Abstract
There has recently been a 6 to 17% rise in candida species infections in the central nervous system. Although Candida can cause infections in both immunocompetent and immunosuppressed individuals, disseminated candidiasis is mostly seen in patients with impaired immunity due to AIDS, diabetes, neutropenia, underlying malignancy, and extensive wounds (burns and operations). Patients with disseminated candidiasis or with any neurosurgical procedure like ventricular shunts are observed with central nervous system (CNS) involvement. Another high-risk group for invasive candidiasis consists of newborns and infants, particularly those with low birth weight (<1.5 kg). Candida crosses the blood–brain barriers by three proposed mechanisms namely the Trojan horse mechanism, paracellular migration, and transcellular migration. Clinical manifestations of neuro-candidiasis are usually variable; however, meningoencephalitis is the most common. Invasive candidiasis mortality is thought to vary from 10 to 70%, rising to 90% in cases when the central nervous system is affected. Analysis of cerebral spinal fluid plus cultures exhibiting growth of budding, yeast-like cells, is used to make laboratory-based diagnoses. The positive serum beta-D-glucan assay aids in the diagnosis but may be positive in patients with various other invasive fungal infections. Liposomal amphotericin B with better CNS concentrations followed by fluconazole as a step-down therapy is considered an effective treatment strategy.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Pathogen
Candida neurological infections are almost always due to C. albicans (Sánchez et al. 2000). However, the world has seen a gradual rise in the frequency of non-C. albicans species over Candida albicans over the past decade (Table 12.1). Candida infects both immunocompetent and immunosuppressed individuals but disseminated disease mostly occurs in the latter (Cesaro et al. 2017). A remarkable surge from 6 to 17% has been noted in the incidence of CNS infection from Candida spp. (Brumble et al. 2017). Candida albicans was the cause of 33% of CNS infections among individuals with underlying malignant illnesses or among those with hematopoietic stem cell transplantations. Non-Candida albicans, however, accounted for 77% of neuro-infections in such patients; the most common strain found was C. parapsilosis, while isolates of Candida glabrata, guilliermondii, krusei, and tropicalis were also found occasionally. Additionally, multispecies involvements were also reported (Cesaro et al. 2017; McCullers et al. 2000; Murthy and Sundaram 2014).
2 Pathogenesis
Although the exact pathogenic mechanisms involved in certain neuro-mycological infections are not entirely known, it is a well-established fact that the fungi must first get past the host defenses in cross the blood–brain barrier (BBB) in order to commence CNS infection. The fungi adhere to the microvasculature of the brain, after which transmigration happens into the brain parenchyma. Trojan horse mechanism, transcellular migration, and paracellular migration are the three mechanisms proposed for crossing the BBB by the fungus (Liu et al. 2011). The building block of BBB is the brain endothelial cells connected with tight junctions; foot process of astrocytes surrounds these cells maintaining its integrity. Fibronectin, vitronectin, and laminin facilitate adhesion of C. albicans to the extracellular matrix. Als3 (agglutinin-like sequence 3) and Ssa1 (stress seventy subfamily A 1) are the fungal invasins that mediate invasion of brain endothelial cells by C. albicans (Shi and Mody 2016). Als3’s affinity for the heat shock protein 96 (gp96), which is expressed on endothelial cells that line the cerebral vessels, promotes the transcytosis of Candida albicans. C. albicans gets engulfed by the phagocyte in the peripheral blood circulation from where the Trojan horse pathway begins. The fungus inside the phagocyte maneuvers its movement toward the brain, where it adheres on the luminal side of the brain capillaries finally crossing the BBB transcellularly and paracellularly (Koutsouras et al. 2016; Liu et al. 2011; Santiago-Tirado and Doering 2017).
Factors that facilitate the penetration of fungi across the blood–brain barrier are downregulation of immunity by various immunosuppressant conditions which lead to increased permeability of the BBB, direct disruption of the BBB by any neurosurgical procedure, colonization of the foreign devices placed in the ventricles of the brain, or activation of microglia and cytokines: Tumor necrosis factor alpha (TNF-α) disrupts the tight junctions of the barrier. After the crossing of the BBB, cerebral and subarachnoid space proliferation of the fungus in the brain parenchyma causes inflammation. Invasion of the brain tissue/meninges by the fungal pathogen after surpassing all the effective barriers surrounding the brain facilitated by the immunosuppressive conditions occurs; subsequently, there is release of immune-enhancing and immune-suppressing chemokines and cytokines by the activated nerve cells occurs. The interplay between these cytokines and chemokines determines the pathogenesis of fungal CNS infections (Koutsouras et al. 2016; Sharma et al. 2012).
