Abstract
Arrhythmia-induced cardiomyopathy (AIC) is classified as a form of dilated cardiomyopathy in which left ventricular systolic dysfunction (LVSD) is triggered by tachycardic or arrhythmic heart rates. On the one hand AIC can develop in patients without cardiac disease and on the other hand it can appear in patients with pre-existing LVSD, leading to a further reduction in left ventricular (LV) ejection fraction. A special aspect of AIC is the potential termination or partial reversibility of LVSD; thus, AIC is curatively treatable by the elimination of the underlying arrhythmia. Since arrhythmias are often seen merely as a consequence than as an underlying cause of LVSD, and due to the fact that the diagnosis of AIC can be made only after recovery of LV function, the prevalence of AIC is probably underestimated in clinical practice. Pathophysiologically, animal models have shown that continuous tachycardic pacing induces consecutive changes such as the occurrence of LVSD, increased filling pressures, LV dilatation, and decreased cardiac output. After termination of tachycardia, reversibility of the described pathologies can usually be observed. Studies in human ventricular myocardium have recently demonstrated that various cellular structural and functional mechanisms are activated even by normofrequent atrial fibrillation, which may help to explain the clinical AIC phenotype.
Zusammenfassung
Die arrhythmieinduzierte Kardiomyopathie (AIC) gehört zum Formenkreis der dilatativen Kardiomyopathie, bei der durch tachykarde bzw. arrhythmische Herzfrequenzen eine linksventrikuläre systolische Dysfunktion (LVSD) ausgelöst wird. Dabei kann sich die AIC sowohl bei Patient*innen ohne kardiale Erkrankung entwickeln als auch auf dem Boden einer bereits bestehenden LVSD zu einer weiteren Reduktion der linksventrikulären (LV) Ejektionsfraktion führen. Einen besonderen Aspekt der AIC stellt die potenziell vollständige oder partielle Reversibilität der LVSD dar. Somit ist die AIC durch kausale Beendigung der zugrunde liegenden Rhythmusstörung kurativ behandelbar. Da eine Rhythmusstörung häufig nur als Folge, aber nicht als zugrunde liegende Ursache einer LVSD gesehen wird und die Diagnose einer AIC erst nach Erholung der LV-Funktion gestellt werden kann, wird die AIC-Prävalenz im klinischen Alltag wahrscheinlich unterschätzt. Pathophysiologisch wurde in Tiermodellen gezeigt, dass durch kontinuierliche tachykarde Stimulation konsekutiv Veränderungen wie das Auftreten einer LVSD, erhöhte Füllungsdrücke, LV-Dilatation sowie ein vermindertes Herzzeitvolumen induziert werden. Nach Beendigung der Tachykardie kann in der Regel eine Reversibilität der genannten pathologischen Veränderungen beobachtet werden. Untersuchungen in humanem ventrikulärem Myokard ergaben, dass auch ein normofrequentes Vorhofflimmern verschiedene funktionelle und strukturelle zelluläre Veränderungen hervorruft, die zur Erklärung des klinischen AIC-Phänotyps beitragen können.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Heart failure (HF) is a major global health burden, affecting about 38 million people worldwide. It is associated with high morbidity and mortality. The rising prevalence of this disease due to general population growth and increasing life expectancy poses a great challenge to healthcare systems [1, 2]. One cause of HF is left ventricular systolic dysfunction (LVSD) triggered by atrial or ventricular arrhythmias, defined as arrhythmia-induced cardiomyopathy (AIC) or tachycardiomyopathy [3, 4]. Arrhythmia-induced cardiomyopathy constitutes a subtype of dilated cardiomyopathy (DCM) and is characterized by arrhythmia-induced LVSD and eventually left ventricular (LV) dilatation [3].
There are two different types of AIC: on the one hand, arrhythmia as the sole cause for the development of AIC (arrhythmia-induced). In this condition, rhythm restoration leads to complete reversibility of LVSD. On the other hand, pre-existing LVSD can be exacerbated by an arrhythmia (arrhythmia-mediated/superimposed) and LV function recovers only partially after rhythm control therapy [5]. The latter type of AIC is even less understood.
Some factors seem to make the occurrence of AIC more likely, for example, an insidious onset of arrhythmia and the persistence of a rhythm disorder. There is no specific threshold for the onset of AIC regarding heart rate. Furthermore, it is likely that predispositions to the disease exist such as genetic causes [4, 6]. This assumption is emphasized by retrospective analysis that showed that patients without a history of coronary artery disease or HF were more likely to develop LVSD after onset of atrial fibrillation (AFib) when they had a first-degree relative with HF [7].
The prevalence of AIC remains unclear because the diagnosis can only be established ex juvantibus, which means after recovery of LV function due to rhythm restoration. In addition, rhythm disorders are often regarded as a result but not considered as a potential trigger of LVSD.
Several studies have demonstrated the existence of a relevant proportion of patients with idiopathic LVSD and concomitant arrhythmia who develop improved left ventricular ejection fraction (LVEF) following rhythm control, suggesting that the AIC prevalence in these cohorts may range from 57% to 94% [8,9,10]. However, there is a huge heterogeneity regarding patient characteristics and selection, for example, some trials have included patients with other causes of LVSD whereas others have not. Therefore, there is a clear need for further well-designed and prospective trials investigating the prevalence of this particular disease.
