Abstract
Half a century after the discovery of chromogranin A as a secreted product of the catecholamine storage granules in the bovine adrenal medulla, the physiological role for the circulating pool of this protein has been recently coined, namely as an important player in vascular homeostasis. While the circulating chromogranin A since 1984 has proved to be a significant and useful marker of a wide range of pathophysiological and pathological conditions involving the diffuse neuroendocrine system, this protein has now been assigned a physiological “raison d’etre” as a regulator in vascular homeostasis. Moreover, chromogranin A processing in response to tissue damage and blood coagulation provides the first indication of a difference in time frame of the regulation of angiogenesis evoked by the intact chromogranin A and its two major peptide products, vasostatin-1 and catestatin. The impact of these discoveries on vascular homeostasis, angiogenesis, cancer, tissue repair and cardio-regulation will be discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Two decades after the reports by Banks and Helle [1] and Blaschko and collaborators [2] on the exocytotic release of catecholamines and chromogranin A (CgA) [3] from the bovine adrenal medulla, O’Connor and Bernstein were the first to demonstrate that human CgA could serve as a conspicuous circulating marker for a wide range of neuroendocrine tumors of the diffuse neuroendocrine system.
Soon thereafter, the primary structure of bovine CgA was deduced independently by two groups, Iachangelo and Eiden, and Huttner and Benedum [4, 5]. Moreover, that same year Tatemoto et al. [6] demonstrated that the pancreatic glucose-induced insulin release was inhibited by a porcine peptide, pancreastatin, that structurally matched with the mid-sequence of CgA. These discoveries led Eiden to postulate that CgA could be the pro-hormone for pancreastatin, while Huttner and Benedum stressed that the pro-hormone function of the widely distributed CgA might not be limited to that of pancreastatin [7, 8]. The most exciting possibility was in their opinion that CgA works as a pro-hormone not only for pancreastatin but also for other, as yet undefined, biologically active peptides.
Two such peptides were soon to be identified, notably the N-terminal vasostatin-1 (CgA1–76) [9] and catestatin (CgA352–372) [10]. These peptides were discovered for their ability to regulate vasoconstriction and catecholamine secretion, respectively, and found later also to be involved in the regulation of angiogenesis, myocardial contractility and innate immunity [11].
The distribution and the structure of CgA and CgA-derived peptides have been the subject of extensive research in a wide range of laboratories since 1984 [11, 12]. However, whether circulating full-length CgA (CgA1–439) has also a direct hormonal function and how, when and to what extent it is processed under normal and pathophysiological conditions, has until recently remained an open question. Recent studies have shed some light on this issue, showing that physiologically relevant levels of circulating CgA can exert important physiological functions on vascular homeostasis, angiogenesis, tissue repair and cardio-regulation [13–16]. The impact of these discoveries will be discussed in the following.
Circulating levels of CgA and its fragments in normal and pathological conditions
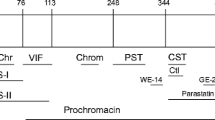
In normal subjects CgA circulates at slightly sub-nanomolar concentration (about 0.5–1 nM), as measured with immunoassays unable to discriminate between full-length CgA and fragments. Using more specific assays (see Fig. 1 for a schematic representation of CgA and assays), we have recently shown that the circulating pool is heterogeneous, consisting of full-length CgA (about 0.1 nM) and a larger proportion of fragments lacking part of, or the entire, C-terminal region [13]. In addition, normal plasma contains a considerable amount of vasostatin-1 (about 0.3–0.4 nM) [13]. Other fragments, not detected by these assays, might be also present. For example, catestatin has been reported to be present in circulation at concentrations ranging from 0.03 nM [17] to 0.33 nM [18] or even up to 1.5 nM [19] in normal subjects. The discrepancies between these values might be related to the use of different antibodies that detect catestatin as well as larger precursors with different efficiency. The molecular entities containing the catestatin sequence detected by these studies were not characterized.
Schematic representation of three different ELISAs with different specificity for full-length CgA and fragments. a. Schematic representation of full-length human CgA1–439. The regions corresponding to vasostatin-1 (CgA1–76, N-terminal region), catestatin (CgA352–372), and C-terminal region 410–439 are also represented with box and circles. b–d Schematic representation of three CgA-ELISAs with different specificity [13]. These assays are based on the use of the same capture antibody (a monoclonal antibody against an epitope present in the N-terminal region of CgA and vasostatin-1) and of three different detection antibodies against epitopes located in the central region of CgA (non-selective ELISA for intact and processed CgA) (b), or against the six C-terminal residues of full-length CgA (selective ELISA for intact CgA) (c), or the six C-terminal residues of vasostatin-1 (selective ELISA for vasostatin-1) (d)
Elevated serum levels of immune-reactive CgA have been found in patients with neuroendocrine tumors, heart failure, renal failure, hypertension, rheumatoid arthritis, diabetic retinopathy, atrophic gastritis, inflammatory bowel disease, sepsis and other inflammatory diseases or in subjects treated with proton pump inhibitors, a class of drugs commonly used to treat acid peptic disorders [11].
A limited number of studies have been published regarding the circulating levels of CgA fragments in pathological conditions. In patients with diabetic retinopathy an attenuation of CgA processing was apparent [20], while recent studies have shown that vasostatin-1 plasma levels are increased in critically ill patients [21]. In these patients vasostatin-1 concentrations above 0.44 nM (>1.4-fold higher than normal values), are associated with poor outcome [21]. Other investigators showed that the catestatin levels, measured using an anti-catestatin antibody capable of cross-reacting with free peptide and full-length CgA, are decreased in patients with essential hypertension and in normotensive subjects with a family history of hypertension and increased epinephrine secretion [19]. Furthermore, plasma catestatin levels, measured with a commercial assay kit, are increased in patients with coronary heart disease and after acute myocardial infarction [18, 22]. However, as mentioned above for normal subjects, the catestatin-containing molecular entities detected by these assays in plasma were not characterized.
