Abstract
You will be able to understand the following after reading this chapter:
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
You will be able to understand the following after reading this chapter:
-
Principles and application of different external techniques of fracture fixation such as bandages, splints, slings, casts, and modified Thomas splint
-
Basic principles and techniques of internal fixation such as intramedullary pins/nails, bone plate, and screws, minimally invasive percutaneous osteosynthesis, and ancillary fixation devices such as orthopedic wires and screws
-
Indications, biomechanics, and different types of external skeletal fixation systems, linear ESF systems for small animals, transfixation pinning and casting, bilateral linear ESF system for large animals, circular ESF, epoxy-pin fixation, and complications of ESF
-
Splint and bandage, the most economical orthopedic application, can be used as a first aid to stabilize fractures temporarily, to prevent preoperative or postoperative swelling or as a primary fixation method in closed fractures of the distal limb bones especially in lightweight animals.
-
Velpeau sling is used to hold the shoulder joint in flexion, while Ehmer sling is used to stabilize the hip joint.
-
Fiberglass cast, a synthetic alternative to the plaster of Paris cast, is preferred for both small and large animal applications as it has greater strength and durability, is lightweight, sets quickly, and allows immediate weight-bearing on the limb.
-
Intramedullary (IM) Steinmann pin is the most widely used internal fixation device in veterinary practice as it can resist bending forces well and maintain bone alignment due to its central position in the medullary cavity. Cross IM pinning can provide stable fixation of small segment fractures, such as supracondylar femoral fractures, with minimal damage to the growth plate.
-
Interlocking nail system is useful to repair comminuted long bone fractures, as the nail is secured to the bone cortex using fixation bolts that provides rotational stability and prevents collapse of fracture segments. Locking plate with threaded screw holes is biomechanically superior to conventional dynamic compression plate.
-
In minimally invasive plate osteosynthesis technique, a bone plate is applied in a bridging fashion through small incisions without exposing the fracture site.
-
External skeletal fixation (ESF) is a versatile and minimally invasive orthopedic procedure with excellent mechanical properties allowing early return to function of the affected limb.
-
The circular and hybrid ESF systems can provide stable fixation of long bone fractures and are effective to treat fractures in angularly placed bones such as the tibia and transarticular stabilization of fractures with small bone segments near the joint.
-
The epoxy-pin fixation technique, wherein the bent fixation pins are incorporated within the epoxy mold to construct the connecting side bars, can be easily applied with minimal facilities and can provide stable fixation of fractures in different species of animals weighing up to about 100 kg.
Fracture fixation techniques can be broadly classified as external fixation techniques, internal fixation techniques, and external skeletal fixation techniques. The basic principle of any technique is to provide stable bone fixation by immobilizing the fractured bone segments to enable early bone healing and functional recovery of the injured limb. The way and the extent to which it is achieved, however, differ among the techniques, apart from the fracture configuration and location.
2.1 External Fixation Techniques
External fixation or external coaptation, often called as conservative fracture management, refers to immobilization of fractures and other skeletal abnormalities with devices applied externally, without the use of any invasive technique. External coaptation has been the most widely used technique for fracture management in man and animals for centuries. Although materials may have changed, techniques largely remain the same with few modifications. Among the external fixation techniques practiced today, bandage and splints, plaster/synthetic cast, modified Thomas splints, and splint-cast combinations are widely used in both small and large animal practices [1,2,3,4,5,6]. As external coaptation techniques are relatively inexpensive and non-invasive, they are frequently applied even in situations where they are not ideal or where there is a high probability of complications (where probably surgical fixation is recommended), mostly due to financial or other constraints. Nevertheless, external coaptation is an integral part of every form of orthopedic therapy, be it to prevent swelling, as a first aid to treat fractures temporarily, as a primary means of fixation in specific fractures, or as an additional support in various conditions such as internal fixation of comminuted unstable fractures, arthrodesis, tendon suturing, etc. Proper case and technique selection is essential for successful outcomes.
2.1.1 Bandages
Application of bandage and splint is the simplest and probably the most economical orthopedic application (Fig. 2.1). It does not need any special materials or instruments and can be easily applied. It looks quite easy to apply bandage and splints, but it may get loosened when not tight enough or may cause serious complications when too tight.
Application of bandages may help to cover the wounds and prevent preoperative or postoperative swelling and as a first aid stabilize fractures temporarily. For bandaging, the animal is properly restrained in lateral recumbency, and the affected limb is held upwards. In forelimb applications, the elbow joint is held in fully extended position, whereas in the hindlimbs, the stifle joint is held partially extended. Help can be taken from an assistant to keep the limb in extended position using an anchor tape/adhesive tape applied along the limb extremity or a cotton bandage tied around and above the toes. Cotton stripes are put between the toes, and adequate padding of the limb is done by wrapping an even layer of cotton roll around the limb, starting from the distal end, including the fractured bone, and up to above the joint proximally. Cotton gauze is then firmly applied by twisting over the cotton padding from the distal to the proximal end, so as to leave 1–2 cm of cotton strip out of the bandage proximally. The cotton gauze is then quickly twisted back from the proximal to the distal end, with each new twist covering 1/2–2/3 of the previous. This ‘to and fro’ covering of cotton gauze is done for 3–4 times. The distal end of the limb may be covered using additional gauze flaps placed from the dorsal to the plantar aspect and then secured with twisting the bandage roll around the limb. Finally, after making sure that the bandage is uniform and firm, if needed, additional coverings are reinforced. An adhesive tape is then wrapped around the limb in a circular fashion intermittently to secure the bandage. The bandage so applied should be changed every 3–4 days depending on the case situation, especially in cases with open wounds/fractures.
Elastic bandage can be used to protect from postoperative oedema and swelling. Normally, the bandage is directly applied over the skin, and if there is a need to keep the bandage for more than 3–4 days, it may be applied over the first layer of the cotton padding. While applying the bandage over the limb, it is important to make sure that the pressure is adequate with same level of elasticity. The end of the bandage is secured with an adhesive tape to prevent loosening, and the proximal edge of the bandage is stuck to the skin.
Robert-Jones bandage is used to prevent soft tissue inflammation and to temporarily immobilize the stable limb fractures below the elbow or stifle joint [7]. In this technique, 3–4 thick layers of cotton padding are done around the leg (as described above), which is then tightly and uniformly compressed by covering with cotton gauze roll. Thick cotton padding around the limb prevents any chance of vascular compromise while tightening the gauze roll. If the outer covering is not tightened firmly, there is possibility of slipping of bandage. This can be prevented by applying adhesive tape along the lateral and medial side of the leg from proximal to distal (with a long tail projecting at the tip of the toe) before the cotton is applied and turning it backwards (180°) to stack it to the bandage before completion. This ‘massive’ bandage often causes inconvenience to the animal. Hence, the modified Robert-Jones bandage having much less cotton padding is commonly used in small animals and small ruminants (Fig. 2.2). The bandage can incorporate splints or casts to increase its rigidity. Two to four wooden or aluminum stripes can be sandwiched between the layers of the bandage equally around the leg or a half-leg; molded thermoplastic cast (caudal half for the front leg, cranial half for the hind leg) can be used to make the bandage stiff and strong. The tips of the toes may be excluded while bandaging, which may allow for daily inspection, but too much exposure and constriction around the toe should be avoided not to obstruct the venous blood flow causing swelling. The Robert-Jones bandage is effective for short-term applications only. The elastic bandage provides the compression to the surface of the limb for very short duration, lasting for not more than 24–48 h; hence, it is inappropriate for any use beyond 1–2 days.
2.1.2 Splints
Splints cover only a part of the limb surface, unlike casts which encircle the entire limb. They are indicated in stable closed fractures distal to the proximal 1/3 of the radius or tibia (mostly with intact ulna or fibula). Open fractures with wounds and unstable comminuted fractures are contraindications for its use. Splints can be either prefabricated (mostly made of plastics or aluminum) or custom-made (plaster/fiberglass cast or thermoplastics). Preformed splints are more convenient but they often do not fit adequately. The disadvantage with wooden or plastic sticks is that they do not adapt to the leg (the leg is adapted to the splint), whereas the cast splint can adapt to the contours of the leg. Hence, wooden sticks or plastics can only be used for first aid and for temporary stabilization of fractures and not preferred for definitive treatment (Fig. 2.3). Thermoplastic material is also not used as definitive fixation device as it also does not adapt to the contours of the leg and hence may not provide stable fixation of fracture segments. Molding several layers of casting tape to the limb produces better fracture stability and a more comfortable fit for animal applications. Plaster of Paris can be easily molded along the contours of the leg and is quite resistant against bending load; however, it is not resistant against humidity and may lose its strength upon wetting. Newer synthetic cast materials such as fiberglass cast are strong and can mold to the shape of the limb, but it is costly and more expensive.
Splints should be applied along the length of a fractured leg, distally from the point of the toes/hoof and proximally up to the joint above the fracture site. It should include the carpal joint in metacarpal fractures and the tarsal joint in case of metatarsal fractures, whereas in fractures distal to the elbow (distal 2/3 of radius-ulna) or stifle (distal 2/3 of tibia-fibula) joints, the splint should extend up to the olecranon and tibial tuberosity, respectively (Fig. 2.4). Half/hemi-splint, covering half of the leg surface is generally ideal, as it provides support to the broken bone, allows for swelling, and is easily removed. In forelimbs, the splint is applied along the caudal surface of the antebrachium, as the ulna is longer and courses more superficially than the radius. In hindlimbs, the splint is applied along the cranial surface of the crus as the tibia is located at the cranial aspect and the presence of the Achilles tendon caudally may not allow its proper placement.
For application of splint, under deep sedation, the animal is restrained with the fractured limb downwards but slightly tilted on its back. Fracture segments are reduced and the limb is held extended. The whole leg is then padded with a thin cotton layer, covering the areas of bony prominences, followed by a layer of cotton gauze bandage. A 6–8-layer plaster strip is immersed in warm water (till the air bubbles stop coming), squeezed to remove excessive water, compressed uniformly, and applied at the right place. When still wet, the plaster is contoured to the surface of the limb and allowed to harden. The splint edges are then smoothened by trimming with a pair of scissors (POP) or a saw (fiberglass), and the splint is properly placed. The uncovered part of the leg is padded with the cotton to fill the gap. The plaster splint along with the cotton is then secured around the limb by applying cotton gauze roll from the distal to the proximal end.
