Abstract
Background
Postoperative peritonitis still remains the cause of a high mortality rate in emergency abdominal surgery. Here we aimed to evaluate the efficacy of different surgical strategies for small-bowel perforations that resulted in postoperative peritonitis.
Methods
Surgical management results for 140 patients with postoperative peritonitis due to small-bowel perforations, necrosis and anastomotic leakage were comparatively analyzed. Using the APACHE-II and MPI scoring systems, different surgeon attitudes were examined in three patient groups (primary anastomosis, delayed anastomosis, and enterostomy).
Results
The surgical approach in patient group I (n = 47, APACHE-II 11.7 ± 1.2, MPI 14.7 ± 1.3) involved the closure of small-bowel perforations or small-bowel resection to place primary anastomosis. The mortality rate was 17%. Patient group II (n = 48, APACHE-II 16.8 ± 0.7, MPI 19.3 ± 0.3) underwent delayed small-bowel anastomosis during planned relaparotomies. The mortality rate was 18.8%. Because patients in patient group III (n = 45, APACHE-II 22.3 ± 1.3, MPI 24.6 ± 1.2) were in very critical condition, anastomoses were not placed after bowel resection, and the surgical procedure was completed with enterostomy. The highest mortality rate of 37.8% was documented in this patient group.
Conclusion
The differentiated surgical approach undertaken herein using delayed small-bowel anastomosis in more serious patients with postoperative peritonitis was able to mitigate the risk of recurrent anastomotic leaks and was not accompanied by a considerable rise in mortality. The mortality for primary repair and delayed primary closure was basically the same (17.0% and 18.8%, p = 0.03); however, delayed anastomosis in the patients with postoperative peritonitis at higher APACHE-II and MPI scores for severity of illness showed 15.1% less complications in the form of anastomotic leaks (p = 0.04).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Postoperative peritonitis distinguishes itself by severe course and difficult surgical treatment, with high mortality rates ranging from 15 to 70% [1,2,3]. This is attributed to the specifics of etiology, pathogenesis, clinical implications and imperfect approaches to surgical management [4, 5]. The most common causes of postoperative peritonitis include intestinal anastomotic leakage, spontaneous small-bowel perforations, abdominal abscesses, and ongoing intestinal necrosis after surgical operations for acute mesenteric ischemia [6,7,8,9]. The surgeons still have mixed views on the surgeon volume in postoperative perforative peritonitis, the number of surgical operations and their completion technique, which are always nonstandard in nature and depend on a specific situation revealed by inspecting the abdominal cavity [10,11,12]. In most cases, it is a common practice to perform relaparotomy with resection of the altered intestinal loop [13]. However, placing new small-bowel anastomoses under conditions of severe peritonitis and abdominal sepsis is really risky because intestinal suture may fail [14,15,16]. In this context, the development of novel tactical and technical approaches becomes especially relevant, and such approaches are associated with the choice of interintestinal anastomosis time and techniques using primary or delayed anastomosis during programmed relaparotomies [17, 18], as well as with the choice of methods focused on enhancing the integrity of anastomoses placed under postoperative peritonitis conditions [19].
The aim of this study was to evaluate the efficacy of different surgical strategies for repairing small-bowel defects that caused postoperative peritonitis.