Novel regulatory roles of circulating CgA and its fragments
CgA and angiogenesis
Up to today we have been at a loss when it comes to grasp the in vivo impact of the normal, low nanomolar levels of circulating CgA. We are even further away from understanding the functional relevance of the elevated levels of plasma CgA characteristic of various forms of neuroendocrine tumors, or of inflammatory and cardiovascular diseases. The recent report by Crippa et al. [13] has thrown new light on the properties of the circulating CgA and how they may change upon processing in healthy subjects. This study showed that full-length CgA and vasostatin-1 are endowed with potent anti-angiogenic activity in various in vitro and in vivo assays performed with biologically relevant concentrations. These findings imply a novel, unforeseen role for the circulating full-length CgA and vasostatin-1 at normal concentrations, namely in maintenance of the vascular endothelium in a quiescent state. Rather unexpectedly, blood coagulation caused, in a thrombin-dependent manner, an almost complete loss of the anti-angiogenic intact CgA and formation of a pro-angiogenic fragment corresponding to CgA1–373 [13]. This fragment contains the catestatin sequence (CgA352–372) and, like catestatin, can induce secretion of basic fibroblast growth factor (bFGF), a potent pro-angiogenic factor, from cultured endothelial cells [13, 15]. Thus, circulating CgA and CgA-derived polypeptides seemingly form a balance of anti- and pro-angiogenic factors tightly regulated by proteolysis. Based on these findings, a model has been proposed that thrombin-induced alteration of this balance may provide a novel mechanism for triggering angiogenesis in pathophysiologic conditions characterized by prothrombin activation, e.g. in tissue damage and repair [13] (see Fig. 2 for a schematic representation of this model).
Schematic representation of the CgA-dependent angiogenic switch activated by thrombin. a Anti-angiogenic sites. The full-length CgA is an anti-angiogenic molecule with the active site in the C-terminal region 410–439. A latent or less active site in the N-terminal region corresponds to vasostatin-1. Proteolytic cleavage at Q76 liberates vasostatin-1, exerting anti-angiogenic activity at physiological concentrations [13]. Both full-length CgA and vasostatin-1 can inhibit bFGF and VEGF, two potent pro-angiogenic factors. Pro-angiogenic sites: full-length CgA contains also a latent pro-angiogenic site within residues 352–372 (corresponding to the catestatin region). Cleavage of CgA at residue R373 by thrombin generates the fragment CgA1–373 that, like catestatin, can promote angiogenesis by inducing the release of bFGF from endothelial cells [13, 15]. b The angiogenic switch. Schematic representation of the thrombin-activated angiogenic switch in CgA. According to this model, systemically circulating CgA and vasostatin-1 maintain endothelial cell quiescence by their anti-angiogenic potencies. Local activation of thrombin, e.g. in damaged tissues, increases CgA1-373 at the expense of full-length CgA, shifting the local balance toward a pro-angiogenic state [13]
Structure–activity relationship studies have shown that CgA contains a functional anti-angiogenic site in the C-terminal region 410–439 [13] and a latent (or less active) site in the N-terminal region, corresponding to vasostatin-1 (Fig. 2a). Thus, proteolytic cleavage and liberation of the vasostatin-1 fragment is also necessary for full activation of its anti-angiogenic activity. Previous studies have shown that about half of the intra-granular fraction of CgA in the bovine adrenal medulla is proteolytically processed at cleavage sites located at both N- and C-terminal regions of the protein, including Q76 and K78 [23]. This may explain the presence of vasostatin-1 in circulation even in normal subjects. Other studies have shown that vasostatin-1 can inhibit endothelial cell migration, motility, sprouting, invasion and capillary-like structure formation induced by vascular endothelial growth factor (VEGF) and basic fibroblast growth factor (bFGF) [24], further supporting the concept that vasostatin-1 has an anti-angiogenic activity.
Although both circulating vasostatin-1 and CgA might exert anti-angiogenic effects, we speculate that these polypeptides have different roles in the spatiotemporal regulation of angiogenesis. An appealing possibility is that circulating CgA has the dual role of inhibiting angiogenesis in normal conditions, yet accelerating local angiogenesis in damaged tissues, e.g. after cleavage by thrombin. In contrast, the circulating pool of vasostatin-1 might serve to preserve endothelial cell quiescence in normal conditions and to counter-balance, at the systemic level, the pro-angiogenic activity of CgA-derived fragments released in the systemic circulation from injured sites (Fig. 2b).
Intriguingly, vasostatin-1 and catestatin exert opposite effects on the formation of new blood vessels. While vasostatin-1 appears to inhibit angiogenesis, catestatin can, in contrast, activate endothelial cell chemotaxis, proliferation, angiogenesis and vascularization, while inhibiting endothelial cell apoptosis [15]. Thus, changes in the relative levels of the pro-/anti-angiogenic forms of CgA-related polypeptides arising locally and systemically as a consequence to altered secretion and/or proteolytic processing, caused by thrombin and possibly by other proteases, emerge as relevant mechanisms for the spatiotemporal regulation of the CgA-related angiogenic balance.
