Abstract
Objectives
Whole-body computed tomography (WBCT) plays an increasingly important role in the diagnostic assessment of trauma room patients. It is still unclear whether its use has led to changes of trauma room procedures and patient outcomes.
Methods
In a retrospective multi-centric study based on the trauma registry of the German Trauma Society (TraumaRegister DGU®), we analysed patients with an ISS ≥ 9 between 2002 and 2013. Two periods of time, i.e. up to 3 years preceding (pre-WBCT) and up to 3 years following the introduction of the WBCT (WBCT-group), were assessed separately for every hospital (TR-DGU Project ID 2014-020).
Results
19,838 patients underwent treatment in 77 hospitals. Of these, 5621 were assigned to the pre-WBCT group and 11,307 to the WBCT group. Basic data did not differ relevantly. The time spent in the trauma room decreased from 77.9 min (pre-WBCT) to 63.3 min (WBCT). Following the introduction of the trauma scan, the number of diagnoses per patient increased from 4.6 to 5.1. The percentage of patients who underwent surgery immediately after the completion of trauma room procedures decreased from 44.5 to 39.1%. There was an increase in mortality from 15.7 to 15.9%.
Conclusions
Routine use of WBCT is not superior to a combination of conventional radiography, ultrasound and focused CT in terms of mortality. The entire process involving the introduction of the trauma scan and the further development of algorithms has caused changes that can be observed in the trauma room setting.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Algorithms are intended to facilitate, standardise and structure decision-making processes. Trauma room algorithms define clear diagnostic and therapeutic priorities that are ultimately directed at improving patient outcome. Diagnostic evaluation is a crucial part of the management of patients in the trauma room setting and helps physicians prioritise and target treatment depending on the injuries identified. Conventional radiography, ultrasound and computed tomography (CT) are imaging modalities that are available in the trauma room. If CT is the only initial imaging modality, CT findings must be available as early as or earlier than the results of conventional radiography and ultrasound. This condition was met in 1998 when technical advances in CT technology led to the introduction of spiral and multi-slice computed tomography (MSCT). This technique allows large volumes of image data to be acquired within a short period of time [1, 2]. In recent years, an increasing number of hospitals have used MSCT to obtain trauma scans (whole-body computed tomography, WBCT) and have introduced WBCT as a standard diagnostic imaging technique [5]. It should be noted, however, that a trauma scan is associated with a high level of radiation exposure and that acute life-threatening conditions can limit the use of diagnostic procedures [3,4,5].
In 2004, Kanz et al. described how WBCT could be integrated into the trauma room algorithms that had been developed at their institution and suggested that their approach should be further developed and validated in a multi-centre study on the basis of the TraumaRegister DGU® [2].
A number of studies that were conducted by different hospitals reported in the past that WBCT reduced trauma room times [3, 6]. In a retrospective study from 2009, Wurmb et al. analysed the time required for the management of patients in the trauma room in a level 1 trauma centre and found that the total treatment time was 82 min for trauma patients who underwent CT after the completion of basic diagnostic procedures including conventional radiography and ultrasound in the trauma room. By contrast, total treatment time was only 47 min for trauma patients who underwent only whole-body MSCT during the initial diagnostic evaluation [3].
It is still unclear, however, whether the introduction of the trauma scan led to changes when it comes to the number of injuries detected, the body parts found to be involved, and patient outcomes. Another aspect to be investigated is the potential influence of the expected higher rates of diagnosis and injury severity on the further indication-dependent management of patients (e.g. no surgery, immediate surgery, surgery after initial stabilisation, transfer to the intensive care unit or a regular ward).
The objective of our retrospective multi-centre study was to analyse data from the TraumaRegister DGU® to assess whether the introduction of the trauma scan led to changes in terms of the number of injuries detected, the body parts affected, the indication-dependent management of patients following the completion of trauma room procedures, and patient outcomes and thus to determine whether trauma room processes before WBCT were different from those after the introduction of the trauma scan as a standard imaging modality. We placed particular emphasis on determining the year in which the trauma scan replaced conventional techniques as the standard diagnostic imaging approach in the trauma room setting individually for every hospital. We did not use a specific year as a general cut-off year for the introduction of WBCT.
