Abstract
Background and Purpose
Differentiating Abusive Head Trauma (AHT) from Non-abusive Head trauma (NAHT) has profound clinical prognostic and legal implications, as certain imaging findings can individually be more suggestive of NAHT, while others are more suggestive of AHT. This study was set out to evaluate for an association between the various imaging findings in AHT with outcome.
Material and Methods
Over 7-years, 55 children (age 0-4 years’) with head trauma and magnetic resonance imaging (MRI) were included as either: abusive (n = 16), non-abusive (n = 35), or indeterminate (n = 4). Two pediatric neuroradiologists jointly reviewed the imaging. The frequency of imaging findings and their association with ≥6 months’ outcome were calculated.
Results
Comparing abusive versus non-abusive head trauma, complex subdural hematoma was present in 81% (n = 13/16) and 29% (n = 10/35), hypoxic-ischemic injury in 44% (n = 7/16) and 6% (n = 2/35), and diffuse axonal injury in 12% (n = 2/16) and 26% (n = 9/35), respectively. Susceptibility-weighted imaging (SWI) retinal hemorrhages were absent in non-abusive trauma (0/35), but present in 44% (n = 7/16) of the abusive group. In abuse, simple subdural hematomas were absent. Significant associations were found between the presence of abusive trauma with both hypoxic ischemic insult (OR = 12.83, p = 0.0024) and complex subdural hematoma (OR = 10.83, p = 0.0007). The presence of hypoxic ischemic injury (HII) did correlate significantly with clinical outcome (p = 0.017), while retinal hemorrhages on SWI and complex subdural hematoma did not (p = 0.1696-p = 0.2496).
Conclusion
Neuroimaging findings can be helpful in discriminating these two conditions on presentation, as well as in helping solidify the suspicion of AHT. Regarding eventual outcome in AHT, the most important predictor is clearly HII.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Traumatic brain injury (TBI) is a leading cause of disability and death in children and assessing the severity of the injury is critical in predicting long-term outcome [1]. The severity and outcome are typically more severe in abusive head trauma (AHT) than in nonabusive head trauma (NAHT) if occurring at the same age [2]. Several factors generally portend a worse outcome in both entities, but the most import overall is the degree of initial injury severity [2].
As a limited number of clinical signs express the degree of underlying neuronal damage in children, radiologic findings commonly used by clinicians to assess the severity and extent of injury include, but are not limited to, assessing the presence of hypoxic ischemic injury (HII), diffuse axonal injury (DAI) or cranial hemorrhage [3]. The presence of such findings correlates with the clinical outcome in AHT [4]. As AHT and NAHT may have some overlap on imaging, it is vital to recognize which findings are more suggestive of AHT.
Differentiating AHT from NAHT has profound clinical prognostic and legal implications, as certain imaging findings can individually be more suggestive of NAHT, while others are more suggestive of AHT [5,6,7]; however, there is some overlap in imaging findings that may be found in either clinical scenario, albeit less commonly in one versus the other. While AHT is a clinicolegal determination that may only be confirmed by law enforcement via a confession or witnessed event, perhaps imaging patterns can help solidify the clinical impression. Hence, this study set out to evaluate an association between the various imaging findings in AHT and outcome. Our hypothesis was that certain magnetic resonance imaging (MRI) findings would be more likely in AHT, and that some of those findings could correlate with outcome.
Material and Methods
Patient Selection
This retrospective study was approved by the local institutional review board. The radiology information system of the local level I trauma center was reviewed for the 7‑plus year period between 2 January 2008 and 11 January 2015 for the terms “head trauma”, “TBI”, “nonaccidental” and “abuse” on reports of MRI examinations of the head in children between 0–4 years old; a total of 59 patients were found. The MRI images degraded by motion artifacts (n = 4) were excluded, whereas the remaining 55 patients were included in the study for the imaging review.
Patients were categorized by the child abuse team’s clinical assessment in the electronic medical record (in combination with the legal assessment) as to whether they had either: (1) suffered NAHT (witnessed trauma such as motor vehicle accident, confirmed mechanism, or other already documented accidental injuries), (2) AHT (based on a legal conviction or confession), or (3) as indeterminate. Notably, children classified as indeterminate were those that had been considered clinically highly suspicious for AHT, but a definitive determination had not been reached, typically lacking legal data, such as a confession or conviction. In this respect, separately from the clinicolegal impression, a radiologic impression of NAHT versus AHT was also formed by consensus, with the neuroradiologists being blinded to the clinical data, in order to eventually compare to the clinical impression.