CgA and the endothelial barrier function
Studies performed in murine models showed that low doses of CgA can enhance the endothelial barrier function in normal tissues and protect vessels from vascular leakage induced by tumor necrosis factor alpha (TNF), a well-known inflammatory cytokine [25]. In vitro experiments showed that low-dose CgA can inhibit the TNF-induced disassembly of VE–cadherin dependent junctions and gap formation in endothelial cell monolayers and, consequently, the paracellular transport of macromolecules [25, 26]. Notably, also the N-terminal fragment of CgA, vasostatin-1, can inhibit the formation of gaps in endothelial cell monolayers and the permeability to macromolecules induced by TNF, VEGF and thrombin [25, 27]. Thus, it seems that intact CgA and its N-terminal fragment at low concentrations close to physiological levels can preserve the endothelial barrier integrity against the disrupting activity of different inflammatory and pro-angiogenic stimuli.
Regarding the mechanism of action, we have shown previously that vasostatin-1 can inhibit TNF-induced phosphorylation of p38-MAPK, by a pertussis toxin-sensitive mechanism, as well as VEGF-induced phosphorylation of ERK in endothelial cells [24, 27], i.e. two signaling pathways that have been implicated in endothelial permeability [28, 29]. Furthermore, the results of high throughput expression profiling of endothelial cells treated with CgA, alone or in combination with TNF, suggest that CgA can affect the expression of many proteins involved in the regulation of cell cytoskeleton rearrangement, a process critical for endothelial cell shape change and vascular permeability [26].
CgA in cardiovascular regulation and inflammation
A growing body of evidence suggests that CgA can contribute to regulate the cardiovascular physiology. The heart, under normal or pathophysiological conditions, is under constant exposure to the circulating CgA derived from the neuroendocrine system. CgA may also derive locally from myocardial production, notably from the diseased ventricle [30]. Under normal conditions, myocardial CgA is expressed at low levels, only detectable by PCR and ELISA, but in the presence of dilated and hypertrophic cardiomyopathy, the protein is also immunologically detectable in tissue sections [30]. The importance of CgA in human cardiovascular homeostasis is suggested by its increased plasma levels and prognostic value in chronic heart failure [31, 32], its overexpression in human dilated and hypertrophic cardiomyopathy [30], and its prognostic value in acute coronary syndromes, independent of conventional risk markers [33]. A regulatory role of CgA in cardiovascular physiology is also suggested by the results of experimental studies performed with ex vivo perfused rat hearts, showing that 0.1–4 nM full-length CgA can dilate coronaries and induce negative inotropism and lusitropism [16]. Remarkably, also the CgA fragments can work as cardio-regulatory hormones, in certain cases with opposite functions. While, full-length CgA, vasostatin-1 and catestatin depress myocardial contractility and relaxation, counteract the β-adrenergic-induced positive inotropism, and modulate coronary tone (via a nitric oxide-dependent mechanism) [16], a fragment corresponding to the C-terminal region CgA411–436, called serpinin, enhances myocardial contractility and relaxation (via a β-adrenergic-cAMP-PKA and nitric oxide-independent pathway) [16, 34–37]. Analysis of the effluents from ex vivo perfused rat hearts showed that exogenous CgA was not cleaved by the heart, suggesting that the circulating, full-length protein can directly induce myocardial effects [16]. However, the same study demonstrated that physically and chemically stimulated rodent hearts can proteolytically process the intracardiac endogenous CgA into fragments. Hence, the systemic and intracardiac fate of full-length CgA and its fragments imply yet other intriguing aspects of the myocardial handling of CgA under normal and pathophysiological conditions.
Interestingly, plasma CgA, which has emerged as an independent marker of mortality in chronic heart failure [30], correlates with TNFα and soluble TNF receptors in these patients [38], pointing to a relationship between high plasma CgA and pro-inflammatory markers. Inflammatory processes, in particular those involving the cardiovascular system, pose clinical challenges in diagnosing and therapy and are acknowledged as pathologic conditions of high clinical significance [39]. Vascular inflammation may induce pathological arterial changes and variable blood pressure, and has been associated with target-organ damage and future cardiovascular complications [40]. Considering the known capability of CgA to inhibit TNF-induced endothelial activation, barrier alteration and vascular leakage [12] the secretion of CgA, in concert with soluble TNF receptors, may contribute to reduce the potentially deleterious effects of TNF on the vascular endothelium.
An inflammatory response is also caused by the myocardial injury arising from ischemic reperfusion (I/R), due to oxidative damage triggering stress-signaling processes that eventually result in myocardial apoptosis and cell death [41]. Apoptosis is a contributor to human myocardial infarction and occurs within 24 h after ischemia, inducing massive losses of myocytes and increasing the susceptibility to cardiac dysfunction [42]. In search of novel therapeutic strategies following myocardial infarction, numerous studies report on ligands and intracellular signaling pathways that may control apoptosis in cardiomyocytes exposed to I/R. Taking into account that CgA is predictive of mortality in patients with chronic heart failure and after acute myocardial infarction, whether elevated circulating levels of CgA are beneficial or detrimental to the heart, has remained an open question. Nevertheless, it is well established that the human recombinant vasostatin-1 preconditions the rat heart against the myocardial necrosis that arise in response to reperfusion of the ischemia-injured tissue [43, 44]. The mechanism for vasostatin-1 eliciting such a protection against ischemic injury appears to involve the endothelial adenosine/nitric oxide signaling pathway [45]. In contrast, catestatin is without pre-conditional effects, yet modulates the reperfusion injury when present during the 2 h post-ischemic reperfusion period. The outcome depends, however, on the mode of ischemia. After global ischemia post-conditioning with catestatin decreased the final reperfusion injury [46], while catestatin significantly enhanced the infarct size when the ex vivo rat heart had been exposed to regional ischemia [47]. In the latter study two forms of catestatin-containing CgA fragments were detected, a 55 kDa form being most prominent in the control heart. Intriguingly, the experimental I/R procedure significantly increased the percentage of a catestatin-containing 27 kDa peptide in the necrotic zones at the expense of the 55 kDa form, indicating that the experimental conditions as such had caused CgA processing [47], distinctly different from the previously reported processing into the vasostatin-1 like, betagranin-containing peptides [48]. CgA is also present in the murine heart. In this species catestatin-related peptides are present both in the cardiocytes and in the heart extracts, consistent with the presence of CgA in cardiac secretory granules [49]. Moreover, the intracardiac processing was far more extensive in the hearts than in the adrenal medulla, giving rise to three main catestatin-containing fragments in the cardiac extracts, while the full-length CgA was virtually absent [49]. Thus, different N- and C-terminal CgA fragments may derive from processing of the circulating and intracardiac pools of CgA in species-specific patterns, not only in the failing or infarcted human heart in situ but also under experimental conditions in animal models [16].