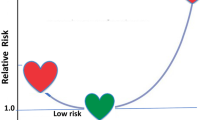
The complicated association of heart failure and arrhythmias
Atrial fibrillation is the most common rhythm disorder in patients with HF [11]. Up to 50% of patients with HF suffer from AFib, and 20–30% of patients with AFib simultaneously have HF [12,13,14]. Even here, in many cases, it remains unclear whether AFib is the cause of HF or whether the arrhythmia occurs secondary to impaired LV function ([15]; the “chicken and egg question”). Therefore, the coexistence of HF and AFib is of high clinical relevance, as it is associated with an elevated risk of cardiovascular morbidity and mortality [16, 17]. To date, the mechanisms by which AFib leads to HF remain incompletely understood and are discussed in the next section. If HF represents the cause of AFib, several mechanisms favor the onset of AFib. This includes elevation of cardiac filling pressures, chronic inflammation, changes in cellular ion homeostasis, and fibrosis and mitral insufficiency, for instance ([12, 18, 19]; Fig. 1).
The vicious cycle of arrhythmias and left ventricular systolic dysfunction (LVSD). There is a close interaction between arrhythmias and LVSD: arrhythmias (mainly atrial fibrillation) can cause or aggravate LVSD, while LVSD can trigger arrhythmias, thereby constituting a vicious circle. Most of the time, it remains unclear whether arrhythmia or LVSD came first
As AIC is currently a diagnosis of exclusion (of other causes for LVSD) and can only be established retrospectively when LVSD has recovered in response to rhythm restoration, it is important to identify predictors of AIC to facilitate primary and precise diagnosis and, on in addition, to help identifying patients who will respond to causal rhythm therapy and those who will not. Unfortunately, there are only a few analyses and reports with mostly limited and retrospective designs. Several clinical trials could demonstrate the superiority of AFib ablation compared to respective medical treatment. The AATAC trial randomized patients with AFib and LVEF < 40% to either catheter ablation or amiodarone. In this trial, AFib ablation was superior in reducing the risk of AFib recurrence after a 2-year-follow-up and lowered the risk for hospitalizations and mortality [20]. Patients with paroxysmal or persistent AFib and LVEF ≤ 35% included in the CASTLE-AF trial were either treated with catheter ablation or medical standard therapy. Medical therapy primarily aimed at restoring sinus rhythm or alternatively focused on adequate rate control. Catheter ablation of AFib led to a reduction of the composite primary endpoint of death from any cause or hospitalization for worsening HF [21]. In addition, further analysis of the CASTLE-AF trial showed that a low AFib burden of < 50% 6 months after the intervention was associated with reduced mortality and hospitalization for HF as well as a distinct improvement of LV function [22].
The CAMERA-MRI study chose an interesting design: Patients with persistent AFib and unexplained LVEF ≤ 45% were randomized to an ablation therapy group or medical rate control group [23]. All patients underwent medical rate control followed by AFib catheter ablation in the intervention arm, so that the tachycardia component between the two groups could not influence the outcome. Recovery of LVEF was significantly more pronounced after AFib ablation and thereby by rhythm restoration compared to medical rate control. Therefore, termination of the arrhythmic excitation of the LV seems to play an important role in LVEF recovery. Next to improved LV function, atrial and ventricular chamber dimensions, brain natriuretic peptide (BNP) levels, and New York Heart Association functional class were reduced. A strength of this study was the exclusion of individuals with other reasons for LVSD, for example, relevant coronary artery disease. Thus, only patients with idiopathic LVEF ≤ 45% were studied [23].
In this trial, it was also shown that cardiac magnet resonance imaging (cMRI) may be a potential tool to possibly predict AIC. Patients underwent cMRI to determine the amount of ventricular fibrosis that was measured by late gadolinium enhancement (LGE). Results showed that absence of LGE was associated with significantly improved LVEF recovery. Furthermore, patients without LGE were more likely to have normal LV function at the end of follow-up (73% vs. 21%). In a univariate analysis, the presence of LGE, indexed left ventricular end systolic volume and indexed left ventricular end diastolic volume were predictive of normalization of LV function. However, the multivariable analysis only identified the absence of LGE as a predictor of LVEF normalization [23]. A limitation was the inclusion of a relatively small number of patients. Thus, ventricular fibrosis as a predictor of AIC should be evaluated in lager prospective clinical trials.
Next to LGE, serial measurement of the N‑terminal pro-B-type natriuretic peptide (NT-proBNP) in peripheral blood samples may be useful for detecting AIC. Once the arrhythmia has been terminated, AIC is associated with a faster decline of NT-proBNP levels and may thus be differentiated from “more irreversible” DCM [4, 24]. A study that included 40 patients with supraventricular arrhythmia who presented with a heart rate ≥ 100 bpm and LVEF < 40% showed that after successful cardioversion was performed, NT-proBNP levels declined more rapidly after a 4-week follow-up period when AIC was diagnosed compared to patients without AIC [25].
Endomyocardial biopsies from patients with a clinical diagnosis of AIC reveal significant changes compared to biopsies from probands with DCM or inflammatory cardiomyopathy. In AIC myocardium, expression of major histocompatibility complex class II molecules and infiltration of CD68+ macrophages were increased, the occurrence of myocardial fibrosis was reduced, and an abnormal distribution pattern of mitochondria was identified. Thus, biopsies may contribute to the detection of AIC, but their significance in daily clinical practice has yet to be evaluated by prospective studies [26].
Lastly, parameters of LV geometry may also predict AIC. In addition to the findings of the CAMERA-MRI study, in a trial with 81 pediatric patients, a smaller left ventricular end diastolic diameter (LVEDD) at baseline was associated with normalization of LVEF [27].
In summary, some clinical parameters that might predict AIC have been suggested. However, prospective evaluation in sufficient clinical trials of this topic is required.