The rate and severity of neuro-infection are determined by the fungus’ pathogenicity and the host’s immunological responsiveness (Koutsouras et al. 2016). Host immune defense against the pathogen in the CNS comprises microglia, endothelial cells, astrocytes, and T cells. They inhibit the fungal infection, thereby limiting the infection by interferon-γ, interleukin (IL)1β, IL6, IL12, TNF-α (i.e., chemokines) production, nitric oxide generation, superoxide anion production, major histocompatibility complex class I (MHC I), and MHC II molecular expression (Koutsouras et al. 2016; Sharma et al. 2012). In invasive cerebral candidiasis, microglial cells are the principle effector cells, and it has been reported that on intracerebral administration; it can limit infection and tissue damage (Blasi et al. 1991; Lionakis et al. 2011). Disruption of tight junction of BBB by cytokine such as TNF-α released by microglial activation has been noted The toll-like receptors (TLR) 2, 4, and 9 are able to identify fungal antigens, including C. albicans’ pseudohyphae. TLR-2, Dectin-1, and CR-3 all recognize mannose and β-glucans, which are present on the surface of C. albicans, as well as on Aspergillus fumigatus, respectively (Koutsouras et al. 2016). The ability of microglia to generate pro-inflammatory cytokines when exposed to the pathogen, however, may be diminished by these carbohydrates attenuating TLR-mediated NF-κB activation (Shah et al. 2009). Candida spp. produces biofilm which is protective, as it helps to evade the host defense such as phagocytosis, cytokines, and nitric oxide by microglial cells (Koutsouras et al. 2016).
Numerous single-nucleotide polymorphisms, known as SNPs, in immune-associated genes, appear to be linked to an increased vulnerability to invasive candidiasis. Independent risk factor for the development of systemic risk factor was homozygosity for the dysfunctional CX3CR1-M280 allele that resulted in dysfunctional monocyte signaling and survival (Collar et al. 2018; Lionakis et al. 2013). Additional variables that are linked to an increased likelihood of invasive yeast infections include a malfunctioning CXCR1-T276 allele, which impairs degranulation of neutrophils, SNPs inCD58, TAGAP genes, LCE4A-C1orf68 locus, and also SNP mutations in mannose-binding lectin genes. Nevertheless, not all of the aforementioned variables particularly raise the likelihood of candidiasis of the central nervous system (Kumar et al. 2014; Swamydas et al. 2016; van Till et al. 2008). The molecule whose deficiency leads to profound susceptibility to neuro-candidiasis is CARD9, a myeloid-expressed signaling adaptor protein (Lionakis et al. 2017). These conclusions are supported by numerous cases that authors have described (Drewniak et al. 2013; Gavino et al. 2014; Glocker et al. 2009; Herbst et al. 2015; Jones et al. 2016).
3 Pathology, Risk Factors, and Clinical Manifestations of Neuro-Candidiasis
Primary candidiasis of central nervous system although uncommon is reported to be around 18–52% of disseminated candidiasis (Jain et al. 2007). Susceptibility rate further increases in neonates, where 66% of the newborns with disseminated candidiasis and 80% with Candida endocarditis have CNS involvement (Drummond and Lionakis 2018; Góralska et al. 2018). Unrecognized infection of CNS has been estimated in 6% of patients with disseminated candidiasis (Shankar et al. 2007). Risk factors for CNS invasion by Candida (Table 12.2) include neonates [LBW/premature] or recent neurosurgery, patients with CNS shunts or catheters, other devices, neutropenia associated with AIDS/diabetes/hematological malignancies/extensive wounds like burns, prolonged use of steroids in high doses, and graft vs. host disease after bone marrow transplantation (Barton et al. 2014).
Candida has predilection for microcirculation particularly in the middle cerebral artery facilitated by its small size results in multiple cerebral microabscesses and leptomeningitis; however, it can also cause aneurysms and thrombosis of microvessels, cerebral vasculitis, and intracerebral or subarachnoid hemorrhage (Sánchez et al. 2000). Primary focus of infection in disseminated candidiasis is mostly lung/respiratory system or gastrointestinal system [GIT] from where it spreads (Kullberg and Arendrup 2015). Dissemination is favored either when impairment of immune system in conditions like AIDS, newborns, organ transplants, hematological malignancies, prolonged corticosteroids therapy, or after interventions like neurosurgical procedures, placement of shunts, catheters surgery (Barton et al. 2014; Cesaro et al. 2017; Katragkou et al. 2017; Kullberg and Arendrup 2015; Neves et al. 2014; O’Brien et al. 2011).