Endothelial cell dysfunction and increased cardiovascular mortality and morbidity are also associated with rheumatoid arthritis [50], a systemic disease characterized by endothelial activation, synovial involvement, bone erosions and with TNFα as a main actor in the pathogenesis. The concentration of circulating CgA in patients with rheumatoid arthritis is higher than in the synovial tissues and is assumed to be of systemic origin [51]. Importantly, CgA1-78, like the sera from rheumatoid arthritis patients, inhibited the TNFα-mediated vascular inflammation [52], suggesting that enhanced levels of CgA may contribute to a negative feedback loop that limits the activation of endothelial cells in rheumatoid arthritis. Further work is needed to establish the relative ratio of full-length CgA to N- and C-terminal processed products in these patients.
CgA in vascular regulation of cancer development
The main reason for the increased circulating levels of CgA in patients with neuroendocrine tumors is that neoplastic cells, in these diseases, store CgA in secretory granules and release it in abnormal amounts, first in the tumor microenvironment and subsequently into the circulation. For these reasons CgA is widely used as a serological marker for neuroendocrine tumor diagnosis and monitoring [3, 53–57]. Notably, the CgA plasma levels, as measured with immunoassays that are unable to discriminate full-length CgA and fragments of CgA, are increased up to 10–100-fold in certain patients, implicating that the blood vessels of neuroendocrine tumors are typically exposed to extremely high concentrations of CgA and/or its fragments. Given their potential ability to regulate tumor vessel biology, these CgA molecules might also contribute to regulate tumor growth. This view is supported by the observation that mouse lymphomas and mammary adenocarcinomas genetically engineered to release CgA showed a reduced growth rate compared to wild type cells [58]. Although these findings demonstrate that CgA, locally produced, might indeed contribute to regulate tumor growth, the degree of CgA proteolytic processing was not characterized in this study. Considering that tumors in patients and animal models may generate different fragments, with potentially different biological effects, further studies are necessary to clarify the role of local CgA in neuroendocrine tumor progression.
Another important issue that deserves to be discussed is whether circulating CgA can affect the growth and progression of non-neuroendocrine tumors, i.e. of tumors unable to release CgA locally, but still exposed to the CgA released by the neuroendocrine system into the blood. A recent study performed in animal models has shown that CgA and vasostatin-1 can reduce the trafficking of tumor cells from tumor-to-blood, from blood-to-tumor and from blood-to-normal tissues (i.e. the tumor “self-seeding” and metastasis processes), by enhancing the endothelial barrier function and reducing the trans-endothelial migration of cancer cells [26]. Furthermore, the findings that pathophysiological levels of CgA can regulate angiogenesis (discussed above) suggest that low levels of full-length CgA or changes in its fragmentation may also affect the growth of primary tumors. Although this hypothesis is supported by the observation that low-dose vasostatin-1 (20 ng, daily) can reduce angiogenesis and tumor growth in three different murine models [13], the key question that remains to be addressed is whether circulating full-length CgA and the other fragments can also affect angiogenesis and tumor growth and how, when and where this protein is processed in different pathological conditions.
Relevant to this discussion is also the observation that full-length CgA shows biphasic dose–response curves in angiogenesis assays, with maximal effects at 1 nM CgA and progressive loss of activity at higher concentrations [13]. This may further complicate the interpretation of the biological effect of CgA in patients with endocrine versus non-neuroendocrine tumors, considering the markedly different local CgA concentrations in tumors and the potentially different proteolytic processing in these clinical settings.
Putative receptors and mechanisms
Two aspects have remained unanswered for decades, namely the question of receptors and the concentrations needed to obtain the reported effects of the intact CgA and of the major peptides, vasostatin-1 and catestatin.
Bovine endothelial cells can bind and internalize 1 nM 125I-labeled CgA [59], which implicates the presence of high affinity binding sites on these cells. Specific high affinity binding proteins with Kd of ~40 nM and an apparent molecular weight of 75 kD have been identified for vasostatin-1 and the N-terminal domain CgA1–40 in cultured calf smooth muscle cells [60] and parathyroid cells [61]. In bovine aortic endothelial cells a mechanism involving the interaction of vasostatin-1 with heparan sulfate proteoglycans, caveolae endocytosis and a phosphoinositide 3-kinase (PI3K)-dependent eNOS phosphorylation has been also proposed [62]. This hypothesis is based on observation that caveolae-dependent endocytosis induced by vasostatin-1 was significantly reduced by heparinase III and wortmannin, a specific PI3K inhibitor, and that these compounds abolished the vasostatin-1-dependent phosphorylation of eNOS [62]. Interaction of vasostatin-1 with proteinase K resistant binding sites, likely phospholipids, and consequent enhancement of cell adhesion to solid phases has been observed in murine and human dermal fibroblasts [63]. Biochemical binding studies performed in the Langmuir apparatus showed that vasostatin-1 and peptide CgA47–66, at 5–10 nM concentrations, can engage in electrostatic and hydrophobic interactions with membrane-relevant phospholipids at physiological conditions, particularly with phosphatidylserine [27].