Left ventricular systolic dysfunction caused by atrial flutter (AFlut) is less well characterized than AFib-induced LVSD and information about the epidemiology of AFlut-related AIC is scarce. Since rate control therapy in AFlut is more difficult than in AFib, catheter ablation is of great therapeutic importance [13, 24]. Brembilla-Perrot et al. retrospectively investigated 1269 patients with AFlut and ablation therapy. They found that 184 patients had reduced LVEF < 40% at baseline, and of these patients, 56% were considered to have AIC because of their marked improvement in LV function following ablation [13]. A small analysis of 11 patients with AFlut and LVEF < 50% demonstrated a significant improvement in LV function (30.9 ± 11.0% to 41.3 ± 16%, p = 0.005) after catheter ablation with six of 11 patients showing complete recovery after a follow-up of 7 months [28]. In another AFlut ablation study, 25% of a total of 111 patients had LVSD at baseline. Of these, 57% developed a significant increase in LVEF that constitutes the relevant AIC component. Interestingly, a higher ventricular heart rate during arrhythmia could predict reversibility of LVSD in this analysis [10].
Frequent premature ventricular contractions (PVCs) can also lead to the development of AIC in patients with or without structural heart disease. The most important factor determining the occurrence of AIC in response to PVCs is the degree of PVC burden. Although there is no precise definition for high PVC burden, > 10,000–25,000 PVCs per day are considered to be of significance. Apparently, a threshold value of about 10,000 PVCs per day is considered, above which AIC can develop [24]. After PVC ablation in patients with impaired LV function, LVEF recovered from 34 to 44% (after 6 months) and 46% (after 12 months) during follow-up. At the same time, BNP levels significantly decreased and NYHA functional class significantly increased [29]. An analysis by Zhong et al. focused on 510 patients with frequent PVCs who were referred for radiofrequency ablation or antiarrhythmic drug therapy. Patients in the radiofrequency ablation group showed markedly improved LV function, while no effect on LVEF was seen in the medical therapy group [30].
In summary, patients with unclear LVSD and a high PVC burden should be evaluated intensively including Holter ECG. It is of great importance to establish an aggressive rhythm therapy if AIC is suspected in order to improve LV function and thereby patient outcome.
Pathophysiology
Several different mechanisms contribute to the development of AIC. However, they are still not fully understood [31]. Most of the evidence on the pathophysiology of AIC is based on animal studies. When rapid ventricular pacing is applied in animals, LVSD accompanied by LV dilatation can be observed within the first weeks [32, 33]. As tachycardic stimulation continues, a further decline in LV function, an increase in LA pressure and LV stiffness, and an elevation in systemic vascular resistance and functional mitral regurgitation are characteristics of an emerging end-stage HF phenotype [34,35,36]. After termination of rapid pacing, these changes are reversible within days to weeks [37].
Myocardial energy depletion is one of the underlying factors in the progression of AIC. Animal models investigating AIC have shown diminished levels of creatine, phosphocreatine, and adenosine triphosphate in addition to a reduction in Na+/K+ ATPase activity [38,39,40]. These alterations may be explained by mitochondrial injury as well as by enhanced activity of Krebs cycle enzymes [31]. Moreover, continuous tachycardic stimulation causes impaired myocardial blood flow and elevated coronary vascular resistance [41, 42]. Remodeling in Ca2+ homeostasis such as reduced activity of sarcoplasmic/endoplasmic reticulum Ca2+-ATPase (SERCA) was reported and may also serve as an explanatory approach for contractile dysfunction in AIC [43, 44]. As HF progresses, neurohumoral changes occur due to a reduced cardiac output. Brain and atrial natriuretic peptide elevation is accompanied by increased cardiac filling pressures; a return to normal levels can be observed after termination of rapid pacing [45, 46].
Although the described findings based on animal models are of importance in understanding cellular alterations in AIC, they can only be partially applied to explain AIC in humans. A major limitation of many studies is the use of right ventricular pacing to induce AIC in animals, because this kind of pacing by itself can lead to HF [5]. The development of LVSD in humans due to arrhythmias such as AFib has been a blind spot of cardiovascular research for a long time. Recently, investigations from our research group demonstrated for the first time the negative effects of AFib on LV function when LV samples from patients with and without AFib were compared (Fig. 2). Ventricular tissue samples from patients with AFib were characterized by reduced Ca2+ transient amplitudes and prolonged action potential durations [47]. In addition, in vitro AFib simulation was performed using normofrequent electrical stimulation for 24 h in LV cardiomyocytes from non-HF donors. Likewise, electrical remodeling including a Ca2+ transient amplitude reduction was observed compared to sinus rhythm simulation thereby proving that the arrhythmic component of AFib in the absence of tachycardia induces negative alterations regarding Ca2+ homeostasis. These results could be verified using human ventricular-induced pluripotent stem cell-derived cardiomyocytes (iPSC-CM), which were exposed to in vitro AFib simulation for 7 days. The findings can potentially be explained by a disturbed expression of SERCA, which leads to reduced uptake of Ca2+ into the sarcoplasmic reticulum. In addition, because of an increase in oxidative stress and consequent activation of Ca2+/calmodulin-dependent protein kinase II (CaMKII), ryanodine-receptor 2 (RyR2) phosphorylation is increased, which causes diastolic Ca2+ leakiness and loss. Interestingly, myocardium from donors with AFib did not show higher fibrosis levels compared to the control group, a finding which is in accordance with the fact that AIC is potentially reversible ([47]; Fig. 2). All these mechanisms are well-known typical hallmarks of HF in the human heart [48, 49].