CNS candidiasis often has varied clinical presentations, meningoencephalitis being the most common others being meningitis, brain abscesses, and ventriculitis. Some more infrequent clinical presentation reported are endophthalmitis, intraventricular fungus balls, hydrocephalus, vasculitis, calcifications, cranial neuropathies, numerous cerebral abscesses accompanied by nodular enhancing lesions, or by ring enhancements, and stroke sequelae in a small number of cases (Huang et al. 1998; Katragkou et al. 2017; McCarthy et al. 2017; Pappas et al. 2016; Shankar et al. 2007).
The symptoms of Candida meningitis are neck rigidity, fever, and headache-altered mental status which are also similar to acute or chronic bacterial meningitis. However, signs and symptoms may be subtle in neonates and severely neutropenic/immunosuppressed individuals. Neonates particularly preterm neonates are considered a very high-risk group for developing invasive candidiasis and subsequently neuro-candidiasis. It is reported that 25% of newborn with birth weight < 1.5 kg develop systemic candidiasis and CNS invasion is seen in 50% of the neonates with disseminated candidiasis with a fatality rate of 70% (Baradkar et al. 2009; Faix and Chapman 2003; Lewis et al. 2015; Murthy and Sundaram 2014; Sánchez et al. 2000; Yoshida et al. 2022). Overall mortality from neuro-candidiasis varies between 10 and 30% (Sánchez et al. 2000). Disseminated candidiasis risk factors include certain surgical procedures, extended hospital stay, intubation (endotracheal), neonates with Apgar scores of below 5, parental lipids, prolonged catheterization, and total parental feeding (Lewis et al. 2015). Additionally, as a result the commensal Candida species’ receptive translocation from the GIT into the bloodstream during necrotizing enterocolitis of newborns is a significant determinant of subsequent disseminated candidiasis occurrence (Barton et al. 2014; Huang et al. 1998).
4 Diagnosis
Patients experiencing CNS manifestations involving any or all of the signs/symptoms listed below should have neurological candida infection suspected (Sánchez et al. 2000):
-
A Candida species isolated in the cerebrospinal fluid (CSF).
-
Candida isolation from a different, typically sterile location among patients with pleocytosis as detected by CSF biochemistries (Table 12.3). Finding Candida species in blood cultures is helpful, but candidemia may not be documented in patients with Candida meningitis.
-
Inadequate response to treatment for suspected mycobacterial or bacterial meningitis.
4.1 CSF Analysis
For establishing a confirmatory diagnosis of CNS candidiasis, obtaining CSF for analysis and culture by lumbar puncture is essential. Around 80% of cases reveal positive cultures. Regardless of whether other microorganisms are found, a positive cerebrospinal fluid culture should not be regarded as a contamination, especially in patients with compromised immunity (Sánchez et al. 2000).
The CSF findings are also variable in patients with neurosurgery-related Candida meningitis. Some have a neutrophilic pleocytosis similar to that seen in bacterial meningitis (Nguyen and Yu 1995), whereas others have a lymphocytic predominance (Sánchez et al. 2000).
Those with chronic meningitis have a harder time being diagnosed since there is only a minimal pathogen count, and the routine CSF cultures produce poorer results. In patients with chronic Candida meningitis, large-volume (10 to 20 mL) spinal taps are frequently necessary to collect enough CSF for culture. The microbiology laboratory should be asked to culture the entire sample or to filter the sample through a Millipore filter and culture the filter on appropriate media.
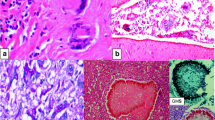
The cell wall of several fungi, notably Candida species, contains 1,3-beta-D-glucan (Fig. 12.1). Several commercial assays are available that detect serum beta-D-glucan. Positivity of the assays indicates toward an invasive fungal infection including invasive candidiasis. Importantly, this test can be positive in the setting of many different fungal infections, and cutoffs to define positivity in CSF are not defined. Test results must therefore be interpreted with caution.
Basic structure of Candida cell wall. (Image source: Frontiers in Microbiology: Volume 10 (Garcia-Rubio et al. 2020)—Copyright restrictions: none; this image is from an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) and thus free of any copyright restriction)
4.2 Neuroimaging
In central nervous system candidiasis, neuroradiological abnormalities are frequently nonspecific and are frequently mistaken for meningitis due to Mycobacterial tuberculosis, or are misinterpreted as CNS tumors, or pyogenic abscesses (Jain et al. 2007). Microabscesses found at the grey–white junction, cerebellum, and basal ganglia are the most frequent pathologic finding, followed by meningitis and macro-abscesses (Pendlebury et al. 1989; Sánchez et al. 2000). Computed tomography (CT) can detect hydrocephalus, which is particularly common in patients with infected CNS shunts (Chiou et al. 1994; Sánchez-Portocarrero et al. 1994). However, the CT scan is often normal and may not detect microabscesses (Pendlebury et al. 1989; Sánchez et al. 2000). In comparison, magnetic resonance imaging (MRI) can detect microabscesses, which appear as multiple, small, enhanced ring lesions, sometimes with a hemorrhagic component (Lai et al. 1997). MRI scans may be utilized to monitor the effectiveness of antifungal medications whenever these types of lesions are present.
