Abstract
Objectives
Endothelial dysfunction is involved in various aspects of vascular biology and different stages of cardiovascular diseases (CVDs). Nucleotide-binding oligomerization domain-containing protein (NOD) 2, a pivotal innate immune receptor for muramyl dipeptide (MDP), has been reported to be a central regulator in CVDs. Previously, we reported that NOD2 played a leading role in MDP-triggered oxidative stress in endothelial cells (ECs). However, whether NOD2 participates in the regulatory mechanism of vascular cell adhesion molecule‑1 (VCAM-1) and endothelin‑1 (ET-1) expression was not elucidated.
Methods
Human umbilical vein endothelial cells (HUVECs) were stimulated with MDP for 12 h. mRNA expression of VCAM‑1 and ET‑1 was detected using real time polymerase chain reaction (PCR). Scrambled control small interfering RNA (siRNA) and NOD2 siRNA were transfected into HUVECs using Lipofectamine 2000 reagent (Invitrogen, Waltham, MA, USA). Furthermore, pyrrolidine dithiocarbamate was adopted to investigate the effect of nuclear factor κB (NF-κB) on NOD2-mediated VCAM‑1 and ET‑1 gene expression in MDP-treated HUVECs.
Results
Data showed that MDP significantly increased VCAM‑1 and ET‑1 mRNA expression, which was dependent on NOD2. In addition, NF-κB inhibition suppressed NOD2-mediated gene expression of VCAM‑1 and ET‑1.
Conclusion
Collectively, we confirmed NOD2 aggravated VCAM‑1 and ET‑1 gene expression through NF-κB in HUVECs treated with MDP.
Zusammenfassung
Zielsetzungen
Eine endotheliale Dysfunktion ist an vielfältigen Aspekten der Gefäßbiologie und an unterschiedlichen Stadien von Herz-Kreislauf-Erkrankungen (CVDs) beteiligt. NOD2 („nucleotide-binding oligomerization domain-containing protein“), ein entscheidender angeborener Immunrezeptor für Muramyldipeptid (MDP), wurde als zentraler Regulator bei Herz-Kreislauf-Erkrankungen beschrieben. In früheren Veröffentlichungen haben wir dargelegt, dass NOD2 eine wesentliche Funktion beim MDP-getriggerten oxidativen Stress in Endothelzellen (ECs) hat. Ob NOD2 jedoch am Regulationsmechanismus der Expression von VCAM‑1 („vascular cell adhesion molecule-1“) und ET‑1 („endothelin-1“) beteiligt ist, ließ sich nicht eindeutig klären.
Methoden
Humane Nabelvenenendothelzellen (HUVECs) wurden 12 h lang mit MDP stimuliert. Wir konnten die mRNA-Expression von VCAM‑1 und ET‑1 mittels Real-time-PCR (Polymerasekettenreaktion) nachweisen. „Scrambled control“ siRNA („small interfering RNA“) und NOD2-siRNA wurden mit Lipofectamine 2000-Reagenz (Invitrogen, Waltham/MA, USA) in HUVECs transfiziert. Ferner wurde Pyrrolidindithiocarbamat eingesetzt, um die Wirkung des nukleären Faktors κB (NF-κB) auf die NOD2-vermittelte VCAM-1- und ET-1-Genexpression in MDP-vorbehandelten HUVECs zu untersuchen.
Ergebnisse
Die Befunde zeigten, dass MDP die von NOD2 abhängige VCAM-1- und ET-1-mRNA-Expression signifikant erhöhte. Darüber hinaus supprimerte die NF-κB-Inhibition die NOD2-vermittelte Genexpression von VCAM‑1 und ET‑1.
Schlussfolgerung
Insgesamt bestätigten wir die durch NOD2 beeinträchtigte VCAM-1- und ET-1-Genexpression mittels NF-κB in mit MDP vorbehandelten HUVECs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular diseases (CVDs) including atherosclerosis are a major cause of death and morbidity worldwide [1]. In China, 45.0% of deaths in rural area and 42.6% of deaths in urban area were caused by CVDs [2]. Although researchers have made great advances in diagnostics and therapy, CVDs still remain the leading cause of death globally. Thus, it is urgent to understand the potential molecular and cellular mechanisms involved in the pathological process of CVDs.