Patients and methods
Trauma registry of the German Trauma Society
The trauma registry of the German Trauma Society (TraumaRegister DGU®) provided the data used (TR-DGU Project ID 2014-020).
The TraumaRegister DGU® of the German Trauma Society (Deutsche Gesellschaft für Unfallchirurgie, DGU) was founded in 1993. The aim of this multi-centre database is the pseudonymised and standardised documentation of diagnostic procedures and care for severely injured patients.
Data are collected prospectively in four consecutive time periods from the site of the accident until discharge from hospital: (a) prehospital phase, (b) emergency room and initial surgery, (c) intensive care unit, and (d) discharge. Documentation includes detailed information on demographics, injury patterns, comorbidities, prehospital and inhospital management, the course on the intensive care unit, relevant laboratory findings including data on transfusion, and outcome. Included are patients who are admitted to hospital via the resuscitation room and subsequently receive intensive or intermediate care and patients who arrive at hospital with vital signs and die before admission to the intensive care unit.
The infrastructure for documentation, data management, and data analysis is provided by the Academy for Trauma Surgery (AUC-Akademie der Unfallchirurgie GmbH). Scientific leadership is provided by the Committee on Emergency Medicine, Intensive Care and Trauma Management (Sektion NIS) of the German Trauma Society. Participating hospitals submit their anonymised data to a central database via a web-based application. Scientific data analysis is approved according to a peer-review procedure established by Sektion NIS. The participating hospitals are primarily located in Germany, but a rising number of hospitals of other countries contribute data as well (i.e. Austria, Belgium, China, Finland, Luxembourg, Slovenia, Switzerland, the Netherlands, and the United Arab Emirates). Currently, approximately 25,000 cases from more than 600 hospitals are entered into the database per year.
Participation in the TraumaRegister DGU® is voluntary. For hospitals associated with TraumaNetzwerk DGU®, however, the entry of at least a basic data set is obligatory for reasons of quality assurance [7, 8]. In 2013, Helm et al. reported that, since the creation of the TraumaRegister DGU® in 1993, this registry had proved to be a valuable tool for externally assessing the quality of the management of patients with major trauma and that continuous quality management, which involved identifying a problem, finding a solution and assessing its impact, had improved the quality of patient care in the trauma room of a level 1 trauma centre [9].
Inclusion and exclusion criteria
The study is based on data that were provided between 2002 and 2013 by hospitals that had contributed data to the TraumaRegister DGU® for at least 5 years. In addition, documentation during the period from 1 year preceding and 1 year following the year in which the trauma scan was introduced was required for inclusion. We collected and analysed data only from patients who were admitted to the trauma room with an Injury Severity Score (ISS) greater than or equal to 9 and who either underwent surgery or were transferred to the intensive care unit (ICU) following management in the trauma room or died in the trauma room. In addition, only patients who underwent primary treatment at a regional (level II) or supraregional (level I) trauma centre were included.
Patient groups
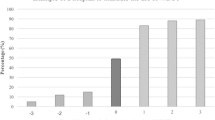
When contributing data to the TraumaRegister DGU®, hospitals can specify the diagnostic procedures performed in the trauma room or operating room settings. They can indicate whether a whole-body CT, abdominal ultrasound, conventional radiography of the chest, pelvis or spine, or focused CT was performed for diagnostic purposes. The time point when whole-body multi-slice CT (i.e. the trauma scan) was introduced in the trauma room setting was determined individually for every hospital included in this study. The year in which the WBCT replaced traditional imaging as the standard diagnostic imaging approach in the trauma room setting was determined individually for every hospital by two independent examiners (MK and HP). When the two examiners disagreed, the opinion of a specialist in biostatistics (RL) was obtained and was the final determination. Up to 3 years before (pre-WBCT group) and up to 3 years after the introduction of the trauma scan (WBCT group) as a standard imaging procedure were analysed and compared (Fig. 1). The year in which the trauma scan was introduced was excluded from analysis since this year was usually a period of transition associated with a mixture of both imaging approaches. A maximum variation of 30% in both the pre-WBCT and the WBCT group provided the basis for decision. In addition, there had to be an increase in the WBCT rate by at least 50% or to at least 60% in the year following the introduction of WBCT when compared to the year preceding the introduction of the trauma scan. On the basis of these inclusion and exclusion criteria, two groups of patients were formed. The pre-WBCT group of patients were managed in the trauma room setting during the 3 years preceding the introduction of the trauma scan as a standard imaging modality and underwent diagnostic procedures such as conventional radiography, abdominal ultrasound and focused CT. The WBCT group consisted of patients who were treated in the trauma room setting during the 3 years following the introduction of whole-body multi-slice CT as the primary diagnostic imaging modality.
