Abstract
The Hippo pathway was originally identified as the signaling that controls organ size in Drosophila, with the core architecture conserved in mammals. In the mammalian Hippo pathway, mammalian Ste20-like kinases (MST1/2) and large tumor suppressor kinases (LATS1/2) regulate transcriptional co-activators, Yes-associated protein (YAP1) and Transcriptional co-activator with a PDZ-binding motif (TAZ). The Hippo pathway was initially thought to be quite straightforward; however, the identification of additional components has revealed its inherent complexity. Regulation of YAP1 and TAZ is not always dependent on MST1/2 and LATS1/2. MST1/2 and LATS1/2 play various YAP1/TAZ-independent roles, while YAP1 and TAZ cross-talk with other signaling pathways. In this review we focus on YAP1 and TAZ and discuss their regulation, function, and the consequences of their dysregulation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction: a short history of the Hippo pathway
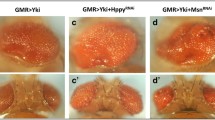
Mosaic genetic screens in Drosophila melanogaster identified Warts (wts) gene about 20 years ago. This gene encodes a tumor suppressor that is a kinase of the nuclear Dbf-2-related kinase family [1, 2]. Cells with wts mutations exhibit tumor phenotypes, as they over-proliferate and are defective with respect to apoptosis. Further screens revealed that the deletion of three genes, Hippo (hpo), Salvador (sav), and Mats (mats), result in similar phenotypes [3–9]. The HPO protein is a Ste20-like serine/threonine kinase that phosphorylates and activates WTS. The protein products of sav and mats interact with HPO and WTS to facilitate WTS activation. Therefore, these four gene products form a kinase cassette that restricts cell growth and proliferation and determines organ size. The downstream target, Yorkie (yki), was found as a WTS-interacting protein [10]. The product of yki is a transcriptional co-activator that is phosphorylated and negatively regulated by WTS. Analysis via genetic epistasis verified yki to be downstream of sav, wts, and hpo. Initially this pathway was referred to as the warts pathway, or the Salvador-Warts-Hippo pathway, but is now referred to as the Hippo pathway.
The components of the Hippo pathway that were first identified are conserved in mammals. Mice that lack the mammalian homolog of wts develop soft tissue sarcoma and ovarian tumors [11]. The human ortholog of sav (WW45) is mutated in colon and renal cancer cell lines [8]. Mutations in mats homologs have been identified in human melanomas and mouse mammary gland carcinomas [9]. Merlin (also called neurofibromatosis 2) is the etiological gene of a familial cancer syndrome and its Drosophila homolog was shown to be an upstream regulator of the Hippo pathway [12]. All these findings indicate that the pathway plays an important tumor suppression role in mammals.
Upon activation of the Hippo pathway, mammalian Ste20-like kinases (MST1 and MST2, HPO homologs) phosphorylate and activate large tumor suppressor kinases (LATS1 and LATS2, WTS homologs). These in turn phosphorylate Yes-associated protein (YAP1) and transcriptional co-activator with PDZ-binding motif (TAZ, also known as WWTR1) [13, 14]. YAP1 and TAZ are considered YKI homologs, and when phosphorylated, are segregated in the cytoplasm and undergo protein degradation. Originally, the pathway was thought to be relatively straightforward.
Later studies revealed numerous additional components that control YAP1 and TAZ. Researchers found that YAP1 and TAZ are regulated independently of MST or LATS kinases. The pathway was named after HPO. However, researchers are currently studying the Hippo pathway independent of HPO. In this review we have focused on YAP1 and TAZ and discussed MST and LATS kinases with respect to YAP1 and TAZ. MST and LATS kinases regulate molecules other than YAP1 and TAZ and play other Hippo pathway-independent roles. Detailed information regarding MST and LATS kinases can be found in other reviews [15, 16].
Molecular structures of YAP1 and TAZ
The N-terminal regions of YAP1 and TAZ interact with TEAD family transcriptional factors [13, 14] (Fig. 1). YAP1 and TAZ contain one or two WW domains in their middle region and a transactivation domain at the C-terminus. They also share a coiled-coil domain and PDZ-binding motif. There are eight isoforms of human YAP1 that are classified into two main groups: YAP1-1 (α, β, γ, and δ) and YAP1-2 (α, β, γ, and δ) [17]. YAP1-1 proteins contain one WW domain, while YAP1-2 members have two WW domains. In this review the amino acid residues we refer to correspond with those of human YAP1-2γ and human TAZ. Three variants of human TAZ are registered in GenBank, yet all of them encode the same protein. Medaka has TAZ isoform with two WW domains; however, human TAZ harbors only a single WW domain [18]. YAP1 has a proline-rich domain at the extreme end of the N-terminus (aa 1–57) and an SH3-binding motif after the second WW domain. YAP1 interacts with heterogeneous nuclear ribonuclear protein U (hnRNP U) via the N-terminal region and with Yes tyrosine kinase via the SH3-binding motif [13, 19]. As TAZ does not have the N-terminal proline-rich domain and the SH3-binding motif, it is unlikely for TAZ to interact with these proteins.
Molecular structure of YAP1. In this review, amino acid residues for human YAP1-2γ are used. The TEAD-binding domain has three interfaces for interaction with TEAD (aa 52–58, β-strand; aa 61–73, α-helix; and aa 74–84, Ω-loop). Stars indicate the five LATS-dependent phosphorylation sites. S127 could also be phosphorylated by Akt. S127 phosphorylation generates the 14-3-3-binding site. Residue S381 phosphorylation primes the phosphorylation of S400 and S403 and leads to protein degradation by the SCFβ-TrCP pathway. Residue Y407 phosphorylation by c-Abl promotes p73-dependent pro-apoptotic transcription
YAP1 and TAZ modifications
Phosphorylation by LATS kinases and subsequent ubiquitination are the most important and well-characterized negative regulatory mechanisms of YAP1 and TAZ. YAP1 up-regulates pro-apoptotic transcription under certain conditions. The phosphorylation of YAP1 by c-Abl and c-Jun N-terminal kinase (JNK) is related to pro-apoptotic properties. The significance of acetylation, methylation, and sumoylation upon YAP1 is not yet fully understood.
Phosphorylations and ubiquitination
YAP1 and TAZ have five and four HXRXXS sequences (H, histidine; R, arginine; S, serine; and X, any amino acid), respectively, that are phosphorylated by LATS kinases. Residues S127 of YAP1 and S89 of TAZ are the most important [10, 14, 20, 21]. Phosphorylation at these sites generates 14-3-3-binding sites (RXXXpSXP and RSXpSXP) (pS, phospho-serine; P, proline) and causes segregation of YAP1 and TAZ in the cytoplasm. When LATS kinases phosphorylate S397 of YAP1 and S311 of TAZ, casein kinase 1ε/δ subsequently phosphorylates S400 and S403 of YAP1 and S314 of TAZ. This then leads ubiquitination of YAP1 and TAZ, and their degradation via an SCF β-TrCP pathway [22, 23]. Phosphorylation of TAZ at S66 by LATS kinases induces phosphorylation by GSK3β at S58 and S62, providing the additional phosphodegron [24].
Many kinases are reported to phosphorylate YAP1 and TAZ, including Yes, Src, Akt, c-Abl, JNK, p38, CDK1, and Nima-related protein kinase 1 (Nek1). As its name indicates, YAP1 interacts with the Yes protein [13]. In embryonal stem (ES) cells, leukemia inhibitor factor (LIF) induces tyrosine phosphorylation of YAP1 through Yes and enhances YAP1-TEAD2-dependent transcription [25]. Yes-mediated phosphorylation induces formation of a YAP1-β-catenin-T-box5 (TBX5) complex on the promoters of anti-apoptotic genes and is involved in the survival of β-catenin-active cell lines [26]. Phosphorylation by Src kinase regulates the repression of Runx2 by YAP1 [27]. Residue S127 of YAP1 does not conform to the consensus sequence for Akt phosphorylation but is referred to as an atypical phosphorylation site [21]. Phosphorylation by Akt also results in YAP1 being trapped by cytoplasmic 14-3-3 and YAP1-regulated transcription being switched off. Akt is a pro-survival kinase; YAP1 that is negatively regulated by Akt is thought to up-regulate transcription of pro-apoptotic genes. It is not entirely clear how YAP1 decides to up-regulate transcription of pro- or anti-apoptotic genes; however, c-Abl and JNK are implicated. In response to DNA damage, c-Abl phosphorylates YAP1 at Y407 [28]. Tyrosine phosphorylation enhances the affinity of the interaction between YAP1 and p73, prevents Itch-mediated ubiquitination of p73, and activates pro-apoptotic transcription [29–31]. JNK phosphorylates T119, S138, T154, S317, and T362 in vitro [32, 33]. In skin cancer BWT cells, ultraviolet radiation induces JNK-dependent phosphorylation of YAP1 and promotes apoptosis. In contrast, in HaCaT cells, JNK-phosphorylated YAP1 interacts with ∆Np63α, stabilizes ∆Np63α by blocking the binding of Itch, and protects cells from p73-dependent apoptosis. CDK1 phosphorylates T119, S289, and S367 when the cell cycle is arrested at G2/M phase [34]. Expression of a phospho-mimetic mutant at these three sites causes mitotic defects. Residues T119 and S289 are phosphorylated during normal mitosis. These findings suggest that CDK1 regulates the cell cycle through phosphorylation of YAP1. Nek1 phosphorylates TAZ at S314 to form phosphodegron. Nek1-dependent phosphorylation of TAZ also triggers degradation of polycystin 2 and is required to suppress the expression of polycystin 2 [35]. ATM triggers the activation of YAP1-Promyelocytic leukemia protein (PML)-p53. YAP1 and ATM are co-immunoprecipitated and YAP1 is phosphorylated in this complex; however, it remains unknown whether YAP1 is a direct substrate of ATM [36].
Protein phosphatases, PP1A and PP2A, counteract LATS kinases; PP1A dephosphorylates TAZ at S89 and S311, and YAP1 at S127 [37, 38]. PP2A dephosphorylates YAP1 at S127 [38]. It has been found that α-catenin blocks the interaction of YAP1 with PP2A and functions as a negative regulator of YAP1 [39]. Non-receptor protein tyrosine phosphatase 14 (PTPN14) binds to the WW domains of YAP1 and dephosphorylates src-induced tyrosine phosphorylation [40–42]. PTPN14 increases cytoplasmic phosphorylated YAP1 during contact inhibition. This negative regulation depends on physical interaction with YAP1 and does not require the phosphatase activity of PTPN14.
Other modifications
Methyl methanesulfonate-induced DNA damage causes acetylation of K494 and K497 of YAP1 [43]. The acetylation does not affect the nuclear localization of YAP1 but its deletion enhances TEAD-reporter activity in HEK293 cells and methyl methanesulfonate-induced cell death in HeLa cells. Residue K494 is methylated by SET-domain-containing lysine methyltransferase (SET7) [44]. This methylation is necessary for the cytoplasmic retention of YAP1. YAP1 is modified by sumoylation [45]; in CDDP-treated H1299 cells, PML stabilizes YAP1 by blocking ubiquitylation and inducing sumoylation.
YAP1 and TAZ regulators
We have summarized the upstream regulators of YAP1 and TAZ. Some of these work through MST1/2 or LATS1/2, while others directly regulate YAP1 and TAZ. The former mode of regulation is referred to as the canonical Hippo pathway (Table 1).
Cell adhesion molecules
In Drosophila protocadherin FAT and Dachsous are upstream of the Hippo pathway. Fat4 is a homolog of FAT, and mutations in Fat4 or DCHS1 (human homolog of Dachsous) cause Van Maldergem syndrome [46]. Reduction in Fat4 or DCHS1 in mouse embryonic neuroepithelial cells increases the number of progenitor cells and decreases the rate of differentiation into neurons. YAP1 suppression recovers this phenotype. In kidney progenitor cells of Fat4−/− mice, nuclear and dephosphorylated YAP1 levels are increased [47]. These findings support that Fat4 and DCHS1 negatively regulate YAP1. Fat4−/− mice develop polycystic kidneys, as do TAZ−/− mice [48–50]. This coincidence is intriguing but paradoxical and needs to be further studied, because Fat4 depletion should impair the Hippo pathway and activate TAZ. CD44, a hyaluronan receptor and cancer stem cell marker, blocks phosphorylation of YAP1 in response to H2O2 treatment in human glioblastoma U87MG cells [51]. In contrast CD44 depletion increases nuclear YAP1 levels in endothelial cells [52]. This discrepancy may be due to the different isoforms of CD44 expressed in U87MG and endothelial cells.
Receptors
Dobutamine induces the recruitment of YAP1 into the cytoplasm of U2OS cells via β-adrenergic receptors [53]. Protease-activated receptor (PAR) 1-activating peptide decreases phosphorylation of YAP1 and TAZ and increases the occurrence of nuclear localization [54]. Lysophosphatidic acid (LPA) and Sphigosine-1-P also trigger YAP1 and TAZ dephosphorylation [55, 56]. Experiments using various G-protein-coupled receptors (GPCRs) revealed that Gs signaling increases YAP1 and TAZ phosphorylation, whereas G12/13, Gq/11, and Gi/o signaling decreases phosphorylation [55]. Cyclic AMP (cAMP) generated by Gs activation stimulates LATS1 via protein kinase A (PKA) in breast cancer cells [57]. PKA does not enhance LATS1 activity in vitro, suggesting that PKA does not directly phosphorylate LATS1 (Fig. 2; Table 2). As the dominant active Rho blocks the effect of cAMP, and PKA represses the phosphorylation of ROCK kinase substrate, cAMP and PKA presumably activate LATS1 through suppression of Rho signaling. Kim et al. studied the effects of cAMP generated by cell detachment [58]; in this scenario, the production of cAMP was independent of Gs. They identified putative PKA phosphorylation sites of LATS2 (S172, S380, S592, and S598) and demonstrated that PKA directly activates LATS2. Among four putative phosphorylation sites, the sequences around S172 and S380 contain the optimal consensus sequence. These sites are not conserved in LATS1. This could possibly explain why PKA does not directly activate LATS1. Regulation by G12/13 signaling is also mediated by Rho and the actin cytoskeleton. Gq/11 mutants detected in human uveal melanoma activate YAP1 via Rho [59, 60]. LIF enriches Scribble at the plasma membrane and activates LATS kinases [61]. Down-regulation of the p130 LIF receptor results in up-regulation of YAP1, and is a prognostic marker of breast cancer metastasis.
Summary of YAP1 and TAZ regulation. The core kinase cassette, comprising MST1/2, WW45, MOB1, and LATS1/2, negatively regulates YAP1 and TAZ by phosphorylation. In the nucleus YAP1 and TAZ interact with various transcription factors. TEAD interacts with Vgll. YAP1 and TAZ are regulated by “Membrane-associated proteins and cell junction proteins”, “Cell adhesion molecules and receptors”, “Actin cytoskeleton” and “Cross-talk with other signaling pathways”. The components are summarized in Table 2. LKB1 alters the localization of Scribble. ILK inactivates Merlin. TAO-1, SIK, and RASSF regulate MST1/2 activities. NPHP4, NPHP9, and ASPP1 directly interact with TAZ or YAP1. HIPK2 and ANKHD1 modulate transcription mediated by YAP1. Cytoplasmic YAP1 and TAZ interact with 14-3-3 and several other proteins. Nuclear YAP1 and TAZ interact with several proteins including PML and MED15 along with transcription factors
Membrane-associated proteins and cell junction proteins
In D. melanogaster, the molecules that determine apical-basal polarity regulate the Hippo pathway. These molecules, and their interactions, are mostly conserved in mammals and regarded as upstream regulators.
Merlin has long been known to play a role in contact inhibition [62]. It interacts with numerous proteins, and it is not clear whether its tumor suppressive role is solely dependent on YAP1. It is, however, clear that Merlin exerts some of its function through the Hippo pathway [63]. Merlin interacts with α-catenin and Par3 in keratinocytes and is involved in the maturation of adherens junctions [64]. It has been shown that α-catenin interacts with phosphorylated YAP1 via 14-3-3 and eventually sequesters YAP1 from the nucleus, implying that Merlin recruits YAP1 into the cytoplasm via α-catenin [39].