Innate immunity is the first barrier to defend against infection which is also associated with a number of sterile inflammatory conditions such as CVDs [3]. Toll-like receptors (TLRs) and NOD-like receptors (NLRs) are two main sensor families in the innate immune system to detect pathogen-associated molecular patterns (PAMPs) and damage-associated molecular patterns (DAMPs) [4, 5]. NOD2 localized in the cytoplasm was one of first receptors characterized in the NLRs family [6]. According to research, NOD2 has recently been reported to be a central regulator of immune and inflammatory responses in CVDs, such as atherosclerosis and cerebral ischemia/reperfusion injury [5, 7]. Muramyl dipeptide (MDP), a peptidoglycan constituent of both Gram-positive and Gram-negative bacteria, is a defined cognate ligand of NOD2. Peptidoglycan has been detected in atherosclerotic plaques and likely derives from gut microbiota [8]. Furthermore, NOD2 regulates microbiota communities in the gut [9]. Thus, it is important and necessary for us to study MDP-triggered NOD2 innate immune responses in CVDs.
CVDs develop due to a complex interplay of inflammation and coagulation, in which endothelial cells (ECs) are considered to be a central regulator [10, 11]. Endothelial injury leads to the release of coagulation and inflammation mediators, accelerating the adhesiveness of leukocytes [11, 12]. Vascular cell adhesion molecule‑1 (VCAM-1) and intercellular cell adhesion molecule‑1 (ICAM-1), which are both members of the immunoglobulin gene superfamily, are overexpressed in the pathogenesis of endothelial dysfunction [13]. VCAM‑1 is capable of mediating molecular adhesion to ECs after induction of inflammatory cytokines [14]. Numerous studies have reported VCAM‑1 and ICAM‑1 serve as markers of early atherosclerosis and play a significant role in development of atherosclerosis [15,16,17,18]. Furthermore, it has been demonstrated that MDP induces mRNA expression of ICAM‑1 in ECs [8], but whether VCAM‑1 expression could be affected by MDP is not fully understood. ET‑1 synthesized and secreted by ECs has been recognized as the most potent endogenous vasoconstrictor [19]. It accelerates the pathophysiologic progress of CVDs via vasoconstriction. Studies have indicated that atherosclerosis is aggravated by the ET-1-triggered NF-κB signaling pathway [20, 21]. Moreover, there have been reports that lipopolysaccharides (LPS), the principal component of Gram-negative bacteria, dose-dependently increase the release and expression levels of ET‑l in HUVECs [22]. However, it remains unanswered whether MDP leads to a change in VCAM‑1 and ET‑1 production in ECs. Since NOD2 is the defined cognate ligand receptor of MDP, triggered NF-κB-dependent transcriptional activity in ECs after MDP stimulation [23], suggested NOD2 played a potential important role in the ECs. Furthermore, we previously proved MDP induced oxidative stress through the NOD2/COX-2/NOX4 signaling pathway in the HUVECs [6]. However, there was no direct evidence whether NOD2 is involved in the production of VCAM‑1 and ET‑1. Thus, in this study, our goal was to investigate the role and mechanism of NOD2 in MDP-triggered VCAM‑1 and ET‑1 gene expression in primary human umbilical vein endothelial cells (HUVECs).
Materials and methods
Cell culture and stimulation
The cell line of HUVECs was purchased from ScienCell Research Laboratories (Carlsbad, CA, USA) which provides a variety of normal human and animal cells for the research community. Briefly, the HUVECs were cultured with endothelial cell medium (ECM, ScienCell Research Labs, Carlsbad, CA, USA) supplemented with 5% fetal bovine serum, 1% penicillin–streptomycin, and 1% endothelial cell growth supplement (ECGS) at 37 °C with 5% CO2.
Reagents
MDP (53678-77‑6, InvivoGen, San Diego, CA, USA) was used at a final concentration of 10 μg/mL. Pyrrolidine dithiocarbamate (PDTC) was obtained from Beyotime Biotechnology (Shanghai, China).
