Abstract
Background
Subcutaneous implantable cardioverter–defibrillators (S-ICDs) have been shown to be non-inferior to transvenous ICDs in the prevention of sudden cardiac death (SCD), but there is still a lack of evidence from clinical trials in China. We investigated whether S‑ICD implantation in the Chinese population is safe and feasible and should be promoted in the future.
Methods
Consecutive patients undergoing S‑ICD implantation at our center were enrolled in this retrospective study. Data were collected within the median follow-up period of 554 days. Data concerning patient selection, implantation procedures, complications, and episodes of shock were analyzed.
Results
In total, 70.2% of all 47 patients (median age = 39 years) were included for secondary prevention of SCD with different etiologies. Vector screening showed that 98% of patients were with > 1 appropriate vector in all postures. An intraoperative defibrillation test was not performed on six patients because of the high risk of disease deterioration, while all episodes of ventricular fibrillation induced post implantation were terminated by one shock. As expected, no severe complications (e.g., infection and device-related complications) were observed, except for one case of delayed healing of the incision. Overall, 15 patients (31.9%) experienced appropriate shocks (AS) with all episodes terminated by one shock. Two patients (4.3%) experienced inappropriate shocks (IAS) due to noise oversensing, resulting in a high Kaplan–Meier IAS-free rate of 95.7%.
Conclusion
Based on appropriate patient selection and standardized implantation procedures, this real-world study confirmed the safety and efficacy of S‑ICD in Chinese patients, indicating that it may help to promote the prevention of SCD in China.
Zusammenfassung
Hintergrund
Subkutane implantierbare Kardioverter-Defibrillatoren (S-ICD) haben sich gegenüber transvenösen ICD bei der Prävention des plötzlichen Herztods (SCD) als nichtunterlegen erwiesen, aber es fehlt bislang noch Evidenz aus klinischen Studien in China. Die Autoren untersuchten, ob die S‑ICD-Implantation in der chinesischen Bevölkerung sicher und praktikabel ist und ob sie in Zukunft gefördert werden sollte.
Methoden
Konsekutiv sich zur S‑ICD-Implantation vorstellende Patienten im Zentrum der Autoren wurden in die vorliegende retrospektive Studie einbezogen. Für eine mittlere Nachbeobachtungsdauer von 554 Tagen wurden dabei Daten erhoben. Ausgewertet wurden die Daten zur Patientenselektion, zu den Implantationsverfahren, zu Komplikationen und Schockereignissen.
Ergebnisse
Zur Sekundärprävention des SCD unterschiedlicher Ätiologie wurden 70,2 % aller 47 Patienten (mittleres Alter: 39 Jahre) in die Studie eingeschlossen. Das Vektorscreening zeigte, dass 98 % der Patienten > 1 entsprechenden Vektor in allen Positionen aufwiesen. Ein intraoperativer Defibrillationstest wurde bei 6 Patienten wegen des hohen Risikos einer Krankheitsverschlechterung nicht durchgeführt, während alle Phasen von Kammerflimmern, die nach Implantation auftraten, durch einen Schock beendet wurden. Wie erwartet, wurden keine schweren Komplikationen (z. B. Infektionen und gerätbezogene Komplikationen) beobachtet, außer in einem Fall eine verzögerte Abheilung der Inzisionsstelle. Bei 15 Patienten (31,9 %) wurden adäquate Schocks (AS) ausgelöst, wobei alle Phasen durch einen Schock beendet wurden. In 2 Fällen (4,3 %) kam es zu inadäquaten Schocks (IAS) aufgrund von Oversensing, was zu einer hohen IAS-freien Rate nach Kaplan-Meier von 95,7 % führte.
Schlussfolgerung
Auf der Grundlage einer entsprechenden Patientenselektion und standardisierter Implantationsverfahren bestätigte die vorliegende Real-World-Studie die Sicherheit und Wirksamkeit von S‑ICD bei chinesischen Patienten als Hinweis darauf, dass diese Methode möglicherweise zur Förderung der Prävention des SCD in China beitragen kann.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Sudden cardiac death (SCD) is a life-threatening challenge worldwide, although substantial progress has been made for the treatment of SCD, for example, with implantable cardioverter–defibrillator (ICDs). A transvenous ICD (TV-ICD), which is effective in reducing the risk of SCD in both primary and secondary prevention [1], is associated with many acute or long-term complications (e.g., pneumothorax, infection, lead malfunction, etc.; [2, 3]). Therefore, a less invasive but more effective system is needed.