FRMD6/Willin is thought to be the ortholog of Drosophila Expanded. FRMD6/Willin expression increases phosphorylation of MST kinases, LATS1, and YAP1 in HEK293 cells. This observation supports the theory that FRMD6/Willin is partially equivalent to Expanded [65]. However, there are some differences between expanded and FRMD6/Willin. Expanded interacts with Merlin but FRMD6/Willin lacks the C-terminal Merlin-binding region, therefore FRMD6/Willin and Expanded possibly work in different ways.
KIBRA forms a complex with Merlin and Expanded and functions upstream of the Hippo pathway in Drosophila [66, 67]. In mammals, KIBRA interacts with Merlin, AMOT, and PTPN14, although the significance of these interactions has not been clarified at the molecular level. KIBRA also binds to and activates LATS kinases [68]. KIBRA depletion reduces YAP1 phosphorylation, supporting the view that KIBRA functions upstream of YAP1. Given that KIBRA is up-regulated by YAP1, there is a feedback loop between KIBRA and YAP1.
The AMOT family of proteins comprises AMOT-p80, AMOT-p130, AMOTL1, and AMOTL2 [69]. AMOT interacts with the PDZ domain of Patj, a component of Crb complex (Crb, Pals1, and Patj), via the PDZ-binding motif and is localized at tight junctions. AMOT also interacts with Merlin via the coiled-coil region and bridges Merlin and Patj [70, 71]. AMOT binds Rich1, a GTPase-activating protein for Rac1 and Cdc42. AMOT functions downstream of Merlin and upstream of Rich1 to activate Rac1 in HEK293 cells. The AMOT family of proteins, with the exception of AMOT-p80, directly bind to YAP1 and TAZ. Overexpression of AMOT recruits YAP1 and TAZ to tight junctions or the actin cytoskeleton and reduces nuclear levels of YAP1 and TAZ [72, 73]. The interaction of AMOT with YAP1 and TAZ does not depend on the phosphorylation of YAP1 and TAZ, but does increase their phosphorylation levels. The AMOT family of proteins bypass LATS1/2, and negatively regulate YAP1 and TAZ. Yi et al. [74] reported that AMOT is necessary for tumorigenesis in Merlin−/− mice. They showed that AMOT-p130 inhibits the interaction betweenYAP1 and LATS1/2 and increases nuclear YAP1 in HEK293 cells. Their results are inconsistent with those reported by others; they argued that in previous studies, researchers used cells that do not endogenously express AMOT-p130 and, therefore, might obtain artificial observations.
Ajuba LIM proteins [Ajuba, LIM domain-containing 1 (LIMD1) and Wilms tumor protein 1-interacting protein (WTIP)] interact with LATS 1/2. Ajuba and WTIP bind to WW45 [75]. LIMD1 reduces YAP1 phosphorylation, while combined knockdown of Ajuba and LIMD1 increases YAP1 phosphorylation in MDCK cells. MAPK signals enhance the interaction between WTIP, LATS1, and WW45 [76]. JNK phosphorylates LIMD1 and WTIP and augments their interaction with LATS1, but not with WW45 [77]. YAP1 is regulated by a mechanical cue; a cyclic stretch increases the binding of LIMD1 to LATS1 via JNK and activates YAP1 [78]. Ajuba is down-regulated in human mesothelioma cells that are associated with YAP1 activation [79]. Ajuba expression consistently enhances YAP1 phosphorylation in mesothelioma cells, suggesting a tumor suppressive role of Ajuba.
ZO-2 is a tight junction protein with PDZ domains that interacts with TAZ and YAP1 [80, 81]. ZO-2 facilitates the nuclear localization of YAP1 and promotes apoptosis in HEK293 cells. ZO-2 co-localizes with TAZ in the nucleus and represses TAZ transactivation.
Actin cytoskeleton
G-protein-coupled receptor signaling activates and inhibits YAP1 via the actin cytoskeleton. Other stimuli that influence the actin cytoskeleton similarly modulate YAP1 and TAZ activities, with Rho involved in most cases. Soft matrix inhibits YAP1 and TAZ, while stiff matrix or cell spreading increases nuclear YAP1 and TAZ through the activation of Rho [82]. The importance of Rho is highlighted by a report showing that inhibition of geranylgeranyl pyrophosphate synthesis impairs the modification of Rho and reduces YAP1 and TAZ nuclear localization [83]. CDC42 inactivation shows a similar phenotype to a YAP1 depletion phenotype in nephrogenesis, supporting that CDC42, a regulator of the actin cytoskeleton, regulates YAP1 [84]. High mechanical stress, such as stretching, activates YAP1 and TAZ. In contrast, under low mechanical stress, YAP1 and TAZ are inhibited by F-actin-capping/severing proteins, such as Cofilin, CapZ, and Gelsolin [85]. Regulation of YAP1 by the extracellular matrix is important in cancer biology and regenerative medicine. YAP1 is activated in cancer-associated fibroblasts and promotes matrix stiffening, which in turn further up-regulates YAP1 [86]. Aging affects the mechanosensing activities of YAP1 and TAZ. In aged mammary epithelial progenitors, YAP1 and TAZ become less sensitive to mechanical cues. Under these conditions, progenitors show biased differentiation towards a luminal-like phenotype [87]. Sun et al. [88] seeded human ES cells on soft matrix to differentiate them into motor neurons by inhibiting YAP1.
Other regulators
Kinases
All molecules that modulate the activities of MST1/2 and LATS1/2 potentially regulate YAP1 and TAZ activities. The Ste20-like kinase TAO-1 phosphorylates and activates MST2 [89, 90]. In Drosophila, salt-inducible kinases (SIK) phosphorylate Salvador and negatively regulate the Hippo pathway [91]. Human SIK2 enhances YAP1-mediated transcription, although the mechanisms involved are not clear. Liver kinase B1 (LKB1) and its substrates, microtubule affinity-regulating kinases (MARK), suppress YAP1 [92]. Knockdown of LATS2 or Scribble cancels the inhibitory effect of LKB1, showing that LKB1 acts via LATS2 and Scribble. Deficiencies in LKB1 activate YAP1 and cause trans-differentiation from adenocarcinoma to squamous cell carcinoma [93]. Integrin-linked kinase (ILK) phosphorylates myosin phosphatase MYPT1-PP1 at the inhibitory site, inactivates Merlin by increasing S518 phosphorylation, and activates YAP1 [94]. Homeodomain-interacting protein kinase (HIPK)2 increases the abundance of YAP1 in parallel with LATS1/2 and enhances TEAD2-depdendent transcription [95]. Kinase activity is necessary, but the direct substrate of HIK2 has not been identified yet.
RASSF
Drosophila dRASSF has the Ras-association (RA) domain and the Salvador/RASSF/Hippo (SARAH) domain [96]. Humans have 10 RASSF proteins (RASSF1-10) [97]; RASSF1-6 have the SARAH domain and are orthologs of dRASSF. RASSF1A activates MST2 in response to DNA damage [98, 99]. RASSF2 and RASSF5 activate the Hippo pathway as upstream regulators [98, 100–102]. In contrast, RASSF6 forms a complex with MST2 and inhibits its activity [103]. When cells are exposed to stress, RASSF6 is dissociated from MST2 and the Hippo pathway is activated. At the same time RASSF6 facilitates auto-ubiquitination of MDM2 and stabilizes p53 to induce cell cycle arrest and apoptosis [104]. The Hippo pathway and RASSF6 are simultaneously activated and accomplish tumor suppressive roles in a parallel manner. In alveolar rhabdomyosarcoma (aRMS), PAX3-FOXO enhances RASSF4 expression, which leads to MST1 inhibition and YAP1 activation [105]. This finding implies that RASSF4 is oncogenic in aRMS. We should consider the possibility that aRMS might harbor p53 mutations. If this is the case, RASSF4 cannot function as a p53-dependent tumor suppressor and apparently plays an oncogenic role. In Drosophila, PP2A negatively regulates the Hippo pathway, and dRASSF is important for HPO to interact with Drosophila Striatin-interacting phosphatase and kinase (dSTRIPAK), a Drosophila PP2A complex [106]. In mammals, RASSF1A inhibits PP2A-dependent dephosphorylation of MST1/2 and activates the Hippo pathway [107].
Cilia-related proteins
The interaction of TAZ with cilia-related proteins is interesting because TAZ−/− mice develop polycystic kidneys. Nek1 phosphorylates TAZ and is important in ciliogenesis and the regulation of polycystin 2 expression. Nephronophthisis (NPHP) is a group of autosomal recessive kidney cystic diseases with 11 causative genes (NPHP1–11). NPHP4, a cilia-associated protein, inhibits interaction between LATS1 and TAZ to activate TAZ [108]. NPHP9, also known as Nek8, directly binds to TAZ and translocates it to the nucleus [109]. Phosphorylation of TAZ by NPHP9 has not been reported, and the kinase-dead mutant of NPHP9 can activate TAZ. Therefore, the physical interaction between NPHP9 and TAZ is important.
Miscellaneous
Vigneron et al. [110] reported that cytoplasmic apoptosis-stimulating protein of p53 (ASPP1) binds to YAP1 and blocks interaction between YAP1 and LATS1. ASPP2 promotes the interaction of TAZ with PP1A to facilitate dephosphorylation of TAZ [37]. In C2C12 cells, selenoprotein WW, which might be an anti-oxidant protein, is reported to regulate the binding of TAZ and 14-3-3 [111]. In Drosophila, multiple ankyrin repeats single KH domain (Mask) functions downstream of Wts and is necessary for Yki-dependent transcription [112, 113]. The human Mask homolog (ANKHD1) forms a complex with YAP1 and is required for full YAP1 activity. ANKHD1 is highly expressed in various prostate cancer cell lines and its depletion suppresses YAP1 expression [114]. PML binds p73 and YAP1, promotes acetylation of p73 by p300, and stabilizes YAP1 by sumoylation [115]. The PML gene is up-regulated by p73/YAP1 [45]; therefore, there is a positive feedback loop between PML and p73/YAP1. WRN is a human RecQ helicase and a causative gene of Werner syndrome characterized by premature aging. In WRN-depleted cells YAP1 expression is augmented, activating p53-dependent transcription and contributing to senescence [36].
Regulation of YAP1 transcription
Our knowledge regarding regulation of YAP1 and TAZ gene expression is limited. GABP and Sox2 bind to the YAP1 promoter and activate its transcription [116]. As GABP is sensitive to the redox state, YAP1 might be a part of the defense mechanisms against oxidants. Sox2 inhibits osteogenesis via YAP1 and induces PPARγ in osteoblastic and adipocytic lineage cells [117]. Induction of adipogenesis by Sox2 is impaired by excessive YAP1 or its depletion and requires the moderate level expression of YAP1. In the developing lung YAP1 controls Sox2 expression [118]. The mutual regulation between YAP1 and Sox2 is likely to be important in determining cell fate.
YAP1 and TAZ functions
As YAP1 and TAZ are transcriptional co-activators, regulation of transcription is an essential part of their functions. However, YAP1 and TAZ also function in the cytoplasm and regulate microRNAs (miRNAs). Cross-talk with other signaling pathways, especially the Wnt pathway, is important for the regulation of stem cells and cancer.
Regulation of transcription
YAP1 and TAZ interact with various transcriptional factors that are overlapped, but are significantly divergent, mirroring the fact that YAP1 and TAZ play distinct roles during development and oncogenesis.
TEAD1–4
TEAD1–4 play important roles in development and cancer cells [119]. All four TEADs have a DNA-binding domain in the N-terminal region and immunoglobulin-like β-sandwich folds in the C-terminal region [120–122]. The C-terminal region functions as a transactivation domain and interacts with YAP1 and TAZ. This domain also binds Vestigial-like (Vgll) proteins and p160 coactivator proteins. The TEAD-interacting domain of YAP1 has a β-strand (aa 52–58), an α-helix (aa 61–73), and an Ω-loop (aa 74–84). YAP1 binds to three interfaces of TEAD1 and TEAD4, whereas Vgll1 uses only the first and second interfaces of TEAD4 [123]. The overall affinities of YAP1 and TAZ for TEAD4 are similar, with closer analysis revealing some differences between YAP1-TEAD4 and TAZ-TEAD4 interactions [124]. In Drosophila, the TEAD homolog, Scalloped (Sd), functions as a default repressor. The Vgll homolog, Tgi, is necessary for this repression [125]. YKI competes with Tgi for binding to Sd and abrogates repression; a similar competition between YAP1 and Vgll1 was shown in vitro. Vgll4 negatively regulates the YAP1-TEAD complex in lung cancer [126]. The synthetic peptide mimicking the sequence of Vgll4 interferes with the interaction of YAP1 and TEAD4 and inhibits gastric cancer growth [127]. Based on these findings we reasoned that YAP1, like YKI, activates transcription by blocking Vgll-TEAD-mediated repression.
SMAD proteins
YAP1 and TAZ interact with SMAD proteins. SMAD-mediated transcription is important in the regulation of stem and cancer cells. Not all combinations of YAP1/TAZ and SMAD1–8 have been tested for interaction. The interaction between YAP1 and SMAD1 is well characterized [128]. SMAD1 mediates bone morphogenesis protein (BMP) signals, while BMP induces the CDK8/9-mediated linker phosphorylation of SMAD1. This phosphorylation enhances the interaction between the WW domains of YAP1 and the PPXY motif in the linker region. Subsequent phosphorylation by GSK3β abrogates YAP1 binding, but overall YAP1 promotes SMAD1-mediated signals. In human mesothelioma cells, the YAP1-TEAD4-SMAD3-p300 complex was detected on the promoter of connective tissue growth factor, suggesting an interaction between YAP1 and SMAD3 [129]. Developing airway epithelial cells are unable to respond to TGFβ in the absence of YAP1 [130], suggesting that YAP1 co-operates with SMAD proteins to transduce TGFβ signaling. YAP1 interacts with SMAD7 in COS-7 cells and potentiates the inhibitory effect against TGFβ signaling [131]. The relationship of YAP1 with SMAD proteins appears to be context-dependent. TAZ interacts with the SMAD2/3–4 complex in a TGFβ-dependent manner, and is necessary for nuclear localization of the complex and TGFβ-induced transcription in human ES cells [132, 133]. TAZ binds to the MH domain of SMAD2. This interaction is not dependent upon the WW domain of TAZ. In mouse mammary epithelial cells seeded at high density, TAZ and YAP1 accumulate in the cytoplasm, with SMAD2/3 concomitantly recruited to the cytoplasm. YAP1 and TAZ regulate SMAD functions at the transcriptional level and in determining subcellular localization.
Other transcription factors
TAZ interacts with Pax3, MyoD, thyroid transcription factor-1 (TTF-1, T-EBP, Nkx2.1), Pax8, Runx2, and peroxisome proliferator-activated receptor (PPAR)γ. The interaction of TAZ with Pax3, TTF-1, or Pax8 is mediated by multiple domains [134, 135]. MyoD binds to the WW domain of TAZ [136]. Runx2 and PPARγ contain the WW domain-binding motif, but it is not known whether interaction of TAZ with Runx2 or PPARγ is dependent on the WW domain [137]. Pax8 and TTF-1 are involved in thyroid development. TAZ−/− mice do not show significant abnormalities during thyroid development. The significance of TAZ interaction with Pax8 and TTF-1 is unclear. In mesenchymal stem cells, TAZ activates Runx2 to promote osteogenesis and represses PPARγ to inhibit adipogenesis [137]. Pax3 and MyoD play important roles in skeletal muscles. In mouse C2C12 cells, TAZ enhances MyoD-mediated myogenesis, but the cellular output of the interaction between TAZ and Pax3 has not been analyzed. YAP1 interacts with Runx2 and p73; however, findings have been inconsistent regarding observed effects [27, 31]. In reporter assays using rat osteosarcoma ROS 17/2.8 and human cervical carcinoma HeLa cells, YAP1 repressed Runx2 [27]. In human bone marrow endothelial cells, YAP1 and Runx2 co-operated to promote cell transformation [138]. Interaction with p73 is required to understand the tumor suppressive properties of YAP1. PML stabilizes YAP1 and p73, and enhances YAP1/p73-mediated transcription [45, 115]. The hnRNP U protein binds to the N-terminal region of YAP1 and suppresses p73-dependent Bax transcription [19]. The interaction of YAP1 with p63 is necessary to regulate p63 target genes in airway basal stem cells [139]. To date, there is no evidence to show interaction between YAP1 and PPARγ, but it has been postulated that because YAP1 overexpression suppresses adipogenesis in 3T3-L1 cells, YAP1 might repress PPARγ [57]. Wbp2, a co-activator of the estrogen receptor (ER), binds to YAP1 and TAZ and is implicated in TAZ-dependent oncogenesis in breast cancers [140, 141]. Wbp2 enhances Scalloped-dependent reporter activity in Drosophila S2 cells to a small extent [142]. It has not been reported whether YAP1 and TAZ modulate ER-dependent transcription via Wbp2. TAZ binds to Gli-similar 3 (Glis3), a Kruppel-like zinc finger protein, and enhances Glis3-meditated transcription [143]. Glis3 is localized to primary cilia. As TAZ is modified by NPHP4 and NPHP9 and TAZ−/− mice develop polycystic kidneys, the interaction between TAZ and Glis3 is an attractive area for further studies [49, 50, 108, 109]. YAP1 forms a complex with Foxo1 on the promoter of catalase and manganese superoxide dismutase, protecting cardiomyocytes against irradiation [144]. TAZ activates hypoxia-inducible factor 1α (HIFα)-dependent transcription and confers malignant properties to cancer cells [145].