Small interfering RNA and cell transfection
Scrambled control small interfering RNA (siRNA) and NOD2 siRNA were purchased from Sangon Biotech Co. Ltd. (Shanghai, China). The sequences of NOD2-targeted siRNA and non-targeted siRNA are listed in Table 1. The HUVECs were seeded in a 6-well plate at a density of 4 × 105 cells per well and cultured overnight to 70% confluence. Scrambled control siRNA and NOD2 siRNA were transfected into the HUVECs at a final dose of 50 nM diluted in the ECM medium without fetal bovine serum by Lipofectamine 2000 reagent (Invitrogen, Waltham, MA, USA), following the manufacturer’s instructions.
RNA extraction and real-time reverse transcription (qRT) PCR
Total RNA was extracted from HUVECs using trizol reagent (Invitrogen, Waltham, MA, USA). RT-PCR was implemented by a prime script RT reagent kit (Takara, Dalian, China) according to the manufacturer’s instruction. The mRNA levels of VCAM‑1 and ET‑1 were measured by qRT-PCR using SYBR premix ex taq II (Takara, Dalian, China) on a Bio-Rad iCycler system (BioRad, Hercules, CA, USA). The 2−∆∆CT method was adopted to determine the relative expression of target genes. The specific primers for qRT-PCR are listed in Table 2. GAPDH was used as the housekeeping gene.
Statistics
All of the experiments were performed in triplicate. Data were expressed as mean ± SEM and analyzed with the student’s t‑test using GraphPad Prism 5.01 software. A value of P < 0.05 was considered statistically significant.
Results
MDP up-regulated mRNA expression levels of VCAM-1 and ET-1
In order to examine the effect of MDP in ECs, we treated HUVECs with MDP for 12 h at a concentration of 10 μg/mL. From the experimental data shown in Fig. 1, both VCAM‑1 and ET‑1 mRNA expression were significantly up-regulated by MDP, especially VCAM‑1. The mRNA expression level of VCAM‑1 in the MDP-treated group was more than twice as high as the control group. These data suggest that NOD2, the MDP specific receptor, might play an important role in VCAM‑1 and ET‑1 gene expression in HUVECs.
Gene expression levels of VCAM‑1 (a) and ET‑1 (b) were promoted by MDP in HUVECs. HUVECs were cultured with MDP for 12 h at an indicated dose of 10 μg/mL. The mRNA expression of VCAM‑1 and ET‑1 in HUVECs was detected via qPCR. *P < 0.05, **P < 0.01 and ***P < 0.001, vs. control. VCAM-1 vascular cell adhesion molecule‑1, ET‑1 endothelin‑1, HUVEC human umbilical vein endothelial cells, MDP muramyl dipeptide, qPCR quantitative polymerase chain reaction
NOD2 gene silence inhibited VCAM-1 and ET-1 gene expression in MDP-treated HUVECs
To assess the exact function of NOD2 in the MDP-induced increase of VCAM‑1 and ET‑1 mRNA levels, NOD2-siRNA was transfected into HUVECs with Lipofectamine 2000 regent according to the manufacturer’s instructions. Our results showed that there was no statistical difference between the two groups regarding NOD2 siRNA or NOD2 siRNA with MDP stimulation, based on the gene expression of VCAM‑1 and ET‑1 (Fig. 2). After NOD2 knockdown, VCAM‑1 and ET‑1 gene expression were both inhibited in MDP-treated HUVECs. Thus, it confirmed that NOD2 plays a critical role in VCAM‑1 and ET‑1 gene up-regulation.