As expected, subcutaneous ICD (S-ICD), a device that is totally implanted outside the thoracic cavity, has been demonstrated to be non-inferior to TV-ICD in terms of the safety and efficacy both in randomized controlled trials and in real-world studies [4,5,6,7,8]. The results of these studies indicated S‑ICD as an alternative choice to TV-ICD for patients with an indication for defibrillator therapy but without an indication for antitachycardia pacing (ATP) or backup pacing.
Although S‑ICDs have already been extensively used for decades, they were certified for use in China only recently, in 2018. Moreover, prior studies regarding S‑ICDs were mostly performed without the enrollment of patients from Asia, resulting in the limited implantation of S‑ICD in Chinese patients and insufficient application evidence among this population. Thus, we performed this retrospective study with patients in our center to verify the safety and efficacy of S‑ICD in Chinese patients. We also attempt to provide the real-world experiences for the optimized application of this device in the future.
Methods
Study design
In this retrospective analysis, all patients who underwent S‑ICD implantation at the Zhongshan Hospital of Fudan University (Shanghai, China) were considered eligible and included consecutively. Data were collected from patient files, while follow-up information was acquired both from regular face-to-face outpatient monitoring and via telephone contact. Ethical approval for this research was granted by our local medical ethics committee.
Vector screening
Electrocardiogram recordings of potential patients were collected in the supine and siting/standing positions at rest. Patients were considered suitable for S‑ICD implantation if at least one sensing vector was acceptable in all tested postures that were analyzed by an automated screening tool (AST) or a manual screening tool (MST; [9]).
S-ICD implantation
Patients were anesthetized after the appropriate location for the device and lead implantation was confirmed and marked via preoperative fluoroscopy. The procedure was typically performed using either the two- or three-incision technique: one incision for the device pocket and xiphoid, with or without a superior sternal incision.
The device was placed in the intermuscular plane between the latissimus dorsi and serratus anterior and sutured to the muscle bed to avoid migration. The distal sensing electrode was positioned adjacent to the manubriosternal junction and the proximal sensing electrode was placed adjacent to the xiphoid process. Air was removed carefully from the lead tunnels and device header. Defibrillation threshold (DFT) tests were performed at the end of the procedure unless foreseeable high risks or shock impedances were recorded. Chest radiography was performed immediately postimplantation to assess the position of the lead and pulse generator [10].
Postoperative programming
A shock zone at 230 bpm and a conditional shock zone at 200 bpm or 10–20 bpm less than the previous ventricular tachycardia (VT) rate were programmed. A SMART-pass filter and the function of pacing after defibrillation (50 bpm for 30 s) were switched on in all devices [11].
Follow-up
Follow-up was performed at in-office visits and/or through phone calls. Device-related complications were observed (including infection, lead replacement, device malfunction, delayed surgical incision healing, etc.). Both appropriate and inappropriate shocks were recorded and analyzed.
Statistical analysis
Descriptive statistics are reported with mean ± standard deviation (SD) or median interquartile range (IQR) for continuous variables and frequency and percentage for categorical variables. Kaplan–Meier analyses were made to estimate event-free rates for appropriate shock (AS) and inappropriate shock (IAS). Learning-curve analysis was determined by logistic regression. All statistical analyses were performed using SPSS version 17.0.
Results
Study population
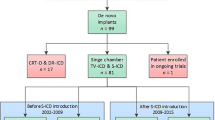
This study enrolled patients who met the aforementioned inclusion criteria in Zhongshan Hospital, Fudan University from August 21, 2018 to January 28, 2022. A total of 47 patients were enrolled consecutively, with a median follow-up duration of 554 days. The clinical characteristics of all patients are summarized in Table 1. Briefly, the majority of the patients were male (78.7%) with the median age of 39 years (IQR: 28, 61). The S‑ICDs were implanted in patients eligible for ICD implantation but without predictable pacing requirements [12] and for various etiologies (e.g., ischemic cardiomyopathy, dilated cardiomyopathy, hypertrophic cardiomyopathy, etc.). Overall, 70.2% of the patients underwent implantation for secondary prevention, with a median left ventricular ejection fraction (LVEF) of 48% (IQR: 35%, 65%). Four of the 47 patients were highly advised to receive S‑ICD implantation because of the high risk of infection associated with TV-ICD (one patient with previous TV-ICD-related infection and three with end-stage renal disease). Among the 47 patients considered suitable for S‑ICD implantation, 46 patients had > 1 appropriate vector in both postures (three appropriate vectors in 57.4% of the patients).