Patients and methods
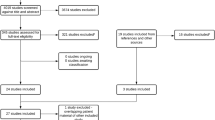
Between May 2010 and October 2018, 140 patients with postoperative peritonitis admitted to our clinical hospital were included in this prospective cohort study. To ensure quality and consistency in the delivery of the intervention, a quality control commission was formed in the clinical hospital and comprised five members including the Chief of General Surgery Department, the Chief of Purulent Surgery Department, Deputy Chief Doctor, Associate Professor at the Chair of Departmental Surgery and Hospital Surgery, and a representative from a Medical University. Ninety-eight males and forty-two females received surgical treatment. The mean age was 51.9 ± 2.2 years. All patients were hospitalized to the clinic with postoperative small-bowel leaks. Primary diagnoses, due to which the patients were operated on at the previous stages, were acute adhesive bowel obstruction (n = 64, 45.7%), acute mesenteric ischemia (n = 21, 15%), incarcerated hernia (n = 20, 14.3%), acute appendicitis (n = 18, 12.9%), pancreonecrosis (n = 9, 6.4%), and tubo-ovarian abscess (n = 8, 5.7%). Primary operations that resulted in small-bowel leakage were adhesiolysis, small-bowel resection with enteroenterostomy, closure of small-bowel perforation, and enterostomy. The major complications from preceding operations that resulted in progression of postoperative peritonitis were small-bowel anastomotic leakage (58.6%), nontraumatic small-bowel perforations (29.3%) and segmental small-bowel necrosis (12.1%). APACHE-II (acute physiology, age, chronic health evaluation) and MPI (Mannheim Peritonitis Index) scores were calculated for all patients on admission to the inpatient treatment facility to assess severity of illness, mortality risk and severity of peritonitis [20, 21]. On the basis of the APACHE-II and MPI scores, the patients with postoperative small-bowel leaks were divided into groups with different anastomotic placement time following small-bowel resection: group I—primary anastomosis (n = 47), group II—delayed anastomosis (n = 48), and group III—anastomosis was not placed and enterostomy was performed (n = 45). The groups were comparable in gender, age, and small-bowel pathology. The clinicopathological characteristics such as gender, age, and causes of postoperative peritonitis for the patient groups are listed in Table 1.
Patient inclusion criteria were postoperative peritonitis as clinical diagnosis and the conduct of relaparotomy. Exclusion criteria were peritoneal cancer and multiple organ dysfunction syndrome.
Statistical analysis
The data were presented as mean ± standard deviation (SD), medians (range), and proportions. Differences in categorical and continuous variables were analyzed using the Student’s t test. The mortality rate and post-surgery complications were compared in the three patient groups with different severity of postoperative peritonitis and different surgical approaches to anastomosis placement: primary anastomosis, delayed anastomosis, and enterostomy. A significant difference was considered when the two-tailed p value was less than 0.05. All statistical analyses were done using the Statistica 6.0 software. The patient assignment to three groups depending on the APACHE-II and MPI score points is given in Table 2.
According to the Clavien–Dindo classification of surgical complications, patient group I had Grade IIIb, group II had Grade IVa and group III had Grade IV complications.
Patient group I included 47 patients (33.6%) who received conventional surgical management during relaparotomy, taking into account the APACHE-II severity of illness and MPI severity of peritonitis. This surgical intervention involved suturing the small-bowel defects or small-bowel resection to place primary anastomosis. The further course of postoperative peritonitis in this patient group implied on-demand relaparotomies.
Group II included 48 patients (34.3%) to whom the delayed anastomosis technique was applied during relaparotomy, taking account of the APACHE-II and MPI scores. During relaparotomy, the affected area of the small bowel was subjected to resection (or in combination with right hemicolectomy) to create small-intestinal stumps (1 and 2) or small-intestinal and colonic stumps (1 and 4) buried with two purse-string sutures. The closed intestinal segments were not brought out into the anterior abdominal wall but were left in the abdominal cavity instead (Fig. 1). A drain tube was introduced into the upper small intestine. Temporary abdominal closure was then performed.
Later on, 48 h postoperatively, the second programmed relaparotomy was done, during which a decision was pending about whether to place delayed interintestinal anastomosis. The criterion for applying delayed interintestinal anastomosis was the subsidence of inflammatory changes (clear exudate, single fibrin deposits, reduced edema, small-bowel wall infiltration, shiny serous membrane of the abdomen).
Group III included 45 patients (32.1%) who had the highest risk of small-bowel suture failure on closing the defects in either primary or delayed anastomosis, as well as the risk of new small-bowel perforations. In this case, resection of the intestine was performed with enterostomy, along with planned relaparotomies and open abdomen management.