Patient Demographics
A total of 55 patients were included for imaging review, consisting of 30 males and 25 females, with a mean age of 16.46 months (±14.27). There were 16 patients (29%) in the AHT group, 35 patients (64%) in the NAHT group, and 4 (7%) in the indeterminate group. The mean age in the AHT group was 11.15 months (±9.77), and in the NAHT group was 19.06 months (±15.65). Notably, the most common causes of NAHT were motor vehicle accidents 60% (n = 21), followed by falls 40% (n = 14).
Image Acquisition
The MRI examinations over the study’s time period were acquired with both 1.5 T and 3 T (Intera; Philips Healthcare, Best, The Netherlands) scanners. Of the 55 included patients, 92% (n = 51) were imaged on a 3 T magnet, and the remaining 8% (n = 4) were obtained with a 1.5 T magnet. The brain MRI protocol for children with TBI included a three-dimensional (3D) acquisition of 1.0 mm isotropic spoiled gradient echo T1-weighted imaging (T1WI) sequence with axial and coronal reconstructions, axial and coronal T2-weighted imaging (T2WI), axial and sagittal fluid-attenuated inversion recovery (FLAIR), susceptibility-weighted imaging (SWI) and axial diffusion-weighted imaging (DWI) without the administration of intravenous contrast medium.
Image Analysis
Both the MRI (n = 55 within 1 week of presentation) and computed tomography (CT) images (n = 51/55 who had a CT scan available within ≤1 week of the MRI) were reviewed by two neuroradiologists, with 7 and 15 years of pediatric neuroradiology experience, respectively (DN, AM), via consensus review. The MRI images were evaluated for the presence of retinal hemorrhage (RH), DAI, HII, subdural hematoma and contusions. Dilated funduscopic examination (DFE) reports in the electronic medical records were also checked for the presence of RH (DFE-RH) and DWI was checked for the presence of HII, with T2WI and FLAIR evaluated for contusional edema. The SWI was used to evaluate for RH or hemorrhagic DAI. The initial presentation CT was used to evaluate for the presence of calvarial fracture, epidural hematoma, or subdural hematoma; a subdural hematoma was defined as being complex if it was either bilateral, had differing internal densities or signal intensities, or had a neomembrane web, while it was called simple if the hematoma was unilateral, had homogeneous signal intensity, and did not exhibit the other aforementioned features of a complex subdural hematoma (cSDH). Notably, CT was the preferred modality to evaluate for a calvarial fracture (n = 51/55), but was not considered necessary for inclusion in this study; thus, plain films (n = 4/55) were used to check for fracture in the minority of cases. In addition to brain MRI and head CT images, other available plain X-ray film and CT images were evaluated for the presence of extracranial imaging findings.
Clinical Outcome Evaluation, Scoring
Clinical outcome was based on abuse specialist’s clinical assessment in follow-up visits. There were 5 categories of outcome used for the >6 month long-term outcome scoring. This scale was based on the pediatric cerebral performance category scale [8], which consisted the following:
-
Grade 1: return to clinical baseline, including all age-appropriate activities,
-
Grade 2: mild persistent neurologic deficit, meaning the patient is able to interact in most age-appropriate activities but may have a mild neurologic deficit,
-
Grade 3: moderate persistent neurologic deficit, i. e. enough function to perform age-appropriate activities but with substantial cognitive impairment,
-
Grade 4: severe outcome, meaning the patient is conscious but entirely dependent on others for daily support due to severely impaired brain function,
-
Grade 5: death or long-term coma.
Statistical Analysis
A biostatistician performed all analyses via SAS software (v. 9.3; SAS Institute, Cary, NC, USA). For statistical purposes, the two groups of patients compared were NAHT versus AHT. The indeterminate group was not included in statistical calculations. Group comparisons of imaging findings in NAHT versus AHT were performed via two-sample t-tests for continuous variables, or Fisher’s exact test for categorical variables. Odds ratios (OR) and 95% confidence intervals (CI) were also calculated for binary (positive versus negative) intracranial findings. In the NAHT cohort, associations were also calculated between the presence of positive image findings and outcome severity scores, using a Wilcoxon test. All p-values were two-sided, with p < 0.05 being set as the threshold for what was considered to be statistically significant.