Regulation of miRNA biogenesis
Two reports have shown that the Hippo pathway regulates miRNA biogenesis, which is relevant to contact inhibition. Chaulk et al. [146] reported that nuclear YAP1 and TAZ increase inhibitory LIN28B levels and suppress Let-7 expression; this is necessary for the processing of pre-miRNA. Mori et al. demonstrated that nuclear YAP1 sequesters p72 (DEAD box helicase 17) from DROSHA and DGCR8 at a low cell density. At a high density, cytoplasmic YAP1 promotes p72 association with Microprocessor [147]. These findings suggest that dysregulation of the Hippo pathway impairs miRNA processing and shed some light on how miRNAs are globally suppressed in cancers.
Roles of cytoplasmic YAP1 and TAZ
In the canonical Hippo pathway, only nuclear YAP1 and TAZ were considered to be functional. However, it now appears that cytoplasmic YAP1 and TAZ also have specific functions. Aylon et al. [148] reported that LATS2 phosphorylates cytoplasmic ASPP1, inducing its nuclear translocation, and promoting transcription of pro-apoptotic genes. As YAP1 blocks the binding of LATS2 to ASPP1, cytoplasmic YAP1 antagonizes the tumor suppressive roles of ASPP1. YAP1, and TAZ affect the subcellular localization of SHP2 tyrosine phosphatase [149]; when YAP1 and TAZ accumulate in the nucleus, SHP2 is recruited to the nucleus and dephosphorylates parafibromin to stimulate TCF/LEF-dependent and TEAD-dependent transcriptions. This is an example of the cross-talk between the Hippo and Wnt pathways. Cytoplasmic YAP1 and TAZ also play an important role in regulating β-catenin [150].
Cross-talk with the Wnt pathway
The yes tyrosine kinase triggers the formation of a YAP1-β-catenin-TBX5 complex [26]. TAZ interacts with DVL in the cytoplasm and inhibits CK1ε/δ-mediated phosphorylation [151]. Similarly, in the intestine, YAP1 interacts with DVL and restricts its nuclear localization to compromise Wnt signaling during regeneration [152]. Imajo et al. [153] found that YAP1 and TAZ bind to β-catenin; they revealed that activation of the Hippo pathway blocks nuclear localization of β-catenin through the cytoplasmic translocation of YAP1. Whether TAZ plays a similar role is not yet clear. In YAP1-induced intestinal dysplasia, increased nuclear β-catenin levels were observed [154]. In WW45-deficient hearts, nuclear β-catenin levels were increased, and YAP1 interacted with β-catenin on Sox2 and Snai2 genes [155]. Azzolin et al. revealed that YAP1 and TAZ interact with Axin1, and recruit β-catenin to the β-TrCP degradation complex. When the Wnt pathway is switched on, YAP1 and TAZ dissociate from Axin1, and β-catenin is stabilized and translocated to the nucleus [150]. These findings suggest that YAP1 and TAZ increase nuclear β-catenin levels, and that the Hippo pathway antagonizes the Wnt pathway. Consistently in MST−/− intestinal epithelia, YAP1 and β-catenin accumulate in the nucleus [156]; however in WW45−/− mice, only YAP1 accumulates in the nucleus [157]. This discrepancy is not yet fully explained. The recent study has revealed that in the Wnt off state, cytoplasmic YAP1 and TAZ regulate β-catenin negatively, while in the Wnt on state, YAP1 and TAZ potentiate the Wnt pathway [150]. It might be possible that in WW45−/− mice, TAZ remains in the cytoplasm to facilitate degradation of β-catenin. It is necessary to detect YAP1 and TAZ with specific antibodies. In YAP1-depleted kidneys, no major changes were observed in the Wnt pathway [84]. Cross-talk between the Hippo and Wnt pathways might vary in different tissues.
Cross-talk between the Hippo and Wnt pathways is bi-directional. Phosphorylated β-catenin bridges TAZ to SCFβ-ΤrCP and promotes its degradation [158]. Canonical Wnt signaling reduces phosphorylated β-catenin, releases TAZ from SCFβ-ΤrCP and leads to a concomitant increase of β-catenin and TAZ levels. TRIB2, a pseudokinase, is a target of the Wnt pathway [159]. In liver tumors with β-catenin mutants, TRIB2 levels are increased and it interacts with β-TrCP, thereby stabilizing YAP1. TRIB2 also induces degradation of C/EBPα. As C/EBPα binds to YAP1 and inhibits the interaction between YAP1 and TEAD, TRIB2 enhances YAP1/TEAD-dependent transcription. Wnt signaling dephosphorylates TAZ via PP1A to induce osteogenesis in C3H10T1/2 cells [160]. Hence, the Wnt pathway up-regulates TAZ and YAP1 functions.
Cross-talk with other signaling pathways (Sonic hedgehog, Notch, and EGF)
The cross-talk between the Hippo and Sonic hedgehog pathway is also bi-directional. YAP1 is overexpressed in human Sonic hedgehog (Shh)-dependent medulloblastoma [161]. Shh up-regulates YAP1 expression at the mRNA and protein level and increases nuclear localization via IRS1. In mouse embryonal carcinoma P19 cells and mouse cortical progenitor cells, YAP1 overexpression blocks neuronal differentiation, while knockdown of Gli2 rescues differentiation [162]. In the intestine, YAP1 activates Notch signaling and γ-secretase inhibition prevents YAP1-induced intestinal dysplasia [154]. In hepatocellular carcinomas, YAP1 up-regulates Jagged-1 and stimulates Notch signaling in a non-cell autonomous manner [163]. Amphiregulin, a ligand of the EGF receptor, is a target of YAP1 and TAZ, and dysfunction of the Hippo pathway up-regulates EGF signals in a non-cell autonomous manner [164, 165].
Roles in cancer
In this section we briefly review disorders of the Hippo pathway observed in human cancers. Dysregulation of the Hippo pathway causes epithelial-mesenchymal transition (EMT), provides cancer cells with stemness, and enhances genomic instability. YAP1 functions as a tumor suppressor in certain cancer cells.
Abnormalities of YAP1 and TAZ in human cancers
Dysfunction of the Hippo pathway and hyperactivity of YAP1 and TAZ correlate with poor prognosis in human cancers. Mutants of YAP1 and TAZ, in which LATS-dependent phosphorylation sites have been replaced, are used experimentally, but have not been seen in human cancers. YAP1 and TAZ mutations are very rare. One missense mutation (F29V) in TAZ has been reported in a basal-like breast cancer [166]. Two mutations in YAP1 have been reported in families with autosomal-dominant inheritance of coloboma but no mutation has been detected in cancer so far [167]. Frequently observed abnormalities of the Hippo pathway include Merlin mutations, down-regulation of Hippo components (KIBRA, RASSF1A, MST2, and LATS1/2) by DNA hypermethylation, and YAP1 gene amplification. Chromosomal rearrangement that results in the fusion of TAZ and CAMTA1, a calmodulin-binding transcription activator, has been detected in epithelioid hemangioendothelioma (EHE) [168]. Fusion of YAP1 and transcription factor 3 (YAP1–TFE3) has also been detected in EHE [169].
How do YAP1 and TAZ hyperactivities lead to oncogenesis?
The WW domains of YAP1 are required for YAP1-induced overgrowth and serum-independent growth in NHI3T3 cells [170]. The WW domain of TAZ is necessary for anchorage-independent growth of MCF10A cells expressing TAZ [141]. The transcription factors interacting with the WW domains play some role in oncogenesis, with TEADs thought to be major contributors to oncogenesis [171–173]. Two studies using a K-ras-driven pancreatic cancer model yielded inconsistent results [174, 175]. Mice with K-ras G12D developed pancreatic ductal adenocarcinoma; suppression of K-ras G12D resulted in tumor regression, but then there was a relapse of K-ras-independent tumors. Both studies found that YAP1 substitutes for the K-ras G12D mutant in tumor relapse cases, but do not agree in the downstream mechanisms. Kapoor et al. compared the mRNA expression profiles between K-ras-dependent and K-ras-independent tumors and focused on TEAD2. They demonstrated that YAP1 and TEAD2 co-operate with E2F to bypass K-ras-oncogenic addiction. Shao et al. observed that the TEAD-binding-deficient YAP1 mutants can rescue proliferation in K-ras G12D-suppressed cells and concluded that AP-1 was a key factor. This discrepancy could be due to differences in experimental methods that the groups used. TEAD is also important in YAP1- and TAZ-induced EMT [172, 176]. Target genes of TEADs include the CCN family (CTGF, Cyr61), Axl, miR-29, and Sox9. CTGF and Cyr61 confer drug resistance to cancer cells [177]. Interleukin-6, metalloproteinase 7, interleukin 1-α, and cyclooxygenase 2 also correlated with YAP1 abundance in pancreatic cancer models [178]. Axl, a receptor tyrosine kinase, determines tumorigenic properties of hepatocellular carcinoma cells [179]. miR-29 suppresses PTEN and activates mTOR [180]. Sox9 provides esophageal cancer cells with stemness [181]. A glioblastoma chromatin immunoprecipitation study demonstrated that TAZ forms a complex with TEAD2 on mesenchymal gene promoters [182]. Considering the importance of TEADs in oncogenesis, YAP1 and TEAD complexes are promising therapeutic targets. Reagents such as verteporfin and Vgll4-mimicking peptide that block the interaction between YAP1 and TAZ with TEADs are tested [127, 183].
EMT is closely related to cancer stemness [184]. Breast cancer cells with mesenchymal properties show cancer stem-like properties. TAZ hyperactivity confers mesenchymal and cancer stem cell-like properties to breast cancer cells [185]. It appears that TAZ introduces molecular signatures into cancer cells that are shared by EMT and cancer stemness. Conversely EMT increases TAZ expression levels; however, when E-cadherin is overexpressed in breast cancer cells with an active TAZ mutant, EMT is reversed but cancer stem cell-like properties are maintained. This indicates that TAZ-mediated cancer stemness is independent of EMT. All these findings suggest that TAZ activation triggers EMT, subsequently activating TAZ to high levels and causing cancer stemness.
It was recently reported that LATS2 is activated in tetraploid cells and is important in arresting the cell-cycle [186]. In tetraploid cells, cytoplasmic YAP1 levels are increased, while TAZ expression is reduced. Expression of constitutively active YAP1 mutants overrides cell cycle arrest and drives tetraploid cells into the cell cycle. Tetraploid cells cannot proliferate while the Hippo pathway is functional; in cancer cells where the Hippo pathway is deficient, YAP1 and TAZ facilitate genomic instability.
YAP1 as a tumor suppressor
Although YAP1 is primarily regarded as an oncogene, it promotes apoptosis in response to DNA damage in some cancer cell lines such as H1299, HCT116, and MCF7 [21, 33]. In human breast cancers, deletion of YAP1 gene locus is observed [187]. In human head and neck squamous carcinoma cells, cytoplasmic YAP1 is abundant, reflecting high Akt activity, with overexpression of nuclear YAP1 causing cell death [188]. In multiple myeloma cells, DNA damage causes nuclear accumulation of c-Abl, but because of low YAP1 expression, these cells evade cell death [189]. If YAP1 is activated in these myeloma cells, cell proliferation is reduced and cell death is induced. YAP1 activation could be beneficial in the treatment of myeloma. Loss of YAP1 expression has also been seen in human colon cancers and is associated with high stage diseases [152]. It is essential to select appropriate cancers for cancer therapies targeting YAP1.
Roles in development and tissue regeneration
YAP1 and TAZ have attracted an increasing amount of interest from researchers in the field of regenerative medicine.
Embryogenesis
It has been shown that YAP1−/− mice die by embryonic day (E) 8.5 due to yolk sac defects [190], while TAZ−/− mice progress through to adulthood, although they suffer from emphysema-like lung defects and polycystic kidneys [49, 50]. The TEAD proteins are expressed at the very early stages of embryogenesis [191, 192]. At the blastocyst stage, blastomeres develop into the outer epithelial trophectoderm (TE) and the inner cell mass (ICM) [193, 194]. In the TE, YAP1 is localized to the nucleus and TEAD4 induces the expression of TE-specific genes such as Cdx2 and Gata3. For the ICM, YAP1 is distributed within the cytoplasm and TEAD4-dependent transcription does not occur. Components of the Hippo pathway, including Merlin, AMOT, and LATS1/2, regulate the subcellular localization of YAP1 in blastomeres [195–197].
ES cells and induced pluripotent stem (iPS) cells
YAP1 is a regulator of mouse ES and iPS cells. In murine ES cells, YAP1 is inactivated during differentiation; YAP1 and TEAD2 promote Oct3/4 and Nanog expression [25]. Depletion of YAP1 and TEAD2 reduces the self-renewal ability and induces differentiation of mouse ES cells. The differentiation of human ES cells into motor neurons is facilitated by the suppression of YAP1 [88]. Overexpression of YAP1 enhances the efficiency of mouse iPS induction [198]. TAZ knockdown has no effect on mouse ES cells [132], but in human ES and iPS cells, TAZ is required. LATS2 knockdown increases the efficiency of reprogramming in human iPS cells, but additional TAZ knockdown counteracts LATS2 knockdown, indicating that TAZ improves efficiency [200]. TAZ controls the shuttling of SMAD2/3–4 between the nucleus and cytoplasm and enhances self-renewal in human ES cells [132]. Proteomic and genomic studies using human ES cells revealed that YAP1 and TAZ form a complex comprising SMAD2/3 and Oct4 and that they repress mesendoderm genes via a nucleosome remodeling and deacetylase (NuRD) complex, and maintain pluripotency [199]. Treatment with activin results in TEAD4 dissociating from the complex, and consequently SMAD2/3 and FOXH1 induce mesendoderm genes. A recent model has shown that the NuRD complex acts as a balance between self-renewal and differentiation [201]. YAP1 promotes self-renewal and blocks differentiation in neural stem cells and myoblasts, whereas TAZ accelerates differentiation in mesenchymal stem cells and in myoblasts. The different properties of YAP1 and TAZ might reflect differing interactions with the NuRD complex.
Roles in adult tissues
YAP1 and TAZ regulate tissue-specific stem cells and are important for tissue homeostasis and regeneration in adult animals. YAP1 is crucial in the liver, intestine, heart, skin, pancreas, lung, and brain. TAZ is involved in the regulation of osteogenesis and adipogenesis in mouse mesenchymal stem cells. YAP1 and TAZ control myogenesis in myoblasts. TAZ plays some role in the heart, but this has not been as widely studied as the role of YAP1 [202]. YAP1−/− mice and TAZ−/− mice show defects in kidney organogenesis [49, 50, 84], but it remains unknown what roles YAP1 and TAZ play in the adult kidney. TAZ−/− mice show emphysema-like changes in the lungs [49], but the role of TAZ in adult lungs is not clear. The size of the pancreas is small in MST1/2 knockout mice because disorganization of the exocrine compartment causes secondary pancreatitis [203, 204]. This observation suggests that proper inactivation of YAP1 is important for development of the pancreas, but the role of YAP1 in the adult pancreas is unknown.