NOD2 inhibition suppressed mRNA expression of VCAM‑1 (a) and ET‑1 (b) in MDP-treated HUVECs. Scrambled siRNA and NOD2 siRNA respectively were transferred into HUVECs. VCAM‑1 and ET‑1 mRNA expression were determined by qPCR. *P < 0.05, **P < 0.01 and ***P < 0.001, vs. control. NOD2 nucleotide-binding oligomerization domain-containing protein 2, VCAM-1 vascular cell adhesion molecule‑1, ET‑1 endothelin‑1, siRNA small interfering RNA, HUVEC human umbilical vein endothelial cells, MDP muramyl dipeptide, qPCR quantitative polymerase chain reaction
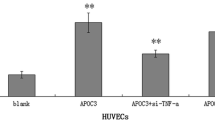
VCAM-1 and ET-1 mRNA expression levels down-regulated by PDTC in MDP-treated HUVECs
NF-κB plays a regulatory role in immune response and participates in inflammatory cytokine production [24, 25]. It was reported that LPS enhances expression of VCAM‑1 via the NF-κB signaling pathway in HUVECs [8]. Furthermore, ET‑1 expression was up-regulated by NF-κB in LPS-treated ECs [22]. Therefore, we speculated that MDP induces VCAM‑1 and ET‑1 gene expression via NF-κB. Next, the HUVECs were pre-incubated with PDTC, which is a specific inhibitor of NF-κB, for 2 h before MDP stimulation. Results indicated that there was a significant difference between the two conditions (Fig. 3). Compared to the MDP group, mRNA expression of VCAM‑1 and ET‑1 were dramatically suppressed in MDP-cultured HUVECs treated with PDTC. Taken together, it was noted that NF-κB is a critical mediator in NOD2-triggered VCAM‑1 and ET‑1 gene overexpression in HUVECs (Fig. 4).
PDTC suppressed the mRNA expression of VCAM‑1 (a) and ET‑1 (b) in MDP-treated HUVECs. HUVECs were pretreated with PDTC at a concentration of 100 μM for 2 h, and then stimulated with MDP for 12 h. qPCR was performed to detect the mRNA expression of VCAM‑1 and ET‑1. *P < 0.05, **P < 0.01 and ***P < 0.001, vs. control. PDTC pyrrolidine dithiocarbamate, VCAM-1 vascular cell adhesion molecule‑1, ET‑1 endothelin‑1, HUVEC human umbilical vein endothelial cells, MDP muramyl dipeptide, qPCR quantitative polymerase chain reaction
Schematic representation showing the NOD2 signaling pathway in HUVECs. MDP stimulation promoted gene expression of VCAM‑1 and ET‑1 in endothelial cells. VCAM-1 vascular cell adhesion molecule‑1, ET‑1 endothelin‑1, HUVEC human umbilical vein endothelial cells, MDP muramyl dipeptide, qPCR quantitative polymerase chain reaction, NF-κB nuclear factor κB
Discussion
Although research into NOD2-mediated innate immune responses in the pathogenesis of inflammatory diseases has recently made great progress, our research provides new insights on NOD2 in CVDs. Vascular endothelium cells are now acknowledged to be a major regulator of vascular homeostasis [26, 27]. ECs dysfunction is a significant marker of CVDs [28]. In the present study, we revealed that MDP, which is regarded as an agonist of NOD2, induced mRNA expression of VCAM‑1 and ET‑1 through NF-κB in the HUVECs.
The innate immune response has been reported to be definitely involved in the chronic inflammation of CVDs [5, 6, 29]. NOD2 which belongs to the NOD-like receptor family is an important mediator in the innate immune system. Growing evidence has confirmed that NOD2 activation triggers the caspase recruitment domain (CARD) and then induces the NF-κB signaling pathway in inflammatory diseases [3, 5, 30]. Compared with the low expression of NOD2 in healthy arteries, its abundance in lesions signifies that the activity of human atherosclerosis is associated with enhanced NOD2-mediated innate immunity [5]. A previous study noted that NOD2 is minimally expressed and readily induced by proinflammatory cytokines in ECs [23]. It indicated that NOD2 is a potential target for the modulation of vascular inflammation. However, there is still doubt of how NOD2 is activated in ECs. An emerging view has been that the gut microbiota is likely the source of peptidoglycans in atherosclerosis. Bacterial phylotypes in atherosclerotic plaques are common to gut microbiota [8]. In several reports, peptidoglycans in vulnerable atherosclerotic plaques were found more often than in stable plaques [5], while MDP, known as a component of most bacterial peptidoglycan, is the only specific ligand for NOD2. Thus, we suggested that MDP might trigger the NOD2 signal pathway in ECs. Moreover, NOD2 plays an important role in the balance of gut microbiota communities [9]. Based on these studies, our goal was to mainly focus on the mechanism of NOD2-induced expression of ET-1 and VCAM-1 rather than other pro-oxidant cytokines.