Results
Being blinded to the clinical and legal data, and based solely on imaging findings, the radiologic impression was AHT in 8 (15%), NAHT in 42 (76%) and indeterminate in 5 (9%) of the 55 patients. Regarding the radiologic impressions of whether or not AHT was present based on the MRI and CT findings, moderate agreement was found between the clinicolegal and radiologic impressions (k = 0.53, p < 0.0001).
Prevalence of Cranial and Orbital Findings in AHT and NAHT
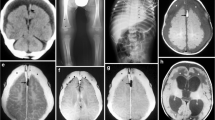
The prevalence and statistical differences of various intracranial findings in AHT versus NAHT (Table 1) are provided. As demonstrated in the table, there were statistically significant associations found between the presence of AHT with respect to the findings of RH (p < 0.0001), HII (p = 0.0024), and cSDH (p = 0.0007). The highest ORs of having AHT were found with the presence of DFE-RH (OR = 36.30), HII (OR = 12.83), or cSDH (OR = 10.83). It is important to note that no patient was positive for SWI-RH in the NAHT group; however, DFE was positive for RH in 2/35 (6%) of NAHT and 11/16 (69%) of AHT patients. No patient was positive for simple subdural hematoma (sSDH) in the AHT group. Additionally, DAI was infrequent, being present in only 12% (2/16) of those children in AHT. Notably, all 6 patients that had each of the three following findings together were deemed to have AHT: SWI-RH, HII, and cSDH. Representative findings are demonstrated in Fig. 1, 2, 3, 4 and 5.
A 34-month-old female with NAHT and sSDH after a motor vehicle accident (negative for skull fracture). On NECT (a), a simple SDH (sSDH, arrows) has uniform hyperdensity, which was also homogeneously hyperintense on 3 T FLAIR (b), T1WI (c), and SWI (d) 1 day later. Note the lack of RH within the posterior globe (dotted arrows) on SWI
A 20-month-old male with DAI and sSDH in NAHT from motor vehicle accident. The NECT (not shown) raised the question of multifocal edema. The 3 T MRI 2 days later demonstrates multifocal DAI (thin arrows), some being hemorrhagic, with contusions (asterisks) of the superior cerebellar vermis, as shown on FLAIR (a), SWI (b), and DWI (c). No RHs were seen in the orbit (dotted arrows) on SWI. On sagittal T1WI (d), homogeneously T1-bright sSDH’s are noted (arrows). On 2‑year follow-up, the child’s seizures continued, with persistent left hemiparesis
A 13-month-old female with cSDH, HII, and RH from AHT. Initial NECT (a), depicts a mixed, complex density cSDH (arrows) underlying a calvarial fracture. On a 3 T MRI 2 days later, T2WI (b) and DWI (c) shows predominantly right-sided cerebral swelling and reduced diffusivity indicative of mostly unilateral HII, being most consistent with AHT. On SWI (d), a single, punctate right RH is noted (dotted arrow), confirmed by DFE; note the lack of hemorrhagic DAI. This child did not develop sensory or motor deficits, but did have persistent seizures
A 4‑month-old female with RH and cSDH’s from AHT. The NECT (not shown), showed bilateral hypodense subdural collections (arrows), without skull fracture. A 3 T MRI 2 days later showed no evidence of HII on DWI (not shown), but there are cSDHs (arrows) on axial T2WI (a, b) and SWI (c, d); note the darker components posteriorly (▪▪) on SWI. On SWI, a left RH is noted (dotted arrows), which were also present clinically on DFE. Also on SWI, at a higher level, note a potential neomembrane on the left (small arrow, d). This child did not suffer any neurologic sequela; a 2-year clinical follow-up found normal development for age
A 41-month-old male with cSDH and HII from AHT, but being a false negative for RH on SWI. In an acutely encephalopathic child, initial NECT (a) demonstrates a mixed-density cSDH (arrows) without calvarial fracture, but with right cerebral hemispheric swelling. On 3 T MRI the next day, FLAIR (b) and DWI (not shown) with apparent diffusion coefficient (ADC) map (c) confirm diffuse hemispheric swelling with mostly unilateral HII. The SWI (d) depicts a false negative for RH (dotted arrows), as small RH’s were noted on DFE. This child died 2 weeks after presentation
Of the 4 patients in the indeterminate group, 2 (50%) had cSDH and 1 (25%) had HII. None of the 4 patients had RH or other cranial findings.