Liver
Various model mice with either liver-specific mutant YAP1 expression or liver-specific ablations of Hippo pathway components (Merlin, WW45, and MST1/2) have been analyzed [63, 154, 205–208]. Although there are differences between models, all animals show proliferation of liver stem cells, known as oval cells, and hepatomegaly, thus supporting the notion that the Hippo pathway controls organ size. In human patients with chronic cholestasis, nuclear YAP1 is prominent in bile duct compartments and induces biliary epithelial cell proliferation [209]. After a hepatectomy, MST1/2, LATS1/2, and MOB1 levels are decreased and YAP1 becomes active during regeneration [210]. It was recently shown that YAP1 activation leads hepatocytes to a ductal fate [211]. YAP1 overexpression induces dedifferentiation of adult hepatocytes into progenitor-like cells. Furthermore, the suppression of YAP1 in hepatocyte-derived progenitor-like cells induces re-differentiation into hepatocytes. These findings imply that during liver damage YAP1 triggers reprogramming of hepatocytes for regeneration.
Intestine
YAP1 hyperactivation expands intestinal progenitors, while YAP1 deletion impairs regeneration in intestines damaged with dextran sodium acetate [154, 157]. There was another report showing that YAP1 antagonizes Wnt signaling and restricts intestinal stem cell expansion [152]. This discrepancy reminds us of the inconsistent nuclear β-catenin localization in WW45−/− (decreased) and MST−/− (increased) intestinal epithelia [155, 156].
Heart
WW45, MST1/2, or LATS1/2 deficiencies and overexpression of YAP1 result in heart overgrowth [212–214]. In a myocardial infarction model, YAP1 promotes regeneration and improves survival [202, 215]. YAP1 stimulates cardiomyocyte proliferation but not hypertrophy. Cardiomyocyte-specific YAP1 depletion increases apoptosis and fibrosis, leading to dilated cardiomyopathy [155]. In the heart, β-catenin forms a complex with unphosphorylated YAP1 in the nucleus. YAP1 and β-catenin concurrently occupy the promoter of Sox2 and Snai2. YAP1 inhibits GSK3β via the insulin-growth factor pathway and activates β-catenin to proliferate cardiomyocytes [216]. YAP1 co-operates with the Wnt pathway in the heart. In arrhythmogenic cardiomyopathy with mutation in intercalated disc proteins, Merlin was activated. As a consequence of this, YAP1 and β-catenin were suppressed and adipogenesis was enhanced [217]. The requirement of YAP1 for heart homeostasis raises concerns about the potential cardiotoxicity of YAP1-targeted cancer drugs.
Skin
During skin development, YAP1 is expressed in the single-layered epithelium, and then in the bulge of the hair follicle, and in the interfollicular epidermis [218, 219]. Nuclear YAP1 is evident in undifferentiated skin progenitors [39]. YAP1 shifts to the cytoplasm as differentiation occurs, and its overexpression results in the expansion of epidermal stem cells and progenitor cells. These findings are consistent with the view that YAP1 blocks differentiation and is important in maintaining self-renewal. Knockdown of YAP1 and TAZ delays skin wound healing [220]. Activation of YAP1 and TAZ could be beneficial for treating skin injuries.
Lung
In the developing lung, YAP1 is located in the nucleus of distal bud progenitors and in the cytoplasm of airway epithelial progenitors [118]. YAP1 regulates Sox2 expression, with Sox2 controlling the differentiation of airway epithelial cells. YAP1 depletion expands aberrant distal progenitors. YAP1 is further necessary for the differentiation of adult airway progenitors. Parallel work has also demonstrated that YAP1 is indispensable for the maintenance of adult airway basal stem cells [139]. Overexpression of YAP1 causes dedifferentiation of secretory cells, which echoes the dedifferentiation of hepatocytes by YAP1.
Brain and nerve tissues
Our knowledge of the roles of YAP1 in mammalian brain is still limited. However, there was a report that increased YAP1 activity was associated with the expansion of neural progenitors in chickens [221]; therefore, YAP1 is thought to be important for the maintenance of neural progenitors. The expansion of neural progenitors has been observed in Fat4−/− mice and in Merlin−/− mice [46, 222]. Suppression of YAP1 in human ES cells facilitates differentiation into motor neurons, which mirrors the inhibitory effect of YAP1 on differentiation [88]. Expression of YAP1 and TAZ is enhanced in the spinal cord after peripheral nerve injury [223]. Researchers have discussed the potential implication of YAP1 and TAZ in neuropathic pain; however, the physiological significance needs to be further investigated.
Mesenchymal stem cells
TAZ promotes osteogenesis and inhibits adipogenesis in mouse mesenchymal stem cells [137]. Kaempferol, a flavonoid, enhances the interaction of TAZ with Runx2 and PPARγ to promote osteogenesis and inhibit adipogenesis [224]. LATS2 overexpression in 3T3-L1 cells induces the recruitment of TAZ to the cytoplasm. Eventually PPARγ regains the activity and the Wnt pathway is suppressed, such that cell proliferation is repressed and adipogenesis is enhanced [225]. Kaempferol and another TAZ activator, TM-25659, are expected to play protective roles against osteoporosis and obesity [224, 226]. Sox2 overexpression in mesenchymal stem cells and C3H10T1/2 cells induces YAP1 expression, with YAP1 inhibiting osteogenesis and adipogenesis [117]. YAP1 overexpression in 3T3-L1 cells also inhibits adipogenesis [198]. As the Hippo pathway is activated by cAMP, serum glucose level should alter YAP1 and TAZ activities. It would be interesting to study whether and how YAP1 and TAZ are involved in the regulation of adipogenesis.
Skeletal muscles
TEADs take part in the regulation of myogenesis. TEAD1 and TEAD4 bind to the Myf5 promoter and regulate its expression [227]. TEAD4 also regulates myogenin expression [228]. As TEAD2 regulates Pax3 in the neural crest, TEAD2 might also regulate Pax3 in skeletal muscles [229]. As YAP1 and TAZ interact with TEADs, it is postulated that they are involved in myogenesis. YAP1 is recruited from the nucleus to the cytoplasm during differentiation in C2C12 cells [230]. When YAP1 activity is augmented in C2C12 cells, the expressions of Myf5 and cyclinD1 remain high, but those of myogenin and Mef2c are low; therefore, myogenesis is inhibited. In Pax7-positive quiescent satellite cells, YAP1 expression is low, while it is high in MyoD-positive active satellite cells and Pax7-positive self-renewal reentering cells [231]. Consistently, YAP1 hyperactivity enhances satellite cell proliferation, increases the number of Pax7-positive MyoD-positive active satellite cells, and inhibits myogenesis from skeletal muscle progenitors. In a mouse model, skeletal muscle fiber-specific expression of an active YAP1 mutant causes muscle degeneration [232]. Lamin A/C gene mutations cause congenital muscle dystrophy. Myoblasts with such mutations are defective in mechanosensing and YAP1 is hyperactive in these cells [233]. All these findings suggest that the moderate and timely activation of YAP1 is important for homeostasis of skeletal muscles. TAZ interacts with Pax3 and MyoD [134, 136]. The precise roles of TAZ in satellite cells are not fully known but its expression is increased in regenerating muscles after injury [136]. In C2C12 cells, TAZ enhances MyoD-mediated myogenesis. TAZ activators promote muscle repair after injury [234, 235]. Unlike YAP1, TAZ activation seemingly enhances self-renewal and replenishment of satellite cells, along with myogenesis.
Others
The study of the Hippo pathway now covers a large number of fields and has provided researchers with many unexpected yet interesting findings. During development of the salivary submandibular gland, TAZ becomes phosphorylated and associated with E-cadherin and α-catenin [236]. Perturbation of the Hippo pathway results in dysmorphogenesis of the gland. In patients with Sjögren’s syndrome, TAZ is mislocalized from cell junctions. Although TAZ mislocalization could be a secondary result of cell junction disruption, it is also possible that dysregulation of the Hippo pathway is implicated in the pathophysiology of Sjögren’s syndrome. Fragmentation of the mouse ovary disrupts the Hippo pathway and promotes follicle formation [237]. Based on this observation, the fragmentation of the ovary with Akt stimulation is used to treat primary ovarian insufficiency.
Conclusions and future perspectives
Almost 10 years ago, the Hippo pathway started with four members (hpo, sav, wts, and mats) that partook in five interactions (HPO-SAV, HPO-WTS, HPO-Mats, SAV-WTS, and WTS-Mats). However, since then, new components have continued to be identified. There have been five recent papers reporting the proteome-scale analysis of the Hippo pathway (one for Drosophila, four for mammals) [238–242]. These papers illustrate the daunting and complicated protein network underlying the Hippo pathway. The original founding members are obscured among numerous proteins. It needs to be discussed which part is the most essential for the Hippo pathway. The pathway was initially defined as the organ size controlling pathway. To build up an organ with its proper size, cells need to behave as players in the mass games. They should receive the information from without, judge their own places, know what the neighboring cells do, and determine whether to proliferate, differentiate, or not. YAP1 and TAZ sense external cues such as cell density, stretching, cell geometry, and matrix rigidity; they are also regulated by the maturity of cell junctions. This combination of properties allows the placement of YAP1 and TAZ at the center of the Hippo pathway.
YAP1 and TAZ are frequently discussed together but have distinct properties. The phenotypes of YAP1 and TAZ knockout mice differ. During development, especially in the early phase, YAP1 appears to be more important than TAZ. In ES cells and tissue progenitor cells, YAP1 promotes self-renewal and inhibits differentiation. This is in sharp contrast to TAZ, which tends to facilitate differentiation. YAP1 and TAZ are both considered to be oncogenes. However, TAZ is more oncogenic. A study using Ha-ras-transformed immortalized human mammalian epithelial MCF10A cells revealed that TAZ, but not YAP1, is up-regulated in malignant subtypes with higher tumor-initiating capacity [185]. In our hands, MCF10A cells expressing the active TAZ mutant can survive under floating conditions and form spheres; MCF10A cells expressing the active YAP1 mutant cannot form spheres (unpublished observation). YAP1 and TAZ differ in their interactions with transcription factors. Unfortunately researchers do not publish the negative data. TAZ interacts with MyoD, but there are no reports to indicate that YAP1 does not interact with MyoD. Likewise, it is not reported that TAZ does not interact with p73. It is important to study YAP1 and TAZ in parallel and compare the results. If YAP1 shifts stem cells towards self-renewal and TAZ shifts them towards differentiation, YAP1 and TAZ are likely to interact with the NuRD complex in different ways. It is essential to detect YAP1 and TAZ with specific antibodies in the interaction with the NuRD complex. To use YAP1- and TAZ-targeted drugs for cancer therapy and in regenerative medicine, it will be necessary to collect baseline information about YAP1 and TAZ. The combined use of YAP1 and TAZ activators could enable us to control tissue regeneration more efficiently.
We also question whether the mammalian Hippo pathway has other function not related to the control of organ size. DNA damage switches on the Hippo pathway to trigger the checkpoint. Genomic instability is a hallmark of cancer, while maintenance of genomic integrity is a central role of the mammalian Hippo pathway. The Hippo pathway functions in hemopoietic cells, but it is not known how the Hippo pathway is activated in these cells. It is possible that they receive signals from cell–cell contacts, cell–matrix contacts, and/or soluble ligands. We now know that glucagon and epinephrine activate the Hippo pathway. This prompts us to ask whether the Hippo pathway is activated in the human body in response to serum glucose levels and sympathetic nerve stimuli. If we reconsider the roles of YAP1 and TAZ as mechanosensors, we need to study how YAP1 and TAZ respond to exercise in skeletal muscles; blood pressure changes in the heart and arteries; shear forces in ciliated epithelial cells; skin stretching, and loads placed upon bone. We hope that the next decade of the Hippo pathway research will allow us to answer these questions.