Atrial fibrillation (AFib)-induced pathomechanisms in the human ventricle. AFib increases oxidative stress in human ventricular myocardium with subsequent activation of CaMKII. This leads to a reduction in SR Ca2+ load due to an increase in diastolic Ca2+. Consequently, Ca2+ transient amplitude is reduced. Among others, increased cellular Na+ concentration and action potential prolongation can be observed. (The image is licensed by Shutterstock.com/GraphicsRF.com)
Another study by our research group demonstrated that there is a specific threshold of the arrhythmic burden that is responsible for cellular structural and functional alterations. When iPSC-CM were exposed to an in vitro AFib simulation model, reduced Ca2+ transient amplitudes, action potential prolongation, and a decrease in sarcomere regularity were detected when cells were stimulated with an AFib burden of 60% or higher [50]. These results are of translational relevance because they may explain the impaired outcome of patients with high AFib burden, as shown in a subanalysis of the CASTLE-AF trial when the AFib burden was > 50% following ablation [22].
Diagnostic algorithm
The diagnosis of AIC can be established when an otherwise inexplicable LVSD in combination with arrythmia and/or tachycardia is detected and LV function recovers within several weeks to months after restoration of sinus rhythm [5]. The definition of recovery from LVSD thereby varies between different studies. Usually, complete recovery of LV function with normalization of LVEF or an absolute LVEF increase of ≥ 15% is requested [13, 25, 51]. In this context, it is worth mentioning that the recovery of LV function differs between the arrythmia-induced and the arrythmia-superimposed form of AIC. While normalization of LVEF after appropriate treatment is realistic when arrhythmia-induced AIC is present, LV function can only recover up to the pre-known LVSD in patients with arrhythmia-superimposed AIC (Fig. 3).
Diagnostic algorithm of arrhythmia-induced cardiomyopathy (AIC). When AIC is suspected, several different examinations should be performed or considered according to current guidelines. When the rhythm disorder remains as sole reason for left ventricular systolic dysfunction (LVSD) and left ventricular ejection fraction increases after an appropriate therapy, AIC can be diagnosed
The diagnosis of AIC is one of exclusion and can only be made when other reasons for LSVD can be ruled out. When patients present with suspected AIC, typical HF diagnostic tests should be performed as is recommended in current guidelines, including laboratory testing, 12-channel ECG, transthoracic echocardiography, coronary angiography, and cardiac magnetic resonance imaging (cMRI; [52]).
In addition to a 12-channel ECG to determine heart rate and rhythm, other tools such as Holter ECG monitoring are of diagnostic value if the arrythmia is paroxysmal [5, 52, 53]. Transthoracic echocardiography can be used to assess LVEF and LV geometry including LVEDD. Although the LVEDD is usually smaller in AIC compared with other forms of DCM, there are no absolute echocardiographic criteria to separate AIC from other cardiomyopathies [24, 54]. Cardiac magnetic resonance imaging should be performed in order to exclude other reasons for LVSD, such as myocarditis or storage disease. In addition to this, in some cases endomyocardial biopsies should be considered [52]. In cMRI, the absence of late gadolinium enhancement (LGE), which indicates structural cardiac damage, is suggestive of an AIC and favors the recovery of LV function [55,56,57].
Management
The management of AIC is based on aggressive rhythm restoration and pharmacological strategies to facilitate LV function recovery. If rhythm restoration is not possible, a rate control therapy may be pursued to normalize ventricular heart rates [5, 31]. However, atrioventricular junction ablation in combination with implantation of a biventricular pacemaker constitutes an emerging therapeutic approach for patients with permanent AFib and LVSD and results in reduced mortality compared to rate control therapy [58]. In patients with recurrent arrhythmia, LVSD can dramatically manifest again with an increased risk of sudden cardiac death [59]. Therefore, patients with AIC should be repeatedly followed up including ECG monitoring and echocardiography in order to evaluate heart rhythm and LV function on a regular basis [24].
Rhythm therapy
There is broad agreement that aggressive approaches to restore and control heart rhythm are of utmost importance in AIC [31]. The majority of supraventricular arrhythmias are successfully treatable by catheter ablation, which is associated with good patient outcome including symptom improvement and recovery from LVSD [6, 10, 60]. Current guidelines clearly recommend catheter ablation therapy to improve LV function in patients with AFib and LVSD when AIC is suspected. This phenomenon highlights the significance of rhythm control therapy in AIC [52]. The intervention should already take place at an initial stage because early ablation therapy leads to fewer symptomatic recurrences of rhythm disorders compared to medical antiarrhythmic treatment alone [61]. Of note, independently of a suspected AIC, the importance of early, aggressive rhythm control therapy to maintain sinus rhythm was also demonstrated in the EAST-AFNET 4 trial, which included patients with newly diagnosed AFib. Early rhythm control approaches reduced the risk of adverse cardiovascular events compared to usual care [62]. These findings support early rhythm control in newly diagnosed AFib with new evidence.
As an alternative to direct ablation therapy, cardioversion can be performed as bridging strategy, which is also associated with promising results in terms of improvement in LV function [63]. In many cases, an implantable cardioverter defibrillator (ICD) is not necessary even if patients initially present with a distinct LVSD because of the expected significant LVEF increase [10]. This was demonstrated in a study by Müller-Edenborn et al., who prospectively investigated 50 patients with AFib and LVSD. An inclusion criterion was the absence of significant valvular and coronary artery disease. On day 40 after successful rhythm restoration by cardioversion, the percentage of patients eligible for an ICD implantation fell from 76 to 11% because of improvement in LV function [64]. In light of this, rhythm restoration in LVSD patients with an indication for an ICD should be considered more often in order to avoid unnecessary device therapy. However, a wearable cardioverter defibrillator represents a possible bridging therapy for some patients during the recovery of LV function [65]. As AIC is also provoked by right ventricular pacing, patients with an indication for a pacemaker implantation may benefit from biventricular devices regarding LVEF and LV geometries, regardless of whether the original LV function is reduced or not [66, 67].