Number of trauma scans per year. Data for the years − 3 to − 1 were used to form the pre-WBCT group. Data for the years 1–3 following the introduction of the trauma scan as a standard imaging modality in the trauma room setting were used to form the WBCT group. The year 0 is the year in which WBCT was introduced
Biostatistical methods and data analysis
In consultation with a biostatistician affiliated with the TraumaRegister DGU®, we decided not to test between-group differences for statistical significance since even small differences that were of no clinical relevance were likely to be statistically significant on account of the large number of cases. For this reason, differences of clinical importance were termed “relevant”. The 95% confidence intervals (CI) were calculated.
Results
We were able to analyse 19,838 cases from 77 hospitals. Of these cases, 5621 patients (28.3%) were managed before the routine use of the trauma scan (pre-WBCT group) and 11,307 patients (57.0%) after the introduction of the trauma scan in the trauma room (WBCT group). A total of 2910 patients (14.7%) underwent an imaging procedure in the year in which the trauma scan was introduced and were not included in this analysis.
The mean age of the patients in the pre-WBCT group (43.0 years [42.1–43.9]) was slightly lower than that of the patients in the WBCT group (46.6 years [45.9–47.2]). The majority of patients were male. The mean Injury Severity Score (ISS) remained almost unchanged and was 23.7 [23.1–24.3] before and 23.9 [23.4–24.3] after the routine use of the trauma scan. These results show that there were no relevant differences between the two patient groups in terms of demographics and injury severity (Table 1).
Imaging modalities
The percentage of patients who underwent CT scanning (focused CT, WBCT) increased from 74.0% [73.3–74.6] to 93.3% [92.9–93.6]. At the same time, the percentage of patients who underwent radiography of the chest decreased from 84.2% [83.7–84.7] to 60.3% [59.6–60.9], radiography of the spine from 61.1% [60.4–61.8] to 12.5% [12.1–13.0], and radiography of the pelvis from 68.7% [68.0–69.3] to 46.4% [45.7–47.0]. The percentage of patients who had a Focused Assessment with Sonography in Trauma (FAST) remained almost unchanged (pre-WBCT group: 87.8% [87.4–88.3]; WBCT group: 88.0% [87.6–88.5]) (Fig. 2).
A marked increase in the number of trauma scans after the introduction of WBCT in the trauma room setting. The change in the standard imaging approach is further demonstrated by the decrease in conventional radiography. The number of ultrasound examinations of the abdomen was high and remained almost unchanged during the study period
When radiography and CT were used as imaging modalities, the use of computed tomography alone increased from 13.4% [12.9–13.9] to 40.1% [39.4–40.9] and the use of radiography alone decreased from 29.6% [28.9–30.2] to 5.5% [5.2–5.8]. When both CT and radiography were used as diagnostic tools, the percentage of patients who underwent a combination of these imaging modalities remained unchanged. There was no difference in the sequence in which the two diagnostic procedures were performed.
Time spent in the trauma room
After the introduction of the trauma scan as a standard imaging modality, the mean time to initial CT decreased from 35.1 min [33.6–36.6] to 24.2 min [23.6–24.8].
There was a reduction in the mean total time spent in the trauma room from 77.9 min [75.7–80.2] to 63.6 min [62.0–65.1]. A more detailed analysis of time management is displayed in Table 1.