References
Justice RW, Zilian O, Woods DF, Noll M, Bryant PJ (1995) The Drosophila tumor suppressor gene warts encodes a homolog of human myotonic dystrophy kinase and is required for the control of cell shape and proliferation. Genes Dev 9:534–546
Xu T, Wang W, Zhang S, Stewart RA, Yu W (1995) Identifying tumor suppressors in genetic mosaics: the Drosophila lats gene encodes a putative protein kinase. Development 121:1053–1063
Harvey KF, Pfleger CM, Hariharan IK (2003) The Drosophila Mst ortholog, hippo, restricts growth and cell proliferation and promotes apoptosis. Cell 114:457–467
Pantalacci S, Tapon N, Léopold P (2003) The Salvador partner Hippo promotes apoptosis and cell-cycle exit in Drosophila. Nat Cell Biol 5:921–927
Udan RS, Kango-Singh M, Nolo R, Tao C, Halder G (2003) Hippo promotes proliferation arrest and apoptosis in the Salvador/Warts pathway. Nat Cell Biol 5:914–920
Wu S, Huang J, Dong J, Pan D (2003) hippo encodes a Ste-20 family protein kinase that restricts cell proliferation and promotes apoptosis in conjunction with salvador and warts. Cell 114:445–456
Jia J, Zhang W, Wang B, Trinko R, Jiang J (2003) The Drosophila Ste20 family kinase dMST functions as a tumor suppressor by restricting cell proliferation and promoting apoptosis. Genes Dev 17:2514–2519
Tapon N, Harvey KF, Bell DW, Wahrer DC, Schiripo TA, Haber D, Hariharan IK (2002) Salvador promotes both cell cycle exit and apoptosis in Drosophila and is mutated in human cancer cell lines. Cell 110:467–478
Lai ZC, Wei X, Shimizu T, Ramos E, Rohrbaugh M, Nikolaidis N, Ho LL, Li Y (2005) Control of cell proliferation and apoptosis by mob as tumor suppressor, mats. Cell 120:675–685
Huang J, Wu S, Barrera J, Matthews K, Pan D (2005) The Hippo signaling pathway coordinately regulates cell proliferation and apoptosis by inactivating Yorkie, the Drosophila Homolog of YAP. Cell 122:421–434
St John MA, Tao W, Fei X, Fukumoto R, Carcangiu ML, Brownstein DG, Parlow AF, McGrath J, Xu T (1999) Mice deficient of Lats1 develop soft-tissue sarcomas, ovarian tumours and pituitary dysfunction. Nat Genet 21:182–186
Hamaratoglu F, Willecke M, Kango-Singh M, Nolo R, Hyun E, Tao C, Jafar-Nejad H, Halder G (2006) The tumour-suppressor genes NF2/Merlin and expanded act through Hippo signalling to regulate cell proliferation and apoptosis. Nat Cell Biol 8:27–36
Sudol M (1994) Yes-associated protein (YAP65) is a proline-rich phosphoprotein that binds to the SH3 domain of the Yes proto-oncogene product. Oncogene 9:2145–2152
Kanai F, Marignani PA, Sarbassova D, Yagi R, Hall RA, Donowitz M, Hisaminato A, Fujiwara T, Ito Y, Cantley LC, Yaffe MB (2000) TAZ: a novel transcriptional co-activator regulated by interactions with 14-3-3 and PDZ domain proteins. EMBO J 19:6778–6791
Qin F, Tian J, Zhou D, Chen L (2013) Mst1 and Mst2 kinases: regulations and diseases. Cell Biosci 3:31
Hergovich A (2013) Regulation and functions of mammalian LATS/NDR kinases: looking beyond canonical Hippo signalling. Cell Biosci 3:32
Gaffney CJ, Oka T, Mazack V, Hilman D, Gat U, Muramatsu T, Inazawa J, Golden A, Carey DJ, Farooq A, Tromp G, Sudol M (2012) Identification, basic characterization and evolutionary analysis of differentially spliced mRNA isoforms of human YAP1 gene. Gene 509:215–222
Webb C, Upadhyay A, Giuntini F, Eggleston I, Furutani-Seiki M, Ishima R, Bagby S (2011) Structural features and ligand binding properties of tandem WW domains from YAP and TAZ, nuclear effectors of the Hippo pathway. Biochemistry 50:3300–3309
Howell M, Borchers C, Milgram SL (2004) Heterogeneous nuclear ribonuclear protein U associates with YAP and regulates its co-activation of Bax transcription. J Biol Chem 279:26300–26306
Lei QY, Zhang H, Zhao B, Zha ZY, Bai F, Pei XH, Zhao S, Xiong Y, Guan KL (2008) TAZ promotes cell proliferation and epithelial-mesenchymal transition and is inhibited by the hippo pathway. Mol Cell Biol 28:2426–2436
Basu S, Totty NF, Irwin MS, Sudol M, Downward J (2003) Akt phosphorylates the yes-associated protein, YAP, to induce interaction with 14-3-3 and attenuation of p73-mediated apoptosis. Mol Cell 11:11–23
Liu CY, Zha ZY, Zhou X, Zhang H, Huang W, Zhao D, Li T, Chan SW, Lim CJ, Hong W, Zhao S, Xiong Y, Lei QY, Guan KL (2010) The hippo tumor pathway promotes TAZ degradation by phosphorylating a phosphodegron and recruiting the SCF{beta}-TrCP E3 ligase. J Biol Chem 285:37159–37169
Zhao B, Li L, Tumaneng K, Wang CY, Guan KL (2010) A coordinated phosphorylation by Lats and CK1 regulates YAP stability through SCF(beta-TRCP). Genes Dev 24:72–85
Huang W, Lv X, Liu C, Zha Z, Zhang H, Jiang Y, Xiong Y, Lei QY, Guan KL (2012) The N-terminal phosphodegron targets TAZ/WWTR1 protein for SCFβ-TrCP-dependent degradation in response to phosphatidylinositol 3-kinase inhibition. J Biol Chem 287:26245–26253
Tamm C, Böwer N, Annerén C (2011) Regulation of mouse embryonic stem cell self-renewal by a Yes-YAP-TEAD2 signaling pathway downstream of LIF. J Cell Sci 124:1136–1144
Rosenbluh J, Nijhawan D, Cox AG, Li X, Neal JT, Schafer EJ, Zack TI, Wang X, Tsherniak A, Schinzel AC, Shao DD, Schumacher SE, Weir BA, Vazquez F, Cowley GS, Root DE, Mesirov JP, Beroukhim R, Kuo CJ, Goessling W, Hahn WC (2012) β-Catenin-driven cancers require a YAP1 transcriptional complex for survival and tumorigenesis. Cell 151:1457–1473
Zaidi SK, Sullivan AJ, Medina R, Ito Y, van Wijnen AJ, Stein JL, Lian JB, Stein GS (2004) Tyrosine phosphorylation controls Runx2-mediated subnuclear targeting of YAP to repress transcription. EMBO J 23:790–799
Levy D, Adamovich Y, Reuven N, Shaul Y (2008) Yap1 phosphorylation by c-Abl is a critical step in selective activation of proapoptotic genes in response to DNA damage. Mol Cell 29:350–361
Levy D, Adamovich Y, Reuven N, Shaul Y (2007) The Yes-associated protein 1 stabilizes p73 by preventing Itch-mediated ubiquitination of p73. Cell Death Differ 14:743–751
Levy D, Reuven N, Shaul Y (2008) A regulatory circuit controlling Itch-mediated p73 degradation by Runx. J Biol Chem 283:27462–27468
Strano S, Munarriz E, Rossi M, Castagnoli L, Shaul Y, Sacchi A, Oren M, Sudol M, Cesareni G, Blandino G (2001) Physical interaction with Yes-associated protein enhances p73 transcriptional activity. J Biol Chem 276:15164–15173
Danovi SA, Rossi M, Gudmundsdottir K, Yuan M, Melino G, Basu S (2008) Yes-associated protein (YAP) is a critical mediator of c-Jun-dependent apoptosis. Cell Death Differ 15:217–219
Tomlinson V, Gudmundsdottir K, Luong P, Leung KY, Knebel A, Basu S (2010) JNK phosphorylates yes-associated protein (YAP) to regulate apoptosis. Cell Death Dis 1:e29
Yang S, Zhang L, Liu M, Chong R, Ding SJ, Chen Y, Dong J (2013) CDK1 phosphorylation of YAP promotes mitotic defects and cell motility and is essential for neoplastic transformation. Cancer Res 73:6722–6733
Yim H, Sung CK, You J, Tian Y, Benjamin T (2011) Nek1 and TAZ interact to maintain normal levels of polycystin 2. J Am Soc Nephrol 22:832–837
Fausti F, Di Agostino S, Cioce M, Bielli P, Sette C, Pandolfi PP, Oren M, Sudol M, Strano S, Blandino G (2013) ATM kinase enables the functional axis of YAP, PML and p53 to ameliorate loss of Werner protein-mediated oncogenic senescence. Cell Death Differ 20:1498–1509
Liu CY, Lv X, Li T, Xu Y, Zhou X, Zhao S, Xiong Y, Lei QY, Guan KL (2011) PP1 cooperates with ASPP2 to dephosphorylate and activate TAZ. J Biol Chem 286:5558–5566
Cai H, Xu Y (2013) The role of LPA and YAP signaling in long-term migration of human ovarian cancer cells. Cell Commun Signal 11:31
Schlegelmilch K, Mohseni M, Kirak O, Pruszak J, Rodriguez JR, Zhou D, Kreger BT, Vasioukhin V, Avruch J, Brummelkamp TR, Camargo FD (2011) Yap1 acts downstream of α-catenin to control epidermal proliferation. Cell 144:782–795
Huang JM, Nagatomo I, Suzuki E, Mizuno T, Kumagai T, Berezov A, Zhang H, Karlan B, Greene MI, Wang Q (2013) YAP modifies cancer cell sensitivity to EGFR and survivin inhibitors and is negatively regulated by the non-receptor type protein tyrosine phosphatase 14. Oncogene 32:2220–2229
Liu X, Yang N, Figel SA, Wilson KE, Morrison CD, Gelman IH, Zhang J (2013) PTPN14 interacts with and negatively regulates the oncogenic function of YAP. Oncogene 32:1266–1273
Wang W, Huang J, Wang X, Yuan J, Li X, Feng L, Park JI, Chen J (2012) PTPN14 is required for the density-dependent control of YAP1. Genes Dev 26:1959–1971
Hata S, Hirayama J, Kajiho H, Nakagawa K, Hata Y, Katada T, Furutani-Seiki M, Nishina H (2012) A novel acetylation cycle of transcription co-activator Yes-associated protein that is downstream of Hippo pathway is triggered in response to SN2 alkylating agents. J Biol Chem 287:22089–22098
Oudhoff MJ, Freeman SA, Couzens AL, Antignano F, Kuznetsova E, Min PH, Northrop JP, Lehnertz B, Barsyte-Lovejoy D, Vedadi M, Arrowsmith CH, Nishina H, Gold MR, Rossi FM, Gingras AC, Zaph C (2013) Control of the hippo pathway by Set7-dependent methylation of Yap. Dev Cell 26:188–194
Lapi E, Di Agostino S, Donzelli S, Gal H, Domany E, Rechavi G, Pandolfi PP, Givol D, Strano S, Lu X, Blandino G (2008) PML, YAP, and p73 are components of a proapoptotic autoregulatory feedback loop. Mol Cell 32:803–814
Cappello S, Gray MJ, Badouel C, Lange S, Einsiedler M, Srour M, Chitayat D, Hamdan FF, Jenkins ZA, Morgan T, Preitner N, Uster T, Thomas J, Shannon P, Morrison V, Di Donato N, Van Maldergem L, Neuhann T, Newbury-Ecob R, Swinkells M, Terhal P, Wilson LC, Zwijnenburg PJ, Sutherland-Smith AJ, Black MA, Markie D, Michaud JL, Simpson MA, Mansour S, McNeill H, Götz M, Robertson SP (2013) Mutations in genes encoding the cadherin receptor-ligand pair DCHS1 and FAT4 disrupt cerebral cortical development. Nat Genet 45:1300–1308
Murphy AJ, Pierce J, de Caestecker C, Libes J, Neblett D, de Caestecker M, Perantoni AO, Tanigawa S, Anderson JR, Dome JS, Das A, Carroll TJ, Lovvorn HN (2014) Aberrant activation, nuclear localization, and phosphorylation of Yes-associated protein-1 in the embryonic kidney and Wilms tumor. Pediatr Blood Cancer 61:198–205
Saburi S, Hester I, Fischer E, Pontoglio M, Eremina V, Gessler M, Quaggin SE, Harrison R, Mount R, McNeill H (2008) Loss of Fat4 disrupts PCP signaling and oriented cell division and leads to cystic kidney disease. Nat Genet 40:1010–1015
Makita R, Uchijima Y, Nishiyama K, Amano T, Chen Q, Takeuchi T, Mitani A, Nagase T, Yatomi Y, Aburatani H, Nakagawa O, Small EV, Cobo-Stark P, Igarashi P, Murakami M, Tominaga J, Sato T, Asano T, Kurihara Y, Kurihara H (2008) Multiple renal cysts, urinary concentration defects, and pulmonary emphysematous changes in mice lacking TAZ. Am J Physiol Renal Physiol 294:F542–F553
Hossain Z, Ali SM, Ko HL, Xu J, Ng CP, Guo K, Qi Z, Ponniah S, Hong W, Hunziker W (2007) Glomerulocystic kidney disease in mice with a targeted inactivation of Wwtr1. Proc Natl Acad Sci USA 104:1631–1636
Xu Y, Stamenkovic I, Yu Q (2010) CD44 attenuates activation of the hippo signaling pathway and is a prime therapeutic target for glioblastoma. Cancer Res 70:2455–2464
Tsuneki M, Madri JA (2014) CD44 regulation of endothelial cell proliferation and apoptosis via modulation of CD31 and VE-cadherin expression. J Biol Chem 289:5357–5370
Bao Y, Nakagawa K, Yang Z, Ikeda M, Withanage K, Ishigami-Yuasa M, Okuno Y, Hata S, Nishina H, Hata Y (2011) A cell-based assay to screen stimulators of the Hippo pathway reveals the inhibitory effect of dobutamine on the YAP-dependent gene transcription. J Biochem 150:199–208
Mo JS, Yu FX, Gong R, Brown JH, Guan KL (2012) Regulation of the Hippo-YAP pathway by protease-activated receptors (PARs). Genes Dev 26:2138–2143
Yu FX, Zhao B, Panupinthu N, Jewell JL, Lian I, Wang LH, Zhao J, Yuan H, Tumaneng K, Li H, Fu XD, Mills GB, Guan KL (2012) Regulation of the Hippo-YAP pathway by G-protein-coupled receptor signaling. Cell 150:780–791
Miller E, Yang J, DeRan M, Wu C, Su AI, Bonamy GM, Liu J, Peters EC, Wu X (2012) Identification of serum-derived sphingosine-1-phosphate as a small molecule regulator of YAP. Chem Biol 19:955–962
Yu FX, Zhang Y, Park HW, Jewell JL, Chen Q, Deng Y, Pan D, Taylor SS, Lai ZC, Guan KL (2013) Protein kinase A activates the Hippo pathway to modulate cell proliferation and differentiation. Genes Dev 27:1223–1232
Kim M, Lee S, Kuninaka S, Saya H, Lee H, Lim DS (2013) cAMP/PKA signalling reinforces the LATS-YAP pathway to fully suppress YAP in response to actin cytoskeletal changes. EMBO J 32:1543–1555
Yu FX, Luo J, Mo JS, Liu G, Kim YC, Meng Z, Zhao L, Peyman G, Ouyang H, Jiang W, Zhao J, Chen X, Zhang L, Wang CY, Bastian BC, Zhang K, Guan KL (2014) Mutant Gq/11 promote uveal melanoma tumorigenesis by activating YAP. Cancer Cell 25:822–830
Feng X, Degese MS, Iglesias-Bartolome R, Vaque JP, Molinolo AA, Rodrigues M, Zaidi MR, Ksander BR, Merlino G, Sodhi A, Chen Q, Gutkind JS (2014) Hippo-independent activation of YAP by the GNAQ uveal melanoma oncogene through a trio-regulated rho GTPase signaling circuitry. Cancer Cell 25:831–845
Chen D, Sun Y, Wei Y, Zhang P, Rezaeian AH, Teruya-Feldstein J, Gupta S, Liang H, Lin HK, Hung MC, Ma L (2012) LIFR is a breast cancer metastasis suppressor upstream of the Hippo-YAP pathway and a prognostic marker. Nat Med 18:1511–1517
Cooper J, Giancotti FG (2014) Molecular insights into NF2/Merlin tumor suppressor function. FEBS Lett 588(16):2743–2752
Zhang N, Bai H, David KK, Dong J, Zheng Y, Cai J, Giovannini M, Liu P, Anders RA, Pan D (2010) The Merlin/NF2 tumor suppressor functions through the YAP oncoprotein to regulate tissue homeostasis in mammals. Dev Cell 19:27–38