Pharmacological therapy
As there is growing evidence underlying the advantages of rhythm control therapy, pharmacological rate control regimes may be considered until rhythm control is achieved or when rhythm control is not possible [68]. As mentioned earlier, an “ablate and pace strategy” in patients with AFib and LVSD is superior to pharmacological rate control [58]. Taken together with our findings of a profound remodeling of the human LV in response to normofrequent AFib, this indicates an important aspect in the treatment of rhythm disorders: not only tachycardia, but also the arrhythmic component alone may lead to negative patient outcome. This is also supported by the prospective CAMERA-MRI trial, which found that patients benefit from restoring sinus rhythm by AFib ablation therapy compared to adequate rate control treatment [23]. Besides rate control, medical cardioversion and long-term antiarrhythmic drug therapy is possible, e.g., using amiodarone, although side effects must be considered [31]. In addition, guideline-directed pharmacological HF therapy, as recommended for the treatment of heart failure with reduced ejection fraction (HFrEF), should be strictly applied for AIC patients because at the time of the initial presentation, the cause of LVSD is usually unclear [5]. In patients with HFrEF, pharmacological treatment should include an angiotensin-converting enzyme (ACE) inhibitor or angiotensin receptor neprilysin inhibitor (ARNI; or angiotensin-receptor blocker if ACE-inhibitor or ARNI are not tolerated), beta-blocker, mineralocorticoid receptor antagonist (MRA), sodium-glucose co-transporter (SGLT) 2 inhibitor, and loop diuretic in the case of volume overload [52]. If-channel inhibitors can be considered in patients with sinus rhythm, LVEF ≤ 35%, and a resting heart rate ≥ 70 bpm. To lower the risk of cardiovascular mortality and HF hospitalizations, soluble guanylate cyclase stimulators may be a therapeutic option. Furthermore, digoxin can be prescribed in symptomatic patients to reduce the risk of hospitalization [52]. If HF with mildly reduced ejection fraction is present, ACE inhibitors/ARNIs, beta-blockers, MRAs and SGLT 2 inhibitors, should also be applied [52].
The duration of pharmacological HF medication in AIC remains unclear especially when LV function has recovered. Even if LV function recovers in AIC, there are certain hints that structural and functional changes remain [24], which is why some continuation of HF therapy may be beneficial. In this context, the new ESC HF guidelines mention “HF with improved LVEF” as a separate form of HF that can be diagnosed when a previous LVSD ≤ 40% recovers to normal levels. Although more research is needed for this special HF entity, the guideline recommends that HF therapy should be continued in patients with HF with improved LVEF [52].
Prognosis
Successful rhythm restoration in patients with AIC usually significantly increases LVEF and LV function recovers to normal levels in many cases. Complete recovery of LVEF is associated with good prognosis in terms of survival [13, 69]. However, even if LV function recovers completely, LV geometry changes such as an enlargement of the LV chamber may still be detected [59].
Conclusion
Cardiac arrythmias can lead to or worsen LVSD and are then referred to as AIC. Due to the difficulty of diagnosing this potentially curable condition, the AIC prevalence remains unclear and is probably underestimated. So far, LVSD caused by AF is the best characterised type of AIC and is accompanied by several electrophysiological changes. Lately, growing evidence arises pointing to the superiority of rhythm control therapy compared to rate control management in patients with AF and impaired LV function. More research including prospective trials is needed to identify predictive factors that help to facilitate diagnosis and to better understand which patients with rhythm disorders and LVSD should definitely be treated by rhythm restoration.
References
Ziaeian B, Fonarow GC (2016) Epidemiology and aetiology of heart failure. Nat Rev Cardiol 13:368–378. https://doi.org/10.1038/nrcardio.2016.25
Burchill LJ, Lee MGY, Nguyen VP et al (2020) Heart failure in adult congenital heart disease. Cardiol Clin 38:457–469. https://doi.org/10.1016/j.ccl.2020.04.010
Mohamed HA (2007) Tachycardia-induced cardiomyopathy (tachycardiomyopathy). Libyan J Med 2:26–29. https://doi.org/10.4176/061226
Huizar JF, Ellenbogen KA, Tan AY et al (2019) Arrhythmia-induced cardiomyopathy: JACC state-of-the-art review. J Am Coll Cardiol 73:2328–2344. https://doi.org/10.1016/j.jacc.2019.02.045
Sossalla S, Vollmann D (2018) Arrhythmia-induced cardiomyopathy. Dtsch Arztebl Int 115:335–341. https://doi.org/10.3238/arztebl.2018.0335
Medi C, Kalman JM, Haqqani H et al (2009) Tachycardia-mediated cardiomyopathy secondary to focal atrial tachycardia: long-term outcome after catheter ablation. J Am Coll Cardiol 53:1791–1797. https://doi.org/10.1016/j.jacc.2009.02.014