In large animals, splint and bandage is often used for temporary stabilization of fractures in straight long bones such as the metatarsus, metacarpus, and radius-ulna (Fig. 2.5). It can also be used as a primary fixation method, especially in lightweight animals. Under sedation, the animal is restrained in lateral recumbency with the fractured leg held uppermost. A long length of cotton gauze/rope is loosely tied around and just above the hoof, to help reduce the fracture by applying traction and counter-traction and to keep the limb in extended position with the help of an assistant. After sprinkling talcum powder over the limb, ‘adequate’ padding of the limb is done by wrapping an even layer of cotton around the limb. A roll of cotton gauze is then firmly wrapped around the limb starting from the distal extremity of the limb and moving upwards, leaving about 1–2 cm cotton strip out of the bandage at the proximal end. After a layer of bandaging, two wooden/metal splints of appropriate length are placed at 90° to each other (one on the medial/lateral aspect and another on the caudal/cranial aspect). In heavy animals, 3–4 splints may be used and are secured by tying cotton gauze roll/ropes around. The width and thickness of the splint may vary as per the animal’s size, but it should not be very light (may break during weight-bearing) or very heavy (may interfere with normal weight-bearing). The length of the splint should span from the hoof up to the joint above the fracture site. The cotton gauze roll is then wrapped over and above the splints by incorporating them within. Depending on the case, several layers of wrapping are done. Extra turns of gauze roll are taken at the distal and proximal ends to secure the splints properly, and at the level of the joints, extra layers of wrapping are done in figure of ‘8’ fashion to provide additional support against bending stress. Before applying the final layers of the bandage, the anchor tapes/ropes are released by loosening/cutting, and the extra length of cotton sticking out is reflected back and included in the bandage. The splint and bandage is then secured by applying adhesive tape rolls around at places, especially at the distal extremity, proximal end, and at the level of joints.
2.1.3 Slings
Slings are infrequently used for external coaptation in animals [7]. Velpeau sling is used to hold the forelimb joints (carpus, elbow, and shoulder) in flexion by bandaging the limb against the body, thus preventing weight-bearing on the affected limb (Fig. 2.6). It is indicated in stabilization of minor fractures of the scapula and humerus or reduced shoulder luxation. The sling can be applied in standing awake animals or in recumbent animals under general anesthesia. The paw and carpus are held in a slightly flexed position, and cotton padding is done followed by wrapping of the elastic bandage roll. By placing the padded portion in the axillary region, the wrap is continued to cover the elbow and shoulder, holding the limb to the side of the torso and encircling the body. Padding is ideally wrapped behind and in front of the opposite limb alternatively to prevent its slippage. While bandaging, a small window may be left at the distal end of the limb to visualize the toes.
Velpeau sling: (a) the paw of the affected limb is loosely wrapped around (lateral to medial) using a gauze bandage; (b) by keeping the carpus, elbow, and shoulder joints in flexed position, the gauze bandage is taken over the lateral aspect of the limb and chest and brought behind the opposite axilla; (c) several such layers of gauze are applied taking around the flexed carpus; (d) gauze bandaging is completed by taking several layers of wrap around the chest and secured
Ehmer sling, which is more popular in veterinary practice, prevents the patient from weight-bearing on the bandaged hindlimb (Fig. 2.7). It is indicated to provide stability following reduction of a cranio-dorsal luxation of the hip joint. The sling if applied properly helps to abduct and internally rotate the femur and thus keep the femur head within the acetabular cavity. This is not indicated in ventral dislocation of the hip, as abduction of the limb may lead to re-luxation. The technique includes soft padding of the hind paw and metatarsal region followed by elastic gauze application starting from the lateral surface of the paw. The gauze roll is then progressed upwards on the medial side and over the quadriceps. By flexing the leg, the bandage roll is continued laterally over the thigh and medial to the hock joint to take it around the paw. This process is repeated 2–3 times and then the gauze bandage is wrapped around the body by keeping the limb close to the body in a flexed position. At the end, the gauze bandage is fixed using one or two pieces of adhesive tape to prevent loosening of the bandage. The sling is kept in place for about 10–15 days to achieve full stability of the joint, constantly observed, and if get wet or loosened, it is reapplied.
Application of Ehmer sling: (a) the hind paw and metatarsal region are soft padded and the elastic gauze is applied starting from the lateral surface of the paw and is then progressed upwards on the medial side and over the quadriceps; (b) by flexing the leg, the bandage roll is continued laterally over the thigh and medial to the hock joint to take it around the paw; (c) rolling of bandage is repeated 2–3 times; and (d) the gauze bandage is wrapped around the body by keeping the limb close to the body in flexed position and secured using clips or adhesive bandage application
2.1.4 Plaster Cast
Plaster cast is the most widely practiced external fixation technique in both small and large animals [2, 6,7,8]. Plaster bandage consists of a cotton bandage impregnated with plaster of Paris that hardens upon wetting. Plaster of Paris is anhydrous calcium sulfate that has been heated. In the presence of water, the soluble form of calcium sulfate becomes insoluble (hardening) with production of heat (exothermic reaction):
2.1.4.1 Indications and Contraindications
It is indicated in fractures below the mid-diaphysis of the radius or tibia (below the elbow or stifle joint) and is most suitable for straight limb applications like fractures of the metacarpus, radius-ulna, and metatarsus. Plaster should be used in only those fractures which can be closely reduced and maintained with at least 50% of the bone ends in contact. Further, fractures that are expected to heal relatively rapidly are chosen for cast application to reduce the chances of cast-related complications. Plaster cast is contraindicated in proximal bones such as the femur and humerus, as the joints above (hip and shoulder joints) cannot be stabilized adequately by a cast. Generally, it is not indicated in open fractures with soft tissue injury.
Plaster should be applied in fresh cases with no or little soft tissue swelling or when the inflammatory swelling has subsided (after 3–4 days of initial injury), to prevent cast loosening and slippage. Until then, the limb may be immobilized using temporary splinting and bandaging.
2.1.4.2 Biomechanics
Full cylindrical cast of adequate thickness, which conforms to the limb and immobilizes the joints above and below the fracture site, can effectively neutralize bending and rotational forces; however, it is generally unable to resist compressive, shear, and tensile forces. A cast applied straight is better able to resist fracture forces than that applied angularly. As the cast is applied around the limb (bone surrounded by soft tissues), there exists a certain distance between the cast and the bone; therefore, the level of fixation stability achieved is much less than internal fixation and also external skeletal fixation, where the bone segments are directly immobilized using fixation implants. Hence, the bones having least coverage of soft tissues, such as radius-ulna, metacarpus, and metatarsus, are better suited for cast application.
Fracture immobilized by a cast heals by secondary healing, i.e. through external callus formation (suggesting adequate stability to allow revascularization and callus formation), but stability is insufficient to allow primary bone union (micro-movement at the fracture site persists).
2.1.4.3 Technique
Usually, the animal is restrained in lateral recumbency with the fractured limb positioned upwards, under deep sedation or general anesthesia. An assistant can help to maintain proper alignment of bone segments and ensure the correct positioning of the limb. In small animals, adhesive tapes (anchor tape) may be placed along the medial and lateral sides of the foot extending about 10 cm beyond the toes, to hold the limb in an extended position. A cotton bandage may also be tied around the toes to hold the limb and apply tension. In large animals, rope restraint may be used; in heavy animals, the limb can be pulled by applying traction using the wires placed through the holes drilled in the hoof wall.
In general, the limb is placed in a comfortable position, with the normal standing angle preferred during casting. The limb should be dry before cast application. The talcum powder may be sprinkled over the limb (shaving is not needed), and an even layer of cotton is applied around the leg in order to protect bony prominences. The cotton padding is extended 1–2 cm beyond the cast to prevent direct contact with the skin. Over-padding should be avoided to prevent cast loosening; further, it may impair immobilization by allowing movement of fracture segments within the cast. A tube of stockinette firmly fitting the limb may be slipped along the length of the limb (Fig. 2.8). If not, a roll of cotton bandage may be used to wrap the limb in spiral fashion. An assistant (may be two are required in large animals) can hold the limb in traction by grasping the stockinette/cotton bandage above and the anchor tape/rope below the area to be covered by the cast.
Application of plaster cast: (a) adhesive tapes applied along the medial and lateral sides of the foot extending beyond the toes to hold the limb in extended position; (b) a stockinette is slipped along the length of the limb (adopted from Leighton, R.L. 1991. Principles of conservative fracture management: splints and casts. Semin Vet Med Surg. 6 (1): 39–51.)
Plaster of Paris bandage is soaked in warm water for a few seconds until air bubbles cease to appear. It is then removed from the water, squeezed, and wrapped over the limb, starting at the fracture site from the distal to the proximal (Fig. 2.9). Subsequently, remaining POP bandages are applied one by one along the entire limb except for the toe pads in dogs and hooves in large animals. A strip of a few (6–8) layers of plaster can be made wet and applied firmly along the caudal surface of the limb to provide greater strength to fixation (Fig. 2.10). During cast application, formation of folds or indentations should be prevented as they may cause injury and necrosis of the underlying skin. Overstretching and tightening of the plaster cast around the limb should also be avoided.
Application of plaster cast: (a) POP bandage is soaked in warm water for a few seconds until air bubbles cease to appear; (b) POP bandage is removed from the water and squeezed; (c, d) POP bandage is then wrapped around the limb, starting at the fracture site from the distal to proximal (adopted from Leighton, R.L. 1991. Principles of conservative fracture management: splints and casts. Semin Vet Med Surg. 6 (1): 39–51.)
Application of plaster cast: (a) a strip of a few layers of plaster (6–8) is made wet, (b) it is then applied firmly along the caudal surface, and the tapes and the stockinette are reflected back onto the cast at both ends, and (c) the final layers of cast are applied, molded by rubbing the layers of cast using a wet hand; a wet plastic sheet may be used to smoothen the surface, and it is then allowed to dry (adopted from Leighton, R.L. 1991. Principles of conservative fracture management: splints and casts. Semin Vet Med Surg. 6 (1): 39–51.)
The strength of the cast can be increased and weight reduced by incorporating the splints within the cast, especially in large animals. Two wooden/metal rods can be placed 900 to each other. In large animal applications, a ‘U’-shaped walking bar (metal strip) may be placed under the hoof and incorporated into the cast (Fig. 2.11). This can reduce the loading forces on the distal limb and thus help protect the fracture site.
The plaster is molded by rubbing with wet hand after each layer before hardening. And before applying the final layers of cast, the tapes and the stockinette are reflected back onto the cast at both ends. If a rope is used, one should not forget to untie the knot (if applied) before allowing the cast to set. At the end, a wet polythene sheet may be pressed over the wet cast to smoothen the surface.
The plaster cast should generally extend from the toe/hoof up to above the level of the joint proximal to the fracture site. In heavy animals, the full-limb cast extending up to the elbow or stifle joint should be applied even if the fracture is in the metacarpus or metatarsus, especially if it is at the proximal end of the bone near the carpal/tarsal joint. The thickness of the cast may vary depending on the case. In small animal applications, 4–5-layer thick cast is usually adequate; in calves weighing up to 150 kg, 6–8-layer thick cast may be required; and in adult large animals, 12–16-layer thick casts may be needed. The cast should be thicker at the level of the joints (applied in figure of 8 fashion), especially at the hock joint (hindlimb) to resist the stress concentration due to the angulation and movement of the joints.