5 Treatment
The most thoroughly researched medication for the medical management of neurological candidiasis is amphotericin B deoxycholate; however, optimal treatment evaluation through a randomized controlled trial is still lacking (Geers and Gordon 1999; Nguyen and Yu 1995; Pappas et al. 2016; Sánchez et al. 2000; Voice et al. 1994). In comparison to amphotericin B lipid complex, 5 mg/kg intravenously, daily, liposomal amphotericin B may produce higher CNS concentrations (Groll et al. 2000). After a positive response to lipid amphotericin B is achieved, either with or without flucytosine (5-FC), fluconazole is advised to serve as a step-down regimen. 5-FC is administered 4 times a day to individuals having normalized kidney functions, at an oral dosage of 25 mg/kg. Treatment ought to be maintained for several weeks to months till resolution of CNS manifestations, CSF anomalies, and radiological clearing has taken place. The specialists advise that contaminated ventricular devices be removed (Alothman et al. 2014).
In neonates, amphotericin B deoxycholate (1.0 mg/kg IV once daily) is the formulation used. Neonates tolerate the deoxycholate formulation better than adults, and there is little experience using the lipid formulations in this group (Fernandez et al. 2000; van den Anker et al. 1995). Flucytosine is not recommended because adverse effects are frequent in neonates (Benjamin et al. 2006).
5.1 Duration
Antifungal treatment ought to be continued till any abscess(es), if present at presentation, have cleared on MRI, the patient’s clinical symptoms/signs have disappeared, and CSF cell counts (pleocytosis), glucose levels, protein concentration, and CSF culture have normalized. The aforementioned steps could take weeks or months to complete, particularly in those suffering from chronic Candida meningitis.
There are no data available concerning the frequency of testing, but the following approach seems reasonable:
-
Repeat MRI scans for patients with brain abscesses are advised to be done after 2 weeks (or sooner if their condition is deteriorating) and then every month till the abscess clears up.
-
In order to confirm that all CSF alterations are reverting to normal as well as that CSF cultures will remain negative, lumbar punctures should be performed weekly during the initial few weeks, in acute meningitis cases.
-
For patients with chronic meningitis, lumbar puncture should be repeated as for acute meningitis. The best parameters to follow are the CSF white cell count and protein and glucose concentrations. A negative CSF culture is insufficient to assess treatment response since the microorganism exists in low quantities and routine CSF cultures of CSF provide poor yields (Voice et al. 1994).
Patients who have cerebral abscesses, are markedly immunocompromised, or have chronic Candida meningitis need longer courses of therapy, and patients who have infected ventricular shunts or implantable CNS devices must have the device removed to achieve cure for the infection (Chiou et al. 1994; Nguyen and Yu 1995; Pappas et al. 2016; Sánchez-Portocarrero et al. 1994).
If at all possible, infected CNS devices such as chemotherapy delivery biopolymer wafers, prosthetic reconstructive devices, shunts, stimulators, and ventriculostomy drains should be removed. In those with a ventricular device that is impractical to remove, amphotericin B deoxycholate may be injected directly into the ventricle via the device (Pappas et al. 2016).
Adjuvant immune therapies, particularly for CARD9-deficient individuals reported by some authors, are abnormalities in GM-CSF seen in myeloid cells with the p.Y91H CARD9 mutation, corrected by recombinant GM-CSF, and the use of GM-CSF therapy to rectify cytokine (IL-17) production errors in p.Q295X-mutant CARD9-deficient patients (Celmeli et al. 2016; Gavino et al. 2014, 2016).