Patterns of injury
Following the introduction of the trauma scan as a standard imaging modality, the mean number of diagnoses increased from 4.6 [4.5–4.7] to 5.1 [5.0–5.2] per patient. The percentage of patients with serious injuries, i.e. injuries with an Abbreviated Injury Scale (AIS) ≥ 2, increased as well: injuries to the head from 49.2% [48.5–49.9] to 55.2% [54.5–55.9], injuries to the chest from 51.5% [50.8–52.2] to 58.7% [58.0–59.4], and injuries to the spine from 25.7% [25.1–26.4] to 30.4% [29.8–31.1]. By contrast, there was a minor decrease in the percentage of patients with serious injuries to the pelvis (AIS ≥ 2). The percentage of patients with serious abdominal injuries (AIS ≥ 2) remained almost unchanged.
Intra-hospital transfer
Before the trauma scan was introduced as a standard imaging modality, a mean percentage of 44.5% [43.7–45.3] of patients underwent surgery immediately after completion of treatment in the trauma room. After the introduction of the trauma scan, the percentage decreased to 39.1% [38.3–39.9]. Likewise, the percentage of patients who required emergency surgery or died during trauma room management fell from 6.8% [6.4–7.2] to 5.1% [4.7–5.5]. At the same time, the percentage of patients who were directly transferred to the ICU rose from 46.2% [45.4–47.0] to 54.4% [53.6–55.2]. In addition, there was a minor decrease in the percentage of patients whose treatment in the trauma room was discontinued for other reasons (e.g. transfer to a regular ward) from 2.5% [2.3–2.8] to 1.3 [1.2–1.5].
Outcome
Mortality was 15.7% [15.2–16.3] in the pre-WBCT group and 15.9% [15.4–16.4] in the WBCT group. The mortality rate can be compared with the Revised Injury Severity Classification (version II) (RISC II) score, which is calculated to predict mortality. The RISC II score was 15.7 for the pre-WBCT group and 15.2 for the WBCT group (Fig. 3).
Observed mortality rates (grey columns) and 95% confidence intervals for the 3 years (Pre 3, Pre 2 and Pre 1) preceding trauma scan introduction, the year in which the trauma scan was introduced (0), and the 3 years following trauma scan introduction (Post 1, Post 2 and Post 3). Cumulative data for the 3-year period preceding trauma scan introduction (Pre 3 to Pre 1) and for the 3-year period following the change in the trauma room algorithms and the introduction of multi-slice computed tomography (MSCT) of the whole body (Post 1 to Post 3) The transverse bars show predicted mortality rates (RISC II) for the different periods. Red bars indicate that observed mortality was higher than predicted mortality. Green bars indicate that observed mortality was lower than predicted mortality
The mean length of ICU stay decreased by 1.7 days from 10.6 days [10.0–11.2] to 8.9 days [8.6–9.3]. Likewise, the mean length of hospital stay decreased by 3.7 days from 25.3 days [24.1–26.4] to 21.6 days [20.9–22.3].
Discussion
The purpose of our study was to analyse data from the TraumaRegister DGU® to assess whether the introduction of the trauma scan in the trauma room led to major changes in terms of the time spent in the trauma room, the indication-dependent management of patients, intra-hospital transfer, and patient outcome.
We were able to show that the changes in the trauma room algorithm are associated with significant improvements in a number of important parameters such as the time spent in the trauma room, time to initial surgery, and transfer to the ICU. Positive effects were noted during the entire hospital stay until discharge. Similar results were reported by Wutzler et al. [10]. Our results show that one reason for the reduction in trauma room time is the shorter duration of imaging in the WBCT group and thus the faster availability of diagnoses that provide the basis for decisions about further diagnostic procedures and treatment. In a retrospective analysis, Wurmb et al. demonstrated that rapid diagnosis in the trauma room setting was an important component of the high-quality management of polytrauma patients [3].