Ebbesen MN, D’Souza M, Andersson C et al (2021) Rate of heart failure following atrial fibrillation according to presence of family history of dilated cardiomyopathy or heart failure: a nationwide study. J Am Heart Assoc 10:e21286. https://doi.org/10.1161/JAHA.120.021286
Gentlesk PJ, Sauer WH, Gerstenfeld EP et al (2007) Reversal of left ventricular dysfunction following ablation of atrial fibrillation. J Cardiovasc Electrophysiol 18:9–14. https://doi.org/10.1111/j.1540-8167.2006.00653.x
Hsu L‑F, Jaïs P, Sanders P et al (2004) Catheter ablation for atrial fibrillation in congestive heart failure. N Engl J Med 351:2373–2383. https://doi.org/10.1056/NEJMoa041018
Pizzale S, Lemery R, Green MS et al (2009) Frequency and predictors of tachycardia-induced cardiomyopathy in patients with persistent atrial flutter. Can J Cardiol 25:469–472. https://doi.org/10.1016/s0828-282x(09)70119-9
Larned JM, Raja Laskar S (2009) Atrial fibrillation and heart failure. Congest Heart Fail 15:24–30. https://doi.org/10.1111/j.1751-7133.2008.00041.x
Anter E, Jessup M, Callans DJ (2009) Atrial fibrillation and heart failure: treatment considerations for a dual epidemic. Circulation 119:2516–2525. https://doi.org/10.1161/CIRCULATIONAHA.108.821306
Brembilla-Perrot B, Ferreira JP, Manenti V et al (2016) Predictors and prognostic significance of tachycardiomyopathy: insights from a cohort of 1269 patients undergoing atrial flutter ablation. Eur J Heart Fail 18:394–401. https://doi.org/10.1002/ejhf.482
Lubitz SA, Benjamin EJ, Ellinor PT (2010) Atrial fibrillation in congestive heart failure. Heart Fail Clin 6:187–200. https://doi.org/10.1016/j.hfc.2009.11.001
Pabel S, Sossalla S (2022) Atrial fibrillation and heart failure: novel insights into the chicken and egg dilemma. Eur Heart J. https://doi.org/10.1093/eurheartj/ehac257
Olsson LG, Swedberg K, Ducharme A et al (2006) Atrial fibrillation and risk of clinical events in chronic heart failure with and without left ventricular systolic dysfunction: results from the candesartan in heart failure-assessment of reduction in mortality and morbidity (CHARM) program. J Am Coll Cardiol 47:1997–2004. https://doi.org/10.1016/j.jacc.2006.01.060
Middlekauff HR, Stevenson WG, Stevenson LW (1991) Prognostic significance of atrial fibrillation in advanced heart failure. A study of 390 patients. Circulation 84:40–48. https://doi.org/10.1161/01.cir.84.1.40
Ben Morrison T, Jared Bunch T, Gersh BJ (2009) Pathophysiology of concomitant atrial fibrillation and heart failure: implications for management. Nat Clin Pract Cardiovasc Med 6:46–56. https://doi.org/10.1038/ncpcardio1414
Tsigkas G, Apostolos A, Despotopoulos S et al (2022) Heart failure and atrial fibrillation: new concepts in pathophysiology, management, and future directions. Heart Fail Rev 27:1201–1210. https://doi.org/10.1007/s10741-021-10133-6
Di Biase L, Mohanty P, Mohanty S et al (2016) Ablation versus amiodarone for treatment of persistent atrial fibrillation in patients with congestive heart failure and an implanted device: results from the AATAC multicenter randomized trial. Circulation 133:1637–1644. https://doi.org/10.1161/CIRCULATIONAHA.115.019406
Marrouche NF, Brachmann J, Andresen D et al (2018) Catheter ablation for atrial fibrillation with heart failure. N Engl J Med 378:417–427. https://doi.org/10.1056/NEJMoa1707855
Brachmann J, Sohns C, Andresen D et al (2021) Atrial fibrillation burden and clinical outcomes in heart failure: the CASTLE-AF trial. JACC Clin Electrophysiol 7:594–603. https://doi.org/10.1016/j.jacep.2020.11.021
Prabhu S, Taylor AJ, Costello BT et al (2017) Catheter ablation versus medical rate control in atrial fibrillation and systolic dysfunction: the CAMERA-MRI study. J Am Coll Cardiol 70:1949–1961. https://doi.org/10.1016/j.jacc.2017.08.041
Gopinathannair R, Etheridge SP, Marchlinski FE et al (2015) Arrhythmia-induced cardiomyopathies: mechanisms, recognition, and management. J Am Coll Cardiol 66:1714–1728. https://doi.org/10.1016/j.jacc.2015.08.038
Nia AM, Gassanov N, Dahlem KM et al (2011) Diagnostic accuracy of NT-proBNP ratio (BNP-R) for early diagnosis of tachycardia-mediated cardiomyopathy: a pilot study. Clin Res Cardiol 100:887–896. https://doi.org/10.1007/s00392-011-0319-y
Mueller KAL, Heinzmann D, Klingel K et al (2017) Histopathological and immunological characteristics of tachycardia-induced cardiomyopathy. J Am Coll Cardiol 69:2160–2172. https://doi.org/10.1016/j.jacc.2017.02.049
Moore JP, Patel PA, Shannon KM et al (2014) Predictors of myocardial recovery in pediatric tachycardia-induced cardiomyopathy. Heart Rhythm 11:1163–1169. https://doi.org/10.1016/j.hrthm.2014.04.023
Luchsinger JA, Steinberg JS (1998) Resolution of cardiomyopathy after ablation of atrial flutter. J Am Coll Cardiol 32:205–210. https://doi.org/10.1016/s0735-1097(98)00183-1