References
Ahmad S, Alfouzan W (2021) Candida auris: epidemiology, diagnosis, pathogenesis, antifungal susceptibility, and infection control measures to combat the spread of infections in healthcare facilities. Microorganisms 9:807. https://doi.org/10.3390/microorganisms9040807
Alothman AF, Al-Musawi T, Al-Abdely HM, Salman JA, Almaslamani M, Yared N, Butt AA, Raghubir N, Morsi WE, Al Thaqafi AO (2014) Clinical practice guidelines for the management of invasive Candida infections in adults in the middle east region: expert panel recommendations. J Infect Public Health 7:6–19. https://doi.org/10.1016/j.jiph.2013.08.002
Badiee P, Alborzi A (2011) Susceptibility of clinical Candida species isolates to antifungal agents by E-test, southern Iran: a five year study. Iran J Microbiol 3:183–188
Baradkar V, Mathur M, Kumar S (2009) Cerebral CANDIDA abscess in an infant. Indian J Med Microbiol 27:70–72. https://doi.org/10.1016/S0255-0857(21)01762-X
Barton M, O’Brien K, Robinson JL, Davies DH, Simpson K, Asztalos E, Langley JM, Le Saux N, Sauve R, Synnes A, Tan B, de Repentigny L, Rubin E, Hui C, Kovacs L, Richardson SE (2014) Invasive candidiasis in low birth weight preterm infants: risk factors, clinical course and outcome in a prospective multicenter study of cases and their matched controls. BMC Infect Dis 14:327. https://doi.org/10.1186/1471-2334-14-327
Ben-Ami R, Berman J, Novikov A, Bash E, Shachor-Meyouhas Y, Zakin S, Maor Y, Tarabia J, Schechner V, Adler A, Finn T (2017) Multidrug-resistant Candida haemulonii and C. auris, Tel Aviv, Israel. Emerg Infect Dis 23:195–203. https://doi.org/10.3201/eid2302.161486
Benjamin DK, Stoll BJ, Fanaroff AA, McDonald SA, Oh W, Higgins RD, Duara S, Poole K, Laptook A, Goldberg R, National Institute of Child Health and Human Development Neonatal Research Network (2006) Neonatal candidiasis among extremely low birth weight infants: risk factors, mortality rates, and neurodevelopmental outcomes at 18 to 22 months. Pediatrics 117:84–92. https://doi.org/10.1542/peds.2004-2292
Blasi E, Mazzolla R, Barluzzi R, Mosci P, Bartoli A, Bistoni F (1991) Intracerebral transfer of an in vitro established microglial cell line: local induction of a protective state against lethal challenge with Candida albicans. J Neuroimmunol 32:249–257. https://doi.org/10.1016/0165-5728(91)90195-d
Brumble L, Reza M, Dhakal L, Cruz G, Abu Saleh O, Heckman M (2017) Fungal infections of the central nervous system: clinical, radiographic and laboratory manifestations. J Microbiol Exp 5:00167. https://doi.org/10.15406/jmen.2017.05.00167
Celmeli F, Oztoprak N, Turkkahraman D, Seyman D, Mutlu E, Frede N, Köksoy S, Grimbacher B (2016) Successful granulocyte colony-stimulating factor treatment of relapsing Candida albicans meningoencephalitis caused by CARD9 deficiency. Pediatr Infect Dis J 35:428–431. https://doi.org/10.1097/INF.0000000000001028
Cesaro S, Tridello G, Castagnola E, Calore E, Carraro F, Mariotti I, Colombini A, Perruccio K, Decembrino N, Russo G, Maximova N, Baretta V, Caselli D (2017) Retrospective study on the incidence and outcome of proven and probable invasive fungal infections in high-risk pediatric onco-hematological patients. Eur J Haematol 99:240–248. https://doi.org/10.1111/ejh.12910
Chiou CC, Wong TT, Lin HH, Hwang B, Tang RB, Wu KG, Lee BH (1994) Fungal infection of ventriculoperitoneal shunts in children. Clin Infect Dis 19:1049–1053. https://doi.org/10.1093/clinids/19.6.1049
Collar AL, Swamydas M, O’Hayre M, Sajib MS, Hoffman KW, Singh SP, Mourad A, Johnson MD, Ferre EMN, Farber JM, Lim JK, Mikelis CM, Gutkind JS, Lionakis MS (2018) The homozygous CX3CR1-M280 mutation impairs human monocyte survival. JCI Insight 3:e95417. https://doi.org/10.1172/jci.insight.95417
Drewniak A, Gazendam RP, Tool ATJ, van Houdt M, Jansen MH, van Hamme JL, van Leeuwen EMM, Roos D, Scalais E, de Beaufort C, Janssen H, van den Berg TK, Kuijpers TW (2013) Invasive fungal infection and impaired neutrophil killing in human CARD9 deficiency. Blood 121:2385–2392. https://doi.org/10.1182/blood-2012-08-450551