Implantation procedure
The second-generation devices were all successfully implanted in the patients. To reduce the intensity of pain and to enable the patients to cooperate better with the operation, all patients received intravenous anesthesia. Specifically, general anesthesia (GA) by the combination of propofol and remifentanil along with mechanical ventilation were successfully applied to the first 19 patients, to avoid patient discomfort and awareness, especially at lead tunneling and the generator insertion sites. The rest of the patients were anesthetized by a combination of monitored anesthesia care (MAC) and local anesthesia at the site of implantation.
As shown in Table 2, intraoperative defibrillation testing (DFT) was not performed for six patients, due to the high risk of either atrial fibrillation-related thrombosis or aggravation of heart failure. One of the six patients received two appropriate shocks, and none of them received inappropriate shock. Moreover, ventricular fibrillation (VF) was successfully induced in 39 patients, all of which were terminated with one 65‑J shock. Nonetheless, the PRAETORIAN score of the patients who did not undergo DFT or failed DFT was< 90 for all patients. The shock impedance was similar between patients who underwent DFT and those who did not (66 ± 14 vs. 72 ± 12 Ω, p = 0.36).
The leads were positioned to the right sternal border in half of the patients, which were determined by both preoperative fluoroscopy and sensing vector tests. Additionally, the increased number of implantations was accompanied by decreased procedure time (Fig. 1).
Complications
During the median follow-up of 554 days (IQR: 257, 934), there was only one patient with delayed healing of the pocket incision but without infection. No other device-related complications were observed (e.g., infection, lead replacement, device malfunction, etc.), and no replacement was needed for the patients, regarding pacing for the treatment of bradycardia, using anti-tachycardia pacing (ATP) therapy or cardiac resynchronization therapy (CRT) (Table 3).
Appropriate shock
During the follow-up, 17 patients received a total of 77 shocks. Two of these patients received 24 and 22 shocks, respectively, due to ventricular electrical storms induced by either gynecological operation or excessive activities with inappropriate discontinuation of medical treatment. Appropriate shocks (AS) were delivered to 15 patients (31.9%) during the follow-up, while all episodes (VT/VF) were successfully terminated by the first shock (Table 3). Overall, 12 patients (80%) received their first AS within 1 year, and the Kaplan–Meier AS-free rate was 58.1% at 2 years (Fig. 2a).
Inappropriate shock
As shown in Table 3, only two patients (4.3%) experienced inappropriate shock (IAS) due to non-cardiac oversensing within 9 days of implantation, resulting in a high Kaplan–Meier IAS-free rate of 95.7% (Fig. 2b).
Specifically, a 67-year-old male patient underwent S‑ICD implantation due to ischemic cardiomyopathy. He experienced IAS without any discomfort before the shock at the third hour after the operation. A contentious baseline shift and frequent oversensing of low-amplitude signals were detected by device interrogation, which was followed by a shock (Fig. 3a). A similar baseline shift, which could be induced by pressing the two incisions, disappeared after massaging the skin along the tract and pocket, indicating that there was subcutaneous air surrounding the proximal electrode [13]. In addition, the sensing vector was changed from secondary to alternate, and further IAS was avoided.
Another 38-year-old male patient with Brugada syndrome experienced IAS while having lunch and being in his usual state of health 9 days after device implantation. Likewise, device interrogation revealed lead noise with evidence of noise oversensing (Fig. 3b), which is similar to a previously reported case, suggesting that noise oversensing might be triggered by fluid or air entrapment within the device header secondary to a physical breach of the seal plug [14]. The relationships between the sensing vectors and the points of lead connecting to the pulse generator are shown in Fig. 4. The impairment of the seal plug may affect the function of point A (Fig. 4b,c), which is associated with the secondary vector (Fig. 4a). Finally, the noise oversensing-induced IAS was resolved after reprogramming the sensing vector from secondary to primary, which is related to points B and C, but not point A (Fig. 4).