In the postoperative period, the number of complications (new small-bowel perforations, recurrent anastomotic leakage) and the mortality rate were studied in the groups.
Results
The favorable prognosis for intestinal defect closure or primary interintestinal anastomosis after small-bowel resection was noticed with APACHE-II < 15 points (11.7 ± 1.2) for morbidity and MPI < 21 points (14.7 ± 1.3) for severity of peritonitis in patient group I. Among the objective intraoperative signs in patients were slight small-bowel serosa hyperemia, single fibrin deposits on the abdomen, reduced small-bowel peristaltic activity, slight small-bowel wall infiltration, moderate small-bowel distension (4–5 cm), and single perforations of up to 0.5 cm wide (Fig. 2).
The technique involving small-bowel obstructive resection and delayed anastomosis was basically used with APACHE-II > 15 points (16.8 ± 0.7) and MPI 21–29 points (19.3 ± 0.3) in patient group II. The main intraoperative changes within the abdominal cavity included absent small-bowel peristalsis, considerable small-bowel distension (over 6.0 cm wide), significant small-bowel wall infiltration and hemorrhage, moderate fibrinous deposits, two and more small-bowel perforations of 0.5–1 cm wide, small-bowel anastomotic leaks, and segmental small-bowel necrosis. There was a very real risk of suture failure in these situations when closing the intestinal defects or placing primary anastomosis. The patients therefore underwent small-bowel resection with delayed anastomosis (Fig. 3) during subsequent planned relaparotomies in 36–48 h.
Group III comprised the most critical patients who had APACHE-II > 20 points (22.3 ± 1.3) and MPI > 30 points (24.6 ± 1.2). The intraoperative changes within the abdominal cavity were significant and exhibited persistent absent peristalsis, massive multiple confluent serosal hemorrhages, small-bowel color change to dirty gray, huge fibrin deposits on the abdomen, pronounced intestinal wall infiltration, multiple small-bowel perforations, small-bowel anastomotic leaks, and ongoing intestinal necrosis after resection. These patients had the highest risk of suture failure both in defect closure and in primary or delayed anastomosis with a real risk of new spontaneous small-bowel perforations to occur. In these cases, small-bowel resection was performed with further enterostomy (Fig. 4a), coupled with planned peritoneal cavity lavage. The patients were subsequently managed by the open abdomen technique to perform a vacuum-assisted abdominal closure (VAC) (Fig. 4b).
At early stages of postoperative peritonitis with low morbidity points (APACHE-II 11.7 ± 1.2), placement of primary interintestinal anastomoses was accompanied by a mortality rate reaching 17%. In patients with severe toxemia and clinical evidence of organ dysfunction (APACHE-II 16.8 ± 0.7 points in patient group II), the suture failure risk when surgical procedures were completed with delayed anastomosis was 1.8% higher than with primary anastomosis (p > 0.05). The mortality rate in patient group II came up to 18.8%. The highest mortality rate was noted in patient group III (APACHE-II 22.3 ± 1.3 points) in which it attained 37.8% with increasing number of laparotomies (4.2 ± 0.8) due to new perforations of the small bowel (31.1%). The overall mortality was 35 patients (25%). Postoperative complications and mortality rates are summarized in Table 3.