Prevalence of Extracranial Imaging Findings
As seen in Table 2, a variety of extracranial imaging findings were observed in the AHT group. The most common extracranial imaging finding was rib fractures. Of 16 AHT patients, 5 (31%) had rib fractures, 4 (80%) being bilateral and multiple (greater than 3 levels). Of the four patients within the indeterminate group, one patient had a single rib fracture and another had a right distal humeral metaphyseal fracture. The remaining two patients did not have any extracranial traumatic injury. In the NAHT group, different types of extracranial imaging findings were observed, including a metatarsal fracture, pubic ramus fracture, clavicular fracture and diastasis of symphysis pubis.
Outcome
The follow-up data ≥6 months after presentation was available for all 16 patients in the AHT group. Of these 16 patients, 3 (19%) died, 2 (12%) suffered severe neurologic impairment, 4 (25%) had moderate neurologic impairment, 4 (25%) had mild impairment, and 3 (19%) returned to baseline. A statistically significant association was found in AHT patients between the outcome severity and the presence of HII (p = 0.0170), but not with the presence of either cSDH or SWI-RH (p = 0.249 and p = 0.169, respectively).
Discussion
Imaging plays a very important role in the characterization of pediatric head trauma. In daily practice, suspicion of abusive head trauma is mostly based on imaging findings and experience of the clinician. In this retrospective study, we have demonstrated that the presence of certain cranial MR imaging findings, such as RH, cSDH and HII favor AHT over NAHT. Of these findings, HII is the only finding that correlates with the long-term outcome severity.
The detection of RH is vital in the scenario of suspected AHT, as RH can be a characteristic finding in AHT; rarely, RH occurs in NAHT as well [6, 7]. Regarding the presence of HII, recent literature has confirmed that the most severe clinical and histologic manifestations of AHT are indeed related to HII [8, 9]. Meanwhile, DAI occurs infrequently in only a minority of patients with suspected AHT, as confirmed in the current study, which is in contrast to hypotheses of older literature which had theorized that the presence of DAI was an indicator of both outcome as well as etiology (i. e. the presence of DAI was suggestive of AHT) [8, 9]. Recent studies focusing on outcome have demonstrated that the severity of outcome in AHT relates to the mechanism of injury with the most severe outcomes involving HII, especially if HII is combined with DAI-related microhemorrhages (found in only a minority of AHT) [10, 11]. Accordingly, in a recent neuropathological study by Matschke et al. HII-related necrosis was the dominant pathological finding in children with AHT who underwent autopsy [12]. Hence, with respect to outcomes in AHT, the current study corroborates the findings of recent studies, in that the presence of HII correlates with outcome if AHT is present.
There are several proposed reasons for why AHT contributes so heavily to outcome in such children. One theory suggests that AHT children are exposed to chronic, repeated trauma with resultant hypoxemia, which puts them at a greater overall risk for HII [13]. Another theory regarding an exacerbator factor for HII in AHT is that a higher risk of respiratory failure exists in AHT children secondary to less mature airway protective reflexes; accordingly, higher risks of respiratory failure and intubation have been noted following AHT in comparison to NAHT [14, 15]. This would be consistent with studies showing that patterns of diffuse HII on DW MRI have poor outcomes in both children and adults with HII, regardless of etiology [16,17,18,19]. Interestingly, a subtype of AHT with unilateral or mostly unilateral hemispheric involvement may have slightly better survival, but still with severe residual neurologic deficits ([10, 16, 17]; Figs. 3 and 5). In this respect, 3/7 patients in this study with HII from the AHT group (i. e. suspicious for AHT) suffered a mostly unilateral insult, a characteristic found more often in AHT than NAHT. While the mechanism for unilateral or mostly unilateral HII is still unknown, one theory involves transient vascular compression, whether related to hyper-flexion/extension involved in shaking, strangling, or from blunt cranial impact [16,17,18,19].