Gladden AB, Hebert AM, Schneeberger EE, McClatchey AI (2010) The NF2 tumor suppressor, Merlin, regulates epidermal development through the establishment of a junctional polarity complex. Dev Cell 19:727–739
Angus L, Moleirinho S, Herron L, Sinha A, Zhang X, Niestrata M, Dholakia K, Prystowsky MB, Harvey KF, Reynolds PA, Gunn-Moore FJ (2012) Willin/FRMD6 expression activates the Hippo signaling pathway kinases in mammals and antagonizes oncogenic YAP. Oncogene 31:238–250
Genevet A, Wehr MC, Brain R, Thompson BJ, Tapon N (2010) Kibra is a regulator of the Salvador/Warts/Hippo signaling network. Dev Cell 18:300–308
Yu J, Zheng Y, Dong J, Klusza S, Deng WM, Pan D (2010) Kibra functions as a tumor suppressor protein that regulates Hippo signaling in conjunction with Merlin and expanded. Dev Cell 18:288–299
Xiao L, Chen Y, Ji M, Dong J (2011) KIBRA regulates Hippo signaling activity via interactions with large tumor suppressor kinases. J Biol Chem 286:7788–7796
Moleirinho S, Guerrant W, Kissil JL (2014) The Angiomotins: from discovery to function. FEBS Lett 588(16):2693–2703
Wells CD, Fawcett JP, Traweger A, Yamanaka Y, Goudreault M, Elder K, Kulkarni S, Gish G, Virag C, Lim C, Colwill K, Starostine A, Metalnikov P, Pawson T (2006) A Rich1/Amot complex regulates the Cdc42 GTPase and apical-polarity proteins in epithelial cells. Cell 125:535–548
Yi C, Troutman S, Fera D, Stemmer-Rachamimov A, Avila JL, Christian N, Persson NL, Shimono A, Speicher DW, Marmorstein R, Holmgren L, Kissil JL (2011) A tight junction-associated Merlin-angiomotin complex mediates Merlin’s regulation of mitogenic signaling and tumor suppressive functions. Cancer Cell 19:527–540
Zhao B, Li L, Lu Q, Wang LH, Liu CY, Lei Q, Guan KL (2011) Angiomotin is a novel Hippo pathway component that inhibits YAP oncoprotein. Genes Dev 25:51–63
Chan SW, Lim CJ, Chong YF, Pobbati AV, Huang C, Hong W (2011) Hippo pathway-independent restriction of TAZ and YAP by angiomotin. J Biol Chem 286:7018–7026
Yi C, Shen Z, Stemmer-Rachamimov A, Dawany N, Troutman S, Showe LC, Liu Q, Shimono A, Sudol M, Holmgren L, Stanger BZ, Kissil JL (2013) The p130 isoform of angiomotin is required for Yap-mediated hepatic epithelial cell proliferation and tumorigenesis. Sci Signal 6:ra77
Das Thakur M, Feng Y, Jagannathan R, Seppa MJ, Skeath JB, Longmore GD (2010) Ajuba LIM proteins are negative regulators of the Hippo signaling pathway. Curr Biol 20:657–662
Reddy BV, Irvine KD (2013) Regulation of Hippo signaling by EGFR-MAPK signaling through Ajuba family proteins. Dev Cell 24:459–471
Sun G, Irvine KD (2013) Ajuba family proteins link JNK to Hippo signaling. Sci Signal 6:ra81
Codelia VA, Sun G, Irvine KD (2014) Regulation of YAP by mechanical strain through jnk and hippo signaling. Curr Biol 24(17):2012–2017
Tanaka I, Osada H, Fujii M, Fukatsu A, Hida T, Horio Y, Kondo Y, Sato A, Hasegawa Y, Tsujimura T, Sekido Y (2013) LIM-domain protein AJUBA suppresses malignant mesothelioma cell proliferation via Hippo signaling cascade. Oncogene. doi:10.1038/onc.2013.528
Oka T, Remue E, Meerschaert K, Vanloo B, Boucherie C, Gfeller D, Bader GD, Sidhu SS, Vandekerckhove J, Gettemans J, Sudol M (2010) Functional complexes between YAP2 and ZO-2 are PDZ domain-dependent, and regulate YAP2 nuclear localization and signalling. Biochem J 432:461–472
Remue E, Meerschaert K, Oka T, Boucherie C, Vandekerckhove J, Sudol M, Gettemans J (2010) TAZ interacts with zonula occludens-1 and -2 proteins in a PDZ-1 dependent manner. FEBS Lett 584:4175–4180
Dupont S, Morsut L, Aragona M, Enzo E, Giulitti S, Cordenonsi M, Zanconato F, Le Digabel J, Forcato M, Bicciato S, Elvassore N, Piccolo S (2011) Role of YAP/TAZ in mechanotransduction. Nature 474:179–183
Sorrentino G, Ruggeri N, Specchia V, Cordenonsi M, Mano M, Dupont S, Manfrin A, Ingallina E, Sommaggio R, Piazza S, Rosato A, Piccolo S, Del Sal G (2014) Metabolic control of YAP and TAZ by the mevalonate pathway. Nat Cell Biol 16:357–366
Reginensi A, Scott RP, Gregorieff A, Bagherie-Lachidan M, Chung C, Lim DS, Pawson T, Wrana J, McNeill H (2013) Yap- and Cdc42-dependent nephrogenesis and morphogenesis during mouse kidney development. PLoS Genet 9:e1003380
Fernández BG, Gaspar P, Brás-Pereira C, Jezowska B, Rebelo SR, Janody F (2011) Actin-Capping Protein and the Hippo pathway regulate F-actin and tissue growth in Drosophila. Development 138:2337–2346
Calvo F, Ege N, Grande-Garcia A, Hooper S, Jenkins RP, Chaudhry SI, Harrington K, Williamson P, Moeendarbary E, Charras G, Sahai E (2013) Mechanotransduction and YAP-dependent matrix remodelling is required for the generation and maintenance of cancer-associated fibroblasts. Nat Cell Biol 15:637–646
Pelissier FA, Garbe JC, Ananthanarayanan B, Miyano M, Lin C, Jokela T, Kumar S, Stampfer MR, Lorens JB, LaBarge MA (2014) Age-related dysfunction in mechanotransduction impairs differentiation of human mammary epithelial progenitors. Cell Rep 7:1926–1939
Sun Y, Yong KM, Villa-Diaz LG, Zhang X, Chen W, Philson R, Weng S, Xu H, Krebsbach PH, Fu J (2014) Hippo/YAP-mediated rigidity-dependent motor neuron differentiation of human pluripotent stem cells. Nat Mater 13:599–604
Boggiano JC, Vanderzalm PJ, Fehon RG (2011) Tao-1 phosphorylates Hippo/MST kinases to regulate the Hippo-Salvador-Warts tumor suppressor pathway. Dev Cell 21:888–895
Poon CL, Lin JI, Zhang X, Harvey KF (2011) The sterile 20-like kinase Tao-1 controls tissue growth by regulating the Salvador-Warts-Hippo pathway. Dev Cell 21:896–906
Wehr MC, Holder MV, Gailite I, Saunders RE, Maile TM, Ciirdaeva E, Instrell R, Jiang M, Howell M, Rossner MJ, Tapon N (2013) Salt-inducible kinases regulate growth through the Hippo signalling pathway in Drosophila. Nat Cell Biol 15:61–71
Mohseni M, Sun J, Lau A, Curtis S, Goldsmith J, Fox VL, Wei C, Frazier M, Samson O, Wong KK, Kim C, Camargo FD (2014) A genetic screen identifies an LKB1-MARK signalling axis controlling the Hippo-YAP pathway. Nat Cell Biol 16:108–117
Gao Y, Zhang W, Han X, Li F, Wang X, Wang R, Fang Z, Tong X, Yao S, Feng Y, Sun Y, Hou Y, Yang Z, Guan K, Chen H, Zhang L, Ji H (2014) YAP inhibits squamous transdifferentiation of Lkb1-deficient lung adenocarcinoma through ZEB2-dependent DNp63 repression. Nat Commun 5:4629
Serrano I, McDonald PC, Lock F, Muller WJ, Dedhar S (2013) Inactivation of the Hippo tumour suppressor pathway by integrin-linked kinase. Nat Commun 4:2976
Poon CL, Zhang X, Lin JI, Manning SA, Harvey KF (2012) Homeodomain-interacting protein kinase regulates Hippo pathway-dependent tissue growth. Curr Biol 22:1587–1594
Polesello C, Huelsmann S, Brown NH, Tapon N (2006) The Drosophila RASSF homolog antagonizes the hippo pathway. Curr Biol 16:2459–2465
Volodko N, Gordon M, Salla M, Ghazaleh HA, Baksh S (2014) RASSF tumor suppressor gene family: Biological functions and regulation. FEBS Lett 588(16):2671–2684
Praskova M, Khoklatchev A, Ortiz-Vega S, Avruch J (2004) Regulation of the MST1 kinase by autophosphorylation, by the growth inhibitory proteins, RASSF1 and NORE1, and by Ras. Biochem J 381:453–462
Matallanas D, Romano D, Yee K, Meissl K, Kucerova L, Piazzolla D, Baccarini M, Vass JK, Kolch W, O’neill E (2007) RASSF1A elicits apoptosis through an MST2 pathway directing proapoptotic transcription by the p73 tumor suppressor protein. Mol Cell 27:962–975
Khokhlatchev A, Rabizadeh S, Xavier R, Nedwidek M, Chen T, Zhang XF, Seed B, Avruch J (2002) Identification of a novel Ras-regulated proapoptotic pathway. Curr Biol 12:253–265
Cooper WN, Hesson LB, Matallanas D, Dallol A, von Kriegsheim A, Ward R, Kolch W, Latif F (2009) RASSF2 associates with and stabilizes the proapoptotic kinase MST2. Oncogene 28:2988–2998
Song H, Oh S, Oh HJ, Lim DS (2010) Role of the tumor suppressor RASSF2 in regulation of MST1 kinase activity. Biochem Biophys Res Commun 391:969–973
Ikeda M, Hirabayashi S, Fujiwara N, Mori H, Kawata A, Iida J, Bao Y, Sato Y, Iida T, Sugimura H, Hata Y (2007) Ras-association domain family protein 6 induces apoptosis via both caspase-dependent and caspase-independent pathways. Exp Cell Res 313:1484–1495
Iwasa H, Kudo T, Maimaiti S, Ikeda M, Maruyama J, Nakagawa K, Hata Y (2013) The RASSF6 tumor suppressor protein regulates apoptosis and the cell cycle via MDM2 protein and p53 protein. J Biol Chem 288:30320–30329
Crose LE, Galindo KA, Kephart JG, Chen C, Fitamant J, Bardeesy N, Bentley RC, Galindo RL, Ashley Chi JT, Linardic CM (2014) Alveolar rhabdomyosarcoma-associated PAX3-FOXO1 promotes tumorigenesis via Hippo pathway suppression. J Clin Invest 124(1):285–296
Ribeiro PS, Josué F, Wepf A, Wehr MC, Rinner O, Kelly G, Tapon N, Gstaiger M (2010) Combined functional genomic and proteomic approaches identify a PP2A complex as a negative regulator of Hippo signaling. Mol Cell 39:521–534
Guo C, Zhang X, Pfeifer GP (2011) The tumor suppressor RASSF1A prevents dephosphorylation of the mammalian STE20-like kinases MST1 and MST2. J Biol Chem 286:6253–6261
Habbig S, Bartram MP, Müller RU, Schwarz R, Andriopoulos N, Chen S, Sägmüller JG, Hoehne M, Burst V, Liebau MC, Reinhardt HC, Benzing T, Schermer B (2011) NPHP4, a cilia-associated protein, negatively regulates the Hippo pathway. J Cell Biol 193:633–642
Habbig S, Bartram MP, Sägmüller JG, Griessmann A, Franke M, Müller RU, Schwarz R, Hoehne M, Bergmann C, Tessmer C, Reinhardt HC, Burst V, Benzing T, Schermer B (2012) The ciliopathy disease protein NPHP9 promotes nuclear delivery and activation of the oncogenic transcriptional regulator TAZ. Hum Mol Genet 21:5528–5538
Vigneron AM, Ludwig RL, Vousden KH (2010) Cytoplasmic ASPP1 inhibits apoptosis through the control of YAP. Genes Dev 24:2430–2439
Jeon YH, Park YH, Lee JH, Hong JH, Kim IY (2014) Selenoprotein W enhances skeletal muscle differentiation by inhibiting TAZ binding to 14-3-3 protein. Biochim Biophys Acta 1843:1356–1364
Sansores-Garcia L, Atkins M, Moya IM, Shahmoradgoli M, Tao C, Mills GB, Halder G (2013) Mask is required for the activity of the Hippo pathway effector Yki/YAP. Curr Biol 23:229–235
Sidor CM, Brain R, Thompson BJ (2013) Mask proteins are cofactors of Yorkie/YAP in the Hippo pathway. Curr Biol 23:223–228
Machado-Neto JA, Lazarini M, Favaro P, Franchi GC, Nowill AE, Saad ST, Traina F (2014) ANKHD1, a novel component of the Hippo signaling pathway, promotes YAP1 activation and cell cycle progression in prostate cancer cells. Exp Cell Res 324:137–145
Strano S, Monti O, Pediconi N, Baccarini A, Fontemaggi G, Lapi E, Mantovani F, Damalas A, Citro G, Sacchi A, Del Sal G, Levrero M, Blandino G (2005) The transcriptional coactivator yes-associated protein drives p73 gene-target specificity in response to DNA Damage. Mol Cell 18:447–459
Wu H, Xiao Y, Zhang S, Ji S, Wei L, Fan F, Geng J, Tian J, Sun X, Qin F, Jin C, Lin J, Yin ZY, Zhang T, Luo L, Li Y, Song S, Lin SC, Deng X, Camargo F, Avruch J, Chen L, Zhou D (2013) The Ets transcription factor GABP is a component of the hippo pathway essential for growth and antioxidant defense. Cell Rep 3:1663–1677
Seo E, Basu-Roy U, Gunaratne PH, Coarfa C, Lim DS, Basilico C, Mansukhani A (2013) SOX2 regulates YAP1 to maintain stemness and determine cell fate in the osteo-adipo lineage. Cell Rep 3:2075–2087
Mahoney JE, Mori M, Szymaniak AD, Varelas X, Cardoso WV (2014) The hippo pathway effector yap controls patterning and differentiation of airway epithelial progenitors. Dev Cell 30:137–150
Pobbati AV, Hong W (2013) Emerging roles of TEAD transcription factors and its coactivators in cancers. Cancer Biol Ther 14:390–398
Chen L, Chan SW, Zhang X, Walsh M, Lim CJ, Hong W, Song H (2010) Structural basis of YAP recognition by TEAD4 in the hippo pathway. Genes Dev 24:290–300
Li Z, Zhao B, Wang P, Chen F, Dong Z, Yang H, Guan KL, Xu Y (2010) Structural insights into the YAP and TEAD complex. Genes Dev 24:235–240
Tian W, Yu J, Tomchick DR, Pan D, Luo X (2010) Structural and functional analysis of the YAP-binding domain of human TEAD2. Proc Natl Acad Sci USA 107:7293–7298
Mesrouze Y, Hau JC, Erdmann D, Zimmermann C, Fontana P, Schmelzle T, Chène P (2014) The surprising features of the TEAD4-Vgll1 protein-protein interaction. Chem Bio Chem 15:537–542
Hau JC, Erdmann D, Mesrouze Y, Furet P, Fontana P, Zimmermann C, Schmelzle T, Hofmann F, Chène P (2013) The TEAD4-YAP/TAZ protein-protein interaction: expected similarities and unexpected differences. Chem Bio Chem 14:1218–1225
Koontz LM, Liu-Chittenden Y, Yin F, Zheng Y, Yu J, Huang B, Chen Q, Wu S, Pan D (2013) The Hippo effector Yorkie controls normal tissue growth by antagonizing scalloped-mediated default repression. Dev Cell 25:388–401
Zhang W, Gao Y, Li P, Shi Z, Guo T, Li F, Han X, Feng Y, Zheng C, Wang Z, Chen H, Zhou Z, Zhang L, Ji H (2014) VGLL4 functions as a new tumor suppressor in lung cancer by negatively regulating the YAP-TEAD transcriptional complex. Cell Res 24:331–343
Jiao S, Wang H, Shi Z, Dong A, Zhang W, Song X, He F, Wang Y, Zhang Z, Wang W, Wang X, Guo T, Li P, Zhao Y, Ji H, Zhang L, Zhou Z (2014) A peptide mimicking VGLL4 function acts as a YAP antagonist therapy against gastric cancer. Cancer Cell 25:166–180
Alarcón C, Zaromytidou AI, Xi Q, Gao S, Yu J, Fujisawa S, Barlas A, Miller AN, Manova-Todorova K, Macias MJ, Sapkota G, Pan D, Massagué J (2009) Nuclear CDKs drive Smad transcriptional activation and turnover in BMP and TGF-beta pathways. Cell 139:757–769
Fujii M, Nakanishi H, Toyoda T, Tanaka I, Kondo Y, Osada H, Sekido Y (2012) Convergent signaling in the regulation of connective tissue growth factor in malignant mesothelioma: TGFβ signaling and defects in the Hippo signaling cascade. Cell Cycle 11:3373–3379
