reported by Soto [39] of 72%, whereas the incidence of SW’s is 36%, again consistent with data reported by Buckman [33], Asensio [33,34,35] and Soto [39], ranging from 28 to 35%. Series by Gao [36], Rodrigues [37], and Topal [38], however, report the majority of their patients sustaining stab wounds ranging from 61 to 87%.
The mean RTS of 1.75 ± 3.22, ISS 27 ± 23 and GCS of 5.70 ± 4.89 are consistent with data reported by the three prospective series in the literature [33,34,35]. The series by Soto [39] reports a mean ISS of 53, however, 96 (93%) of their 135 patients were DOA. Series by Gao [36], Rodrigues [37] and Topal [38] do not report these data. The low RTS, ISS and GCS, which is an indirect indicator of perfusion, reveal a severely physiologically compromised population with a high degree of anatomic injury.
Physiologic condition of patients upon arrival proved to be statistically significant between survivors versus non-survivors; some of these parameters have been confirmed in previous series [11, 16, 22, 31, 33,34,35,36,37,38]. The CVRS score [33,34,35] could not be calculated for the 2016 patients in this series. Similarly, it is known that the need for field CPR and EDT are also strong predictors of outcome [11, 16, 22, 33,34,35,36,37,38]. Aortic cross-clamping, however, has only been statistically proven as a predictor of outcome in two series [34, 35]. In this study, the need for EDT and aortic cross-clamping were strong predictors of outcome.
Stepwise logistic regression confirmed a larger number of strong independent predictors of outcome, which include the presence of an associated abdominal GSW (n = 6), cardiac gunshot wounds, need for field CPR, the absence of spontaneous ventilation, need for ED airway and need for aortic cross-clamping as independent predictors of outcome with a predictive power for this model of 93%. These data are consistent with another series [35] whose logistic regression model identified a triad (n = 3) consisting of gunshot wounds exsanguination and restoration of blood pressure as the strongest independent predictors for mortality in a model with a max-rescaled R 2 of 0.81 and a predictive power of 95%. No doubt, the larger number of patients in the NTDB allowed other independent predictors of outcome to emerge and be validated.
The overall survival rate of 33% is comparable to the largest prospective series in the literature [35]. Survival rate stratified to mechanism of injury—GSWs 10% is slightly lower than reported by Asensio [34, 35]—14 to 16% but within statistical range. Whereas survival for SWs—76% in this study is slightly higher than previously reported [34, 35]—65 to 68%, again, within statistical range, and is similar to that reported in Buckman’s [33] prospective series −80%. ED thoracotomy survival rate for this series is 5.7% versus Asensio [34, 35] survival rate of 14–16%; this is lower, but may be accounted by the fact that in these two series there was one group of Trauma Surgeons performing these procedures under strict protocols [34, 35, 40].
The NTDB has become an important tool for clinical research and bench marking; however, it has limitations. It is not population based; some of the patients may not be completely representative; as much of the data is obtained from verified Trauma Centers or State Trauma Registries that may be geographically concentrated. As with any large database, there may be errors in the entry of data, missing or invalid entries and misclassifications; especially missing data from pre-hospital EMS (Emergency Medical Services) personnel. Furthermore, it does not report detailed operative data nor does it classify organ injuries. Therefore, these are limitations of this study as well as all of the NTDB. Be that as it may, the NTDB remains the best available sample of data to study mortality and generate predictive models for survival for different injuries.
We believe that this retrospective analysis of prospectively collected data from the NTDB reports the largest volume of penetrating cardiac injury patients in the literature thus far, and provides a comprehensive analysis of current outcomes in America. It has allowed the creation of a predictive model of outcome with greater number of predictors; and validates previous predictive models prospectively reported for cardiac injury.
Conclusions
In this study, predictors of outcomes were identified. Overall survival rates are lower than most retrospective studies reported. Data suggests that patients can be selected for salvage and outcomes predicted. Decisions must be undertaken to direct salvage efforts including ED thoracotomy to patients presenting with signs of life in the field and short transport times to 10 versus 12 min prior to arrival at the Trauma Center. Consideration should be given to patients that have been successfully intubated in the field and have a secure airway. For these patients, resuscitative thoracotomy may be undertaken based on an institutional experience upon their arrival at Trauma Centers, to improve outcomes and decrease health care costs. The predictive model generated from the NTDB, with all of its previously cited limitations, generated a larger number of strong independent predictors as outcome (n = 6) validating previous predictive models reported prospectively in the literature.