The plaster is then allowed to become dry and hard before letting the animal bear weight on the limb. This may take about 30–45 min in small animals and about 1–2 h in large animals. However, complete drying and hardening of the cast (attaining full strength) may take 24–72 h depending on the thickness.
‘Bi-halving’ can be done after applying the cast, allowing it to set, and then making it into two halves by cutting longitudinally along the medial and lateral aspects of the cast. After placing back the halved cast on the limb, it is then wrapped with an elastic bandage to hold it firmly. Bi-halving a cast allows examination of the underlying soft tissues if need arises and allows easy removal of the cast if swelling develops, and it can be reapplied. This technique is often used in small animals and rarely practiced in large animals, as bi-halving reduces the fixation strength of the cast considerably.
2.1.4.4 Post-application Care and Management
In open fractures, for drainage and daily dressing of the skin wound, an opening (window) is made in the cast at the level of the wound. The window at the wound site can also be left at the time of cast application. One should remember that creating a ‘window’ in the cast will reduce its strength considerably and make the window site prone for breakage, especially when it is at the level of joints.
Complications can occur with application of cast both in small and large animals [2, 9,10,11]. The toes/hooves are inspected several times during the first 48 h for any swelling, coldness, or constriction. If the toe/hoof gets swollen or gets cold, pressure at the end of the cast should be relieved by removing the cast, and the cast may be reapplied after swelling subsides. Similarly, if the cast gets loosened and slips (due to subsiding of inflammatory swelling present earlier), the cast should be reapplied.
The plastered animal should be kept in a dry place (to prevent the cast from getting wet) with soft bedding (to prevent slippage). Wetting is more common in hindlimbs due to urination; it weakens the cast and may lead to its breakage. Plastic (polythene) sheets may be wrapped around the cast to prevent wetting.
Cast may be retained for up to 3–4 weeks in young dogs, sheep, and goats and 4–6 weeks in adult dogs, sheep/goats, and calves. In adult large animals, clinical union of fracture (development of bridging callus with adequate fracture stability) may normally take place by 8–10 weeks, but often, it may require 12–16 weeks or more. Plaster is removed using a saw after radiographic fracture union (complete bony union with obliteration of fracture line), which generally takes a few weeks to months after the clinical union. After removal of the cast, the affected limb is massaged to promote circulation. Movement is restricted till the limb regains its normal function.
2.1.5 Fiberglass Cast
Fiberglass cast, unlike traditional plaster cast, is strong, lightweight, and radiolucent. Due to its desirable qualities, fiberglass cast has become the preferred type of casting both in human and veterinary orthopedics [12,13,14,15,16].
2.1.5.1 Advantages over Plaster Cast
Fiberglass cast is made of water-activated polyurethane resin combined with bandaging materials, so it offers greater strength and durability. It weighs less and hence more comfortable to the patient. The setting time is very quick and therefore needs less care and restraint during application, and the animal can be allowed to use the limb almost immediately. Fiberglass cast is radiolucent and hence allows better radiographic evaluation of fracture repair. It is also water impermeable (waterproof); therefore, the inside padding does not get wet. If the cast gets wet, it quickly becomes dry.
2.1.5.2 Drawbacks
Fiberglass cast is costlier than traditional plaster cast; hence, it may be a constraint in veterinary practice. As fiberglass cast hardens quickly, there is less time to apply. The synthetic materials leave less room for swelling; if more tightly applied, it may lead to vascular compromise. Knitted fiberglass and resin bandages are less moldable than a traditional plaster, so sometimes a less comfortable fit is achieved. Fiberglass bandage is less smooth and more likely to snag clothing or to cause skin bite injuries.
2.1.5.3 Technique
Technique of application of fiberglass cast is almost similar to that of plaster cast. The fractured limb is first padded with cotton or any other waterproof padding material. Then, the knitted fiberglass bandage is wrapped around the limb in several layers (Fig. 2.12). The use of stockinettes and/or cast padding is essential to avoid direct contact between the cast and the skin. Wearing of protective gloves is a must during its application to prevent sticking of the cast material (once get stick, it is difficult to remove).
When the cast material is immersed in water, it should be squeezed firmly before applying. Cast should be applied quickly, to prevent premature hardening. Application of 3–4 layers of the cast is enough in small animals and 6–8 layers in large animals. Further, application of additional support strip or splints is not needed (stronger than plaster cast). The cast may be smoothed with a smoothing gel or lubricating gel.
2.1.5.4 Post-application Care and Management
A fiberglass cast requires less care and maintenance than a plaster cast, and weight-bearing can be allowed as early as 15–20 min post-application. The limb immobilized with a fiberglass cast should be watched carefully in the first 24–48 h after the application for any swelling, coldness, or bad odor, as there is less room for swelling. Complications are more in equine patients (skin is more sensitive) than bovines. In case of any doubt, the cast should be removed and reapplied after the swelling subsides. For removal of the cast, an electric/power saw is needed, as it is difficult to cut the cast using a hand saw. While cutting the cast, it is taken care to prevent any possible injury to the skin.
2.1.6 Modified Thomas Splints
Modified Thomas splint (Schroeder-Thomas splint) is a whole limb traction splint, wherein the fracture ends are brought together and held in alignment by application of traction in specific directions using traction tapes/ropes/bandages, which are anchored to the supporting side rods [6, 7, 17]. This technique is not widely used in practice nowadays due to the advent of better internal and external skeletal fixation techniques; however, if properly used, it can give satisfactory results in many types of fractures, especially in small lightweight animals. Modified Thomas splint and cast combination has been used successfully for treatment of different long bone fractures in large ruminants too.
2.1.6.1 Indications and Contraindications
Modified Thomas splints are generally indicated for treatment of fractures at the distal femur and humerus, tibia-fibula, and radius-ulna in dogs, cats, sheep, goats, and young calves. Splint-cast combination is indicated in heavy animals. It is either used as a sole method of fracture fixation or as an ancillary method along with internal fixation techniques such as intramedullary pins.
Modified Thomas splint is not indicated in long oblique and comminuted fractures, where it is difficult to reduce the fracture segments by close method and prevent overriding of bone ends. Further, fractures near the joints, unless properly reduced, may lead to malunion and degenerative joint disease.
2.1.6.2 Materials Required
Aluminum rods (for dogs, cats, sheep/goats) or steel rods (for calves/foals) of varied diameter (5–7 mm is adequate in most cases; in adult large animals, 8–12 mm rods may be needed depending on the size of the animal), rod bender, pin cutter, cotton roll, gauze bandage, and adhesive tape are needed.
2.1.6.3 Technique of Application
Under deep sedation/tranquilization (general anesthesia may be preferred where severe overriding of fracture segments is present), the animal is restrained in lateral recumbency with the fractured leg held upwards. The splint is customized to the individual case, so as to fit well to the front limb or hindlimb of the patient.
Firstly, the aluminum rod is bent to make a ring (1½ circle, taking the help of a splint mold or any cylindrical object of appropriate size) to properly fit in the patient’s groin or axilla and secured using adhesive tapes (Figs. 2.13 and 2.14). The size of the ring should be kept adequate to accommodate wrapping of the ring with cotton roll and bandages. For hindlimb splint, the ring diameter should be the distance from the tuber ischii to the tuber coxae. For the forelimb, the distance from the axilla to the midpoint on the scapula should be the diameter of the ring. The ring is bent inwardly (toward medial side) at 45° angle from the vertical rods. The ring is then wrapped with a thin strip of cotton roll and secured with gauze bandage and adhesive tape. Sufficient padding is done at the bottom of the ring to protect the groin/axilla region when the splint is applied with the limb under traction.
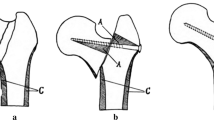
Application of Modified Thomas splint: (a) an aluminum rod is bent to make a ring (1½ circle) and secured using an adhesive tape; (b) the ring is bent at 450 angle from the vertical rods; (c) the limb is temporarily inserted into the rings to determine the length of side rods, and the side bar is bent at the level of the stifle and hock; (d) the extra length of the rod is cut and joined to give the final shape
The limb is temporarily inserted into the rings to determine the length of side rods. The length of the splint should be slightly longer than the extended limb. If the length is too long, it will hinder locomotion; and if it is short, proper tension cannot be applied. The total length of the rod is calculated as 2(3D + 1) + 2 L + 20, where D = diameter of the ring and L = length of the splint bar. For the forelimb, the diameter (D) is the length from axilla to midpoint of the scapula, and the length of bar (L) is the distance from axilla to the tip of the toe in an extended leg, whereas for the hindlimb, the diameter (D) is the length from tuber ischii to tuber coxae, and the length of bar (L) is the distance from the thigh to the tip of the toe in an extended leg.
For forelimb splint, both splint rods (cranial and caudal) are bent slightly at the level of the elbow to conform to the standing angle, whereas for the hindlimb, the caudal as well as the cranial rods can be bent to conform to the standing angles of stifle and hock joints, or the caudal rod can be kept straight without any bend and the cranial rod may be bent at stifle and hock (Fig. 2.15). The distal end of side rods is bent inwards and secured together using adhesive tape.
In bovine calves, iron/steel rods may be used in place of aluminum rods to construct the splint to provide greater strength to fixation (Fig. 2.16). Rings have to be secured by welding (rather than by adhesive tape), and an oval-shaped iron sheet of the size of hoof is welded at the distal end of side rods to provide a suitable anchorage for the hoof. The side rods of the splint are generally kept straight without any angulation/bending. The whole length of side rods may be tightly wrapped with gauze bandage, which is then anchored with adhesive tapes at different places.
At the distal extremity of the limb, adhesive tape strips are attached, one on the dorsal and another on the palmar/plantar surface, and the extended portions of the adhesive tapes are stuck together below the toes (dogs/cats) or hooves (sheep/goats) (Fig. 2.17). A thin layer of cotton roll is wrapped around the limb over the tape strips (from toe up to the knee/hock joint), which is then covered with a firm wrap of gauze bandage and anchored at places using circular wrap of adhesive tape to ensure that the tape strips applied on the limb do not slip while applying traction. In large animals, cotton rope may be anchored above the fetlock using a loose slip knot in place of adhesive tape strips to enable traction with greater force.
Anchoring the limb in MTS: (a) adhesive tape strips are applied on the dorsal and palmar/plantar aspect, and the extended portions of the adhesive tapes are stuck together below the toes; (b) wrapped around the limb using cotton roll and gauze bandage; and (c) securing the tape strip to the ‘U’ bottom of the splint under tension
The limb is inserted into the ring (bend should be held toward the inner/medial side of the limb) and ensured that the ring is properly and firmly fit in the region of the groin/axilla. Traction is applied at the extremity of the limb by tensioning the tapes/ropes and the tape strip/rope is secured to the ‘U’ portion of the splint under tension, in such a way that the leg is slightly rotated inwardly. Then, as per the fracture location and displacement of bone segments, the traction is applied at different levels, and the bones are fixed to the frame using cotton strips or bandages.