Discussion
Multiple studies have verified the safety and efficacy of S‑ICD, and also proved that they are associated with lower risks of periprocedural complications as well as device-related complications and IAS, as compared with TV-ICD [15,16,17,18]. Regrettably, there is limited experience on this treatment in East-Asia populations, due to the significantly lower number of patients undergoing implantation, as compared with the increasing number of patients in other regions. This study confirmed the safety and efficacy of S‑ICD in Chinese patients by providing the evidence from a single center.
Patient selection
In general, candidates for ICD therapy without backup pacing demand may be suitable for S‑ICD treatment, especially for patients with a high risk of infection and young patients, regardless of whether for it used for primary or secondary prevention. The median age of patients who received S‑ICD implantation at our hospital was 39 years, and in most cases it was for secondary prevention. This may also account for the high rate of AS in this study. As in previous studies, most patients underwent S‑ICD implantation for primary prevention [4,5,6]. In view of the very low prevalence of ICD utilization in China (approx. only 1.5 device per 1 million people; [19]) this less invasive and well-accepted system may give an impetus to promote the prevention of SCD [20].
To further identify suitable patients for S‑ICD implantation, vector screening should be performed; in this study, eligibility was defined by the presence of ≥ 1 appropriate vector in all postures. The majority of patients (98%) in this study had more than one appropriate vector in all postures, which made it possible to reprogram the sensing vectors in the two patients who experienced IAS. Thus, from our point of view, the location (right or left parasternal position) that has ≥ 2 appropriate vectors may be preferred for lead implantation, in the case of an unpredictable need for reprogramming the sensing vector in the future.
Anesthesia for the operation
With the accumulation of surgical experience, and to minimize the drawbacks associated with GA such as procedure length, airway injury, and post-anesthesia care, MAC with dexmedetomidine hydrochloride and local anesthesia with lidocaine were simultaneously delivered to the rest of patients. Both of these anesthesia strategies are acceptable, while local anesthesia alone may not be preferred because of the difficulty to tolerate the pain during the whole operation. Additionally, device-related pain may be severe in the first 3 days postimplantation and could be successfully managed with nonsteroidal anti-inflammatory drugs [21].
DFT in implantation
Currently, DFT is recommended in S‑ICD implantation to determine the ability of the device in terminating fatal ventricular arrythmia [22, 23]. In this study, 87.5% of the patients successfully underwent DFT, which is similar to reports from a previous study [24]. The PRAETORIAN score is a tool evaluating the implant position and predicting the defibrillation success of the S‑ICD. Specifically, < 90 points represents a low risk, 90–< 150 points represents an intermediate risk, and ≥ 150 points represents a high risk of conversion failure [25]. The six patients who did not undergo DFT owing to a high risk of disease deterioration all had a PRAETORIAN score of < 90, and none of them experienced unsuccessful termination of VT/VF, indicating that the PRAETORIAN score is helpful in identifying patients at risk for ineffective shock conversion [25]. Additionally, it also implies that implantation of S‑ICD without DFT may be safe and effective [26]. Moreover, it is doubted that DFT is still needed routinely at implantation, given the extremely high success rate of such procedures today [5, 27]. Therefore, the undergoing randomized controlled trial assessing DFT in the S‑ICD should further elucidate the need for DFT [28].
S-ICD-related complications
During the longest follow-up period of 1334 days, no serious complications were observed except for delayed healing of the pocket incision in one patient. This is consistent with the superiority of S‑ICD implantation presented in other studies, which reported fewer infections, thrombotic events, and wire-related complications [29, 30].