Penela D, Van Huls Van Taxis C, Van Huls Van Taxis C et al (2013) Neurohormonal, structural, and functional recovery pattern after premature ventricular complex ablation is independent of structural heart disease status in patients with depressed left ventricular ejection fraction: a prospective multicenter study. J Am Coll Cardiol 62:1195–1202. https://doi.org/10.1016/j.jacc.2013.06.012
Zhong L, Lee Y‑H, Huang X‑M et al (2014) Relative efficacy of catheter ablation vs antiarrhythmic drugs in treating premature ventricular contractions: a single-center retrospective study. Heart Rhythm 11:187–193. https://doi.org/10.1016/j.hrthm.2013.10.033
Simantirakis EN, Koutalas EP, Vardas PE (2012) Arrhythmia-induced cardiomyopathies: the riddle of the chicken and the egg still unanswered? Europace 14:466–473. https://doi.org/10.1093/europace/eur348
Spinale FG, Hendrick DA, Crawford FA et al (1990) Chronic supraventricular tachycardia causes ventricular dysfunction and subendocardial injury in swine. Am J Physiol 259:H218–29. https://doi.org/10.1152/ajpheart.1990.259.1.H218
Armstrong PW, Stopps TP, Ford SE et al (1986) Rapid ventricular pacing in the dog: pathophysiologic studies of heart failure. Circulation 74:1075–1084. https://doi.org/10.1161/01.cir.74.5.1075
Ohno M, Cheng CP, Little WC (1994) Mechanism of altered patterns of left ventricular filling during the development of congestive heart failure. Circulation 89:2241–2250. https://doi.org/10.1161/01.cir.89.5.2241
Shinbane JS, Wood MA, Jensen DN et al (1997) Tachycardia-induced cardiomyopathy: a review of animal models and clinical studies. J Am Coll Cardiol 29:709–715. https://doi.org/10.1016/s0735-1097(96)00592-x
Howard RJ, Moe GW, Armstrong PW (1991) Sequential echocardiographic-Doppler assessment of left ventricular remodelling and mitral regurgitation during evolving experimental heart failure. Cardiovasc Res 25:468–474. https://doi.org/10.1093/cvr/25.6.468
Moe GW, Stopps TP, Howard RJ et al (1988) Early recovery from heart failure: insights into the pathogenesis of experimental chronic pacing-induced heart failure. J Lab Clin Med 112:426–432
Coleman HN, Taylor RR, Pool PE et al (1971) Congestive heart failure following chronic tachycardia. Am Heart J 81:790–798. https://doi.org/10.1016/0002-8703(71)90083-4
Moe GW, Montgomery C, Howard RJ et al (1993) Left ventricular myocardial blood flow, metabolism, and effects of treatment with enalapril: further insights into the mechanisms of canine experimental pacing-induced heart failure. J Lab Clin Med 121:294–301
Spinale FG, Clayton C, Tanaka R et al (1992) Myocardial Na+,K(+)-ATPase in tachycardia induced cardiomyopathy. J Mol Cell Cardiol 24:277–294. https://doi.org/10.1016/0022-2828(92)93165-g
Spinale FG, Grine RC, Tempel GE et al (1992) Alterations in the myocardial capillary vasculature accompany tachycardia-induced cardiomyopathy. Basic Res Cardiol 87:65–79. https://doi.org/10.1007/BF00795391
Shannon RP, Komamura K, Shen YT et al (1993) Impaired regional subendocardial coronary flow reserve in conscious dogs with pacing-induced heart failure. Am J Physiol 265:H801–9. https://doi.org/10.1152/ajpheart.1993.265.3.H801
O’Brien PJ, Ianuzzo CD, Moe GW et al (1990) Rapid ventricular pacing of dogs to heart failure: biochemical and physiological studies. Can J Physiol Pharmacol 68:34–39. https://doi.org/10.1139/y90-004
Perreault CL, Shannon RP, Komamura K et al (1992) Abnormalities in intracellular calcium regulation and contractile function in myocardium from dogs with pacing-induced heart failure. J Clin Invest 89:932–938. https://doi.org/10.1172/JCI115674
Moe GW, Grima EA, Wong NL et al (1993) Dual natriuretic peptide system in experimental heart failure. J Am Coll Cardiol 22:891–898. https://doi.org/10.1016/0735-1097(93)90208-I
Moe GW, Angus C, Howard RJ et al (1990) Pathophysiological role of changing atrial size and pressure in modulation of atrial natriuretic factor during evolving experimental heart failure. Cardiovasc Res 24:570–577. https://doi.org/10.1093/cvr/24.7.570
Pabel S, Knierim M, Stehle T et al (2022) Effects of atrial fibrillation on the human ventricle. Circ Res 130:994–1010. https://doi.org/10.1161/CIRCRESAHA.121.319718
Fischer TH, Herting J, Tirilomis T et al (2013) Ca2+/calmodulin-dependent protein kinase II and protein kinase A differentially regulate sarcoplasmic reticulum Ca2+ leak in human cardiac pathology. Circulation 128:970–981. https://doi.org/10.1161/CIRCULATIONAHA.113.001746
Sossalla S, Fluschnik N, Schotola H et al (2010) Inhibition of elevated Ca2+/calmodulin-dependent protein kinase II improves contractility in human failing myocardium. Circ Res 107:1150–1161. https://doi.org/10.1161/CIRCRESAHA.110.220418
Körtl T, Stehle T, Riedl D et al (2022) Atrial fibrillation burden specifically determines human ventricular cellular remodeling. JACC Clin Electrophysiol. https://doi.org/10.1016/j.jacep.2022.07.016
Hasdemir C, Yuksel A, Camli D et al (2012) Late gadolinium enhancement CMR in patients with tachycardia-induced cardiomyopathy caused by idiopathic ventricular arrhythmias. Pacing Clin Electrophysiol 35:465–470. https://doi.org/10.1111/j.1540-8159.2011.03324.x