2.1.6.4 Application of Traction
The fracture site is supported and secured to the side rods with the help of cotton strips/bandages for applying traction at least at two locations (one above and one below the fracture site) around the non-fractured bones of the limb.
To apply traction, the cotton strip/bandage is secured to the side bar toward the direction at which the traction is desired (say, cranial). It is then wrapped around the portion of the limb by taking it through the medial, caudal, and lateral sides and bringing it back to the original side bar with firm traction, to allow pulling of that portion of the limb toward the side bar (cranial). Few more layers of similar wrappings may be done to provide additional support. The cotton bandage is then encircled around the limb including both side rods 2–3 times and secured using an adhesive tape.
In middle or distal diaphyseal fractures of humerus, the side rods are bent at a more acute angle at the elbow, and both the foot and the radius-ulna are drawn caudally by using traction bandages (Fig. 2.18). In middle or proximal diaphyseal fractures of the radius-ulna, the side rods are only slightly angled at the elbow to provide an almost straight pull on the limb; the traction is applied caudally at the lower limb as well as at the humerus.
In fractures of the femur or tibia, the lower limb cotton strip/bandage should secure the foot in caudal position. The proximal strip should pull the tibia and stifle (in femoral fractures) or the femur (in tibial fractures) toward the cranial side (Fig. 2.19).
In fractures of carpals/metacarpals, the side bars of the splint are more acutely bent at the hock corresponding to the normal standing angle of the joint. The distal bandage strip should hold the foot caudally and the proximal strip should draw the femur cranially.
Once the splint is properly secured and traction applied appropriately, the entire splint may be covered with a stockinette or cotton bandage rolls and secured using adhesive tapes at desired places, before allowing the weight-bearing on the limb.
2.1.6.5 Postoperative Care
The animal must be checked frequently for any injury at the groin or axilla that may have been caused due to rubbing of the ring. The splint is kept in place for 3–6 weeks as per the fracture type and location or till the radiographic healing occurs. All skin wounds created by rubbing of splint, if any, may be treated with antibiotic ointment/powder.
2.1.7 Thomas Splint-Cast Combination
2.1.7.1 Indication
Modified Thomas splint-cast combination is indicated for treating closed radius-ulna and tibial fractures in heavy large animals, in which full-limb cast alone does not provide adequate immobilization [2, 18,19,20]. Generally, it is not recommended in very young animals and also in cases of severe comminuted fractures and in fractures near the joint (metaphyseal or epiphyseal fractures).
2.1.7.2 Biomechanics
The fractured limb is spared from weight-bearing stresses, which are taken by the splint rods, preventing collapse of the fracture segments. Adequate immobilization of fracture segments allows healing of the bone by external callus formation.
2.1.7.3 Technique
Under sedation or general anesthesia, the animal is positioned in lateral recumbency with the affected limb held upwards. The limb is held in extended position using a tape strip/traction rope tied above the pastern. Alternatively, holes can be drilled in the hoof wall of both distal phalanges, and a suitable size wire threaded through these holes can be used to apply traction and subsequently secure the limb with the splint rod.
An appropriate size steel rod (10–12 mm) is bent from the middle of the rod (using a template) to make a ring (1½ circle), with the extended part of the rod to make the legs (side rods) of the splint (Fig. 2.20). The splint ring should be large enough to properly fit into the axilla or groin region without causing any harm to the bony prominences. Care is also needed to avoid exerting pressure on the scrotum in bulls and udder in dairy cows. The ring is bent at its middle to about 30–40° toward the inner/medial side, and the rod extending from the ring is cut to the limb length. The contralateral normal limb may be used to measure the normal length of the limb.
A second piece of the rod is bent to a U-shaped bar, cut to the length of limb, and fixed to the extended bars of the ring and to the ring itself using adhesive tapes or welded in case of iron/steel rods to provide adequate strength to the splint. The distal end of the splint may be welded to a steel plate, conforming to the hoof. The side rods are not generally bent but kept straight.
The ring is padded using cotton roll and bandages and secured using adhesive tape. The inner portion of the ring must be adequately padded to avoid pressure sores. The side bars of the splint may be padded with foam rubber pipe/cotton roll and bandages for insulation.
The limb is inserted into the ring and the distal end of splint (U-bar) is attached to the foot using the wires threaded through the hoof wall. The splint is firmly anchored in the axillary or groin region so that maximum load can be transferred. However, the limb is fixed to the splint with minimum traction (traction applied should only be sufficient to keep the limb extended and hold the bone segments in alignment) to avoid pressure sores at the contact points of the splint in the axillary or inguinal area and to prevent interference in venous drainage and locomotion.
The cast (preferably fiberglass/POP) is applied first directly over the fractured limb constructing a lightweight cast. Care is taken to prevent medial bowing of the limb by supporting the carpus or hock joint with a sling of plaster bandage. The cast is fixed to the splint using a casting tape, and the splint is then incorporated within the cast to make a splint-cast unit, which would help to prevent limb movement and rotation during locomotion.
In the forelimbs, the limb is attached to both side rods of the splint throughout the length, whereas in the hindlimbs, the thigh is attached to the cranial rod, the hock is attached to both side rods, and the limb below the hock is attached to the caudal side bar of the splint using a casting tape. Generally, the total cast material required is less (about 1/3 to ½ less) than the full-limb cast alone. It is better to extend the cast proximally up to the medial aspect of the ring to strengthen the splint and also to prevent the opposite limb from getting entrapped and to prevent urine and manure accumulation between the skin and the cast.
2.1.7.4 Postoperative Care, Management, and Complications
The animal must be assisted while getting up during the first few days until it learns to rise on its own without help, especially a heavy animal [13]. The animal must be watched frequently to make sure that it is not lying on the splint side. The animal must be inspected for any loosening of the cast around the fracture site leading to slipping of the splint, which can occur after the initial soft tissue swelling subsides. Refracture may be seen in some cases of slipped splint. Hence, in such cases, the splint-cast should be replaced. The animal must also be checked frequently for any injury or decubital ulcers in the flank and inguinal area under the ring; decubital ulcers may also occur due to prolonged recumbency and struggling to rise. They should be checked and treated properly. Splint-cast is kept in place for 6–8 weeks depending on the type and location of fracture and animal’s age and weight.
Laxity in the immobilized limb immediately after removal of the cast is common, which can be reversed gradually by regular exercise. Poor alignment and lateral deviation/outward rotation of the limb are common complications; however, it generally does not adversely affect the fracture healing and functional recovery of the limb.
2.2 Internal Fixation Techniques
Internal fixation of fractures by open reduction provides good alignment and rigid fixation of the bone segments. In small animal practice, internal fixation is the preferred method for fixation of long bone fractures, especially of the femur, humerus, and tibia. It can be achieved either by intramedullary fixation techniques like pinning/nailing or by extramedullary techniques like bone plating. Screws, wires, and staples are generally used as ancillary fixation devices along with plates and nails.
2.2.1 Intramedullary Pin/Nail
Intramedullary (IM) Steinmann pins are most commonly and widely used for fracture fixation in veterinary practice [21,22,23]. Nail/IM pin can be used either alone or along with other ancillary techniques like cerclage wiring. Due to their central position within the medullary cavity, IM pins can resist bending forces well and maintain alignment. Single IM pin cannot, however, resist compression and rotational forces. The technique of IM pinning is simple and needs minimum instruments, such as variable size Steinmann pins, Jacobs chuck with handle and key, and pin cutter in addition to the general surgical instruments. There are different types of IM pinning techniques.
2.2.1.1 Single IM Pin
It is indicated in simple transverse or slight oblique diaphyseal fractures of long bones (mostly the femur, humerus, and tibia). The pin can be introduced either by normograde technique (through one end of the bone) or by retrograde technique (through the fracture site) [21] (Fig. 2.21). In retrograde pinning, after exposing the fracture site through standard surgical incision, the fracture segments are identified and reduced either manually or using forceps. While separating and exteriorizing the bone segments, the bone ends are protected by covering with finger tips, so that the sharp bone ends do not damage the surrounding soft tissues and especially the vessels and nerves. At the exposed distal end of the proximal bone segment, a Steinmann pin of adequate diameter is inserted into the medullary cavity using a chuck until the pin exits the proximal bone cortex (Fig. 2.22). Subsequently, the chuck is reversed and the pin is withdrawn from the proximal end up to the level of fracture site. The bone segments are then aligned and the pin is driven into the medullary cavity of the distal bone segment until it reaches the distal metaphysis or epiphysis, where a resistance to pin insertion is felt. At this time, the chuck is removed, and the extra length of the pin is cut short at the proximal end using a pin cutter. The cut end of the pin is then pushed into the metaphysis/epiphysis by gently hitting the cut end of the pin using the T-handle. Rotating the pin at the point of final seatment should be avoided as it may loosen the pin and predispose to pin migration. Subsequently, the skin is drawn over the cut end of the pin and an interrupted suture may be applied.
Retrograde technique of IM pin fixation in the femur: (a) insertion of IM pin through the distal end of proximal fragment using a chuck; (b) the pin inserted through the proximal cortex; (c) the pin is withdrawn from the proximal end up to the level of fracture site; (d) the bone fragments are aligned and the pin is then driven into the distal bone fragment; and (e) the pin is seated in the distal metaphysis/epiphysis
In normograde technique of pinning, the Steinmann pin is inserted from one end of the bone. Normograde pinning is often done by closed/blind method in recent incomplete or simple transverse and sort oblique fractures with minimal displacement of bone segments after closed reduction [24, 25]. In long oblique/spiral and comminuted fractures, open reduction and fixation are always done. Once the pin reaches at the fracture site, the bone segments are reduced and the pin is then inserted into the medullary cavity of the opposite bone segment. The pin is driven up to the level of metaphysis and ensured that it is properly seated, and then, the extra length of the pin is cut close to the skin level.
There are some basic principles of IM pinning [23, 26]. One should not use pin fixation for non-reconstructable and unstable fracture configurations (comminuted fractures) and where uncontrolled loading is predicted. One should have a pack of large number of pins of different diameter and always select two pins of the same length, one pin for insertion and one pin to be used as a ‘measuring pin’ to estimate the depth of pin insertion in the medullary cavity. It is always better to select a smaller-diameter pin first, because we can easily remove and replace it with a larger pin, if needed. But if we use larger diameter pin first, it cannot be replaced by a smaller pin, and it may lead to pin loosening and migration. Assessment of pin seating can be done by (i) feeling resistance to further insertion, (ii) a measuring pin, or by (iii) radiographic examination. One should not cut and countersink a pin unless we are absolutely certain of its proper position, which can be confirmed by radiography or by image intensifier.