Discussion
In recent years, damage control surgery (DCS) involving programmed relaparotomies has increasingly been gaining ground [22, 23], and the open abdomen (OA) management combined with vacuum-assisted closure (VAC) therapy is becoming the standard of care [10, 24, 25]. The principal and most reliable method to achieve source control of intraabdominal infection [26, 27] is to perform resection of the intestine during both primary surgery and repeated lavage of the abdominal cavity. However, placing interintestinal anastomoses as the final surgical step comes amid an enhanced risk of anastomotic leaks under conditions of diffuse suppurative inflammation in the abdominal cavity and anterior abdominal wall, mesenteric circulatory disorder, and deficiency in enteral nutrition [28,29,30]. Obstructive resection of the small bowel was first performed in patients with acute mesenteric ischemia that occurred in the territory of the superior mesenteric artery and was accompanied by the intestinal necrosis [31]. To control the condition of the remaining intestinal segments in this situation, the second-look laparotomy procedure was developed. It was reported that the frequency of the planned second-look surgery was 10%, in which case the need for repeat intestinal resection arose in 25% of cases [32]. Given the high incidence of postoperative complications and fatal outcomes, it becomes evident that a new surgical approach is needed for the restoration of intestinal continuity. The differentiated approach to primary and delayed anastomoses in patients with postoperative peritonitis, which relies on evaluating the severity of illness and intraoperative picture of peritonitis in the abdominal cavity [18], could serve this purpose.
Strengths and limitations of this study:
-
To the best of our knowledge, no differentiated approach to repeat anastomoses (primary or delayed) in patients with postoperative peritonitis, on the basis of the APACHE-II and MPI scores, exists in Russia.
-
The findings from this study will help choose a repeat surgical strategy to treat patients suffering from postoperative peritonitis resulting from small-bowel anastomotic leakage, perforations and segmentary necrosis.
-
Delayed anastomosis in patients with postoperative peritonitis has a limitation that should be borne in mind when one considers it for application in surgery. For instance, 45 patients had a very critical condition, with 22.3 ± 1.3 APACHE-II and 24.6 ± 1.2 MPI, indicating a high mortality risk. In such cases, delayed anastomosis cannot be advised and the operation should be completed with enterostomy. However, if the section of the small-bowel proximal is short (less than 20 cm), enterostomy is not appropriate due to the jejunal stump and related substantial intestinal losses. In this case, one should consider delayed colonic anastomosis (entero-colonic anastomosis).
Following on from the data obtained on the use of delayed anastomosis in surgical management of patients with postoperative peritonitis, plans are underway to study delayed anastomosis time, anastomosis type (enteroenterostomy, entero-colonic anastomosis), and temporary and ultimate abdominal closure techniques after programmed relaparotomies.
Conclusion
Obstructive resection of the small bowel with delayed anastomosis in patients with postoperative peritonitis during planned relaparotomies improves surgical treatment outcomes, because the incidence of anastomotic leaks goes down and the mortality rate does not rise. The surgical indications for obstructive resection of the small bowel are as follows: small-bowel perforations, small-bowel anastomotic leakage, small-bowel necrosis or right-sided colonic necrosis, with APACHE-II > 15 points for severity of illness and МPI > 20 points for severity of peritonitis. Placement of the final small-bowel anastomosis in delayed anastomotic repair is recommended when hemodynamic parameters and hemostatic profile of the patient in the intensive care unit are stabilized, suppurative inflammation of the peritoneal cavity is abated and infiltration of the small intestine at the anastomotic site is reduced during programmed relaparotomies.
References
Torer N, Yorganci K, Elker D, Sayek I. Prognostic factors of the mortality of postoperative intraabdominal infections. Infection. 2010;38:255–60. https://doi.org/10.1007/s15010-010-0021-4.
Sartelli M, Griffiths EA, Nestori M. The challenge of post-operative peritonitis after gastrointestinal surgery. Updates Surg. 2015;67(4):373–81. https://doi.org/10.1007/s13304-015-0324-1.
Bensignor T, Lefevre JH, Creavin B, Chafai N, Lescot T, Hor T, Debove C, Paye F, Balladur P, Tiret E, Parc Y. Postoperative peritonitis after digestive tract surgery: surgical management and risk factors for morbidity and mortality, a cohort of 191 patients. World J Surg. 2018;42(11):1–10. https://doi.org/10.1007/s00268-018-4687-6.
Lock JF, Eckmann C, Germer CT. Characteristics of postoperative peritonitis. Der Chirurg. 2016;87(1):20–5. https://doi.org/10.1007/s00104-015-0110-0.
