Abstract
Purpose
To describe a novel configuration of pipeline embolization device for internal carotid bifurcation region aneurysm, named horizontal stenting.
Clinical presentation
A 64-year-old woman, with visual deficit, harboring a large wide-necked aneurysm located at the junction between left internal carotid artery and left A1 segment of anterior cerebral artery, was submitted to endovascular treatment. As she had pre-existing occlusion of left internal carotid, approach from the contralateral internal carotid was used to advance the pipeline embolization device through the anterior communicating artery and place the flow diverter horizontally across the neck (from M1 to A1). Coil embolization was also performed through a microcatheter navigated via posterior communicating artery. The intervention was uneventful, with total aneurysm occlusion. Patient presented with visual improvement on follow-up.
Conclusion
Horizontal deployment of pipeline embolization device appears to be an acceptable and feasible alternative to treat internal carotid bifurcation aneurysms. Long-term follow-up and a greater number of cases are mandatory to establish the safety of this strategy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Purpose
The development of flow-diverting devices represented a groundbreaking invention in intracranial aneurysm (IA) treatment. Moreover, it has significantly changed the treatment paradigm of challenging cerebral aneurysms, such as large-to-giant, wide-necked, dissecting, and fusiform lesions [1].
The pipeline embolization device (PED; Covidien Vascular Therapies, Mansfield, MA, USA) was initially approved for the treatment of IAs situated between the petrous and the superior hypophyseal segments of the internal carotid artery [1]. However, a growing number of publications have been reported about PED utilization in different locations, beyond the sidewall aneurysms, including bifurcation aneurysms [1, 2, 3].
We present here a novel configuration of PED for treatment of a wide-necked internal carotid artery bifurcation region aneurysm. The horizontal deployment of flow-diverting stents via anterior communicating artery (A1 to M1 segment) to treat carotid tip region aneurysms has never been reported.
Clinical Presentation
A 64-year-old woman presented with a six-month history of intermittent throbbing headaches associated with progressive bilateral visual loss, worse on the left side. She had systemic hypertension and a history of aortic valve replacement. Because of the prosthetic heart valve she was kept continuously anticoagulated with warfarin. Computed tomography scan revealed a left, well circumscribed, round smooth-walled strong and uniformly enhancing hyperdense lesion at the internal carotid bifurcation region, suggestive of an aneurysm. Angiogram showed a large wide-necked aneurysm, involving the junction between left A1 segment and the internal carotid tip. Additionally, the left internal carotid artery (ICA) was occluded at the level of cavernous segment. Its territory was supplied through the right ICA and vertebral arteries via anterior and posterior communicating arteries (PCAs), respectively (Fig. 1).
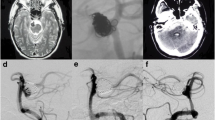
a Right internal carotid angiogram, AP view, shows large, wide-necked aneurysm of left carotid bifurcation region. b Vertebral artery arteriogram, Towne view, demonstrates perfusion of the left internal carotid artery territory through posterior communicating artery. c and d 3D rotational angiography with simultaneously injection into vertebral and carotid arteries, shows the aneurysm located at the left A1-internal carotid region
Considering the large volume of the aneurysm (18 mm); optic apparatus compression; need of continuous use of warfarin; left carotid occlusion, and need for A1 preservation to keep collateral flow to left side; endovascular treatment was chosen.
We also considered that optimal endovascular treatment should occlude the aneurysm and decrease the mass effect. Trapping of left A1 segment, even keeping the carotid tip patent and thus flow to middle cerebral artery (MCA) territory via posterior communicating artery, was excluded because it would lead to ischemia due to medial group lenticulostriate arteries occlusion. Simple coiling was not possible because of the wide neck. Additionally, stent- or balloon-assisted coiling would increase the compression on the optic tract, and the chance of recanalization would not be negligible. Therefore, it was decided to treat the aneurysm with a flow-diverting stent to promote aneurysm size regression. Since the patient would require aspirin, clopidogrel, and warfarin, it was decided to place a small amount of coils, fearing early hemorrhagic complications associated to aneurysm rupture. These coils would promote faster aneurysm occlusion without significantly increasing mass effect.