The retrograde pinning has the advantage of simpler passage of pin and easier selection of pin diameter, whereas normograde pinning has the advantage of accurate placement of pins and better purchase at the smaller bone segment (mostly used in metaphyseal/epiphyseal fractures). The diameter of the pin should be near to that of the medullary cavity, i.e. 70–90% of medullary cavity diameter (Fig. 2.23). The pin should run the whole length of the bone and then anchored at the distal metaphysis or epiphysis. The main limitation of single IM pin fixation is its inability to resist rotational forces and inability to hold the bone fragments in comminuted fractures. The use of full-cerclage or hemi-cerclage wires along with single IM pin provides greater stability against the rotational forces, especially in long oblique/spiral fractures.
2.2.1.2 Stack Pins
The use of more than one pin (of relatively small diameter) is indicated in transverse or slight oblique fractures of long bones to provide more stable fixation [27]. It is also indicated in long bones with relatively large medullary cavity, where a single pin cannot fill the medullary cavity adequately (calves and foals in particular). The use of more number of pins can snugly fit the medullary cavity and thus provide enhanced stability against shear and rotational forces [21]. Each pin is inserted through a separate proximal hole into the medullary cavity, preferably allowing the opposite ends of the pins to diverse within the opposite metaphysis (Fig. 2.24). This technique also cannot completely resist the rotational forces and sometimes may lead to pin loosening and migration.
Technique of stack pinning: (a) more than one pins (3–4) are inserted through the proximal fragment through separate holes in the cortex; (b) bone fragments are reduced and the pins are driven across the fracture line into the distal fragment; (c) if needed, one or two more pins are inserted between the multiple stack pins to snugly fit in the medullary cavity; and (d) all the pins are then seated in the distal metaphysis, and the extra length of the pins is cut short at the proximal end
2.2.1.3 Rush Pins
Rush pins, described by Dr. Leslie Rush, are solid curved cylindrical pins [22, 28]. Rush pin has a hooked end, which helps to drive and seat the pin in the bone, and another end is tapered that helps to bounce off the opposite inner cortex of the bone and thus prevent penetration of the bone cortex. Rush pins are indicated for the stabilization of metaphyseal/epiphyseal fractures of long bones, especially at the distal femur and proximal humerus or tibia. Two pins are passed from opposite sides (normally medial and lateral) of the cortex in the smaller bone segment (Fig. 2.25). The pins are inserted at about 30° angle to the long axis of the bone so that they cross each other above the fracture site and then glance off the endosteal surface of the diaphyseal bone to provide spring loaded tension. Bending the pins into a slight curve prior to insertion (prestressing) is useful to prevent penetration of the opposite cortex. Paired Rush pins held in spring loaded tension are expected to provide rotational stability. Rush pinning is contraindicated in very young animals, where the soft bony cortex (with relatively large medullary cavity) may get easily penetrated by the pin. Rush pinning may damage the growth plate leading to its rapid closure and shortening of the bone. Rush pins are also contraindicated in cases where there is longitudinal crack in the bone segment.
Technique of Rush pinning: (a) two proper size Rush pins are inserted on opposite sides of the small distal fragment, alternatively, at an acute angle (300) to the long axis of the bone to exit at the fracture site; (b) bone fragments are held in reduction and the pins are alternatively driven into large proximal fragment; (c) once the pins are driven completely, they glance off the opposite cortex and are held in spring loaded tension; and (d) the pin can be removed using Rush pin driver/extractor and a mallet
2.2.1.4 Cross IM Pins
Cross intramedullary pins (two small diameter Steinmann pins/K-wires) can also be used instead of Rush pins, and they are allowed to exit from the opposite end of the bone to facilitate pin removal in the later stage. This dynamic cross IM pinning using small diameter pins provides stable fixation of small fracture segments (mostly supracondylar femoral fracture or proximal tibial fracture) with minimal injury to the physeal plate [29, 30]. The technique of pin insertion and removal is easier than Rush pinning (Fig. 2.26). As the pins are inserted from the outer surfaces of the condyles, there is generally no interference with the extension and flexion of the joint. Further, the pins are crossed and remain in spring loaded tension; hence, fracture fixation is more stable with rotational stability, and pin migration is also rare.
Cross IM pinning of supracondylar femur fracture: (a) two relatively small diameter pins are inserted from opposite cortices of the small distal fragment, alternatively, at an acute angle (300) to the bone axis to exit at the fracture site; (b) bone fragments are held in reduction and the pins are alternatively driven into the proximal fragment so that the pins are crossed in the medullary cavity above the fracture site; (c) the pins are further progressed into the proximal fragment to glance off the opposite cortex and exit from the proximal end; and (d) the pins are withdrawn from the proximal end so as to seat into the distal end just below the articular surface; and (e) the extra length of the pins is cut from the proximal end
2.2.1.5 Kuntscher Nail
‘Clover leaf’ of ‘V’-shaped Kuntscher nails are hollow IM nails with an ‘eye’ at either ends [31]. They have the advantage of lightweight and can provide three-point fixation. They are indicated in transverse or short oblique fractures of the long bones, especially the femur, humerus, and tibia, where the cortex is good with no longitudinal cracks [22]. The technique is preferred in calves, foals, small ruminants, and large dogs, where medullary cavity diameter is large. The medullary cavity is first reamed using a reamer, and then using a guide wire, a proper diameter K-nail is introduced through one end of the bone (normograde technique, through the trochanteric fossa in femur), driven across the fracture site (after reducing the bone segments using bone clamps) and placed in the distal metaphysis (Fig. 2.27). It is important to cut the nail at one end (lower) to the desired length before insertion by measuring the length of the medullary canal (using preoperative radiograph or using a guide wire during surgery) so that the other end of the nail with the ‘eye’ will be left on the upper side to facilitate removal of the nail after fracture repair. K-nail is removed by a K-nail extractor, which is attached to the nail through the ‘eye’. K-nail extractor is a must during insertion of K-nail as well as for its removal.
Technique of K-nailing: the medullary cavity is reamed using a reamer (a); a guide wire (b) is introduced into the medullary cavity (which will help measure the length of the bone and also guide the insertion of the nail); a proper diameter and length K-nail (c) is inserted along the guide wire (normograde) using the K-nail driver (d) and mallet (e) and seated in the distal metaphysis; K-nail extractor (f) attached to the nail through the ‘eye’ facilitates extraction of the nail
2.2.1.6 Interlocking Nail
Interlocking intramedullary nail is a relatively new and an advanced device used mostly in human and small animal practice [32,33,34,35,36,37]; however, in recent years, it is becoming popular in large animal applications too [38,39,40,41,42,43]. The first interlocking nail (ILN) was described by the German surgeon Gerhard Küntscher in 1939. Johnson and Huckstep in 1986 first reported the use of ILN fixation in experimental dogs with comminuted femoral diaphyseal fracture, which required fluoroscopic guidance. Dueland and his colleagues from the USA in 1993 first reported the use of veterinary ILN system with an alignment guide (jig) for insertion of transverse locking screws. Since then, it is being used more frequently in small animal fracture fixation.
Interlocking nail is basically a cylindrical intramedullary (IM) nail with transverse cannulations secured (locked) in position by proximal and distal transfixing screws/bolts, which secure the nail to the bone cortex, thereby effectively neutralizing bending, rotational, and axial forces. It is performed using an image intensifier or a jig system.
Unlike a bone plate, the ILN allows biological osteosynthesis with minimal soft tissue trauma and vascular injury. Interlocking nail system is useful to repair simple and comminuted fractures of different long bones such as the humerus, femur, and tibia. Due to its mechanical advantages, the ILN provides rigid and stable bone fixation by neutralizing all the forces at the fracture site. As the implant is placed in the middle of the medullary cavity along the bone’s biomechanical axis (like IM Steinmann pin), it effectively counteracts bending force. As the nail is secured to the cortex using fixation bolts, it provides rotational stability (resists axial and rotational forces unlike IM Steinmann pins) and prevents collapse and overriding of bone segments at the fracture site. Intramedullary position of ILN, unlike eccentric placement of bone plates, makes it more resistant to compressive, torsional, and bending forces. By increasing the number of fixation bolts in each bone segment and the locking mechanism in the nail, the strength of fixation can be increased, which is particularly important in large animal fracture fixations. The ILN also allows dynamization at the fracture site in delayed or non-healing cases.
Different systems of interlocking nails are available today, such as regular interlocking nails (Dueland), angle-stable interlocking nails (Dejardin), inverse interlocking nails (Unger and Brückner, Germany), etc. However, the Dueland ILN system is the basic and first ILN system exclusively commercialized for use in veterinary practice and currently available commercially in India (Fig. 2.28).
The ILN is a solid steel rod with transverse openings usually at both ends. The one end of the nail has a trocar point to help in insertion and proper anchoring of the nail. The other end has negative threading (on the inner side), which helps to fix the alignment guide through the extension rod. The diameter of the nail generally ranges from 4 mm to 10 mm (Table 2.1), and any diameter nail can be custom-made. The lengths of 6–10 mm diameter nails vary from 120–230 mm, and 4 and 4.7 mm diameter nails vary from 68 to 134 mm. The number of holes in the nail vary from 3 (2 at one end and 1 at other end) to 4 (2 holes at both ends). The hole diameter varies from 2 to 4.5 mm. The holes are placed 22 mm apart in model 22 series (normally used for repair of diaphyseal fractures) and are placed 11 mm apart in 11 series (mostly used for repair of metaphyseal fractures). 4.0/4.7 mm nails are available only in the model 11 series.
Jig is an aiming device, which is fixed to the ILN using nail extension to facilitate correct placement of locking bolts/screws along the transverse openings of the nail without the need for image intensifier. The jig is attached to the nail with an extension so as to position it parallel to the nail with the jig holes corresponding to the nail holes. The nail extension, available as short or long extension, is temporarily attached to the nail to facilitate deep placement of the proximal nail end so that it does not protrude out of the bone once implanted. Locking screws (threaded)/bolts (smooth) are fixed in the cis- and trans-cortex of the bone through the hole in the nail, so that the nail is locked with the bony cortex and the bone and nail can act as a single unit.
Interlocking nails are commonly placed in different long bones, namely, femur, humerus, and tibia. The surgical approach for placement of ILN is same as IM pin fixation. The nail is introduced into the medullary cavity of long bones in normograde technique, either by closed or open approach (Fig. 2.29). Using a bone awl/Steinmann pin, a hole is created in the proximal bone cortex, which is enlarged with successively larger diameter reamers to a size that allows passage of the nail into the bone. The proper diameter nail with adequate length that can fit into the medullary cavity is chosen. A guide wire is passed in the proximal bone segment from the fracture site, so that it exits through the bone cortex and the skin at the proximal end. The nail attached to the jig is driven into the bone along the guide wire so that it is well seated in the proximal bone segment. Subsequently, the fracture segments are reduced, and the nail is further driven into the distal bone segment up to the level of metaphysis (till there is resistance to insertion). The holes for fixation screws/bolts are then drilled through predetermined sites by giving small stab incisions in the soft tissue and are directed through the bone and through the holes in the nail by utilizing the jig that aligns the drilling site with the holes in the nail.