Mahoney WM, Hong JH, Yaffe MB, Farrance IK (2005) The transcriptional co-activator TAZ interacts differentially with transcriptional enhancer factor-1 (TEF-1) family members. Biochem J 388:217–225
Ferrigno O, Lallemand F, Verrecchia F, L’Hoste S, Camonis J, Atfi A, Mauviel A (2002) Yes-associated protein (YAP65) interacts with Smad7 and potentiates its inhibitory activity against TGF-beta/Smad signaling. Oncogene 21:4879–4884
Varelas X, Sakuma R, Samavarchi-Tehrani P, Peerani R, Rao BM, Dembowy J, Yaffe MB, Zandstra PW, Wrana JL (2008) TAZ controls Smad nucleocytoplasmic shuttling and regulates human embryonic stem-cell self-renewal. Nat Cell Biol 10:837–848
Varelas X, Samavarchi-Tehrani P, Narimatsu M, Weiss A, Cockburn K, Larsen BG, Rossant J, Wrana JL (2010) The Crumbs complex couples cell density sensing to Hippo-dependent control of the TGF-β-SMAD pathway. Dev Cell 19:831–844
Murakami M, Tominaga J, Makita R, Uchijima Y, Kurihara Y, Nakagawa O, Asano T, Kurihara H (2006) Transcriptional activity of Pax3 is co-activated by TAZ. Biochem Biophys Res Commun 339:533–539
Di Palma T, D’Andrea B, Liguori GL, Liguoro A, de Cristofaro T, Del Prete D, Pappalardo A, Mascia A, Zannini M (2009) TAZ is a coactivator for Pax8 and TTF-1, two transcription factors involved in thyroid differentiation. Exp Cell Res 315:162–175
Jeong H, Bae S, An SY, Byun MR, Hwang JH, Yaffe MB, Hong JH, Hwang ES (2010) TAZ as a novel enhancer of MyoD-mediated myogenic differentiation. FASEB J 24:3310–3320
Hong JH, Hwang ES, McManus MT, Amsterdam A, Tian Y, Kalmukova R, Mueller E, Benjamin T, Spiegelman BM, Sharp PA, Hopkins N, Yaffe MB (2005) TAZ, a transcriptional modulator of mesenchymal stem cell differentiation. Science 309:1074–1078
Vitolo MI, Anglin IE, Mahoney WM, Renoud KJ, Gartenhaus RB, Bachman KE, Passaniti A (2007) The RUNX2 transcription factor cooperates with the YES-associated protein, YAP65, to promote cell transformation. Cancer Biol Ther 6:856–863
Zhao R, Fallon TR, Saladi SV, Pardo-Saganta A, Villoria J, Mou H, Vinarsky V, Gonzalez-Celeiro M, Nunna N, Hariri LP, Camargo F, Ellisen LW, Rajagopal J (2014) Yap tunes airway epithelial size and architecture by regulating the identity, maintenance, and self-renewal of stem cells. Dev Cell 30:151–165
Chen HI, Einbond A, Kwak SJ, Linn H, Koepf E, Peterson S, Kelly JW, Sudol M (1997) Characterization of the WW domain of human yes-associated protein and its polyproline-containing ligands. J Biol Chem 272:17070–17077
Chan SW, Lim CJ, Huang C, Chong YF, Gunaratne HJ, Hogue KA, Blackstock WP, Harvey KF, Hong W (2011) WW domain-mediated interaction with Wbp2 is important for the oncogenic property of TAZ. Oncogene 30:600–610
Zhang X, Milton CC, Poon CL, Hong W, Harvey KF (2011) Wbp2 cooperates with Yorkie to drive tissue growth downstream of the Salvador-Warts-Hippo pathway. Cell Death Differ 18:1346–1355
Kang HS, Beak JY, Kim YS, Herbert R, Jetten AM (2009) Glis3 is associated with primary cilia and Wwtr1/TAZ and implicated in polycystic kidney disease. Mol Cell Biol 29:2556–2569
Shao D, Zhai P, Del Re DP, Sciarretta S, Yabuta N, Nojima H, Lim DS, Pan D, Sadoshima J (2014) A functional interaction between Hippo-YAP signalling and FoxO1 mediates the oxidative stress response. Nat Commun 5:3315
Bendinelli P, Maroni P, Matteucci E, Luzzati A, Perrucchini G, Desiderio MA (2013) Hypoxia inducible factor-1 is activated by transcriptional co-activator with PDZ-binding motif (TAZ) versus WWdomain-containing oxidoreductase (WWOX) in hypoxic microenvironment of bone metastasis from breast cancer. Eur J Cancer 49:2608–2618
Chaulk SG, Lattanzi VJ, Hiemer SE, Fahlman RP, Varelas X (2014) The Hippo pathway effectors TAZ/YAP regulate dicer expression and microRNA biogenesis through Let-7. J Biol Chem 289:1886–1891
Mori M, Triboulet R, Mohseni M, Schlegelmilch K, Shrestha K, Camargo FD, Gregory RI (2014) Hippo signaling regulates microprocessor and links cell-density-dependent miRNA biogenesis to cancer. Cell 156:893–906
Aylon Y, Ofir-Rosenfeld Y, Yabuta N, Lapi E, Nojima H, Lu X, Oren M (2010) The Lats2 tumor suppressor augments p53-mediated apoptosis by promoting the nuclear proapoptotic function of ASPP1. Genes Dev 24:2420–2429
Tsutsumi R, Masoudi M, Takahashi A, Fujii Y, Hayashi T, Kikuchi I, Satou Y, Taira M, Hatakeyama M (2013) YAP and TAZ, Hippo signaling targets, act as a rheostat for nuclear SHP2 function. Dev Cell 26:658–665
Azzolin L, Panciera T, Soligo S, Enzo E, Bicciato S, Dupont S, Bresolin S, Frasson C, Basso G, Guzzardo V, Fassina A, Cordenonsi M, Piccolo S (2014) YAP/TAZ incorporation in the β-catenin destruction complex orchestrates the Wnt response. Cell 158(1):157–170
Varelas X, Miller BW, Sopko R, Song S, Gregorieff A, Fellouse FA, Sakuma R, Pawson T, Hunziker W, McNeill H, Wrana JL, Attisano L (2010) The Hippo pathway regulates Wnt/beta-catenin signaling. Dev Cell 18:579–591
Barry ER, Morikawa T, Butler BL, Shrestha K, de la Rosa R, Yan KS, Fuchs CS, Magness ST, Smits R, Ogino S, Kuo CJ, Camargo FD (2013) Restriction of intestinal stem cell expansion and the regenerative response by YAP. Nature 493:106–110
Imajo M, Miyatake K, Iimura A, Miyamoto A, Nishida E (2012) A molecular mechanism that links Hippo signalling to the inhibition of Wnt/β-catenin signalling. EMBO J 31:1109–1122
Camargo FD, Gokhale S, Johnnidis JB, Fu D, Bell GW, Jaenisch R, Brummelkamp TR (2007) YAP1 increases organ size and expands undifferentiated progenitor cells. Curr Biol 17:2054–2060
Heallen T, Zhang M, Wang J, Bonilla-Claudio M, Klysik E, Johnson RL, Martin JF (2011) Hippo pathway inhibits Wnt signaling to restrain cardiomyocyte proliferation and heart size. Science 332:458–461
Zhou D, Zhang Y, Wu H, Barry E, Yin Y, Lawrence E, Dawson D, Willis JE, Markowitz SD, Camargo FD, Avruch J (2011) Mst1 and Mst2 protein kinases restrain intestinal stem cell proliferation and colonic tumorigenesis by inhibition of Yes-associated protein (Yap) overabundance. Proc Natl Acad Sci USA 108:E1312–E1320
Cai J, Zhang N, Zheng Y, de Wilde RF, Maitra A, Pan D (2010) The Hippo signaling pathway restricts the oncogenic potential of an intestinal regeneration program. Genes Dev 24:2383–2388
Azzolin L, Zanconato F, Bresolin S, Forcato M, Basso G, Bicciato S, Cordenonsi M, Piccolo S (2012) Role of TAZ as mediator of Wnt signaling. Cell 151:1443–1456
Wang J, Park JS, Wei Y, Rajurkar M, Cotton JL, Fan Q, Lewis BC, Ji H, Mao J (2013) TRIB2 acts downstream of Wnt/TCF in liver cancer cells to regulate YAP and C/EBPα function. Mol Cell 51:211–225
Byun MR, Hwang JH, Kim AR, Kim KM, Hwang ES, Yaffe MB, Hong JH (2014) Canonical Wnt signalling activates TAZ through PP1A during osteogenic differentiation. Cell Death Differ 21:854–863
Fernandez-L A, Northcott PA, Dalton J, Fraga C, Ellison D, Angers S, Taylor MD, Kenney AM (2009) YAP1 is amplified and up-regulated in hedgehog-associated medulloblastomas and mediates Sonic hedgehog-driven neural precursor proliferation. Genes Dev 23:2729–2741
Lin YT, Ding JY, Li MY, Yeh TS, Wang TW, Yu JY (2012) YAP regulates neuronal differentiation through Sonic hedgehog signaling pathway. Exp Cell Res 318:1877–1888
Tschaharganeh DF, Chen X, Latzko P, Malz M, Gaida MM, Felix K, Ladu S, Singer S, Pinna F, Gretz N, Sticht C, Tomasi ML, Delogu S, Evert M, Fan B, Ribback S, Jiang L, Brozzetti S, Bergmann F, Dombrowski F, Schirmacher P, Calvisi DF, Breuhahn K (2013) Yes-associated protein up-regulates Jagged-1 and activates the Notch pathway in human hepatocellular carcinoma. Gastroenterology 144(1530–1542):e1512
Zhang J, Ji JY, Yu M, Overholtzer M, Smolen GA, Wang R, Brugge JS, Dyson NJ, Haber DA (2009) YAP-dependent induction of amphiregulin identifies a non-cell-autonomous component of the Hippo pathway. Nat Cell Biol 11:1444–1450
Yang N, Morrison CD, Liu P, Miecznikowski J, Bshara W, Han S, Zhu Q, Omilian AR, Li X, Zhang J (2012) TAZ induces growth factor-independent proliferation through activation of EGFR ligand amphiregulin. Cell Cycle 11:2922–2930
Ding L, Ellis MJ, Li S, Larson DE, Chen K, Wallis JW, Harris CC, McLellan MD, Fulton RS, Fulton LL, Abbott RM, Hoog J, Dooling DJ, Koboldt DC, Schmidt H, Kalicki J, Zhang Q, Chen L, Lin L, Wendl MC, McMichael JF, Magrini VJ, Cook L, McGrath SD, Vickery TL, Appelbaum E, Deschryver K, Davies S, Guintoli T, Crowder R, Tao Y, Snider JE, Smith SM, Dukes AF, Sanderson GE, Pohl CS, Delehaunty KD, Fronick CC, Pape KA, Reed JS, Robinson JS, Hodges JS, Schierding W, Dees ND, Shen D, Locke DP, Wiechert ME, Eldred JM, Peck JB, Oberkfell BJ, Lolofie JT, Du F, Hawkins AE, O’Laughlin MD, Bernard KE, Cunningham M, Elliott G, Mason MD, Thompson DM, Ivanovich JL, Goodfellow PJ, Perou CM, Weinstock GM, Aft R, Watson M, Ley TJ, Wilson RK, Mardis ER (2010) Genome remodelling in a basal-like breast cancer metastasis and xenograft. Nature 464:999–1005
Williamson KA, Rainger J, Floyd JA, Ansari M, Meynert A, Aldridge KV, Rainger JK, Anderson CA, Moore AT, Hurles ME, Clarke A, van Heyningen V, Verloes A, Taylor, Wilkie AO, Fitzpatrick, Consortium UK (2014) Heterozygous loss-of-function mutations in YAP1 cause both isolated and syndromic optic fissure closure defects. Am J Hum Genet 94:295–302
Errani C, Zhang L, Sung YS, Hajdu M, Singer S, Maki RG, Healey JH, Antonescu CR (2011) A novel WWTR1-CAMTA1 gene fusion is a consistent abnormality in epithelioid hemangioendothelioma of different anatomic sites. Genes Chromosomes Cancer 50:644–653
Antonescu CR, Le Loarer F, Mosquera JM, Sboner A, Zhang L, Chen CL, Chen HW, Pathan N, Krausz T, Dickson BC, Weinreb I, Rubin MA, Hameed M, Fletcher CD (2013) Novel YAP1-TFE3 fusion defines a distinct subset of epithelioid hemangioendothelioma. Genes Chromosomes Cancer 52:775–784
Zhao B, Kim J, Ye X, Lai ZC, Guan KL (2009) Both TEAD-binding and WW domains are required for the growth stimulation and oncogenic transformation activity of yes-associated protein. Cancer Res 69:1089–1098
Chan SW, Lim CJ, Loo LS, Chong YF, Huang C, Hong W (2009) TEADs mediate nuclear retention of TAZ to promote oncogenic transformation. J Biol Chem 284:14347–14358
Zhao B, Ye X, Yu J, Li L, Li W, Li S, Lin JD, Wang CY, Chinnaiyan AM, Lai ZC, Guan KL (2008) TEAD mediates YAP-dependent gene induction and growth control. Genes Dev 22:1962–1971
Lamar JM, Stern P, Liu H, Schindler JW, Jiang ZG, Hynes RO (2012) The Hippo pathway target, YAP, promotes metastasis through its TEAD-interaction domain. Proc Natl Acad Sci USA 109:E2441–E2450
Kapoor A, Yao W, Ying H, Hua S, Liewen A, Wang Q, Zhong Y, Wu CJ, Sadanandam A, Hu B, Chang Q, Chu GC, Al-Khalil R, Jiang S, Xia H, Fletcher-Sananikone E, Lim C, Horwitz GI, Viale A, Pettazzoni P, Sanchez N, Wang H, Protopopov A, Zhang J, Heffernan T, Johnson RL, Chin L, Wang YA, Draetta G, DePinho RA (2014) Yap1 activation enables bypass of oncogenic kras addiction in pancreatic cancer. Cell 158(1):185–197
Shao DD, Xue W, Krall EB, Bhutkar A, Piccioni F, Wang X, Schinzel AC, Sood S, Rosenbluh J, Kim JW, Zwang Y, Roberts TM, Root DE, Jacks T, Hahn WC (2014) KRAS and YAP1 converge to regulate EMT and tumor survival. Cell 158(1):171–184
Zhang H, Liu CY, Zha ZY, Zhao B, Yao J, Zhao S, Xiong Y, Lei QY, Guan KL (2009) TEAD transcription factors mediate the function of TAZ in cell growth and epithelial-mesenchymal transition. J Biol Chem 284:13355–13362
Lai D, Ho KC, Hao Y, Yang X (2011) Taxol resistance in breast cancer cells is mediated by the hippo pathway component TAZ and its downstream transcriptional targets Cyr61 and CTGF. Cancer Res 71:2728–2738
Zhang W, Nandakumar N, Shi Y, Manzano M, Smith A, Graham G, Gupta S, Vietsch EE, Laughlin SZ, Wadhwa M, Chetram M, Joshi M, Wang F, Kallakury B, Toretsky J, Wellstein A, Yi C (2014) Downstream of mutant KRAS, the transcription regulator YAP is essential for neoplastic progression to pancreatic ductal adenocarcinoma. Sci Signal 7:ra42
Xu MZ, Chan SW, Liu AM, Wong KF, Fan ST, Chen J, Poon RT, Zender L, Lowe SW, Hong W, Luk JM (2011) AXL receptor kinase is a mediator of YAP-dependent oncogenic functions in hepatocellular carcinoma. Oncogene 30:1229–1240
Tumaneng K, Schlegelmilch K, Russell RC, Yimlamai D, Basnet H, Mahadevan N, Fitamant J, Bardeesy N, Camargo FD, Guan KL (2012) YAP mediates crosstalk between the Hippo and PI(3)K–TOR pathways by suppressing PTEN via miR-29. Nat Cell Biol 14:1322–1329
Song S, Ajani JA, Honjo S, Maru DM, Chen Q, Scott AW, Heallen TR, Xiao L, Hofstetter WL, Weston B, Lee JH, Wadhwa R, Sudo K, Stroehlein JR, Martin JF, Hung MC, Johnson RL (2014) Hippo coactivator YAP1 upregulates SOX9 and endows stem-like properties to esophageal cancer cells. Cancer Res 74(15):4170–4182
Bhat KP, Salazar KL, Balasubramaniyan V, Wani K, Heathcock L, Hollingsworth F, James JD, Gumin J, Diefes KL, Kim SH, Turski A, Azodi Y, Yang Y, Doucette T, Colman H, Sulman EP, Lang FF, Rao G, Copray S, Vaillant BD, Aldape KD (2011) The transcriptional coactivator TAZ regulates mesenchymal differentiation in malignant glioma. Genes Dev 25:2594–2609
Liu-Chittenden Y, Huang B, Shim JS, Chen Q, Lee SJ, Anders RA, Liu JO, Pan D (2012) Genetic and pharmacological disruption of the TEAD-YAP complex suppresses the oncogenic activity of YAP. Genes Dev 26:1300–1305
Mani SA, Guo W, Liao MJ, Eaton EN, Ayyanan A, Zhou AY, Brooks M, Reinhard F, Zhang CC, Shipitsin M, Campbell LL, Polyak K, Brisken C, Yang J, Weinberg RA (2008) The epithelial-mesenchymal transition generates cells with properties of stem cells. Cell 133:704–715