VCAM‑1, which functions as the mediator of immune cells migration, is a major member in the immunoglobulin superfamily of adhesion molecules [31]. ET‑1 produced by vascular ECs is an amino acid vasoconstrictor peptide and is mainly expressed in the cardiovascular system [32]. It has been demonstrated that ET‑1 overexpression leads to vascular oxidative stress and inflammation, which significantly contributes to development of atherosclerosis [32,33,34]. Our results showed that mRNA expression levels of VCAM‑1 and ET‑1 are up-regulated in HUVECs cultured with MDP for 12 h, which suggests that NOD2 in vascular endothelium might be a potential regulator in adhesion molecules and ET-1expression. Since VCAM‑1 and ICAM‑1 are both endothelial adhesion molecules in the Ig gene superfamily, this is consistent with the report that low expression of NOD2 enabled ECs to express ICAM‑1 in response to MDP [8]. In support of our suggestion, we also investigated the role of NOD2 in MDP-induced VCAM‑1 and ET‑1 expression. The data illustrate that NOD2 indeed mediates the gene levels of VCAM‑1 and ET‑1 in HUVECs stimulated with MDP. As cells lacking NOD2 showed little VCAM‑1 and ET‑1 gene expression, we speculated it might be supplemented by other signaling pathways. Furthermore, because there was no significant difference between the two NOD2-knockdown groups with MDP stimulation or without, it suggested that NOD2 is one of the most critical inducers.
Nevertheless, it still remains unknown how NOD2 mediates VCAM‑1 and ET‑1 overexpression. Coincidentally, we noticed that NOD2-mediates IL‑6, IL‑8, and VCAM‑1 expression in the Porphyromonas gingivalis-induced NF-κB signaling pathway [35]. Previous studies indicated that NOD2 induces NF-κB-dependent transcriptional activity in HUVECs [23]. NF-κB is an important modulator of ET‑1 production in the ECs [36]. In addition, NF-κB participates in the inflammatory signaling pathways in CVDs, leading to the increase of VCAM‑1 expression and monocyte adhesion [37, 38]. Therefore, we investigated whether NF-κB was involved in MDP-induced VCAM‑1 and ET‑1 gene overexpression in HUVECs. As expected, our results from this investigation showed that mRNA levels of VCAM‑1 and ET‑1 are suppressed by PDTC which serves as a NF-kB inhibitor in HUVECs stimulated with MDP. These investigations are in accordance with the report that the expression levels of VCAM‑1 and ET‑1 are up-regulated after LPS treatment [39]. Thus, we confirmed that NF-κB plays a pivotal role in the NOD2-mediated VCAM‑1 and ET‑1 gene expression in HUVECs.
Overall, this study concentrated on NOD2-mediated VCAM‑1 and ET‑1 gene expression in ECs, thus, contributing to our understanding of the innate immune mechanism of ECs. However, since protein levels reveal the regulatory mechanism more accurately and rigorously, it would be more informative and convincing if the protein expression data of VCAM‑1 and ET‑1 were provided. As significant exploration of NOD2 in the pathological process of ECs is needed, we will be conducting these protein experiments in the future.
Conclusion
We confirmed that MDP stimulation triggered mRNA overexpression of VCAM‑1 and ET‑1 in HUVECs. Although NOD2 expression in the ECs was low, it was a significant modulator in VCAM‑1 and ET‑1 mRNA expression. Furthermore, NOD2 mediated VCAM‑1 and ET‑1 gene expression via NF-κB in HUVECs treated with MDP.