Technique of interlocking nail fixation: using a chuck (a) fixed with Steinmann pin (b), a hole is drilled in the proximal cortex; the intramedullary cavity is reamed with a corresponding size reamer (c); a guide wire is introduced into the medullary cavity in normograde manner, and a proper length nail (d) is selected; before insertion of the nail, holes along the jig arm corresponding to the holes in the selected nail should be noted; the nail attached to the extension (e) insertion tool (g) and firmly anchored to the jig (f) is inserted into the medullary cavity along the guide wire; the jig-nail unit is rotated to align in medio-lateral plane (desired for screw/bolt placement); then, interlocking screws/bolts are fixed first by drilling holes by placing guide sleeve/drill guide (h) and drill bit (i) in the corresponding hole in the jig; the most distal bolt is placed first, followed by other bolts in proximal and distal fragments as per the situation. At the end of fixation, the jig along with extension-insertion tool is detached from the nail by unscrewing, so that the nail will remain within the bone
If the screws/bolts are fixed in both proximal and distal bone segments, the fixation is called static (load-bearing mode), which is commonly used in small animals, especially in comminuted fractures with instability. Two screws/bolts fixed on both bone segments provide stable fixation. When the screw/bolt is fixed in only one bone segment, either proximal or distal, it is called dynamic fixation (load-sharing mode) allowing micromotion at the fracture site. Dynamic fixation does not neutralize rotational and axial forces and weight-bearing results in axial compression promoting bone healing. In large animal fixations, as many fixation bolts as possible should be used in proximal and distal bone segments to provide greater stability. In fractures of the distal metaphysis/epiphysis of the femur, the nail can be introduced through the intercondylar fossa to achieve greater purchase in the smaller distal segment. In canine femur, 4–8 mm nails are generally adequate. In bovine femur and humerus, 14–18 mm diameter straight nails are optimum, whereas in the tibia, 12–14 mm angular nails are adequate.
General guidelines for ILN fixation include selection of proper nail (appropriate diameter, length, and model) based on preoperative radiographs of the fractured bone and the contralateral intact bone. A Steinmann pin is used to create a hole in the bone cortex, and it is then passed in a retrograde (in femur/humerus) or normograde (tibia) fashion to establish an intramedullary channel in the proximal bone segment. Intramedullary reaming is not generally required and may be avoided to reduce endosteal injury and cortical ischaemia. ILN should be tightly fit with the jig for proper alignment of holes in the jig and nail, and the holes in the jig through which fixation bolts (proximal and distal) need to be fixed should be ascertained based on the fracture location and configuration. The holes should not be drilled very close to the fracture site and should be at least 1 cm away. Undue pressure on the arm of the jig should be avoided while driving the nail (as it may lead to mal-alignment between the jig and nail) and ensure that the nail is properly seated in the distal metaphysis. Before drilling for transfixation bolts, if needed, the jig may be rotated to orient transfixation holes in the medio-lateral plane. The guide sleeve should always be used before inserting the drill/tap guides, and the holes are drilled using long drill bits without putting any pressure on the jig arm to ensure accurate drilling. A transfixation hole may be drilled in the proximal bone segment first, and the drill bit is left in situ to temporarily stabilize the jig to ensure accurate drilling in the distal bone segment. Before drilling any transfixation holes in the distal segment, it is ensured that the distal bone segment is rotationally aligned with proximal segment. After drilling at the most distal hole and inserting the drill bit in the distal bone segment, rotate the distal segment to ascertain that the distal drill bit has engaged the nail; if engaged, the nail will not rotate with the distal segment, and if not, the nail will freely rotate. Care should be taken while placing the distal-most screw as there is every chance for getting misplaced. It is better to fix two fixation bolts on both bone segments, but in distal metaphyseal fractures, at least one bolt/screw should be placed in the small distal bone segment. It is also advised not to leave an empty hole at the fracture site.
Interlocking nail can be placed in semi-closed manner; hence, soft tissue morbidity and vascular interference are lesser leading to biological osteosynthesis as compared to plating. It also permits early weight-bearing and return of limb function. The nail can be removed after bone healing, but it is not necessary to remove it if there are no complications.
The common complications with ILN include malpositioning of the nail in the medullary cavity leading to mal-alignment of the nail and jig and damage to the threaded proximal end of the nail. Misplacement of locking bolts/screws in the distal hole of the nail is also common. Other complications may include bending and breakage of screws and angular deformation of the nail. Complications of bone healing such as delayed union, non-union, and osteomyelitis can also be seen at times.
Hybrid ILN-ESF systems have been developed to improve the bending and torsional stiffness and overcome slack and interfragmentary movements. Type I ESF can be connected to ILN by tie-in configuration using an ILN extension or extended locking bolts. ILN can also be combined with epoxy-pin fixation using extended locking bolts. These hybrid fixators have the advantage of achieving dynamization at the fracture site by controlled destabilization. Further, it also facilitates easy removal of ILN after bone union. However, complications such as difficulty in postoperative care, poor patient tolerance, loosening of external pins, pin-tract infections, and additional soft tissue trauma offset the mechanical advantages of hybrid constructs. Attempts have also been made to combine ILN with bone plates (plate-ILN construct) to achieve maximum mechanical advantages of both implants in a single system so that all the forces acting at the fracture site can be more effectively neutralized.
The angle-stable ILNs have been developed to enhance the construct stability of the standard ILN by improving the torsional and bending deformation and by reducing slack and interfragmentary motion. The basic design of an angle-stable ILN is almost similar to standard ILN, with some modifications. The locking bolt has a threaded conical central part that matches with the shape and threads of the nail holes to create an angle-stable rigid fixation between the bolt and nail. The solid triangular end of the bolt is designed to engage the cis-cortex and is driven into the nail, and the thinner cylindrical end is designed to engage the trans-cortex. The locking bolts are available in different diameters, and they can be cut to appropriate length as per the requirement. The AS-ILN has been designed in an hourglass shape, which reduces damage to medullary circulation and increases overall construct stability. The core diameter of the nail is relatively less; hence, it is easy to insert without reaming the medullary cavity. The bullet-shaped distal tip of the nail minimizes tissue trauma, especially injury to the joint. AS-ILN is currently available in 6 mm, 7 mm, and 8 mm diameters, ranging in lengths from 122 to 203 mm.
Even though interlocking nail systems from different manufacturers are available for use in small animals, ILN systems for use in large animal fracture repair are not freely available commercially. Mostly, the implants developed for use in human applications are being used in large animals, but they are not strong enough due to their tubular designs, which compromise the fixation strength. However, a prototype of equine interlocking nail (manufactured by IMEX Veterinary, Longview, TX, USA) [44, 45] and bovine interlocking nails (Nebula Surgical Pvt. Ltd., Rajkot, India) [39, 41] for use in the humerus, femur, and tibia of young horses and bovines has been developed.
2.2.1.7 Interlocking Nails for Bovine
The ICAR-Indian Veterinary Research Institute has developed interlocking nails for fixation of fractures in bovine tibia and femur. The tibial ILN developed using 316L stainless steel has a diameter of 12 mm and length of 250 mm (Fig. 2.30). The nails are solid and have 9 holes, either all holes threaded or non-threaded (smooth), along its length to facilitate application to a variety of diaphyseal fracture configurations. The direction of holes is cranio-caudal. The nails are given a cranial angular bend of 10° at the proximal one-fifth of length to facilitate easy insertion and alignment with the medullary cavity of the tibia. Locking bolts are of 4.9 mm diameter (self-cutting trocar tip, self-tapping) and are either standard bolts (high pitch) for nails with non-threaded holes or a modified locking bolts (with low pitch), having two types of threads, the proximal part with threads complementary to hole threads to snugly fix the bolt with the nail in locking fashion (in nails with threaded holes) and the distal part with threading as of standard locking bolt (Fig. 2.31).
The nail-bone (buffalo tibia) constructs (with 10 mm mid-diaphyseal transverse ostectomy) developed using 4 or 8 standard locking bolts and 8 modified locking bolts were subjected to axial compression and 3-point cranio-caudal bending and torsion tests using a universal testing machine. ILN-bone constructs with 8 bolts were significantly stronger than the constructs with 4 bolts under compression, bending, and torsion loads [39]. The constructs with 8 modified bolts showed highest mechanical values. The compressive stiffness was 1.852 ± 0.04 MPa, yield load 18.475 ± 0.40 kN, and ultimate failure load 21.6 ± 0.39 kN. Bending moment was 419.03 ± 10.61 Nm, stiffness 0.583 ± 0.01 MPa, yield load 6.15 ± 0.17 kN, and ultimate failure load 6.33 ± 0.16 kN. Yield loads under compression and bending in constructs with modified bolts were significantly higher than in constructs with standard bolts. Under torsion, the constructs with 8 modified locking bolts showed ultimate failure load of 265.53 ± 10.23 Nm and ultimate failure displacement of 31.79 ± 0.82°. Both in vitro mechanical tests and clinical studies have shown that ILN developed for bovine tibia was sufficiently strong to stabilize diaphyseal fractures in young adult cattle and buffaloes weighing up to about 250–350 kg.
The ILNs developed for bovine femur (with solid or tubular shaft) measured 16 mm in diameter and 240 mm in length. The tubular nail has an inner diameter of 10 mm. The nails had 8 threaded holes (4 each in the proximal and distal part), for fixation of 6 mm locking bolts (Fig. 2.32). The nails were subjected to in vitro mechanical tests and clinical application.
For mechanical testing, nail-bone constructs were prepared using cadaver buffalo femur bones. The constructs developed using either solid or tubular ILNs (with eight 6-mm diameter, self-cutting trocar tip modified locking bolts, 40–75 mm length) with 5-mm mid-diaphyseal osteotomy were subjected to compression and cranio-caudal bending and torsion tests [41]. The compressive stiffness (MPa), yield load (kN), and ultimate failure load (kN) recorded for solid and tubular nails were 5.77 ± 0.23 and 5.35 ± 0.12, 46.89 ± 0.66 and 45.22 ± 0.86, and 51.39 ± 0.52 and 49.98 ± 0.51, respectively, with no significant difference between the solid or tubular nail constructs. The bending stiffness (MPa), bending moment (Nm), yield load (kN), and ultimate failure load (kN) for solid and tubular nail-bone constructs were 1.07 ± 0.05 and 0.86 ± 0.09, 680.55 ± 10.83 and 622.59 ± 23.13, 8.32 ± 0.25 and 7.36 ± 0.31, and 9.49 ± 0.28 and 8.18 ± 0.35, respectively (bending moment and failure load significantly different between the nail constructs). Under torsion testing, ultimate failure load (kN) and failure displacement (°) recorded for solid and tubular nail-bone constructs were 331.56 ± 4.87 and 312.48 ± 2.71 and 20.27 ± 0.39 and 18.33 ± 0.37, respectively (failure load significantly different between the nail constructs). These results suggested that solid nails were mechanically more stronger than tubular nails, but both solid and tubular nails were sufficiently strong to immobilize femur fractures in young adult cattle and buffaloes weighing at least 250–350 kg.