Cordenonsi M, Zanconato F, Azzolin L, Forcato M, Rosato A, Frasson C, Inui M, Montagner M, Parenti AR, Poletti A, Daidone MG, Dupont S, Basso G, Bicciato S, Piccolo S (2011) The Hippo transducer TAZ confers cancer stem cell-related traits on breast cancer cells. Cell 147:759–772
Ganem NJ, Cornils H, Chiu SY, O’Rourke KP, Arnaud J, Yimlamai D, Théry M, Camargo FD, Pellman D (2014) Cytokinesis failure triggers hippo tumor suppressor pathway activation. Cell 158:833–848
Yuan M, Tomlinson V, Lara R, Holliday D, Chelala C, Harada T, Gangeswaran R, Manson-Bishop C, Smith P, Danovi SA, Pardo O, Crook T, Mein CA, Lemoine NR, Jones LJ, Basu S (2008) Yes-associated protein (YAP) functions as a tumor suppressor in breast. Cell Death Differ 15:1752–1759
Ehsanian R, Brown M, Lu H, Yang XP, Pattatheyil A, Yan B, Duggal P, Chuang R, Doondeea J, Feller S, Sudol M, Chen Z, Van Waes C (2010) YAP dysregulation by phosphorylation or ΔNp63-mediated gene repression promotes proliferation, survival and migration in head and neck cancer subsets. Oncogene 29:6160–6171
Cottini F, Hideshima T, Xu C, Sattler M, Dori M, Agnelli L, Ten Hacken E, Bertilaccio MT, Antonini E, Neri A, Ponzoni M, Marcatti M, Richardson PG, Carrasco R, Kimmelman AC, Wong KK, Caligaris-Cappio F, Blandino G, Kuehl WM, Anderson KC, Tonon G (2014) Rescue of Hippo coactivator YAP1 triggers DNA damage-induced apoptosis in hematological cancers. Nat Med 20:599–606
Morin-Kensicki EM, Boone BN, Howell M, Stonebraker JR, Teed J, Alb JG, Magnuson TR, O’Neal W, Milgram SL (2006) Defects in yolk sac vasculogenesis, chorioallantoic fusion, and embryonic axis elongation in mice with targeted disruption of Yap65. Mol Cell Biol 26:77–87
Kaneko KJ, DePamphilis ML (1998) Regulation of gene expression at the beginning of mammalian development and the TEAD family of transcription factors. Dev Genet 22:43–55
Yagi R, Kohn MJ, Karavanova I, Kaneko KJ, Vullhorst D, DePamphilis ML, Buonanno A (2007) Transcription factor TEAD4 specifies the trophectoderm lineage at the beginning of mammalian development. Development 134:3827–3836
Ota M, Sasaki H (2008) Mammalian Tead proteins regulate cell proliferation and contact inhibition as transcriptional mediators of Hippo signaling. Development 135:4059–4069
Nishioka N, Inoue K, Adachi K, Kiyonari H, Ota M, Ralston A, Yabuta N, Hirahara S, Stephenson RO, Ogonuki N, Makita R, Kurihara H, Morin-Kensicki EM, Nojima H, Rossant J, Nakao K, Niwa H, Sasaki H (2009) The Hippo signaling pathway components Lats and Yap pattern Tead4 activity to distinguish mouse trophectoderm from inner cell mass. Dev Cell 16:398–410
Hirate Y, Hirahara S, Inoue K, Suzuki A, Alarcon VB, Akimoto K, Hirai T, Hara T, Adachi M, Chida K, Ohno S, Marikawa Y, Nakao K, Shimono A, Sasaki H (2013) Polarity-dependent distribution of angiomotin localizes Hippo signaling in preimplantation embryos. Curr Biol 23:1181–1194
Cockburn K, Biechele S, Garner J, Rossant J (2013) The Hippo pathway member Nf2 is required for inner cell mass specification. Curr Biol 23:1195–1201
Lorthongpanich C, Messerschmidt DM, Chan SW, Hong W, Knowles BB, Solter D (2013) Temporal reduction of LATS kinases in the early preimplantation embryo prevents ICM lineage differentiation. Genes Dev 27:1441–1446
Lian I, Kim J, Okazawa H, Zhao J, Zhao B, Yu J, Chinnaiyan A, Israel MA, Goldstein LS, Abujarour R, Ding S, Guan KL (2010) The role of YAP transcription coactivator in regulating stem cell self-renewal and differentiation. Genes Dev 24:1106–1118
Beyer TA, Weiss A, Khomchuk Y, Huang K, Ogunjimi AA, Varelas X, Wrana JL (2013) Switch enhancers interpret TGF-β and Hippo signaling to control cell fate in human embryonic stem cells. Cell Rep 5:1611–1624
Qin H, Blaschke K, Wei G, Ohi Y, Blouin L, Qi Z, Yu J, Yeh RF, Hebrok M, Ramalho-Santos M (2012) Transcriptional analysis of pluripotency reveals the Hippo pathway as a barrier to reprogramming. Hum Mol Genet 21:2054–2067
Allen HF, Wade PA, Kutateladze TG (2013) The NuRD architecture. Cell Mol Life Sci 70:3513–3524
Xin M, Kim Y, Sutherland LB, Murakami M, Qi X, McAnally J, Porrello ER, Mahmoud AI, Tan W, Shelton JM, Richardson JA, Sadek HA, Bassel-Duby R, Olson EN (2013) Hippo pathway effector Yap promotes cardiac regeneration. Proc Natl Acad Sci USA 110:13839–13844
Gao T, Zhou D, Yang C, Singh T, Penzo-Méndez A, Maddipati R, Tzatsos A, Bardeesy N, Avruch J, Stanger BZ (2013) Hippo signaling regulates differentiation and maintenance in the exocrine pancreas. Gastroenterology 144:1543–1553
George NM, Day CE, Boerner BP, Johnson RL, Sarvetnick NE (2012) Hippo signaling regulates pancreas development through inactivation of Yap. Mol Cell Biol 32:5116–5128
Dong J, Feldmann G, Huang J, Wu S, Zhang N, Comerford SA, Gayyed MF, Anders RA, Maitra A, Pan D (2007) Elucidation of a universal size-control mechanism in Drosophila and mammals. Cell 130:1120–1133
Lee KP, Lee JH, Kim TS, Kim TH, Park HD, Byun JS, Kim MC, Jeong WI, Calvisi DF, Kim JM, Lim DS (2010) The Hippo-Salvador pathway restrains hepatic oval cell proliferation, liver size, and liver tumorigenesis. Proc Natl Acad Sci USA 107:8248–8253
Lu L, Li Y, Kim SM, Bossuyt W, Liu P, Qiu Q, Wang Y, Halder G, Finegold MJ, Lee JS, Johnson RL (2010) Hippo signaling is a potent in vivo growth and tumor suppressor pathway in the mammalian liver. Proc Natl Acad Sci USA 107:1437–1442
Zhou D, Conrad C, Xia F, Park JS, Payer B, Yin Y, Lauwers GY, Thasler W, Lee JT, Avruch J, Bardeesy N (2009) Mst1 and Mst2 maintain hepatocyte quiescence and suppress hepatocellular carcinoma development through inactivation of the Yap1 oncogene. Cancer Cell 16:425–438
Bai H, Zhang N, Xu Y, Chen Q, Khan M, Potter JJ, Nayar SK, Cornish T, Alpini G, Bronk S, Pan D, Anders RA (2012) Yes-associated protein regulates the hepatic response after bile duct ligation. Hepatology 56:1097–1107
Grijalva J, Huizenga M, Mueller K, Rodriguez S, Brazzo J, Camargo F, Sadri-Vakili G, Vakili K (2014) Dynamic alterations in Hippo signaling pathway and YAP activation during liver regeneration. Am J Physiol Gastrointest Liver Physiol 307(2):G196–204
Yimlamai D, Christodoulou C, Galli GG, Yanger K, Pepe-Mooney B, Gurung B, Shrestha K, Cahan P, Stanger BZ, Camargo FD (2014) Hippo pathway activity influences liver cell fate. Cell 157:1324–1338
Matsui Y, Nakano N, Shao D, Gao S, Luo W, Hong C, Zhai P, Holle E, Yu X, Yabuta N, Tao W, Wagner T, Nojima H, Sadoshima J (2008) Lats2 is a negative regulator of myocyte size in the heart. Circ Res 103:1309–1318
von Gise A, Lin Z, Schlegelmilch K, Honor LB, Pan GM, Buck JN, Ma Q, Ishiwata T, Zhou B, Camargo FD, Pu WT (2012) YAP1, the nuclear target of Hippo signaling, stimulates heart growth through cardiomyocyte proliferation but not hypertrophy. Proc Natl Acad Sci USA 109:2394–2399
Del Re DP, Matsuda T, Zhai P, Gao S, Clark GJ, Van Der Weyden L, Sadoshima J (2010) Proapoptotic Rassf1A/Mst1 signaling in cardiac fibroblasts is protective against pressure overload in mice. J Clin Invest 120:3555–3567
Lin Z, von Gise A, Zhou P, Gu F, Ma Q, Jiang J, Yau AL, Buck JN, Gouin KA, van Gorp PR, Zhou B, Chen J, Seidman JG, Wang DZ, Pu WT (2014) Cardiac-specific YAP activation improves cardiac function and survival in an experimental murine myocardial infarction model. Circ Res 115(3):354–363
Xin M, Kim Y, Sutherland LB, Qi X, McAnally J, Schwartz RJ, Richardson JA, Bassel-Duby R, Olson EN (2011) Regulation of insulin-like growth factor signaling by Yap governs cardiomyocyte proliferation and embryonic heart size. Sci Signal 4:ra70
Chen SN, Gurha P, Lombardi R, Ruggiero A, Willerson JT, Marian AJ (2014) The Hippo pathway is activated and is a causal mechanism for adipogenesis in arrhythmogenic cardiomyopathy. Circ Res 114(3):454–468
Zhang H, Pasolli HA, Fuchs E (2011) Yes-associated protein (YAP) transcriptional coactivator functions in balancing growth and differentiation in skin. Proc Natl Acad Sci USA 108:2270–2275
Beverdam A, Claxton C, Zhang X, James G, Harvey KF, Key B (2013) Yap controls stem/progenitor cell proliferation in the mouse postnatal epidermis. J Invest Dermatol 133:1497–1505
Lee MJ, Ran Byun M, Furutani-Seiki M, Hong JH, Jung HS (2014) YAP and TAZ regulate skin wound healing. J Invest Dermatol 134:518–525
Cao X, Pfaff SL, Gage FH (2008) YAP regulates neural progenitor cell number via the TEA domain transcription factor. Genes Dev 22:3320–3334
Lavado A, He Y, Paré J, Neale G, Olson EN, Giovannini M, Cao X (2013) Tumor suppressor Nf2 limits expansion of the neural progenitor pool by inhibiting Yap/Taz transcriptional coactivators. Development 140:3323–3334
Li N, Lim G, Chen L, McCabe MF, Kim H, Zhang S, Mao J (2013) Spinal expression of Hippo signaling components YAP and TAZ following peripheral nerve injury in rats. Brain Res 1535:137–147
Byun MR, Jeong H, Bae SJ, Kim AR, Hwang ES, Hong JH (2012) TAZ is required for the osteogenic and anti-adipogenic activities of kaempferol. Bone 50:364–372
An Y, Kang Q, Zhao Y, Hu X, Li N (2013) Lats2 modulates adipocyte proliferation and differentiation via hippo signaling. PLoS ONE 8:e72042
Jang EJ, Jeong H, Kang JO, Kim NJ, Kim MS, Choi SH, Yoo SE, Hong JH, Bae MA, Hwang ES (2012) TM-25659 enhances osteogenic differentiation and suppresses adipogenic differentiation by modulating the transcriptional co-activator TAZ. Br J Pharmacol 165:1584–1594
Ribas R, Moncaut N, Siligan C, Taylor K, Cross JW, Rigby PW, Carvajal JJ (2011) Members of the TEAD family of transcription factors regulate the expression of Myf5 in ventral somitic compartments. Dev Biol 355:372–380
Benhaddou A, Keime C, Ye T, Morlon A, Michel I, Jost B, Mengus G, Davidson I (2012) Transcription factor TEAD4 regulates expression of myogenin and the unfolded protein response genes during C2C12 cell differentiation. Cell Death Differ 19:220–231
Milewski RC, Chi NC, Li J, Brown C, Lu MM, Epstein JA (2004) Identification of minimal enhancer elements sufficient for Pax3 expression in neural crest and implication of Tead2 as a regulator of Pax3. Development 131:829–837
Watt KI, Judson R, Medlow P, Reid K, Kurth TB, Burniston JG, Ratkevicius A, De Bari C, Wackerhage H (2010) Yap is a novel regulator of C2C12 myogenesis. Biochem Biophys Res Commun 393:619–624
Judson RN, Tremblay AM, Knopp P, White RB, Urcia R, De Bari C, Zammit PS, Camargo FD, Wackerhage H (2012) The Hippo pathway member Yap plays a key role in influencing fate decisions in muscle satellite cells. J Cell Sci 125:6009–6019
Judson RN, Gray SR, Walker C, Carroll AM, Itzstein C, Lionikas A, Zammit PS, De Bari C, Wackerhage H (2013) Constitutive expression of Yes-associated protein (Yap) in adult skeletal muscle fibres induces muscle atrophy and myopathy. PLoS ONE 8:e59622
Bertrand AT, Ziaei S, Ehret C, Duchemin H, Mamchaoui K, Bigot A, Mayer M, Quijano-Roy S, Desguerre I, Lainé J, Ben Yaou R, Bonne G, Coirault C (2014) Cellular microenvironments reveal defective mechanosensing responses and elevated YAP signaling in LMNA-mutated muscle precursors. J Cell Sci 127:2873–2884
Yang Z, Nakagawa K, Sarkar A, Maruyama J, Iwasa H, Bao Y, Ishigami-Yuasa M, Ito S, Kagechika H, Hata S, Nishina H, Abe S, Kitagawa M, Hata Y (2014) Screening with a novel cell-based assay for TAZ activators identifies a compound that enhances myogenesis in C2C12 cells and facilitates muscle repair in a muscle injury model. Mol Cell Biol 34:1607–1621
Park GH, Jeong H, Jeong MG, Jang EJ, Bae MA, Lee YL, Kim NJ, Hong JH, Hwang ES (2014) Novel TAZ modulators enhance myogenic differentiation and muscle regeneration. Br J Pharmacol 171(17):4051–4061
Enger TB, Samad-Zadeh A, Bouchie MP, Skarstein K, Galtung HK, Mera T, Walker J, Menko AS, Varelas X, Faustman DL, Jensen JL, Kukuruzinska MA (2013) The Hippo signaling pathway is required for salivary gland development and its dysregulation is associated with Sjogren’s syndrome. Lab Invest 93:1203–1218
Kawamura K, Cheng Y, Suzuki N, Deguchi M, Sato Y, Takae S, Ho CH, Kawamura N, Tamura M, Hashimoto S, Sugishita Y, Morimoto Y, Hosoi Y, Yoshioka N, Ishizuka B, Hsueh AJ (2013) Hippo signaling disruption and Akt stimulation of ovarian follicles for infertility treatment. Proc Natl Acad Sci USA 110:17474–17479
Kwon Y, Vinayagam A, Sun X, Dephoure N, Gygi SP, Hong P, Perrimon N (2013) The Hippo signaling pathway interactome. Science 342:737–740
Wang W, Li X, Huang J, Feng L, Dolinta KG, Chen J (2014) Defining the protein-protein interaction network of the human hippo pathway. Mol Cell Proteomics 13:119–131
Couzens AL, Knight JD, Kean MJ, Teo G, Weiss A, Dunham WH, Lin ZY, Bagshaw RD, Sicheri F, Pawson T, Wrana JL, Choi H, Gingras AC (2013) Protein interaction network of the Mammalian hippo pathway reveals mechanisms of kinase-phosphatase interactions. Sci Signal 6:rs15
Hauri S, Wepf A, van Drogen A, Varjosalo M, Tapon N, Aebersold R, Gstaiger M (2013) Interaction proteome of human Hippo signaling: modular control of the co-activator YAP1. Mol Syst Biol 9:713
Kohli P, Bartram MP, Habbig S, Pahmeyer C, Lamkemeyer T, Benzing T, Schermer B, Rinschen MM (2014) Label-free quantitative proteomic analysis of the YAP/TAZ interactome. Am J Physiol Cell Physiol 306:C805–C818
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kodaka, M., Hata, Y. The mammalian Hippo pathway: regulation and function of YAP1 and TAZ. Cell. Mol. Life Sci. 72, 285–306 (2015). https://doi.org/10.1007/s00018-014-1742-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00018-014-1742-9