Compared with TV-ICD, making a device pocket for S‑ICD is more traumatic, which may be more likely to result in local infection and bleeding. Thus, the intermuscular technique (between the latissimus dorsi and serratus anterior muscles) is regularly adopted to reduce pocket complications and infections. Moreover, ensuring optimal initial placement and securing of the device to the deep fascia so as to avoid migration into a more anterior pocket are of crucial importance to guarantee high shock efficacy [31]. Furthermore, perioperative management of anticoagulation may help minimize the events of pocket hematomas. It has been reported that antiplatelet therapy with clopidogrel appears to increase the risk for hematoma following S‑ICD implantation [32]. Considering that uninterrupted use of warfarin is associated with an increased risk of lateral pocket hematoma [33], interruption of anticoagulation without bridging should be considered for patients with an acceptable risk status [32]. In conclusion, a risk–benefit assessment must be made when deciding to stop or continue anticoagulation.
Safety and efficacy
No significant prognostic differences were observed between S‑ICD and TV-ICD regarding all-cause mortality, cardiac death, and non-cardiac death. [16]. Moreover, the safety and efficacy of S‑ICD for discrete and storm episodes have been confirmed by long-term studies, with the first and final shock efficacy of more than 90% and 95%, respectively. [8, 31]. Likewise, all VT/VF episodes were terminated by the first shock in our study, which may be due to the relatively small number of the patients and short follow-up duration. The safety and efficacy of the therapy could be enhanced by improving controllable factors, such as suitable patient selection and standardized implanting procedure.
With the increased experience of operators in implantation and programming, as well as improvements in the detection, filtering, and discriminative algorithms, the incidence of IAS has decreased yearly to an annualized rate of less than 4% [31, 34, 35]. This is consistent with the promisingly high Kaplan–Meier IAS-free rate (95.7%) in our study. Moreover, unlike TV-ICD, S‑ICD was found to be associated with a significantly lower risk of IAS due to supraventricular arrhythmias, but an increase risk due to oversensing [16], such as T wave oversensing and myopotentials [4, 36, 37]. Likewise, the IAS episodes experienced by two patients in our study were all induced by noise oversensing, which was eventually resolved by altering the sensing vector. Thus, conditionally reprogramming sensory vectors may reduce episodes of IAS or prevent future episodes once they are detected [38]. In addition, it should be emphasized that releasing any residual subcutaneous air through the incisions prior to closing and avoiding violent actions during the operation are also helpful to minimize noise sensing-induced IAS.
Learning curve
Previous research showed that the complication rate and procedure time stabilized after > 13 implants, indicating a short learning curve for physicians adopting the S‑ICD procedure [39]. Our experience also demonstrated that the technique could be well mastered by physicians shortly within 20 implantations, which is suggested by the shortened and stable procedure time.
Limitations
This study has several limitations. Firstly, it was a single-center study with a relatively small sample size, which carries inherent limitations. Secondly, the single-arm, retrospective design of the study did not allow for a comparative assessment of the safety and efficacy between S‑ICD and TV-ICD. Thirdly, most of the patients enrolled were for the secondary prevention of SCD with different etiologies and therefore the results may not be translated to cases of primary prevention with specific etiology.
Conclusion
This real-world study confirmed the safety and efficacy of subcutaneous implantable cardioverter–defibrillators (S-ICD) in the prevention of sudden cardiac death (SCD). A high rate of successful appropriate shocks and a low rate of inappropriate shocks were achieved based on appropriate patient selection, standardized implanting procedures, and programming experience. Although S‑ICD have been used in dozens of hospitals in China, the number of treated patients is still relatively small. Thus, S‑ICD should be promoted in more centers to benefit more patients and enhance the prevention of SCD.