Trauma scans were found to be associated with a higher rate of diagnosis than a combination of conventional radiography and focused CT. In our analysis, we found a clear increase in the number of detected injuries for almost all body parts investigated. This applies in particular to injuries to the head, chest and spine. The number of injuries that were detected in the region of the abdomen remained unchanged. Sierink et al. regarded these additionally detected injuries as incidental findings that would have remained undiscovered without the use of whole-body CT. They reported that a total of 186 incidental findings were identified in 143 of 321 patients who underwent WBCT in the trauma room. These findings were grouped into three categories, depending on their severity. The majority of incidental findings were found to have no relevance to the further management of patients [11]. In 2012, Venugopal et al. too reported that WBCT identified unexpected findings in 66% of emergency department trauma patients and that WBCT results differed from clinical findings in 73% of these patients [12]. In a very recent study, Linder et al. found that high-energy trauma patients who were mentally alert, who were not intoxicated and who had only minor injuries did not benefit from WBCT. The risk of missing relevant injuries is low whereas the risk of developing radiation-induced cancer is significantly increased in young patients [13].
On the whole, we found in our study that the introduction of the trauma scan as a standard diagnostic procedure in the trauma room setting was accompanied by changes in patient management processes. They were associated with some decreases in the rate of the surgical procedures that were performed immediately after trauma room management and in ICU and regular ward length of stay.
Outcome
Contrary to what was generally expected, the mortality rate reported for the initial years following the introduction of the trauma scan did not improve when compared with the rate that was calculated for the investigated years preceding the routine use of WBCT. A comparison of the RISC II scores for the two periods even showed that observed mortality was higher than predicted mortality. Version II of the RISC score was developed when the observed mortality was found to be below the mortality rate that was predicted on the basis of RISC. RISC II now includes a few more relevant prognostic factors and can be calculated even for patients for whom some data are missing [14].
By contrast, Ruchholtz et al. analysed data that had been entered into the TraumaRegister DGU® during the period from 1993 to 2005 and reported a significant decrease in the mortality of trauma patients [15]. A comparison of our study and the study by Ruchholtz et al. showed that there was only a 3-year overlap between the two long study periods and that there were differences in inclusion criteria (e.g. injury severity).
Hilbert et al. reported differences in mortality rates between trauma centres [16]. The mortality rate reported for the top ten trauma centres was only half as high as that reported for the bottom ten centres. This study too was based on data from the TraumaRegister DGU®. The years covered by the study (from 2004 to 2007) are included in our study period. There are, however, a number of differences in inclusion criteria.
We found that the length of stay in the ICU and in hospital decreased. Weninger et al., who conducted a retrospective analysis in 2007, reported a similar result. They too observed a decrease in the length of ICU stay and hospital stay. Moreover, they observed that patients who underwent MSCT had fewer complications such as multi-organ failure than patients who were managed before the introduction of MSCT. Weninger et al. too compared two groups. One group of patients underwent diagnostic procedures such as conventional radiography, FAST and focused CT, the other group underwent whole-body multi-slice CT [6]. We obtained similar results on the basis of an analysis that was multi-centred and in which the time point when WBCT was introduced in the trauma room setting was determined individually for every hospital.
On the whole, our results confirm once again that the use of the trauma scan for almost all trauma room patients (i.e. trauma room patients with an ISS ≥ 9) is not sufficient to improve survival as a parameter of outcome. This may be attributable to the group of patients with minor injuries since Huber-Wagner et al. reported that WBCT increased the probability of survival especially in severely and critically injured patients [17, 18]. Sierink et al. conducted a prospective randomised multi-centre study and investigated outcome and the time spent in the trauma room [19]. The study included 1083 trauma patients (mean ISS = 20) who were managed between 2011 and 2014. These patients underwent either immediate WBCT or conventional imaging and selective CT scanning. The authors found no significant difference in 30-day mortality (16% for both imaging approaches). The same applies to results obtained in a subgroup analysis for patients with polytrauma and patients with traumatic brain injury. Similar to our study, Sierink et al. reported that the primary use of WBCT led to a significant reduction in the time spent in the trauma room from 72 to 63 min.
Limitations
One limitation of our study was our method of determining the year in which the trauma scan was introduced as a standard imaging modality. For some hospitals, it was difficult to identify a clear increase in the annual number of WBCT scans and it was impossible to establish whether the trauma scan had been introduced at the beginning or the end of the year identified. The exact time point, however, has a considerable influence on the number of cases and thus on what year we considered to represent the introduction of the trauma scan. Since we examined a very large number of cases and did not include the year of introduction in our analysis, this limitation is likely to play only a minor role.