References
Demetriades D, Van Der Veen BW. Penetrating injuries of the heart: experience over two years in South Africa. J Trauma. 1983;23:1034–41.
Abbott JA, Cousineau M, Cheitlin M, et al. Late sequelae of penetrating cardiac wounds. J Thorac Cardiovasc Surg. 1978;75:510–8.
Attar S, Suter CM, Hankins JR, et al. Penetrating cardiac injuries. Ann Thorac Surg. 1991;51:711–6.
Beall AC Jr, Patrick TA, Ikles JE, et al. Penetrating wounds of the heart: changing patterns of surgical management. J Trauma. 1972;12:468–73.
Beach PM Jr, Bognolo D, Hutchinson JE. Penetrating cardiac trauma, experience with thirty-four patients in a hospital without cardiopulmonary bypass capability. Am J Surg. 1976;131:411–4.
Breaux EP, Dupont JB Jr, Albert HM, et al. Cardiac tamponade following penetrating mediastinal injuries: improved survival with early pericardiocentesis. J Trauma. 1979;19:461–6.
Carrasquilla C, Wilson RF, Walt AJ, et al. Gunshot wounds of the heart. Ann Thorac Surg. 1972;13:208–13.
Degennaro VA, Bonfils-Roberts EA, Ching N, et al. Aggressive management of potential penetrating cardiac injuries. J Thorac Cardiovasc Surg. 1980;79:833–7.
Demetriades D. Cardiac penetrating injuries: personal experience of 45 cases. Br J Surg. 1984;71:95–7.
Evans J, Gray LA Jr, Payner A, et al. Principles for the management of penetrating cardiac wounds. Ann Surg. 1979;189:777–84.
Feliciano DV, Bitondo CG, Mattox KL, et al. Civilian trauma in the 1980s. A one year experience with 456 vascular and cardiac injuries. Ann Surg. 1980;1984(199):717–24.
Harvey JC, Pacifico AD. Primary operative management: method of choice for stab wounds to the heart. South Med J. 1975;68:149–52.
Ivatury RR, Rohman M, Steichen FM, et al. Penetrating cardiac injuries: twenty-year experience. Ann Surg. 1987;53:310–7.
Mandal AK, Awariefe SO, Oparah SS. Experience in the management of 50 consecutive penetrating wounds of the heart. Br J Surg. 1979;66:565–8.
Mandal AK, Oparah SS. Unusually low mortality of penetrating wounds of the chest: twelve years’ experience. J Thorac Cardiovasc Surg. 1989;97:119–25.
Moreno C, Moore EE, Majure JA, et al. Pericardial tamponade: a critical determinant for survival following penetrating cardiac wounds. J Trauma. 1986;26:821–5.
Naughton MJ, Brissle RM, Bessey PQ, et al. Demography of penetrating cardiac trauma. Ann Surg. 1989;209:676–83.
Sugg WL, Rea WJ, Ecker RR, et al. Penetrating wounds of the heart: analysis of 459 cases. J Thorac Cardiovasc Surg. 1968;56:531–45.
Symbas PN, Harlaftis N, Waldo WJ. Penetrating cardiac wounds: a comparison of different therapeutic methods. Ann Surg. 1976;183:377–81.
Tavares S, Hankins JR, Moulton AL, et al. Management of penetrating cardiac injuries: the role of emergency thoracotomy. Ann Thorac Surg. 1984;38:183–7.
Blake DP, Gisbert VL, Ney AL, et al. Survival after emergency department versus operating room thoracotomy for penetrating cardiac injuries. Am Surg. 1992;58:329–33.
Buchman TG, Phillips J, Menker JB. Recognition, resuscitation and management of patients with penetrating cardiac injuries. SGO. 1992;174:205–10.