Drummond RA, Lionakis MS (2018) Candidiasis of the central nervous system in neonates and children with primary immunodeficiencies. Curr Fungal Infect Rep 12:92–97. https://doi.org/10.1007/s12281-018-0316-y
Egger NB, Kainz K, Schulze A, Bauer MA, Madeo F, Carmona-Gutierrez D (2022) The rise of Candida auris: from unique traits to co-infection potential. Microb Cell 9:141–144. https://doi.org/10.15698/mic2022.08.782
Faix RG, Chapman RL (2003) Central nervous system candidiasis in the high-risk neonate. Semin Perinatol 27:384–392. https://doi.org/10.1016/S0146-0005(03)00065-X
Fernandez M, Moylett EH, Noyola DE, Baker CJ (2000) Candidal meningitis in neonates: a 10-year review. Clin Infect Dis 31:458–463. https://doi.org/10.1086/313973
Garcia-Rubio R, de Oliveira HC, Rivera J, Trevijano-Contador N (2020) The fungal cell wall: Candida, cryptococcus, and aspergillus species. Front Microbiol 10:10
Gavino C, Cotter A, Lichtenstein D, Lejtenyi D, Fortin C, Legault C, Alirezaie N, Majewski J, Sheppard DC, Behr MA, Foulkes WD, Vinh DC (2014) CARD9 deficiency and spontaneous central nervous system candidiasis: complete clinical remission with GM-CSF therapy. Clin Infect Dis 59:81–84. https://doi.org/10.1093/cid/ciu215
Gavino C, Hamel N, Zeng JB, Legault C, Guiot M-C, Chankowsky J, Lejtenyi D, Lemire M, Alarie I, Dufresne S, Boursiquot J-N, McIntosh F, Langelier M, Behr MA, Sheppard DC, Foulkes WD, Vinh DC (2016) Impaired RASGRF1/ERK-mediated GM-CSF response characterizes CARD9 deficiency in French-Canadians. J Allergy Clin Immunol 137:1178–1188.e7. https://doi.org/10.1016/j.jaci.2015.09.016
Geers TA, Gordon SM (1999) Clinical significance of Candida species isolated from cerebrospinal fluid following neurosurgery. Clin Infect Dis 28:1139–1147. https://doi.org/10.1086/514755
Glocker E-O, Hennigs A, Nabavi M, Schäffer AA, Woellner C, Salzer U, Pfeifer D, Veelken H, Warnatz K, Tahami F, Jamal S, Manguiat A, Rezaei N, Amirzargar AA, Plebani A, Hannesschläger N, Gross O, Ruland J, Grimbacher B (2009) A homozygous CARD9 mutation in a family with susceptibility to fungal infections. N Engl J Med 361:1727–1735. https://doi.org/10.1056/NEJMoa0810719
Góralska K, Blaszkowska J, Dzikowiec M (2018) Neuroinfections caused by fungi. Infection 46:443–459. https://doi.org/10.1007/s15010-018-1152-2
Groll AH, Giri N, Petraitis V, Petraitiene R, Candelario M, Bacher JS, Piscitelli SC, Walsh TJ (2000) Comparative efficacy and distribution of lipid formulations of amphotericin B in experimental Candida albicans infection of the central nervous system. J Infect Dis 182:274–282. https://doi.org/10.1086/315643
Herbst M, Gazendam R, Reimnitz D, Sawalle-Belohradsky J, Groll A, Schlegel P-G, Belohradsky B, Renner E, Klepper J, Grimbacher B, Kuijpers T, Liese J (2015) Chronic Candida albicans meningitis in a 4-year-old girl with a homozygous mutation in the CARD9 gene (Q295X). Pediatr Infect Dis J 34:999–1002. https://doi.org/10.1097/INF.0000000000000736
Huang CC, Chen CY, Yang HB, Wang SM, Chang YC, Liu CC (1998) Central nervous system candidiasis in very low-birth-weight premature neonates and infants: US characteristics and histopathologic and MR imaging correlates in five patients. Radiology 209:49–56. https://doi.org/10.1148/radiology.209.1.9769811
Jain KK, Mittal SK, Kumar S, Gupta RK (2007) Imaging features of central nervous system fungal infections. Neurol India 55:241. https://doi.org/10.4103/0028-3886.35685
Jones N, Garcez T, Newman W, Denning D (2016) Endogenous Candida endophthalmitis and osteomyelitis associated with CARD9 deficiency. BMJ Case Rep 2016:bcr2015214117. https://doi.org/10.1136/bcr-2015-214117
Katragkou A, Fisher BT, Groll AH, Roilides E, Walsh TJ (2017) Diagnostic imaging and invasive fungal diseases in children. J Pediatr Infect Dis Soc 6:S22–S31. https://doi.org/10.1093/jpids/pix055