Regarding the presence of subdural hematomas, cSDHs are perhaps the most frequently described imaging findings in infants with AHT [9]. As such, the current study found a significant association and high OR between the presence of cSDH and AHT. Accordingly, a meta-analysis of extra-axial hemorrhage in AHT showed that cSDH was the type of hemorrhage most strongly associated with AHT [20]. When SDHs of mixed attenuation are discovered in victims of AHT, the most commonly cited explanation has been repeated episodes of head injury [21, 22]. The mixed-density on CT may reflect the combination of high-attenuation blood from acute hemorrhage or clot retraction and lower density fluid from unclotted blood, serum, or cerebrospinal fluid (CSF) [23, 24]. It is postulated that the re-rupture of fragile neovessels in an organizing subdural membrane may explain this mixed-density hematoma; similarly, in adults, a cSDH (mixed-density) may result from recurrent hemorrhage into a chronic SDH in the absence of traumatic head injury [25, 26]; however, unlike adults, spontaneous re-bleeding into a chronic SDH is much less common in infants. Therefore, many authors believe that a heterogeneous, mixed-density SDH in an infant implies an acute-on-chronic head injury, being a pattern suggestive of repetitive head injury [27, 28]. Regardless of the physiologic mechanism, this study confirms that cSDHs are much more likely in AHT, while homogeneous density/intensity sSDHs were present only in NAHT [29].
There are several limitations of this study, including the retrospective nature; however, due to the nature of this phenomenon it is almost impossible to perform prospectively. In particular, to make a definitive diagnosis of abuse may necessitate years of investigation and following a victim’s course, where a confirmed diagnosis or conviction may never be obtained (as was the case in four patients in this study). A second potential limitation is that the overall number of NAHT patients in a population would be expected to be much larger than the overall number with AHT; thus, a selection bias for more severe findings in either entity could result when similar numbers of patients undergo MRI for both entities, although NAHT is overall more common. A third limitation of this study may be the use of two different MRI field strengths, which could have theoretically lowered the sensitivity of SWI in detecting RH. The lack of sSDH in the AHT group may raise the question of some referral bias. Finally, the relatively low number of definitive cases of AHT (n = 16) and difference in sample size could be a limitation.
Conclusion
The presence of either RHs on SWI or cSDH and HII is much more likely to occur in AHT, as compared to NAHT, while both sSDHs and DAI are much more likely to occur in NAHT. Thus, the abovementioned neuroimaging findings can be helpful in discriminating these two conditions on presentation, as well as in helping solidify the suspicion of AHT. Regarding eventual outcome in AHT, the most important predictor is clearly HII. Prospective studies could confirm the likelihood that the triad of SWI-RH, HII, and cSDH is highly indicative of AHT.
References
Schutzman SA, Greenes DS. Pediatric minor head trauma. Ann Emerg Med. 2001;37(1):65–74.
Chevignard MP, Lind K. Long-term outcome of abusive head trauma. Pediatr Radiol. 2014;44(Suppl 4):548–58.
Sigmund GA, Tong KA, Nickerson JP, Wall CJ, Oyoyo U, Ashwal S. Multimodality comparison of neuroimaging in pediatric traumatic brain injury. Pediatr Neurol. 2007;36(4):217–26.
Foerster BR, Petrou M, Lin D, Thurnher MM, Carlson MD, Strouse PJ, Sundgren PC. Neuroimaging evaluation of non-accidental head trauma with correlation to clinical outcomes: a review of 57 cases. J Pediatr. 2009;154(4):573–7.
Jenny C, Hymel KP, Ritzen A, Reinert SE, Hay TC. Analysis of missed cases of abusive head trauma. JAMA. 1999;282(1):29.
Kemp AM, Jaspan T, Griffiths J, Stoodley N, Mann MK, Tempest V, Maguire SA. Neuroimaging: what neuroradiological features distinguish abusive from non-abusive head trauma? A systematic review. Arch Dis Child. 2011;96(12):1103–12.
Kivlin JD. A 12-year ophthalmologic experience with the shaken baby syndrome at a regional children’s hospital. Trans Am Ophthalmol Soc. 1999;97:545–81.
Geddes JF, Hackshaw AK, Vowles GH, Nickols CD, Whitwell HL. Neuropathology of inflicted head injury in children. I. Patterns of brain damage. Brain. 2001;124(7):1290–8.
Duhaime AC, Alario AJ, Lewander WJ, Schut L, Sutton LN, Seidl TS, Nudelman S, Budenz D, Hertle R, Tsiaras WI, Loporchio S. Head injury in very young children: mechanisms, injury types, and ophthalmologic findings in 100 hospitalized patients younger than 2 years of age. Pediatrics. 1992;90(2 Pt 1):179–85.
Maguire SA, Watts PO, Shaw AD, Holden S, Taylor RH, Watkins WJ, Mann MK, Tempest V, Kemp AM. Retinal haemorrhages and related findings in abusive and non-abusive head trauma: a systematic review. Eye (Lond). 2013;27(1):28–36.