Mitchell ME, Muakkassa FF, Poole GV, et al. Surgical approach of choice for penetrating cardiac wounds. J Trauma. 1993;34:17–20.
Macho JR, Markison RE, Schecter WP. Cardiac stapling in the management of penetrating injuries of the heart: rapid control of hemorrhage and decreased risk of personal contamination. J Trauma. 1993;34:711–6.
Roberge RR, Ivatury RR, Stahl W, et al. Emergency department thoracotomy for penetrating injuries: predictive value of patient classification. Am J Emerg Med. 1986;4:129–35.
Knott-Craig CJ, Dalton RP, Rossouw GJ, et al. Penetrating cardiac trauma: management strategy based on 129 surgical emergencies over 2 years. Ann Thorac Surg. 1992;53:1006–9.
Steichen FM, Dargan EL, Efron G, et al. A graded approach to the management of penetrating wounds of the heart. Arch Surg. 1971;103:574–80.
Brown SE, Gomez GA, Jacobson LE, et al. Penetrating chest trauma: should indications for emergency room thoracotomy be limited? Am Surg. 1996;62:530–4.
Hirshberg A, Wall MJ, Allen MK, et al. Double jeopardy: thoracoabdominal injuries requiring surgical intervention in both chest and abdomen. J Trauma. 1995;39:225–31.
Mazzorana V, Smith RS, Morabito DJ, et al. Limited utility of emergency department thoracotomy. Am Surg. 1994;60:516–21.
Saadia R, Levy RD, Degiannis E, et al. Penetrating cardiac injuries: clinical classification and management strategy. Br J Surg. 1994;81:1572–5.
Kaplan AJ, Norcross ED, Crawford FA. Predictors of mortality in penetrating cardiac injury. Am Surg. 1993;59:338–41.
Buckman RF, Badellino MM, Mauro LH, Asensio JA, et al. Penetrating cardiac wounds: prospective study of factors influencing initial resuscitation. J Trauma. 1993;34:717–27.
Asensio JA, Murray J, Demetriades D, et al. Penetrating cardiac injuries: a prospective study of variables predicting outcomes. J Am Coll Surg. 1998;186:24–34.
Asensio JA, Berne JD, Demetriades D, Chan L, Murray J, Falabella A, et al. One hundred five penetrating cardiac injuries: a 2-year prospective evaluation. J Trauma. 1998;44(6):1073–82.
Gao JM, Gao YH, Wei GB, Liu GL, Tian XY, Hu P, Li CH. Penetrating cardiac wounds: principles for surgical management. World J Surg. 2004;28(10):1025–9 (Epub 2004 Sep 29).
Rodrigues AJ, Lopes-Furlanetti LL, Bijos-Faidiga G, Scarpelivi S, et al. Penetrating cardiac injuries: a 13 year retrospective evaluation form a Brazilian trauma center. Interact Cardiovasc Thorac Surg. 2005;4:p212–5.
Topal AE, Celik Y, Eren MN. Predictors of outcome in penetrating cardiac injuries. J Trauma. 2010;69(3):574–8.
Murry JS, Truitt MS, Dunn EL. Penetrating cardiac injuries at a level II trauma center: a 15-year review. Am Surg. 2015;81(3):324–5.
Asensio JA, Stewart BM, Murray J, et al. Penetrating cardiac injuries. Surg Clin North Am. 1996;76:685–724.
Author information
Authors and Affiliations
Contributions
Study conception and design: JAA. Acquisition of data: PP. Analysis and interpretation of data: JA, PP. Drafting of manuscript: AO. Critical revision: JA, AO, AOU, MW, RB, BP, DLC.
Corresponding author
Ethics declarations
Conflict of interest
J. A. Asensio, O. A. Ogun, P. Petrone, A.J. Perez-Alonso, M. Wagner MD, R. Bertellotti, B. Phillips, D. L. Cornell, and A. O. Udekwu, all declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Asensio, J.A., Ogun, O.A., Petrone, P. et al. Penetrating cardiac injuries: predictive model for outcomes based on 2016 patients from the National Trauma Data Bank. Eur J Trauma Emerg Surg 44, 835–841 (2018). https://doi.org/10.1007/s00068-017-0806-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-017-0806-6