Bilateral femoral approach was chosen to allow simultaneously navigation through the anterior and posterior communicating artery. Under general anesthesia and anticoagulation, a 6 F guiding catheter (Stryker Neurovascular, Fremont, CA, USA) was placed into the right vertebral artery to coaxially navigate an Excelsior SL10 microcatheter. A tri-axial system was used to achieve good support for PED navigation: a long 6 F introducer (Epsylar, Optimed, Ettlingen, Germany) was placed within the cervical portion of right internal carotid artery; a 6 F guiding catheter (Neuron, Penumbra, Alameda, CA, USA) was then navigated into the right petrous internal carotid artery; and finally, the delivery microcatheter (Marksman, Covidien, USA) was navigated distally to the aneurysm neck via the anterior communicating artery toward the left M1 segment for subsequent deployment of flow diverter (Fig. 2).
a Roadmapping shows catheterization of the left middle cerebral artery (MCA) via anterior communicating artery, crossing the aneurysm neck. b Roadmapping shows catheterization of the aneurysm via posterior communicating artery. c Fluoroscopy demonstrates both microcatheters position. d Final control from right internal carotid. e Final control from right vertebral artery. f Pipeline embolization device (PED) and coils cast
After crossing the aneurysm neck with the Marksman catheter, the Excelsior microcatheter was navigated through the left posterior communicating artery toward the left internal carotid artery and finally placed into the aneurysm. A PED 2.5 × 16 mm was first deployed covering the aneurysm neck, from left M1 to left A1. We have paid special attention to choose the length of the device to avoid deployment inside the anterior communicating artery. Despite marked contrast stagnation inside the sac, a small number of coils (Target, Stryker Neurovascular, Fremont, CA, USA) were inserted promoting total aneurysm occlusion.
The patient had an uneventful recovery and presented with visual field improvement after six-month follow-up.
Discussion
Endosaccular embolization of IA with or without device assistance is a widely adopted treatment modality. However, many aneurysms have configurations that are unsuitable or unsafe for embolization and/or conventional stenting. Wide-necked bifurcation region aneurysms continue to present with major challenges. Another important issue of coil embolization of aneurysms is how to decrease recanalization rates [3, 4].
Various configurations of stenting have been proposed and performed for bifurcation aneurysms, including a simple stent, waffle-cone stent, horizontal stent, Y-stent, kissing stent [4]. Stent-assisted coiling (SAC) promotes occlusion of incompletely coiled aneurysms and lowers recanalization rates compared with non-stenting embolization. Despite this, recanalization rates of SAC are 8.1–17.2 % [4].
Additionally, in some circumstances the anterograde approach may be restrictive, because of lack of an optimal angle to allow adequate positioning of a balloon and/or stent into the parent artery, completely covering the aneurysm neck. Moreover, ipsilateral vessel occlusion is likely to be an increasing circumstance given the fact we are treating older and a wider range of patients. A solution to overcome this difficulty was proposed by Moret et al. [5] in 2000, named retrograde approach via a communicating vessel. In the majority of cases remodeling technique was used.
In 2005, Cross et al. [6] first described the placement of one stent horizontally at the basilar termination via posterior communicating approach for coiling of a wide-necked basilar tip aneurysm. After that, several reports and case series described horizontal stenting in two different configurations, PCA to PCA to treat basilar bifurcation aneurysms, and M1 to A1 to treat internal carotid bifurcation aneurysms [6–9].
There are several potential advantages of this approach: (1) use of only one stent and reduction in device-related cost; (2) total coverage of the aneurysm neck; (3) reduction in the amount of metal remaining permanently within the parent artery. Meanwhile, horizontal technique is highly dependent on the patency, lack of tortuosity, and size of communicating arteries. On the other hand, the need of bilateral femoral puncture and simultaneously catheterization of carotid and vertebral arteries are the main disadvantages [6–9].
Although PED was initially approved for the treatment of IAs situated between the petrous and the superior hypophyseal segments of the internal carotid artery, we decided to treat the carotid tip region aneurysm with this device [1–3]. It would represent a definitive treatment and could provide the greater chance of mass effect improvement [1, 10]. Despite that, initial worsening of visual function could happen secondary to aneurysm sac thrombosis and swelling. Concerned about early hemorrhagic complication, mainly because of double antiplatelet regimen and warfarin, it was placed a small amount of coils, just sufficient to immediately occlude the aneurysm without significantly increasing the mass effect. It could permit aneurysm shrinkage on follow-up.