The introduction of the trauma scan can be assumed to have led to changes and improvements in hospital algorithms. As a result, the changes that we observed were not necessarily caused by the introduction of the trauma scan alone but rather by a combination of the trauma scan and associated modifications of trauma room processes [3]. The entire process is thus responsible for changes in the management of patients in the trauma room setting.
On the one hand, using different inclusion criteria, e.g. only intubated and mechanically ventilated patients or vice versa only spontaneously breathing patients the results of our study turn out differently. On the other hand, the used inclusion criteria fit from our point of view best with the treatment reality in German trauma rooms.
Conclusions
Our study shows that the trauma scan is not superior to a combination of conventional radiography, ultrasound and focused CT in terms of mortality in a non-selected population of patients (ISS ≥ 9). Against this background, more importance should be placed on decision trees that are independent of imaging modalities and allow trauma team leaders to decide on an individual basis whether a patient is a candidate for a trauma scan. Our study also showed, however, that the introduction of the trauma scan as a standard imaging modality led to a relevant reduction in almost all trauma room processes and enabled trauma teams to make faster treatment decisions. We observed an increase in the number of diagnoses per patient. Since we were also able to prove that the introduction of the trauma scan was associated with a relevant decrease in the length of ICU stay and hospital stay, trauma teams should adhere to current practices and procedures until the aforementioned decision trees are available.
References
Linsenmaier U, Krotz M, Hauser H, Rock C, Rieger J, Bohndorf K, et al. Whole-body computed tomography in polytrauma: techniques and management. Eur Radiol. 2002;12:1728–40.
Kanz KG, Korner M, Linsenmaier U, Kay MV, Huber-Wagner SM, Kreimeier U, et al. Priority-oriented shock trauma room management with the integration of multiple-view spiral computed tomography. Unfallchirurg. 2004;107:937–44.
Wurmb T, Balling H, Fruhwald P, Keil T, Kredel M, Meffert R, et al. Polytrauma management in a period of change: time analysis of new strategies for emergency room treatment. Unfallchirurg. 2009;112:390–9.
Donaubauer B, Fakler J, Gries A, Kaisers UX, Josten C, Bernhard M. Interdisciplinary management of trauma patients: update 3 years after implementation of the S3 guidelines on treatment of patients with severe and multiple injuries. Anaesthesist. 2014;63:852–64.
Topp T, Lefering R, Lopez CL, Ruchholtz S, Ertel W, Kuhne CA. Radiologic diagnostic procedures in severely injured patients—is only whole-body multislice computed tomography the answer? Int J Emerg Med. 2015;8:1–6.
Weninger P, Mauritz W, Fridrich P, Spitaler R, Figl M, Kern B, et al. Emergency room management of patients with blunt major trauma: evaluation of the multislice computed tomography protocol exemplified by an urban trauma center. J Trauma. 2007;62:584–91.
Academy of Traumatology. http://www.traumaregister-dgu.de/de/startseite_tr.html. Accessed 2 Nov 2017.
TraumaRegister DGU®. 20 years TraumaRegister DGU®: development, aims and structure. Injury 2014; 45(Suppl 3):S6–13.
Helm M, Bitzl A, Klinger S, Lefering R, Lampl L, Kulla M. The TraumaRegister DGU® as the basis of medical quality management. Ten years experience of a national trauma centre exemplified by emergency room treatment. Unfallchirurg. 2013;116:624–32.
Wutzler S, Westhoff J, Lefering R, Laurer HL, Wyen H, Marzi I, et al. Time intervals during and after emergency room treatment. An analysis using the trauma register of the German Society for Trauma Surgery. Unfallchirurg. 2010;113:36–43.
Sierink JC, Saltzherr TP, Russchen MJAM, de Castro SMM, Beenen LFM, Schep NWL, et al. Incidental findings on total-body CT scans in trauma patients. Injury. 2014;45:840–4.