References
Saeedf A, Dabhadkar K, Virani SS et al (2018) Cardiovascular disease prevention: training opportunities, the challenges, and future directions. Curr Atheroscler Rep 20(7):35
Ma LY, Wang W, Wu YZ et al (2018) A12514 outline of the report on cardiovascular diseases in China. J Hypertens 36:e322
Chen L, Kong LJ, Wei XB et al (2019) β‑arrestin 2 negatively regulates NOD2 signalling pathway through association with TRAF6 in microglia after cerebral ischaemia/reperfusion injury. J Cell Mol Med 23(5):3325–3335
Stefano DA, Ricciardolo FLM, Caramori G et al (2017) Bronchial inflammation and bacterial load in stable COPD is associated with TLR4 overexpression. Eur Respir J 49(5):1602006
Liu HQ, Zhang XY, Edfeldt K et al (2013) NOD2-mediated innate immune signaling regulates the eicosanoids in atherosclerosis. Arterioscler Thromb Vasc Biol 33:2193–2201
Kong LJ, Liu XQ, Xue Y et al (2018) Muramyl dipeptide induces reactive oxygen species generation through the NOD2/COX-2/NOX4 signaling pathway in human umbilical vein endothelial cells. J Cardiovasc Pharmacol 71(6):352–358
Huiqing L, Xinbing W, Lingjun K et al (2015) NOD2 is involved in the inflammatory response after cerebral ischemia-reperfusion injury and triggers NADPH oxidase 2‑derived reactive oxygen species. Int J Biol Sci 11(5):525–535
Johansson ME, Zhang XY, Edfeldt K et al (2014) Innate immune receptor NOD2 promotes vascular inflammation and formation of lipid-rich necrotic cores in hypercholesterolemic mice. Eur J Immunol 44(10):3081–3092
Ohlsson C, Nigro G, Boneca IG et al (2017) Regulation of bone mass by the gut microbiota is dependent on NOD1 and NOD2 signaling. Cell Immunol 317:55–58
Witkowski M, Landmesser U, Rauch U (2016) Tissue factor as a link between inflammation and coagulation. Trends Cardiovasc Med 26(4):297–303
van Hinsbergh VWM (2012) Endothelium-role in regulation of coagulation and inflammation. Semin Immunopathol 34(1):93–106
Chen YW, Apostolakis S, Lip GYH (2014) Exercise-induced changes in inflammatory processes: implications for thrombogenesis in cardiovascular disease. Ann Med 46(7):439–455
Habas K, Shang LJ (2018) Alterations in intercellular adhesion molecule 1 (ICAM-1) and vascular cell adhesion molecule 1 (VCAM-1) in human endothelial cells. Tissue Cell 54:139–143
Pober JS, Sessa WC (2015) Inflammation and the blood microvascular system. Cold Spring Harb Perspect Biol 7(1):a16345
Rostampour N, Fekri K, Hashemi-Dehkordi E et al (2017) Association between vascular endothelial markers and carotid intima-media thickness in children and adolescents with type 1 diabetes mellitus. J Clin Diagn Res 11(9):SC1–SC5
Peter K, Weirich U, Nordt TK et al (1999) Soluble vascular cell adhesion molecule‑1 (VCAM-1) as potential marker of atherosclerosis. Thromb Haemost 82(S01):38–43
El-Ashmawy HM, Selim FO, Hosny TAM et al (2019) Association of low serum meteorin like (Metrnl) concentrations with worsening of glucose tolerance, impaired endothelial function and atherosclerosis. Diabetes Res Clin Pract 150:57–63
Di Franco M, Lucchino B, Conti F et al (2018) Asymmetric dimethyl arginine as a biomarker of atherosclerosis in rheumatoid arthritis. Mediators Inflamm 2018:ID3897295
Houde M, Desbiens L, D’Orléans-Juste P (2016) Endothelin-1: biosynthesis, signaling and vasoreactivity. Adv Pharmacol 77:143–175
Kowalczyk A, Kleniewska P, Kolodziejczyk M et al (2015) The role of endothelin‑1 and endothelin receptor antagonists in inflammatory response and sepsis. Arch Immunol Ther Exp 63(1):41–52
Jackson AO, Regine MA, Subrata C et al (2018) Molecular mechanisms and genetic regulation in atherosclerosis. Int J Cardiol Heart Vasc 21:36–44
Gopalakrishna D, Pennington S, Karaa A et al (2016) ET‑1 stimulates superoxide production by eNOS following exposure of vascular endothelial cells to endotoxin. Shock 46(1):60–66
Oh HM, Lee HJ, Seo GS et al (2005) Induction and localization of NOD2 protein in human endothelial cells. Cell Immunol 237(1):37–44