The interlocking nail provides rigid fixation of the bone allowing early weight-bearing and functional recovery of the limb. Additionally, the soft tissue morbidity is also minimal. The nail can be removed after bone healing, but it is not necessary to remove it if there are no complications. Non-availability of proper size and shape of the nail and the cost of the instruments, however, limit their routine use in large animal applications.
2.2.2 Bone Plate and Screw Fixation
Bone plate and screw fixation provides rigid and stable internal fixation, especially in unstable comminuted fractures [22, 46,47,48,49]. It also facilitates early mobilization of the joints leading to quick functional recovery of the affected limbs. Plates can be used to function in different ways (Fig. 2.33):
-
(i)
Neutralization plate: Here, the plate acts as a bridge to protect a comminuted area that has been constructed with lag screws. It transmits the force from one end of the bone to another via the plate, bypassing the area of fracture, and thus acts as a mechanical link between the main bone segments above and below the fracture site. It does not produce compression between the bone segments.
-
(ii)
(ii) Tension band plate/compression plate: Compression of the main segments of a fracture can result in absolute stability, with complete abolition of interfragmentary movement. By fixing the plate on the tension side of the bone (such as the lateral side of the femur, the craniolateral aspect of the tibia, the anterior aspect of the humerus, the anterolateral aspect of the radius, and the caudal aspect of the proximal ulna) (Fig. 2.34) and by the use of dynamic compression plate principle, compression can be achieved at the fracture site.
-
(iii)
(iii) Buttress plate: The plate is used to bridge a diaphyseal defect with a comminuted fracture or a gap filled with a bone graft or a substitute. Its function is to prevent the fracture from collapsing until the new bone fills the diaphyseal bone defect. The buttress plate is never applied under tension.
-
(iv)
(iv) Bridge plate: In comminuted diaphyseal fractures with severe soft tissue injury, a plate is often attached to the main bone segments spanning the fracture site. It is used to restore the bone length and alignment, even though fixation stability is less. This technique allows biological healing with external callus. Bridge plating is often performed by minimally invasive surgery.
Functions of plate: Neutralization, transmits the force from one end of the bone to another via the plate; compression, plate fixed in tension side of the bone or fixed in principles of DCP brings compression between the bone ends favoring bone healing; buttress plate, bridges the diaphyseal bone defect and thus prevents collapse and shortening at the fracture site; and bridge plate, the plate is attached to the main fragments spanning the fracture site and restores the bone length and alignment
Why should the plate be applied on the tension side of the bone? Normally, a long bone is subjected to bending stress (tension on one side and tension on the opposite side). If the plate is fixed on the tension side, compression occurs between the bone ends on opposite side favoring bone formation. If plate is fixed in compression side, gapping occurs on the tension side leading to fixation failure
There are four basic types of plates: (i) straight rigid plates for diaphysis, (ii) flexible/cuttable plates which can be easily contoured to the bone surface/cut to the desired length, such as reconstruction plates and veterinary cuttable plates, (iii) special plates like mini plate, ‘T’/‘L’ plate for the epiphysis and metaphysis of long bones, and (iv) special plates for specific applications like angled/hooked plates for the proximal and distal end of long bones like the femur, acetabular plate, tibial plateau leveling osteotomy (TPLO) plate, pancarpal and pantarsal arthrodesis plates, etc. Straight plates are most widely used for repair of long bone fractures in veterinary practice. Special T/L plates offer greater purchase in small segment fractures, as 2–3 screws can be easily fixed. Reconstruction plates are more often preferred in fractures of irregular bones such as the mandible and pelvis as these plates can be more readily contoured to the irregular bone surfaces.
The selection of bone plate is made carefully based on animal’s size and age, the bone involved, and the type and location of fracture (Table 2.2). Commonly, 2.7 mm and 3.5 mm plates are used in small animals; however, 1.5 mm and 2.0 mm plates are often used, especially in cats. In large animal applications, generally, 4.5 and 5.5 mm broad plates are utilized. Plates selected should be large enough to neutralize the forces acting at the fracture site but not too thick or heavy for the bone they cover. Before application, the plate should be contoured to the shape and curvature of the bone. Plates should be fixed using at least four cortices or two screws on both sides of the fracture site. There should be no gap between the bone and the plate and between the plate and screw head.
For application of plate, the fracture site is approached as per the standard procedure, and the soft tissue is then retracted along the whole length of the affected bone. Fracture segments are then reduced in their original position. After selecting a proper size plate, it is contoured to the bone accurately using a plate bender. The contoured plate is placed on the bone centered over the fracture and aligned along the axis of the bone and secured using bone-holding forceps. To ensure proper alignment of the plate along the axis of the bone, screws can be first fixed at either ends of the plate. Then, the fracture alignment can be re-checked before remaining screw holes are drilled and screws fixed. On the other hand, if plate-bone alignment can be easily ensured, the screws can be first fixed in the screw holes close to the fracture site on both sides of the fracture. The screws in the remaining holes of the plate are then fixed alternatively in both bone segments. Once all the screws are inserted, the correct alignment of the fracture segments is ascertained, and the screws are tightened one by one.
Screw holes in the bone are predrilled using a proper size drill bit, which is one size smaller than the screw size (Table 2.3). After drilling the hole in one of the screw holes, the screw length is measured by considering the plate thickness, and the proper length screw is chosen. If self-tapping screws are used, they can be directly inserted into the hole. If non-self-tapping screws are chosen, then the drill holes need to be tapped using a threaded tap (of same size as screw). Threads carved in the tap are sharper than the screw threads, and tapping helps to clear the bone debris and facilitate screw insertion. Tapping also reduces the heat generation during the screw insertion.
2.2.2.1 Dynamic Compression Plate
Dynamic compression plate (DCP), first introduced in 1969, is an improvised plate having special oval holes unlike traditional plates with round holes. The DCP allows achieving axial compression at the fracture site (without a tension device) by eccentric placement of screws. When a screw is tightened along the sloping design of the oval screw hole, the plate moves away from the fracture resulting in compression of the bone segments [50,51,52,53,54,55].
A DCP is applied by drilling a hole in one of the bone segments (say, proximal segment) close to the fracture site (about 1 cm away) using a neutral guide, and the plate is then secured by inserting a screw. Another screw hole is then drilled eccentrically in the opposite bone segment (say, distal segment) close to the fracture with the aid of a loaded (eccentric) drill guide (Fig. 2.35). Insertion of screw through the eccentrically drilled hole and tightening against the slope of the screw hole result in self-compression of fracture by displacing the plate. The remaining screws are then inserted alternatively in the proximal and distal bone segments using the neutral drill guide. It is also possible to use more than one eccentrically placed screw on either side of the fracture. Before the second compression screw is tightened, the first screw has to be loosened to allow the plate to slide and achieve compression at the fracture site; the first compression screw is then tightened.
In dynamic compression plating, a hole is drilled in the center of the screw hole close to the fracture site in the proximal bone fragment using a neutral guide, and the plate is then secured by inserting a screw. An eccentric hole is drilled in the screw hole in the distal bone fragment close to the fracture site with the help of an eccentric drill guide. As the screw is inserted and tightened through the eccentrically drilled hole, the fracture is self-compressed by displacing the plate. The remaining screws are then inserted alternatively using the neutral drill guide
Bone plating requires complete exposure of the fractured bone, sometimes leading to disruption of soft tissue attachments and hence vascular compromise at the fracture site. When the plate is rigidly fixed, it may protect the underlying bone from loading stresses. This ‘stress protection’ along with vascular compromise may lead to weakening of the bone (osteoporotic). In recent years, limited contact dynamic compression plates (LC-DCPs) have been developed [52, 54, 56]. These plates are designed to reduce the contact between the plate and the bone with the presence of undercuts beneath and between the screw holes. This in turn reduces the stress protection and vascular compromise and thus allows periosteal callus formation at the fracture site. In LC-DCP, the holes are symmetrical, which allows eccentric placement of a screw in either direction. It helps to achieve compression at any level along the plate and thus facilitate treatment of a segmental fracture. LC-DCP also allows relatively more inclining of screws (40°) along the longitudinal direction than a DCP (25°). LC-DCPs are now being used more frequently in clinical practice than before.
The DCPs are available for small animal use in a variety of sizes like, 2.0, 2.7, 3.5, and 4.5, which are used with 2 mm, 2.7 mm, 3.5 mm, and 4.5 mm cortex screws, respectively. 4 mm cancellous screw can be used with DCP 3.5, and 6.5 mm cancellous screw can be used along with DCP 4.5. Whereas in large animal applications, 4.5 or 5.5 broad DCPs are used, broad DCPs are wider and thicker than standard DCPs (4.5 mm broad DCP has a width of 16 mm and thickness of 4.8 mm as against 13.5 mm width and 4.2 mm thickness of standard narrow DCP) and have staggered screw holes. In heavy large animals, double plates are recommended for fixation of fractures in load-bearing bones. Though plates have been developed specifically for use in large animal orthopedics, they are not readily available. Compression can also be obtained with any of the straight plates by using a compression device (Fig. 2.36). Here, a suitable length plate is used across the fracture site and is fixed to one (proximal) fracture segment using one or more screws. At the opposite (distal) end of bone segment, the compression device is fixed using a small cortical screw and is anchored with the last screw hole. As the screw in the device is tightened, the plate is pulled toward the device achieving compression between the fracture segments. Subsequently, the screws are fixed in the remaining holes of the plate, and then, the compression device is removed by loosening the small screw fixing the device.
The use of a compression device to achieve compression between fracture fragments: (a) a plate is applied across the fracture site and is attached to the proximal fragment with 2–3 screws, and at the opposite end of fracture fragment, the compression device is fixed with a small cortical screw and is attached to the last screw hole; (b) the compression device is tightened to bring the two bone fragments closer; (c) with the fragments in the proper position, the screws are fixed in the distal aspect of the plate; (d) the device is then detached by removing the small screw
Plate luting: Fixation stability with a bone plate is achieved from friction between the plate and the bone, and therefore, it is directly proportional to the extent of plate contact with the bone cortex. The technique of ‘plate luting’ has been developed to obtain maximum plate-bone contact, through interfacing a layer of bone cement between the plate and the bone. Plate luting is mostly used in large animal fixations to achieve greater fixation strength [57, 58]. The technique involves placement of all screws in the plate first, and then, the screws are loosened to lift the plate off the bone. PMMA dough (incorporated with a broad-spectrum antibiotic) is filled between the bone and the plate, and all the screws are soon tightened, and the excess spilled cement is removed. Hardened PMMA cement, filled between the plate and screws and in the screw holes around the screw heads, provides stable plate-bone fixation. While applying PMMA dough, care should be taken to prevent penetration of bone cement into the fracture line, which may hamper bone healing. Further, as hardening of PMMA (polymerization) is an exothermic reaction with releasing of heat, the bone and the implants have to be cooled using cold saline solution during the process.