The first indication of a defined receptor for the full-length CgA and its N-terminal fragment vasostatin-1 stems from a recent study on wound healing in injured mice [64]. A selective binding of CgA and vasostatin-1 to integrin αvβ6 was demonstrated in the low nanomolar range. The binding region contains the RGD motif (CgA43–45) followed by an amphipathic α-helix (CgA47–63), both crucial for binding affinity and selectivity. No binding has been observed, to other RGD-dependent and -independent integrins, such as αvß3, αvß5, αvß8, α5ß1, α1ß1, α3ß1, α6ß4, α6ß7 and α9ß1, in the low nanomolar range. However, it is noteworthy that various peptides of different length containing the integrin-binding region of vasostatin-1 could recognize, in the low micromolar range, also the integrin αvß3 [64]. For example, in competitive binding assays the peptide CgA39–63 could bind αvß3 and αvß6 with a Ki of 1.7 µM and 7 nM, respectively. Thus, both integrin αvß3 and αvß6 are recognized by these peptides, although with markedly different affinities. The significance and potential physiological relevance of the interactions αvß6 and αvß3 will be discussed in the following.
The αvß6-integrin is an epithelial-specific integrin that work as a receptor for the extracellular matrix (ECM) proteins fibronectin, vitronectin, tenascin and the latency associated protein (LAP) on TGF-ß1 [65–67]. This integrin has been shown to modulate cancer cell invasion, inhibit apoptosis, regulate the expression of matrix metalloproteases (MMP) and is involved in TGF-ß1 maturation [65, 67]. Integrin αvß6 is upregulated in keratinocytes and epithelial cells during tissue repair and in cancer [67] and regulates keratinocyte physiology in wound healing [64, 68]. Interestingly, full-length CgA, but not a mutant having RGD replaced with the inactive RGE motif, could regulate keratinocyte physiology and promote wound healing in mice [64], suggesting that the RGD/integrin interaction is important for the physiological functions of CgA in wound healing. The relevance of this interaction for the homeostatic regulation of the cardiovascular system and tumor vessels remains to be investigated. Regarding αvß3, this integrin is emerging as an important player for endothelial cell biology during angiogenesis and tumor growth [69, 70]. Although its low affinity for CgA peptides (in the low micromolar range) argues against a direct role as a receptor for circulating CgA and peptides at physiological levels, it is possible that this interactions is relevant locally, i.e. at sites where CgA is produced and released in the tissue microenvironment at high concentrations, for example in neuroendocrine tumors. Furthermore, the interactions with this integrin might occur on endothelial cell membranes after interaction with high affinity binding sites (discussed above).
While the nicotinic acetylcholine receptor is a well-established mediator of the autocrine inhibitory effect of catestatin on catecholamine secretion in the sympato-adrenal system [10], receptors for this fragment on other target cells have yet to be identified. Catestatin-induced proliferation, migration and anti-apoptotic effects in endothelial cells are mediated via G protein, MAPK and Akt, and further mediated, indirectly, via induction of bFGF and bFGF-receptor signaling [15].
Characteristic membrane-penetrating properties have been assigned to both vasostatin-1 and catestatin, and pertussis toxin sensitivity is shared by a number of their responses, notably in the vascular and cardiac endothelium [14]. Pertussis toxin-sensitive, receptor-independent activation via heterotrimeric G proteins and G alpha i/o subunits have been proposed as possible mechanisms for the inhibitory effects of these two structurally different CgA peptides on vascular and cardiac elements [14].
Although further work is definitely necessary to elucidate the receptors of CgA and its fragments in cardiovascular homeostasis, the results so far accumulated undoubtedly highlights the complexity of the “chromogranin A system”, in terms of ligands and receptor mechanisms potentially involved. The complexity of this system is further highlighted by the observation that full-length CgA shows a biphasic dose–response curve in angiogenesis and cardio-regulatory assays, with a dose-dependent activity at 0.1–1 nM and paradoxical loss of activity when the concentration is increased above 5–10 nM [13, 16]. Whether the biphasic dose–response curves derive from responses to receptors with antagonistic effects is not understood and remains a challenge.
Conclusions
The full-length CgA and its major fragment vasostatin-1 have recently been shown to exert a novel role in angiogenesis when circulating at physiologically relevant, sub-nanomolar concentrations. In particular, the recent findings have demonstrated that the circulating intact CgA and vasostatin-1 can act as important anti-angiogenic factors, thereby preserving endothelial quiescence during normal situations. Moreover, the angiogenic switch, evoked by thrombin-induced C-terminal processing of CgA yielding catestatin-containing fragments, suggests a pro-angiogenic role for the processed CgA with important implications in tissue repair. A model for the functional consequences of this unique angiogenic switch is presented. As presently reviewed, these discoveries have wide implications, not only for our understanding of the contributions of systemic and locally produced CgA to cardiovascular homeostasis and tumor development, but also for treatment of a wide range of inflammatory pathologies and diseases with an angiogenesis component.