Koutsouras GW, Ramos RL, Martinez LR (2016) Role of microglia in fungal infections of the central nervous system. Virulence 8:705–718. https://doi.org/10.1080/21505594.2016.1261789
Kullberg BJ, Arendrup MC (2015) Invasive candidiasis. N Engl J Med 373:1445–1456. https://doi.org/10.1056/NEJMra1315399
Kumar V, Cheng S-C, Johnson MD, Smeekens SP, Wojtowicz A, Giamarellos-Bourboulis E, Karjalainen J, Franke L, Withoff S, Plantinga TS, van de Veerdonk FL, van der Meer JWM, Joosten LAB, Bochud P-Y, Marchetti O, Perfect JR, Xavier R, Kullberg BJ, Wijmenga C, Netea MG (2014) Immunochip SNP array identifies novel genetic variants conferring susceptibility to candidemia. Nat Commun 5:4675. https://doi.org/10.1038/ncomms5675
Lai PH, Lin SM, Pan HB, Yang CF (1997) Disseminated miliary cerebral candidiasis. AJNR Am J Neuroradiol 18:1303–1306
Lee Y, Puumala E, Robbins N, Cowen LE (2021) Antifungal drug resistance: molecular mechanisms in Candida albicans and beyond. Chem Rev 121:3390–3411. https://doi.org/10.1021/acs.chemrev.0c00199
Lewis L, Jayashree P, Bhat Y (2015) Multiple fungal brain abscesses in a neonate: successful treatment with liposomal amphotericin B. Manipal J Nurs Health Sci 1:69
Lionakis MS, Lim JK, Lee C-CR, Murphy PM (2011) Organ-specific innate immune responses in a mouse model of invasive candidiasis. J Innate Immun 3:180–199. https://doi.org/10.1159/000321157
Lionakis MS, Swamydas M, Fischer BG, Plantinga TS, Johnson MD, Jaeger M, Green NM, Masedunskas A, Weigert R, Mikelis C, Wan W, Lee C-CR, Lim JK, Rivollier A, Yang JC, Laird GM, Wheeler RT, Alexander BD, Perfect JR, Gao J-L, Kullberg B-J, Netea MG, Murphy PM (2013) CX3CR1-dependent renal macrophage survival promotes Candida control and host survival. J Clin Invest 123:5035–5051. https://doi.org/10.1172/JCI71307
Lionakis MS, Iliev ID, Hohl TM (2017) Immunity against fungi. JCI. Insight 2:e93156. https://doi.org/10.1172/jci.insight.93156
Liu Y, Mittal R, Solis NV, Prasadarao NV, Filler SG (2011) Mechanisms of Candida albicans trafficking to the brain. PLoS Pathog 7:e1002305. https://doi.org/10.1371/journal.ppat.1002305
McCarthy MW, Kalasauskas D, Petraitis V, Petraitiene R, Walsh TJ (2017) Fungal infections of the central nervous system in children. J Pediatr Infect Dis Soc 6:e123–e133. https://doi.org/10.1093/jpids/pix059
McCullers JA, Vargas SL, Flynn PM, Razzouk BI, Shenep JL (2000) Candidal meningitis in children with cancer. Clin Infect Dis 31:451–457. https://doi.org/10.1086/313987
Mendoza-Reyes DF, Gómez-Gaviria M, Mora-Montes HM (2022) Candida lusitaniae: biology, pathogenicity, virulence factors, diagnosis, and treatment. Infect Drug Resist 15:5121–5135. https://doi.org/10.2147/IDR.S383785
Murthy JMK, Sundaram C (2014) Fungal infections of the central nervous system. In: Biller J, Ferro J (eds) Handbook of clinical neurology. Elsevier, New York, NY, pp 1383–1401
Neves N, Santos L, Reis C, Sarmento A (2014) Candida albicans brain abscesses in an injection drug user patient: a case report. BMC Res Notes 7:837. https://doi.org/10.1186/1756-0500-7-837
Nguyen MH, Yu VL (1995) Meningitis caused by Candida species: an emerging problem in neurosurgical patients. Clin Infect Dis 21:323–327. https://doi.org/10.1093/clinids/21.2.323
O’Brien D, Stevens NT, Lim CH, O’Brien DF, Smyth E, Fitzpatrick F, Humphreys H (2011) Candida infection of the central nervous system following neurosurgery: a 12-year review. Acta Neurochir 153:1347–1350. https://doi.org/10.1007/s00701-011-0990-9
Pappas PG, Kauffman CA, Andes DR, Clancy CJ, Marr KA, Ostrosky-Zeichner L, Reboli AC, Schuster MG, Vazquez JA, Walsh TJ, Zaoutis TE, Sobel JD (2016) Clinical practice guideline for the management of candidiasis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis 62:e1–e50. https://doi.org/10.1093/cid/civ933
Pappas PG, Lionakis MS, Arendrup MC, Ostrosky-Zeichner L, Kullberg BJ (2018) Invasive candidiasis. Nat Rev Dis Primer 4:1–20. https://doi.org/10.1038/nrdp.2018.26