In the reported case, retrograde approach with horizontal stent deployment was mandatory because of ipsilateral internal carotid artery occlusion. The anterior communicating artery was chosen because its diameter was compatible with Marksman microcatheter, allowing adequate stent deployment from M1 to A1.
Recent studies demonstrate that the use of flow diverters (FD) in bifurcation aneurysms could carry a greater risk compared to their use in internal carotid sidewall aneurysms. Pistocchi et al. [3] reported neurological complication in 11.1 % of patients and no mortality. Aneurysm at and beyond the circle of Willis were included. Saleme et al. [2] reported new permanent neurological deficit in 9.4 % of patients with bifurcation aneurysms. Additionally, symptomatic side-branch remodeling occurred in 13.5 % of the cases, all of which were transient and recovered completely. The behavior of horizontally deployed flow diverter is unknown. More cases are necessary to allow comparison with other FD configurations.
Horizontal deployment of PED could be an alternative method in two situations: internal carotid or basilar bifurcation regions, and difficult access through the parent artery. We recommend special attention while choosing PED length. Its deployment inside the communicating arteries could result in inadequate expansion and thromboembolic complications.
Finally, at the moment, this novel PED configuration should be used in very specific situations, when other endovascular and neurosurgical approaches are not suitable.
Conclusion
Horizontal deployment of pipeline embolization device appears to be an acceptable and feasible alternative in very specific situations. A greater number of cases are necessary to determine the usefulness and safety of this technique.
Conflict of Interest
On behalf of all authors, the corresponding author states there is no conflict of interest.
References
Leung GKK, Tsang ACO, Lui WM. Pipeline embolization device for intracranial aneurysm: a systemic review. Clin Neuroradiol. 2012;22:295–303.
Saleme A, Iosif C, Ponomarjova S, Mendes G, Camilleri Y, Caire F, Boncoeur MP, Mounayer C. Flow-diverting stents for intracranial bifurcation aneurysm treatment. Neurosurgery. 2014;75:623–31.
Pistocchi S, Blanc R, Bartolini B, Piotin M. Flow diverters at and beyond the level of the circle of Willis for the treatment of intracranial aneurysm. Stroke. 2012;43:1032–8.
Kono K, Terada T. Hemodynamics of 8 different configurations of stenting for bifurcation aneurysms. AJNR Am J Neuroradiol. 2013;34:1980–6.
Moret J, Boss IB, Piotin M. The retrograde approach: a consideration for the endovascular treatment of aneurysms. AJNR Am J Neuroradiol. 2000;21:262–8.
Cross DT, III, Moran CJ, Derdeyn CP, Mazumbar A, River D, Chicoine MM. Neuroform stent deployment for treatment of a basilar tip aneurysm via a posterior communicating artery route. AJNR Am J Neuroradiol. 2005;26:2578–81.
Black SL, Kadkhodayan Y, Shekhtman E, Derdeyn CP, Cross DT, III, Christopher M. Treatment of basilar tip aneurysms with horizontal PCA to PCA stent-assisted coiling: case series. J Neurointervent Surg. 2013;5:212–6.
Bendorf G, Klucznik RP, Meyer D, Strother CM, Mawad ME. “Cross-over” technique for horizontal stenting of an internal carotid bifurcation aneurysm using a new self-expandable stent: technical case report. Neurosurgery. 2006;58(Suppl 1):ONS–E172.
Siddiqui MA, Bhattacharya JJ, Lindsay KW, Jenkins S. Horizontal stent-assisted coil embolization of wide-necked intracranial aneuryms with the enterprise stent—a case series with early angiographic follow-up. Neuroradiology. 2009;51:411–8.
Puffer RC, Piano M, Lanzino G, Valvassori L, Kallmes DF, Quilici L, Cloft HJ, Boccardi E. Treatment of cavernous sinus aneurysms with flow diversion: results in 44 patients. AJNR Am J Neuroradiol. 2014;35:948–51.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Trivelato, F., Araújo, J., Salles Rezende, M. et al. A Novel Configuration of Pipeline Embolization Device for Internal Carotid Bifurcation Region Aneurysms: Horizontal Deployment. Clin Neuroradiol 27, 57–60 (2017). https://doi.org/10.1007/s00062-015-0414-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00062-015-0414-y