Johnson CC, Baldessarre J, Levison ME. Peritonitis: update on pathophysiology, clinical manifestations, and management. Clin. Infect. Dis. 1997;24(6):1035–45. https://doi.org/10.1086/513658.
Afridi SP, Malik F, Ur-Rahman S, Shamim S, Samo KA. Spectrum of perforation peritonitis in Pakistan: 300 cases Eastern experience. World J Emerg Surg. 2008;3:31. https://doi.org/10.1186/1749-7922-3-31.
Babu RG, Malolan A, Chowdary PB. Ileostomy for non-traumatic ileal perforations: Is this the beginning of the end? Clin Diagn Res. 2016;10(3):23–6. https://doi.org/10.7860/JCDR/2016/18461.7473.
Khalid S, Burhanulhuq, Bhatti AA. Non-traumatic spontaneous ileal perforation: experience with 125 cases. J Ayub Med Coll Abbottabad. 2014;26(4):526–9.
Yanar H, Taviloglu K, Ertekin C, Ozcinar B, Yanar F, Guloglu R, Kurtoglu M. Planned second-look laparoscopy in the management of acute mesenteric ischemia. World J Gastroenterol. 2007;13(24):3350–3.
Regner JL, Kobayashi L, Coimbra R. Surgical strategies for management of the open abdomen. World J Surg. 2012;36(3):497–510. https://doi.org/10.1007/s00268-011-1203-7.
Pauly S, Schulze FP, Horstmann O, Becker H, Grade M, Ghadimi M. Value of one-stage surgical treatment of diffuse peritonitis (relaparotomy on demand): a single-center analysis. Zentralbl Chir. 2013;138(3):289–94. https://doi.org/10.1055/s-0032-1328006.
Van Ruler O, Mahler CW, Boer KR, et al. Comparison of on-demand vs planned relaparotomy strategy in patients with severe peritonitis: a randomized trial. JAMA. 2007;298(8):865–72. https://doi.org/10.1001/jama.298.8.865.
Scriba MF, Laing GL, Bruce JL, Sartorius B, Clarke DL. The role of planned and on-demand relaparotomy in the developing world. World J Surg. 2016;40(7):1558–64. https://doi.org/10.1007/s00268-015-3379-8.
Banasiewicz T, Dziki A, Lampe P, Lorenc Z, Szczepkowski M, Zieliński J, Wallner G. Anastomotic leaks in gastrointestinal surgery and their prevention. Pol Przegl Chir. 2017;89(2):49–56. https://doi.org/10.5604/01.3001.0009.8979.
Morse BC, Simpson JP, Jones YR, Johnson BL, Knott BM, Kotrady JA. Determination of independent predictive factors for anastomotic leak: analysis of 682 intestinal anastomoses. Am J Surg. 2013;206(6):950–5. https://doi.org/10.1016/j.amjsurg.2013.07.017.
Shogan BD, Belogortseva N, Luong PM, et al. Collagen degradation and MMP9 activation by Enterococcus faecalis contribute to intestinal anastomotic leak. Sci Transl Med. 2015;7(286):286ra68. https://doi.org/10.1126/scitranslmed.3010658.
De Graaf JS, van Goor H, Bleichrodt RP. Primary small bowel anastomosis in generalized peritonitis. Eur J Surg. 1996;162(1):55–8.
Ordonez CA, Puyana JC. Management of peritonitis in the critically ill patient. Surg Clin North Am. 2006;86(6):1323–49.
Kotze PG, de Barcelosa IF, Ropelato RV, Coy CSR. Human fibrinogen and thrombin patch for extraluminal protection of intestinal anastomosis. J Coloproctol. 2013;33(3):174–8. https://doi.org/10.1016/j.jcol.2013.08.004.
Demmel N, Muth G, Maag K, Osterholzer G. Prognosescoresbei peritonitis: Mannheimer Peritonitis-Index oder APACHE II? Langenbecks Archiv für Chirurgie. 1994;379:347–52. https://doi.org/10.1007/BF00191581.