Venugopal K, Kinghorn AF, Emordi CE, Atkinson PR, Kendall RJ. An evaluation of the use of whole-body computed tomography in trauma patients at a United Kingdom trauma centre. Eur J Emerg Med. 2012;19:193–5.
Linder F, Mani K, Juhlin C, Eklöf H. Routine whole body CT of high energy trauma patients leads to excessive radiation exposure. Scand J Trauma Resusc Emerg Med. 2016;24:7.
Lefering R, Huber-Wagner S, Nienaber U, Maegele M, Bouillon B. Update of the trauma risk adjustment model of the TraumaRegister DGU™: the Revised Injury Severity Classification, version II. Crit Care. 2014;18:476.
Ruchholtz S, Lefering R, Paffrath T, Oestern HJ, Neugebauer E, Nast-Kolb D, et al. Reduction in mortality of severely injured patients in Germany. Dtsch Arztebl. 2008;105:225–31.
Hilbert P, Lefering R, Stuttmann R. Trauma care in Germany: major differences in case fatality rates between centers. Dtsch Arztebl Int. 2010;107:463–79.
Huber-Wagner S, Lefering R, Qvick LM, Körner M, Kay MV, Pfeifer KJ, Reiser M, Mutschler W, Kanz KG; On behalf of the Working Group on Polytrauma of the German Trauma Society. Effect of whole-body CT during trauma resuscitation on survival: a retrospective, multicentre study. Lancet. 2009;373:1455–61.
Huber-Wagner S, Biberthaler P, Häberle S, Wierer M, Dobrittz M, Rummeny EJ, van Griensven M, Kanz KG, Lefering R; Trauma Registry of the German Society for Trauma Surgery. Whole-body CT in haemodynamically unstable severely injured patients—a retrospective, multicentre study. PLoS One. 2013;8:e68880. https://doi.org/10.1371/journal.pone.0068880.
Sierink JC, Treskes K, Edwards MJR, Beuker BJA, den Hartog D, Hohmann J, Dijkgraaf MGW, Luitse JSK, Beenen LFM, Hollmann MW, Goslings JC. Immediate total-body CT scanning versus conventional imaging and selective CT scanning in patients with severe trauma (REACT-2): a randomised controlled trial. Lancet. 2016;388:673–83.
Acknowledgements
The two first authors, Hans-Georg Palm and Martin Kulla, state that major parts of this article are based on a doctoral dissertation that will be submitted to the Medical School of the University of Ulm by Magdalena Wettberg. The authors would like to thank Klaus Efinger (Bundeswehrhospital Ulm, Department of Radiology, German Armed Forces) for his valuable comments and suggestions regarding the analysis and interpretation of data. Finally, we would like to thank Barbara Isenberg of the German Federal Office of Languages for its assistance in translating our manuscript.
Author information
Authors and Affiliations
Consortia
Contributions
Patricia Lang, Martin Kulla and Hans-Georg Palm designed the study. Rolf Lefering analysed and interpreted the data with Martin Kulla, Patricia Lang, Bendikt Friemert, Magdalena Wettberg and Hans-Georg Palm. Martin Kulla and Hans-Georg Palm wrote the manuscript. Benedikt Friemert, Patricia Lang and Martin Kulla were providing scientific support and valuable advice working on the manuscript. All authors proofread the manuscript and revised it critically. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Hans-Georg Palm, Martin Kulla, Magdalena Wettberg, Rolf Lefering, Benedikt Friemert and Patricia Lang declare that they have no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Availability of data and materials
All data that are relevant for the study are included in this published article. Further datasets analysed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
The present study is in line with the publication guidelines of the TraumaRegister DGU® and registered as TR-DGU Project ID 2014-020. As register data are assessed anonymously, individual informed consent is not required.
Rights and permissions
About this article
Cite this article
Palm, HG., Kulla, M., Wettberg, M. et al. Changes in trauma management following the implementation of the whole-body computed tomography: a retrospective multi-centre study based on the trauma registry of the German Trauma Society (TraumaRegister DGU®). Eur J Trauma Emerg Surg 44, 759–766 (2018). https://doi.org/10.1007/s00068-017-0870-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-017-0870-y