References
Banks P, Helle KB (1965) The release of protein from the stimulated adrenal medulla. Biochem J 97:40C–41C
Blaschko H, Comline RS, Schneider FH, Silver M, Smith AD (1967) Secretion of a chromaffin granule protein, chromogranin, from the adrenal gland after splanchnic stimulation. Nature 215:58–59
O’Connor DT, Bernstein KN (1984) Radioimmunoassay of chromogranin A in plasma as a measure of exocytotic sympathoadrenal activity in normal subjects and patients with pheochromocytoma. N Engl J Med 311:764–770
Iacangelo A, Affolter HU, Eiden LE, Herbert E, Grimes M (1986) Bovine chromogranin A sequence and distribution of its messenger RNA in endocrine tissues. Nature 323:82–86
Benedum UM, Baeuerle PA, Konecki DS, Frank R, Powell J, Mallet J, Huttner WB (1986) The primary structure of bovine chromogranin A: a representative of a class of acidic secretory proteins common to a variety of peptidergic cells. EMBO J 5:1495–1502
Tatemoto K, Efendic S, Mutt V, Makk G, Feistner GJ, Barchas JD (1986) Pancreastatin, a novel pancreatic peptide that inhibits insulin secretion. Nature 324:476–478
Eiden LE (1987) Is chromogranin a prohormone? Nature 325:301
Huttner WB, Benedum UM (1987) Chromogranin A and pancreastatin. Nature 325:305
Aardal S, Helle KB (1992) The vasoinhibitory activity of bovine chromogranin A fragment (vasostatin) and its independence of extracellular calcium in isolated segments of human blood vessels. Regul Pept 41:9–18
Mahata SK, O’Connor DT, Mahata M, Yoo SH, Taupenot L, Wu H, Gill BM, Parmer RJ (1997) Novel autocrine feedback control of catecholamine release. A discrete chromogranin a fragment is a noncompetitive nicotinic cholinergic antagonist. J Clin Invest 100:1623–1633
Helle KB, Corti A, Metz-Boutigue MH, Tota B (2007) The endocrine role for chromogranin A: a prohormone for peptides with regulatory properties. Cell Mol Life Sci 64:2863–2886
Corti A, Ferrero E (2012) Chromogranin A and the endothelial barrier function. Curr Med Chem 19:4051–4058
Crippa L, Bianco M, Colombo B, Gasparri AM, Ferrero E, Loh YP, Curnis F, Corti A (2013) A new chromogranin A-dependent angiogenic switch activated by thrombin. Blood 121:392–402
Helle KB (2010) The chromogranin A-derived peptides vasostatin-I and catestatin as regulatory peptides for cardiovascular functions. Cardiovasc Res 85:9–16
Theurl M, Schgoer W, Albrecht K, Jeschke J, Egger M, Beer AG, Vasiljevic D, Rong S, Wolf AM, Bahlmann FH et al (2010) The neuropeptide catestatin acts as a novel angiogenic cytokine via a basic fibroblast growth factor-dependent mechanism. Circ Res 107:1326–1335
Pasqua T, Corti A, Gentile S, Pochini L, Bianco M, Metz-Boutigue MH, Cerra MC, Tota B, Angelone T (2013) Full-length human Chromogranin-A cardioactivity: myocardial, coronary and stimulus-induced processing evidence in normotensive and hypertensive male rat hearts. Endocrinology 154(9):3353–3365
Ji L, Pei ZQ, Ma DF, Zhang J, Su JS, Gao XD, Xue WZ, Chen XP, Wang WS (2012) Prognostic value of circulating catestatin levels for in-hospital heart failure in patients with acute myocardial infarction. Zhonghua Xin Xue Guan Bing Za Zhi 40:914–919
Meng L, Wang J, Ding WH, Han P, Yang Y, Qi LT, Zhang BW (2013) Plasma catestatin level in patients with acute myocardial infarction and its correlation with ventricular remodelling. Postgrad Med J 89:193–196
O’Connor DT, Kailasam MT, Kennedy BP, Ziegler MG, Yanaihara N, Parmer RJ (2002) Early decline in the catecholamine release-inhibitory peptide catestatin in humans at genetic risk of hypertension. J Hypertens 20:1335–1345
Fournier I, Gaucher D, Chich JF, Bach C, Shooshtarizadeh P, Picaud S, Bourcier T, Speeg-Schatz C, Strub JM, Van Dorsselaer A et al (2011) Processing of chromogranins/secretogranin in patients with diabetic retinopathy. Regul Pept 167:118–124
Schneider F, Bach C, Chung H, Crippa L, Lavaux T, Bollaert PE, Wolff M, Corti A, Launoy A, Delabranche X et al (2012) Vasostatin-I, a chromogranin A-derived peptide, in non-selected critically ill patients: distribution, kinetics, and prognostic significance. Intensive Care Med 38:1514–1522
Liu L, Ding W, Zhao F, Shi L, Pang Y, Tang C (2013) Plasma levels and potential roles of catestatin in patients with coronary heart disease. Scand Cardiovasc J 47:217–224
Metz-Boutigue MH, Garcia-Sablone P, Hogue-Angeletti R, Aunis D (1993) Intracellular and extracellular processing of chromogranin A. Determination of cleavage sites. Eur J Biochem 217:247–257
Belloni D, Scabini S, Foglieni C, Veschini L, Giazzon A, Colombo B, Fulgenzi A, Helle KB, Ferrero ME, Corti A et al (2007) The vasostatin-I fragment of chromogranin A inhibits VEGF-induced endothelial cell proliferation and migration. FASEB J 21:3052–3062