Yurdagul A, Sulzmaier FJ, Chen XL et al (2016) Oxidized LDL induces FAK-dependent RSK signaling to drive NF-κB activation and VCAM‑1 expression. J Cell Sci 129(8):1580–1591
Girardin SE, Boneca IG, Viala J et al (2003) NOD2 is a general sensor of peptidoglycan through muramyl dipeptide (MDP) detection. J Biol Chem 278:8869–8872
Rubanyi GM (1993) The role of endothelium in cardiovascular homeostasis and diseases. J Cardiovasc Pharmacol 22:S1–14
Haynes WG, Webb DJ (1998) Endothelin as a regulator of cardiovascular function in health and disease. J Hypertens 16(8):1081–1098
Haybar H, Shahrabi S, Rezaeeyan H et al (2019) Endothelial cells: from dysfunction mechanism to pharmacological effect in cardiovascular disease. Cardiovasc Toxicol 19(1):13–22
Xin Z, Chonghuai G, Chenghui Y et al (2016) NALP3-inflammasome-related gene polymorphisms in patients with prehypertension and coronary atherosclerosis. Biomed Res Int 2016:1–10
Ting JP, Duncan JA, Lei Y (2010) How the noninflammasome NLRs function in the innate immune system. Science 327:286–290
Henseleit U, Steinbrink K, Sunderkötter C et al (1994) Expression of murine VCAM‑1 in vitro and in different models of inflammation in vivo: correlation with immigration of monocytes. Exp Dermatol 3(6):249–256
Javeshghani D, Barhoumi T, Idris-Khodja N et al (2013) Reduced macrophage-dependent inflammation improves endothelin-1-induced vascular injury. Hypertension 62(1):112–117
Idriskhodja N, Ouerd S, Trindade M et al (2017) Vascular smooth muscle cell peroxisome proliferator-activated receptor γ protects against endothelin-1-induced oxidative stress and inflammation. J Hypertens 35(7):1390–1401
Sofiane O, Noureddine IK, Rehman MMO et al (2016) Lbps 01-03 endothelin‑1 overexpression exaggerates diabetes-induced endothelial dysfunction by altering oxidative stress balance. J Hypertens 34:e174
Liu J, Wang Y, Ouyang X (2014) Beyond toll-like receptors: porphyromonas gingivalis induces IL‑6, IL‑8, and VCAM‑1 expression through NOD-mediated NF-κB and ERK signaling pathways in periodontal fibroblasts. Inflammation 37(2):522–533
Duerrschmidt N, Wippich N, Goettsch W et al (2000) Endothelin‑1 induces NAD(P)H oxidase in human endothelial cells. Biochem Biophys Res Commun 269(3):713–717
Jiang Y, Jiang LLI, Maimaitirexiati XMZY et al (2015) Irbesartan attenuates TNF-α-induced ICAM‑1, VCAM‑1, and E‑selectin expression through suppression of NF-κB pathway in HUVECs. Eur Rev Med Pharmacol Sci 19(17):3295–3302
Addabbo F, Nacci C, Benedictis LD et al (2011) Globular adiponectin counteracts VCAM-1-mediated monocyte adhesion via AdipoR1/NF-κB/COX‑2 signaling in human aortic endothelial cells. Am J Physiol Endocrinol Metab 301(6):E1143–E1154
Huang DG, Zhao QL, Liu HF et al (2016) PPAR‑α agonist WY-14643 inhibits LPS-induced inflammation in synovial fibroblasts via NF-kB pathway. J Mol Neurosci 59(4):544–553
Acknowledgements
The experiments were performed at Biological Medical Research Center of Zhongshan Hospital, Fudan University.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
L.-j. Kong, Y.-n. Wang, Z. Wang and Q.-Z. Lv declare that they have no competing interests.
For this article no studies with human participants or animals were performed by any of the authors. All studies performed were in accordance with the ethical standards indicated in each case.
Rights and permissions
About this article
Cite this article
Kong, Lj., Wang, Yn., Wang, Z. et al. NOD2 induces VCAM-1 and ET-1 gene expression via NF-κB in human umbilical vein endothelial cells with muramyl dipeptide stimulation. Herz 46 (Suppl 2), 265–271 (2021). https://doi.org/10.1007/s00059-020-04996-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-020-04996-y
Keywords
- Nucleotide-Binding Oligomerization Domain-Containing Protein 2 (NOD2)
- Vascular cell adhesion molecule‑1
- Endothelin‑1
- Endothelial dysfunction
- Cardiovascular diseases