Pendlebury WW, Perl DP, Munoz DG (1989) Multiple microabscesses in the central nervous system: a clinicopathologic study. J Neuropathol Exp Neurol 48:290–300. https://doi.org/10.1097/00005072-198905000-00006
Sánchez PJ, Pérez Cecilia E, Corral O, Romero Vivas J, Picazo JJ (2000) The central nervous system and infection by Candida species. Diagn Microbiol Infect Dis 37:169–179. https://doi.org/10.1016/S0732-8893(00)00140-1
Sánchez-Portocarrero J, Martín-Rabadán P, Saldaña CJ, Pérez-Cecilia E (1994) Candida cerebrospinal fluid shunt infection. Report of two new cases and review of the literature. Diagn Microbiol Infect Dis 20:33–40. https://doi.org/10.1016/0732-8893(94)90016-7
Santiago-Tirado FH, Doering TL (2017) False friends: phagocytes as Trojan horses in microbial brain infections. PLoS Pathog 13:e1006680. https://doi.org/10.1371/journal.ppat.1006680
Sendid B, Caillot D, Baccouch-Humbert B, Klingspor L, Grandjean M, Bonnin A, Poulain D (2003) Contribution of the Platelia Candida-specific antibody and antigen tests to early diagnosis of systemic Candida tropicalis infection in neutropenic adults. J Clin Microbiol 41:4551–4558. https://doi.org/10.1128/JCM.41.10.4551-4558.2003
Shah VB, Williams DL, Keshvara L (2009) β-Glucan attenuates TLR2- and TLR4-mediated cytokine production by microglia. Neurosci Lett 458:111–115. https://doi.org/10.1016/j.neulet.2009.04.039
Shankar SK, Mahadevan A, Sundaram C, Sarkar C, Chacko G, Lanjewar DN, Santosh V, Yasha TC, Radhakrishnan VV (2007) Pathobiology of fungal infections of the central nervous system with special reference to the Indian scenario. Neurol India 55:198. https://doi.org/10.4103/0028-3886.35680
Sharma R, Pawar S, Lad S, Mishra G, Netalkar A, Rege S (2012) Fungal infections of the central nervous system. In: Schmidek and sweet: operative neurosurgical techniques, pp 1691–1732
Shi M, Mody CH (2016) Fungal infection in the brain: what we learned from intravital imaging. Front Immunol 7:7
Swamydas M, Gao J-L, Break TJ, Johnson MD, Jaeger M, Rodriguez CA, Lim JK, Green NM, Collar AL, Fischer BG, Lee C-CR, Perfect JR, Alexander BD, Kullberg B-J, Netea MG, Murphy PM, Lionakis MS (2016) CXCR1-mediated neutrophil degranulation and fungal killing promote Candida clearance and host survival. Sci Transl Med 8:322ra10. https://doi.org/10.1126/scitranslmed.aac7718
Trofa D, Gácser A, Nosanchuk JD (2008) Candida parapsilosis, an emerging fungal pathogen. Clin Microbiol Rev 21:606–625. https://doi.org/10.1128/CMR.00013-08
van den Anker JN, van Popele NM, Sauer PJ (1995) Antifungal agents in neonatal systemic candidiasis. Antimicrob Agents Chemother 39:1391–1397
van Till JWO, Modderman PW, de Boer M, Hart MHL, Beld MGHM, Boermeester MA (2008) Mannose-binding lectin deficiency facilitates abdominal Candida infections in patients with secondary peritonitis. Clin Vaccine Immunol 15:65–70. https://doi.org/10.1128/CVI.00297-07
Voice RA, Bradley SF, Sangeorzan JA, Kauffman CA (1994) Chronic Candidal meningitis: an uncommon manifestation of candidiasis. Clin Infect Dis 19:60–66. https://doi.org/10.1093/clinids/19.1.60
Yoshida K, Matsuda N, Sato T, Watanabe T, Nakamura K, Saito K, Kanai K, Ugawa Y (2022) Candida brain abscesses in a patient with anorexia nervosa receiving total parenteral nutrition. Clin Neurol Neurosurg 212:107058. https://doi.org/10.1016/j.clineuro.2021.107058
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Fatima, N., Ahmed, S. (2023). Neuro-Infections Caused By Candida Species. In: Sami, H., Firoze, S., Khan, P.A. (eds) Viral and Fungal Infections of the Central Nervous System: A Microbiological Perspective . Springer, Singapore. https://doi.org/10.1007/978-981-99-6445-1_12
Download citation
DOI: https://doi.org/10.1007/978-981-99-6445-1_12
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-99-6444-4
Online ISBN: 978-981-99-6445-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)