Ferrero E, Scabini S, Magni E, Foglieni C, Belloni D, Colombo B, Curnis F, Villa A, Ferrero ME, Corti A (2004) Chromogranin A protects vessels against tumor necrosis factor alpha-induced vascular leakage. FASEB J 18(3):554–555
Dondossola E, Crippa L, Colombo B, Ferrero E, Corti A (2012) Chromogranin A regulates tumor self-seeding and dissemination. Cancer Res 72:449–459
Blois A, Srebro B, Mandalà M, Corti A, Helle KB, Serck-Hanssen G (2006) The chromogranin A peptide vasostatin-I inhibits gap formation and signal transduction mediated by inflammatory agents in cultured bovine pulmonary and coronary arterial endothelial cells. Regul Pept 135:78–84
Breslin JW, Pappas PJ, Cerveira JJ, Hobson RW 2nd, Duran WN (2003) VEGF increases endothelial permeability by separate signaling pathways involving ERK-1/2 and nitric oxide. Am J Physiol Heart Circ Physiol 284:H92–H100
Koss M, Pfeiffer GR 2nd, Wang Y, Thomas ST, Yerukhimovich M, Gaarde WA, Doerschuk CM, Wang Q (2006) Ezrin/radixin/moesin proteins are phosphorylated by TNF-alpha and modulate permeability increases in human pulmonary microvascular endothelial cells. J Immunol 176:1218–1227
Pieroni M, Corti A, Tota B, Curnis F, Angelone T, Colombo B, Cerra MC, Bellocci F, Crea F, Maseri A (2007) Myocardial production of chromogranin A in human heart: a new regulatory peptide of cardiac function. Eur Heart J 28:1117–1127
Ceconi C, Ferrari R, Bachetti T, Opasich C, Volterrani M, Colombo B, Parrinello G, Corti A (2002) Chromogranin A in heart failure; a novel neurohumoral factor and a predictor for mortality. Eur Heart J 23:967–974
Goetze JP, Hilsted LM, Rehfeld JF, Alehagen U (2014) Plasma chromogranin A is a marker of death in elderly patients presenting with symptoms of heart failure. Endocr Connect 3:47–56
Jansson AM, Rosjo H, Omland T, Karlsson T, Hartford M, Flyvbjerg A, Caidahl K (2009) Prognostic value of circulating chromogranin A levels in acute coronary syndromes. Eur Heart J 30:25–32
Tota B, Gentile S, Pasqua T, Bassino E, Koshimizu H, Cawley NX, Cerra MC, Loh YP, Angelone T (2012) The novel chromogranin A-derived serpinin and pyroglutaminated serpinin peptides are positive cardiac beta-adrenergic-like inotropes. FASEB J 26:2888–2898
Angelone T, Quintieri AM, Brar BK, Limchaiyawat PT, Tota B, Mahata SK, Cerra MC (2008) The antihypertensive chromogranin a peptide catestatin acts as a novel endocrine/paracrine modulator of cardiac inotropism and lusitropism. Endocrinology 149:4780–4793
Cerra MC, De Iuri L, Angelone T, Corti A, Tota B (2006) Recombinant N-terminal fragments of chromogranin-A modulate cardiac function of the Langendorff-perfused rat heart. Basic Res Cardiol 101:43–52
Loh YP, Cheng Y, Mahata SK, Corti A, Tota B (2012) Chromogranin A and derived peptides in health and disease. J Mol Neurosci 48:347–356
Corti A, Ferrari R, Ceconi C (2000) Chromogranin A and tumor necrosis factor-alpha (TNF) in chronic heart failure. Adv Exp Med Biol 482:351–359
Ben-Haim S, Gacinovic S, Israel O (2009) Cardiovascular infection and inflammation. Semin Nucl Med 39:103–114
Tatasciore A, Zimarino M, Renda G, Zurro M, Soccio M, Prontera C, Emdin M, Flacco M, Schillaci G, De Caterina R (2008) Awake blood pressure variability, inflammatory markers and target organ damage in newly diagnosed hypertension. Hypertens Res 31:2137–2146
Anaya-Prado R, Toledo-Pereyra LH (2002) The molecular events underlying ischemia/reperfusion injury. Transplant Proc 34:2518–2519
Rodriguez-Sinovas A, Abdallah Y, Piper HM, Garcia-Dorado D (2007) Reperfusion injury as a therapeutic challenge in patients with acute myocardial infarction. Heart Fail Rev 12:207–216
Cappello S, Angelone T, Tota B, Pagliaro P, Penna C, Rastaldo R, Corti A, Losano G, Cerra MC (2007) Human recombinant chromogranin A-derived vasostatin-1 mimics preconditioning via an adenosine/nitric oxide signaling mechanism. Am J Physiol Heart Circul Physiol 293:H719–H727
Penna C, Tullio F, Perrelli MG, Mancardi D, Pagliaro P (2012) Cardioprotection against ischemia/reperfusion injury and chromogranin A-derived peptides. Curr Med Chem 19:4074–4085
Cappello S, Angelone T, Tota B, Pagliaro P, Penna C, Rastaldo R, Corti A, Losano G, Cerra MC (2007) Human recombinant chromogranin A-derived vasostatin-1 mimics preconditioning via an adenosine/nitric oxide signaling mechanism. Am J Physiol Heart Circ Physiol 293:H719–H727
Penna C, Alloatti G, Gallo MP, Cerra MC, Levi R, Tullio F, Bassino E, Dolgetta S, Mahata SK, Tota B et al (2010) Catestatin improves post-ischemic left ventricular function and decreases ischemia/reperfusion injury in heart. Cell Mol Neurobiol 30:1171–1179