Haviland J, Russell RI. Outcome after severe non-accidental head injury. Arch Dis Child. 1997;77(6):504–7.
Matschke J, Büttner A, Bergmann M, Hagel C, Püschel K, Glatzel M. Encephalopathy and death in infants with abusive head trauma is due to hypoxic-ischemic injury following local brain trauma to vital brainstem centers. Int J Legal Med. 2015;129(1):105–14.
Parizel PM, Ceulemans B, Laridon A, Ozsarlak O, Van Goethem JW, Jorens PG. Cortical hypoxic-ischemic brain damage in shaken-baby (shaken impact) syndrome: value of diffusion-weighted MRI. Pediatr Radiol. 2003;33(12):868–71.
Squier W. The “Shaken baby” syndrome: pathology and mechanisms. Acta Neuropathol. 2011;122(5):519–42.
Greiner MV, Lawrence AP, Horn P, Newmeyer AJ, Makoroff KL. Early clinical indicators of developmental outcome in abusive head trauma. Childs Nerv Syst. 2012;28(6):889–96.
Tanoue K, Aida N, Matsui K. Apparent diffusion coefficient values predict outcomes of abusive head trauma. Acta Paediatr. 2013;102(8):805–8.
Ichord RN, Naim M, Pollock AN, Nance ML, Margulies SS, Christian CW. Hypoxic-ischemic injury complicates inflicted and accidental traumatic brain injury in young children: the role of diffusion-weighted imaging. J Neurotrauma. 2007;24(1):106–18.
Goldsmith W, Plunkett J. A biomechanical analysis of the causes of traumatic brain injury in infants and children. Am J Forensic Med Pathol. 2004;25(2):89–100.
McKinney AM, Thompson LR, Truwit CL, Velders S, Karagulle A, Kiragu A. Unilateral hypoxic-ischemic injury in young children from abusive head trauma, lacking craniocervical vascular dissection or cord injury. Pediatr Radiol. 2008;38(2):164–74.
Maguire SA, Kemp AM, Lumb RC, Farewell DM. Estimating the probability of abusive head trauma: a pooled analysis. Pediatrics. 2011;128(3):e550–64.
Hymel KP, Rumack CM, Hay TC, Strain JD, Jenny C. Comparison of intracranial computed tomographic (CT) findings in pediatric abusive and accidental head trauma. Pediatr Radiol. 1997;27(9):743–7.
Zimmerman RA, Bilaniuk LT, Bruce D, Schut L, Uzzell B, Goldberg HI. Interhemispheric acute subdural hematoma: a computed tomographic manifestation of child abuse by shaking. Neuroradiology. 1978;16:39–40.
Bergström M, Ericson K, Levander B, Svendsen P. Computed tomography of cranial subdural and epidural hematomas: variation of attenuation related to time and clinical events such as rebleeding. J Comput Assist Tomogr. 1977;1(4):449–55.
Lee KS, Bae WK, Bae HG, Doh JW, Yun IG. The computed tomographic attenuation and the age of subdural hematomas. J Korean Med Sci. 1997;12(4):353–9.
Schachenmayr W, Friede RL. The origin of subdural neomembranes. I. Fine structure of the dura-arachnoid interface in man. Am J Pathol. 1978;92(1):53–68.
Friede RL, Schachenmayr W. The origin of subdural neomembranes. II. Fine structural of neomembranes. Am J Pathol. 1978;92(1):69–84.
Krous HF, Byard RW. Shaken infant syndrome: selected controversies. Pediatr Dev Pathol. 1999;2(6):497–8.
Sinal SH, Ball MR. Head trauma due to child abuse: serial computerized tomography in diagnosis and management. South Med J. 1987;80(12):1505–12.
Girard N, Brunel H, Dory-Lautrec P, Chabrol B. Neuroimaging differential diagnoses to abusive head trauma. Pediatr Radiol. 2016;46(5):603–601.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M. Gencturk, H.G. Tore, D.R. Nascene, L. Zhang, Y. Koksel and A.M. McKinney declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Gencturk, M., Tore, H.G., Nascene, D.R. et al. Various Cranial and Orbital Imaging Findings in Pediatric Abusive and Non-abusive Head trauma, and Relation to Outcomes. Clin Neuroradiol 29, 253–261 (2019). https://doi.org/10.1007/s00062-018-0663-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00062-018-0663-7