References
Miller JD, Yousuf O, Berger RD (2015) The implantable cardioverter-defibrillator: an update. Trends Cardiovasc Med 25:606–611
Burri H, Starck C, Auricchio A et al (2021) EHRA expert consensus statement and practical guide on optimal implantation technique for conventional pacemakers and implantable cardioverter-defibrillators: endorsed by the heart rhythm society (HRS), the asia pacific heart rhythm society (APHRS), and the latin-American heart rhythm society (LAHRS). Europace 23:983–1008
Koneru JN, Jones P, Hammill EF et al (2018) Risk factors and temporal trends of complications associated with transvenous Implantable cardiac defibrillator leads. J Am Heart Assoc 7:e7691
Knops RE, Olde Nordkamp L, Delnoy PHM et al (2020) Subcutaneous or transvenous defibrillator therapy. N Engl J Med 383:526–536
Gold MR, Lambiase P, El-Chami MF et al (2021) Primary results from the understanding outcomes with the S‑ICD in primary prevention patients with low ejection fraction (UNTOUCHED) trial. Circulation 143:7–17
Lambiase PD, Theuns D, Murgatroyd F et al (2022) Subcutaneous implantable cardioverter-defibrillators: long-term results of the EFFORTLESS study. Eur Heart J. https://doi.org/10.1093/eurheartj/ehab921
Khanra D, Hamid A, Patel P et al (2022) A real-world experience of subcutaneous and transvenous implantable cardiac defibrillators-comparison with the PRAETORIAN study. J Arrhythm 38:199–212
Knops RE, van der Stuijt W, Delnoy PPHM et al (2022) Efficacy and safety of appropriate shocks and antitachycardia pacing in transvenous and subcutaneous implantable defibrillators: analysis of all appropriate therapy in the PRAETORIAN trial. Circulation 145:321–329
Bögeholz N, Pauls P, Güner F et al (2018) Direct comparison of the novel automated screening tool (AST) versus the manual screening tool (MST) in patients with already implanted subcutaneous ICD. Int J Cardiol 265:90–96
Schukro C, Santer D, Prenner G et al (2020) State-of-the-art consensus on non-transvenous implantable cardioverter-defibrillator therapy. Clin Cardiol 43:1084–1092
Tachibana M, Nishii N, Banba K et al (2019) SMART pass will prevent inappropriate operation of S‑ICD. J Arrhythm 35:86–91
Priori SG, Blomström-Lundqvist C, Mazzanti A et al (2015) 2015 ESC guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: the task force for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death of the European society of cardiology (ESC). Endorsed by: association for European paediatric and congenital cardiology (AEPC). Eur Heart J 36:2793–2867
Nishinarita R, Kishihara J, Matsuura G et al (2019) Early inappropriate shock in a subcutaneous cardiac defibrillator due to subcutaneous air. J Arrhythm 35:682–684
Barnett A, Eckhardt L, Leal MA (2018) Seal plug damage causing inappropriate detection and therapy in a subcutaneous defibrillator system. HeartRhythm Case Rep 5:66–69
Nso N, Nassar M, Lakhdar S et al (2022) Comparative assessment of transvenous versus subcutaneous Implantable cardioverter-defibrillator therapy outcomes: an updated systematic review and meta-analysis. Int J Cardiol 349:62–78
Rordorf R, Casula M, Pezza L et al (2021) Subcutaneous versus transvenous implantable defibrillator: an updated meta-analysis. Heart Rhythm 18:382–391
Su L, Guo J, Hao Y, Tan H (2021) Comparing the safety of subcutaneous versus transvenous ICDs: a meta-analysis. J Interv Card Electrophysiol 60:355–363
Basu-Ray I, Liu J, Jia X et al (2017) Subcutaneous versus transvenous Implantable defibrillator therapy: a meta-analysis of case-control studies. JACC Clin Electrophysiol 3:1475–1483
Shu Z (2015) Sudden cardiac death in China: current status and future perspectives. Europace 2:14–18
Vicentini A, Bisignani G, De Vivo S et al (2022) Patient acceptance of subcutaneous versus transvenous defibrillator systems: a multi-center experience. J Cardiovasc Electrophysiol 33:81–89
Okabe T, Miller A, Koppert T et al (2020) Feasibility and safety of same day subcutaneous defibrillator implantation and send home (DASH) strategy. J Interv Card Electrophysiol 52:311–318
Frommeyer G, Zumhagen S, Dechering DG et al (2016) Intraoperative defibrillation testing of subcutaneous implantable cardioverter-defibrillator systems—a simple issue? J Am Heart Assoc 5:e3181
Rudic B, Tülümen E, Fastenrath F et al (2020) Defibrillation failure in patients undergoing replacement of subcutaneous defibrillator pulse generator. Heart Rhythm 17:455–459