Brar BK, Helgeland E, Mahata SK, Zhang K, O’Connor DT, Helle KB, Jonassen AK (2010) Human catestatin peptides differentially regulate infarct size in the ischemic-reperfused rat heart. Regul Pept 165:63–70
Glattard E, Angelone T, Strub JM, Corti A, Aunis D, Tota B, Metz-Boutigue MH, Goumon Y (2006) Characterization of natural vasostatin-containing peptides in rat heart. FEBS J 273:3311–3321
Biswas N, Curello E, O’Connor DT, Mahata SK (2010) Chromogranin/secretogranin proteins in murine heart: myocardial production of chromogranin A fragment catestatin (Chga(364–384)). Cell Tissue Res 342:353–361
Foster W, Carruthers D, Lip GY, Blann AD (2009) Relationships between endothelial, inflammatory and angiogenesis markers in rheumatoid arthritis: implications for cardiovascular pathophysiology. Thromb Res 123:659–664
Capellino S, Lowin T, Angele P, Falk W, Grifka J, Straub RH (2008) Increased chromogranin A levels indicate sympathetic hyperactivity in patients with rheumatoid arthritis and systemic lupus erythematosus. J Rheumatol 35:91–99
Di Comite G, Rossi CM, Marinosci A, Lolmede K, Baldissera E, Aiello P, Mueller RB, Herrmann M, Voll RE, Rovere-Querini P et al (2009) Circulating chromogranin A reveals extra-articular involvement in patients with rheumatoid arthritis and curbs TNF-alpha-elicited endothelial activation. J Leukoc Biol 85:81–87
Portela-Gomes GM, Grimelius L, Wilander E, Stridsberg M (2010) Granins and granin-related peptides in neuroendocrine tumours. Regul Pept 165:12–20
Taupenot L, Harper KL, O’Connor DT (2003) The chromogranin-secretogranin family. N Engl J Med 348:1134–1149
Guerin M, Guillemot J, Thouennon E, Pierre A, El-Yamani FZ, Montero-Hadjadje M, Dubessy C, Magoul R, Lihrmann I, Anouar Y et al (2010) Granins and their derived peptides in normal and tumoral chromaffin tissue: implications for the diagnosis and prognosis of pheochromocytoma. Regul Pept 165:21–29
Corti A (2010) Chromogranin A and the tumor microenvironment. Cell Mol Neurobiol 30:1163–1170
Stridsberg M, Eriksson B, Oberg K, Janson ET (2003) A comparison between three commercial kits for chromogranin A measurements. J Endocrinol 177:337–341
Colombo B, Curnis F, Foglieni C, Monno A, Arrigoni G, Corti A (2002) Chromogranin a expression in neoplastic cells affects tumor growth and morphogenesis in mouse models. Cancer Res 62:941–946
Mandala M, Stridsberg M, Helle KB, Serck-Hanssen G (2000) Endothelial handling of chromogranin A. Adv Exp Med Biol 482:167–178
Angeletti RH, Aardal S, Serck-Hanssen G, Gee P, Helle KB (1994) Vasoinhibitory activity of synthetic peptides from the amino terminus of chromogranin A. Acta Physiol Scand 152:11–19
Russell J, Gee P, Liu SM, Angeletti RH (1994) Inhibition of parathyroid hormone secretion by amino-terminal chromogranin peptides. Endocrinology 135:337–342
Ramella R, Boero O, Alloatti G, Angelone T, Levi R, Gallo MP (2010) Vasostatin 1 activates eNOS in endothelial cells through a proteoglycan-dependent mechanism. J Cell Biochem 110:70–79
Dondossola E, Gasparri A, Bachi A, Longhi R, Metz-Boutigue MH, Tota B, Helle KB, Curnis F, Corti A (2010) Role of vasostatin-1 C-terminal region in fibroblast cell adhesion. Cell Mol Life Sci 67:2107–2118
Curnis F, Gasparri A, Longhi R, Colombo B, D’Alessio S, Pastorino F, Ponzoni M, Corti A (2012) Chromogranin A binds to αvβ6-integrin and promotes wound healing in mice. Cell Mol Life Sci 69:2791–2803
Thomas GJ, Nystrom ML, Marshall JF (2006) Alphavbeta6 integrin in wound healing and cancer of the oral cavity. J Oral Pathol Med 35:1–10
Busk M, Pytela R, Sheppard D (1992) Characterization of the integrin alpha v beta 6 as a fibronectin-binding protein. J Biol Chem 267:5790–5796
Bandyopadhyay A, Raghavan S (2009) Defining the role of integrin alphavbeta6 in cancer. Curr Drug Targets 10:645–652
Koivisto L, Larjava K, Hakkinen L, Uitto VJ, Heino J, Larjava H (1999) Different integrins mediate cell spreading, haptotaxis and lateral migration of HaCaT keratinocytes on fibronectin. Cell Adhes Commun 7:245–257
Avraamides CJ, Garmy-Susini B, Varner JA (2008) Integrins in angiogenesis and lymphangiogenesis. Nat Rev Cancer 8:604–617
Desgrosellier JS, Cheresh DA (2010) Integrins in cancer: biological implications and therapeutic opportunities. Nat Rev Cancer 10:9–22
Acknowledgments
This work was supported by Associazione Italiana per la Ricerca sul Cancro (AIRC 14338 and 9965) of Italy.
Conflict of interest
The authors have no conflicts of interest that are directly relevant to the content of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Helle, K.B., Corti, A. Chromogranin A: a paradoxical player in angiogenesis and vascular biology. Cell. Mol. Life Sci. 72, 339–348 (2015). https://doi.org/10.1007/s00018-014-1750-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00018-014-1750-9