McDonagh TA, Metra M, Adamo M et al (2021) 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 42:3599–3726. https://doi.org/10.1093/eurheartj/ehab368
Brugada J, Katritsis DG, Arbelo E et al (2020) 2019 ESC guidelines for the management of patients with supraventricular tachycardiathe task force for the management of patients with supraventricular tachycardia of the European society of cardiology (ESC). Eur Heart J 41:655–720. https://doi.org/10.1093/eurheartj/ehz467
Jeong Y‑H, Choi K‑J, Song J‑M et al (2008) Diagnostic approach and treatment strategy in tachycardia-induced cardiomyopathy. Clin Cardiol 31:172–178. https://doi.org/10.1002/clc.20161
Addison D, Farhad H, Shah RV et al (2016) Effect of late gadolinium enhancement on the recovery of left ventricular systolic function after pulmonary vein isolation. J Am Heart Assoc. https://doi.org/10.1161/JAHA.116.003570
Ling L‑H, Taylor AJ, Ellims AH et al (2013) Sinus rhythm restores ventricular function in patients with cardiomyopathy and no late gadolinium enhancement on cardiac magnetic resonance imaging who undergo catheter ablation for atrial fibrillation. Heart Rhythm 10:1334–1339. https://doi.org/10.1016/j.hrthm.2013.06.019
Lishmanov A, Chockalingam P, Senthilkumar A et al (2010) Tachycardia-induced cardiomyopathy: evaluation and therapeutic options. Congest Heart Fail 16:122–126. https://doi.org/10.1111/j.1751-7133.2010.00147.x
Brignole M, Pentimalli F, Palmisano P et al (2021) AV junction ablation and cardiac resynchronization for patients with permanent atrial fibrillation and narrow QRS: the APAF-CRT mortality trial. Eur Heart J 42:4731–4739. https://doi.org/10.1093/eurheartj/ehab569
Nerheim P, Birger-Botkin S, Piracha L et al (2004) Heart failure and sudden death in patients with tachycardia-induced cardiomyopathy and recurrent tachycardia. Circulation 110:247–252. https://doi.org/10.1161/01.CIR.0000135472.28234.CC
Furushima H, Chinushi M, Sugiura H et al (2004) Radiofrequency catheter ablation for incessant atrioventricular nodal reentrant tachycardia normalized H‑V block associated with tachycardia-induced cardiomyopathy. J Electrocardiol 37:315–319. https://doi.org/10.1016/j.jelectrocard.2004.07.009
Andrade JG, Wells GA, Deyell MW et al (2021) Cryoablation or drug therapy for initial treatment of atrial fibrillation. N Engl J Med 384:305–315. https://doi.org/10.1056/NEJMoa2029980
Kirchhof P, Camm AJ, Goette A et al (2020) Early rhythm-control therapy in patients with atrial fibrillation. N Engl J Med 383:1305–1316. https://doi.org/10.1056/NEJMoa2019422
Zimmermann AJ, Bossard M, Aeschbacher S et al (2015) Effects of sinus rhythm maintenance on left heart function after electrical cardioversion of atrial fibrillation: implications for tachycardia-induced cardiomyopathy. Can J Cardiol 31:36–43. https://doi.org/10.1016/j.cjca.2014.10.032
Müller-Edenborn B, Minners J, Allgeier J et al (2019) Rapid improvement in left ventricular function after sinus rhythm restoration in patients with idiopathic cardiomyopathy and atrial fibrillation. Europace 21:871–878. https://doi.org/10.1093/europace/euz013
Erath JW, Vamos M, Benz AP et al (2018) Usefulness of the WCD in patients with suspected tachymyopathy. Clin Res Cardiol 107:70–75. https://doi.org/10.1007/s00392-017-1159-1
Yu C‑M, Chan JY‑S, Zhang Q et al (2009) Biventricular pacing in patients with bradycardia and normal ejection fraction. N Engl J Med 361:2123–2134. https://doi.org/10.1056/NEJMoa0907555
Kindermann M, Hennen B, Jung J et al (2006) Biventricular versus conventional right ventricular stimulation for patients with standard pacing indication and left ventricular dysfunction: the Homburg biventricular pacing evaluation (HOBIPACE). J Am Coll Cardiol 47:1927–1937. https://doi.org/10.1016/j.jacc.2005.12.056
Camm AJ, Naccarelli GV, Mittal S et al (2022) The increasing role of rhythm control in patients with atrial fibrillation: JACC state-of-the-art review. J Am Coll Cardiol 79:1932–1948. https://doi.org/10.1016/j.jacc.2022.03.337
Ju W, Yang B, Li M et al (2014) Tachycardiomyopathy complicated by focal atrial tachycardia: incidence, risk factors, and long-term outcome. J Cardiovasc Electrophysiol 25:953–957. https://doi.org/10.1111/jce.12428
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
T. Körtl, C. Schach and S. Sossalla declare that they have no competing interests.
For this article no studies with human participants or animals were performed by any of the authors. All studies mentioned were in accordance with the ethical standards indicated in each case.
Rights and permissions
About this article
Cite this article
Körtl, T., Schach, C. & Sossalla, S. How arrhythmias weaken the ventricle: an often underestimated vicious cycle. Herz 48, 115–122 (2023). https://doi.org/10.1007/s00059-022-05158-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-022-05158-y
Keywords
- Arrhythmia-induced cardiomyopathy
- Atrial fibrillation
- Tachycardia
- Left ventricular systolic dysfunction
- Left ventricular ejection fraction