Liang JJ, Okamura H, Asirvatham R et al (2019) Comparative outcomes of subcutaneous and transvenous cardioverter-defibrillators. Chin Med J (Engl) 132:631–637
Quast ABE, Baalman S, Brouwer TF et al (2019) A novel tool to evaluate the implant position and predict defibrillation success of the subcutaneous implantable cardioverter-defibrillator: the PRAETORIAN score. Heart Rhythm 16:403–410
Al-Ghamdi B, Shafquat A, Alruwaili N et al (2017) Subcutaneous implantable cardioverter defibrillators implantation without defibrillation threshold testing: a single center experience. Cardiol Res 8:319–326
Burke MC, Aasbo J, El-Chami MF et al (2020) 1‑year prospective evaluation of clinical outcomes and shocks: the subcutaneous ICD post approval study. JACC Clin Electrophysiol 6:1537–1550
Quast ABE, Baalman S, Betts TR et al (2019) Rationale and design of the PRAETORIAN-DFT trial: a prospective randomized comparative trial of SubcutanEous Implantable CardiOverter-DefibrillatoR ImplANtation with and without defibrillation testing. Am Heart J 214:167–174
Chen CF, Jin C, Liu MJ, Xu YZ (2019) Efficacy, safety, and in-hospital outcomes of subcutaneous versus transvenous implantable defibrillator therapy: a meta-analysis and systematic review. Medicine 98:e15490
León Salas B, Trujillo‐Martín M, García García J et al (2019) Subcutaneous implantable cardioverter-defibrillator in primary and secondary prevention of sudden cardiac death: a meta-analysis. Pacing Clin Electrophysiol 42:1253–1268
Francia P, Biffi M, Adduci C et al (2020) Implantation technique and optimal subcutaneous defibrillator chest position: a PRAETORIAN score-based study. Europace 22:1822–1829
Sheldon SH, Cunnane R, Lavu M et al (2018) Perioperative hematoma with subcutaneous ICD implantation: Impact of anticoagulation and antiplatelet therapies. Pacing Clin Electrophysiol 41:799–806
Evenson C, Saour B, Afzal MR et al (2019) Increased risk of hematoma with uninterrupted warfarin in patients undergoing implantation of subcutaneous implantable cardioverter defibrillator. Pacing Clin Electrophysiol 42:1111–1114
Jan S (2020) The subcutaneous ICD for prevention of sudden cardiac death: current evidence and future directions. Pacing Clin Electrophysiol 43:1421–1427
Abdin A, Aktaa S (2022) Subcutaneous ICD for more and transvenous ICD for few?! Clin Res Cardiol. https://doi.org/10.1007/s00392-022-01990-8
Nordkamp OLR, Dabiri Abkenari L, Boersma LV et al (2012) The entirely subcutaneous implantable cardioverter-defibrillator: initial clinical experience in a large Dutch cohort. J Am Coll Cardiol 60:1933–1939
Lambiase PD, Barr C, Theuns DA et al (2014) Worldwide experience with a totally subcutaneous implantable defibrillator: early results from the EFFORTLESS S‑ICD registry. Eur Heart J 35:1657–1665
Kooiman KM, Knops R, Olde Nordkamp L et al (2014) Inappropriate subcutaneous implantable cardioverter-defibrillator shocks due to T‑wave oversensing can be prevented: implications for management. Heart Rhythm 11:426–434
Knops RE, Brouwer T, Barr CS et al (2016) The learning curve associated with the introduction of the subcutaneous implantable defibrillator. Europace 18:1010–1005
Funding
Sources: This study was supported by the National Key Clinical Specialty Discipline Construction Program of China (No. YW2021-002), the Shanghai Clinical Research Center for Interventional Medicine (No. 19MC1910300), and the Science and Technology Commission of Shanghai Municipality (No. 19441906500).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
L. Zhang, X. Li, Y. Liang, J. Wang, M. Li, L. Pan, X. Chen, S. Qin, J. Bai, W. Wang, Y. Su and J. Ge declare that they have no competing interests.
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
The authors Lei Zhang, Xiao Li, and Yixiu Liang contributed equally to the manuscript.
Rights and permissions
About this article
Cite this article
Zhang, L., Li, X., Liang, Y. et al. Real-world evidence for the use of subcutaneous implantable cardioverter–defibrillators in China: A single-center experience. Herz 48, 462–469 (2023). https://doi.org/10.1007/s00059-023-05192-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-023-05192-4
Keywords
- Subcutaneous implantable cardioverter–defibrillator
- Sudden cardiac death
- Efficacy
- Safety
- Chinese population