Budzyński P, Dworak J, Natkaniec M, Pędziwiatr M, Major P, Migaczewski M, Matłok M, Budzyński A. The usefulness of the Mannheim Peritonitis Index score in assessing the condition of patients treated for peritonitis. Pol Przegl Chir. 2015;87(6):301–6. https://doi.org/10.1515/pjs-2015-0058.
Khan A, Hsee L, Mathur S, Civil I. Damage-control laparotomy in nontrauma patients: review of indications and outcomes. J Trauma Acute Care Surg. 2013;75:365–8. https://doi.org/10.1097/TA.0b013e31829cb65e.
Becher RD, Peitzman AB, Sperry JL, Gallaher JR, Neff LP, Sun Y, Miller PR, Chang MC. Damage control operations in non-trauma patients: defining criteria for the staged rapid source control laparotomy in emergency general surgery. Nord J Emerg Surg. 2016;11:10. https://doi.org/10.1186/s13017-016-0067-4.
Atema JJ, Gans SL, Boermeester MA. Systematic review and meta-analysis of the open abdomen and temporary abdominal closure techniques in nontrauma patients. World J Surg. 2015;39:912–25. https://doi.org/10.1007/s00268-014-2883-6.
Mutafchiyski VM, Popivanov GI, Kjossev KT, Chipeva S. Open abdomen and VAC® in severe diffuse peritonitis. J R Army Med Corps. 2016;162(1):30–4. https://doi.org/10.1136/jramc-2014-000386.
Strobel O, Werner J, Büchler MW. Surgical therapy of peritonitis. Chirurg. 2011;82(3):242–8. https://doi.org/10.1007/s00104-010-2015-2.
Caronna R, Boukari AK, Zaongo D, Hessou T, Gayito RC, Ahononga C, Adeniran S, Priuli G. Comparative analysis of primary repair vs resection and anastomosis, with laparostomy, in management of typhoid intestinal perforation: results of a rural hospital in northwestern Benin. BMC Gastroenterol. 2013;13(1):102. https://doi.org/10.1186/1471-230X-13-102.
Oldenburg WA, Lau LL, Rodenberg TJ, Edmonds HJ, Burger CD. Acute mesenteric ischemia: a clinical review. Arch Intern Med. 2004;164(10):1054–62.
Kiewiet JJ, van Ruler O, Reitsma JB, Boermeester MA. Treatment of secondary peritonitis: slow progress. Ned Tijdschr Geneeskd. 2009;153:A386.
Schikata S, Yamagishi H, Taji Y, Shimada T, Noguchi Y. Single-versus two-layer intestinal anastomosis: a meta-analysis of randomized controlled trials. BMC Surg. 2006;6:1471–6. https://doi.org/10.1186/1471-2482-6-2.
Shaw RS. The ``second look’’ after superior mesenterial embolectomy or reconstruction for mesenteric infarction. current surgical management. Philadelphia: W. B. Sounders Company; 1965.
Schneider TA, Longo WE, Ure T, Vernava AM. Mesenteric ischemia. Acute arterial syndromes. Dis Colon Rectum. 1994;37:1163–74. https://doi.org/10.1007/BF02049824.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the Ethics Committee of the Altai State Medical University and informed consent was obtained from all patients who agreed to participate in the study. All the Ethics Committee members (100%) unanimously approved this study.
Research registration unique identifying number (UIN)
ClinicalTrials.gov ID: NCT03690687.
Rights and permissions
About this article
Cite this article
Zharikov, A.N., Lubyansky, V.G. & Zharikov, A.A. A differentiated approach to repeat small-bowel anastomoses in patients with postoperative peritonitis: a prospective cohort study. Eur J Trauma Emerg Surg 46, 1055–1061 (2020). https://doi.org/10.1007/s00068-019-01084-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-019-01084-7