2.2.2.2 Veterinary Cuttable Plate (VCP) and Reconstruction Plates
Veterinary cuttable plates are special plates that can be customized for use in bones of varied length by cutting them to desired length [59, 60]. VCP is not a compression plate. They are available in two sizes: small plates can accommodate 1.5 mm and 2.0 mm screws, and larger plates can accommodate 2.0 mm and 2.7 mm screws. The length of plate is 30 cm having 50 round holes. As these plates are relatively weak, they can be used only in small animals with simple fractures.
Reconstruction plates are flexible plates, which can be contoured in two planes [61]. The presence of deep notches between the screw holes makes them relatively flexible but much weaker than standard bone plates. The different sizes of plates available are 2.7, 3.5, and 4.5. The plates have oval holes, which allow for compression between the bone segments. Reconstruction plates are particularly useful for fixation in pelvic fractures, mandibular fractures, and distal humeral or femoral fractures.
2.2.2.3 Special and Mini Plates
Special T- and L-plates are available in variable sizes (2.0, 2.7, and 3.5) for veterinary applications. Other special plates include acetabular plates (2.0 and 2.7) [62, 63], hook plate for proximal femoral fracture, tibial plateau leveling osteotomy plate, pantarsal and pancarpal arthrodesis plates, and tubular plates for bones with minimal soft tissue coverage and osteoporotic bones, etc. Small fragment mini plates are also available in variable sizes (1.0, 1.3, 1.5, and 2.0), shapes, and lengths as T-plate, L-plate, round-hole plate, cuttable plate, and DCP [64]. Generally, self-tapping screws are used. Mini plates are commonly used for fractures of the mandible, maxilla, metacarpals, and metatarsals in small breed dogs and cats.
2.2.2.4 Locking Plate-Screw Systems
Locking plate-screw system, a more recent concept, is a bone plate having threaded screw holes that allow locking head screws to snugly fix into the plate. This combination of plate and screw functions as a fixed-angle device [65,66,67,68,69,70,71,72]. Locking plate systems have several advantages over other conventional plating systems. The locking plate is biomechanically superior to traditional DCP [73, 74]. In the DCP, friction at the bone-plate interface brings about compression of the plate to the bone; as the axial load is increased, the screws may start toggling and loosening, leading to fracture instability and implant failure. Thus, it is difficult to attain and maintain adequate screw-plate stability, especially in unstable comminuted fractures and in metaphyseal and osteoporotic bones. The conventional plate fixation may also compromise the periosteal circulation and vascularity at the fracture site. The locking plate need not be in close contact with the underlying bone; hence, perfect contouring of the plate is not essential. Thus, reduced contact between the plate and the bone can help preserve the periosteal circulation and reduce osteoporosis underneath the plate. The locking plates do not cause friction between the plate and the screws, and the angularly stable screw-plate interfaces provide stable fixation. In other words, the locking plates act as external fixators positioned under the skin with little distance between the bone and plate, providing more stable fixation. Further, the screws need not be fixed through both bone cortices (can only be fixed in the near cortex); it allows locking plates to be used in a variety of applications like in mandibular and acetabular fractures and in double plate fixations.
2.2.2.4.1 Locking Compression Plate
Innovation of locking compression plate (LCP) is the presence of combi holes to allow fixation of either locking head screws or conventional non-locking screws (Fig. 2.37). The locking compression plates with combi holes are available in standard DCP/LC-DCP sizes of 3.5, 4.5, and 5.5. Combi hole has one part similar to standard compression plate that allows fixation of conventional screw allowing compression or an angled lag screw [65]. The other part of the hole is threaded, which allows fixation of locking head screw exactly at perpendicular to the plate, providing angular stability. Special threaded drill guide, which can fix to the hole threads, facilitates precise drilling for fixation of locking screws. Depending on the situation and function, the plate can be used as a compression plate or a fixed angle internal fixator. Locking head screws are available in two forms, either only self-tapping screws (for fixation in unstable fracture conditions) or self-drilling and self-tapping screws (for unicortical fixations). Locking screws have smaller threads (as there is no need to achieve compression between the plate and the bone) and have a larger core diameter (ensures greater bending and shear strength). Locking screws are designed with new Stardrive head, which can withstand 65% greater insertion torque than conventional hexagonal head, and it is also self-retaining (screw stays on the screwdriver).
Locking compression plates can be used to treat most of the fractures where plating is indicated, especially in unstable conditions. In small animals and in sheep and goats, 2.7/3.5 plates can be used to immobilize the fractures of different long bones such as the femur, humerus, tibia, and radius-ulna, apart from the mandibular, pelvic, and spinal fractures. In large animals (horses, cattle, and buffaloes), diaphyseal fractures of the tibia and radius are more amenable to plate fixation, although they can also be used to treat certain fractures of the femur, humerus, metacarpus, and metatarsus using 4.5/5.5 broad locking compression plates.
2.2.2.4.2 Locking Plate (UniLock)
The UniLock locking plate has round holes with locking mechanism for fixation of locking head screws [75]. This is available in two systems, 2.0 (allow 2.0 mm locking screws) and 2.4 (allow 2.4 and 3.0 mm locking screws), which allow fixation of self-tapping locking screws. Locking screws are fixed perpendicular to the plate using special threaded drill guide. The UniLock plates can be particularly useful in mandibular and pelvic fractures and small bones of dogs and cats.
2.2.2.4.3 String of Pearls (SOP) Plate
SOP plate with locking mechanism is a unique fixation system; mechanically, it acts as an internal external fixator [70]. Its design allows the use of cortical screws as locking screws and allows contouring in six degrees of freedom (medio-lateral bending, cranio-caudal bending, and torsion) with high bending strength. The SOP plate is narrower but has greater moment of inertia than DCP, LC-DCP, or LCP of similar size. Mechanically, the bending strength of SOP is 30–50% greater than conventional plates.
Basically, the plate has two components, cylindrical and spherical, arranged alternatively. The cylindrical component (internode) is designed to contour the plate by bending or twisting. The spherical component (node) is designed to accept the head of a standard screw; as the screw head is tightened, the screw threads get locked along the threads carved within its deeper part to provide rigid fixation. Both bicortical and monocortical screws can be fixed in SOP plates.
SOP plates are available in two sizes, 2.7 and 3.5. As it can be bent and twisted to contour to the shape of the bone, it has a variety of clinical applications like long bone fractures, pelvic and acetabular fractures, and spinal fractures. Bending and twisting, however, reduce the plate strength (twisting should not be more than 20° per internode). SOP plate cannot be used to achieve compression but can be used as a buttress or neutralization plate.
2.2.2.4.4 Clamp-Rod Internal Fixator (CRIF)
The CRIF is another versatile system, which consists of a rod, clamps, and standard screws. It can be readily contoured to the bone surface and easily applied with minimal instrumentation, and it is relatively economical [43, 76,77,78]. CRIF system favors vascularization at the fracture site as only the clamps placed along the rod touch the bone. Clamps can be arranged on either side of the rod contouring to the outer surface of the bone to provide rigid fixation. Tightening of screws allows firm fixation of the clamps to the rods. The available CRIF systems can utilize 2.0, 2.7, 3.5, and 4.5 mm screws, for use in different long bones of small animals and young large animals.
2.2.2.5 Contoured Locking Plates for Bovines
The novel locking plates specifically contoured to different long bones such as the radius, femur, and tibia (designer plates) have been developed by the Indian Veterinary Research Institute, using 316L stainless-steel alloy for use in large bovines [41, 79, 80]. The plates are contoured to the cranial surface of the radius, craniolateral surface of the femur, and craniomedial surface of the tibia. The screw holes are placed in two rows and are directed in different planes to facilitate proper placement and fixation of screws in the bone cortex and also to provide greater fixation stability.
The contoured plate developed for the radius has a length of 180 mm, thickness 4.5 mm, and width 32 mm (Fig. 2.38). The plate has 7 combi holes on medial and lateral border each, and the distance between the two screw holes (longitudinal) is 15 mm. Curvature of the plate (arc) is 45° (1/8th of circle). The plate has two additional locking holes at both ends between the two rows of combi holes. Both rows are angled at each other at about 40° to prevent penetration of medial and lateral radial surfaces during screw fixation.
The locking plate developed for the femur has a length of 180 mm, thickness 4 mm, and width (straight) 35 mm at proximal and distal portions and 32 mm at the central portion (Fig. 2.39). The number of combi holes on medial and lateral border is 8 each, and the distance between the two screw holes is 25 mm, whereas the distance between the screw holes on the same border (longitudinal) is 10 mm. The medial border of the plate is straight, whereas the curvature of the plate on the lateral border (arc) is 45° (1/8th of circle), which is nearly flattened at the distal end. The plate has two additional locking holes, one at either ends, between the two rows of screw holes. The holes on both rows are placed alternatively and angled at each other at about 40° to prevent collision and proper purchase of screws in both bone cortices (cis- and trans-cortices) during screw fixation.
The locking plate developed for the tibia has a length of 240 mm, thickness 5 mm, and maximum and minimum width of 55 mm and 24 mm (Fig. 2.40). The number of holes on the cranial and caudal border is 8 and 7, respectively. The distance between two screw holes (longitudinal) is 15 mm. The tibial plate has three additional combi holes in between the two rows of screws. The first five screws in the craniomedial row are at an acute angle to the screws of caudal row to allow the craniomedial screws to enter the far cortex without penetrating through the lateral surface of the bone.
The threaded component of combi holes in all the plates can accept 5.0 mm locking screws with a core diameter of 4.4 mm and a thread pitch of 1 mm. The oval component can accept 4.5 mm cortical screws with a core diameter of 3.0 mm, thread pitch of 1.75 mm, and head diameter of 8 mm.
The novel locking plates developed for different bones were subjected to in vitro mechanical tests using plate-bone constructs developed using buffalo cadaver bones. In the radius, mid-diaphyseal transverse osteotomy model was used; in the tibia, a long oblique osteotomy was used; and in the femur, a transverse ostectomy with a 5 mm gap was used to develop bone-plate constructs. Different locking plate-bone constructs were subjected to axial compression and cranio-caudal 3-point bending and torsion (only femur constructs) tests and compared with different plate-bone constructs such as non-locking plate-bone, single locking plate-bone, and double locking plate-bone constructs using a universal testing machine. For compression testing, specimens were loaded in compression at a constant actuator displacement rate of 10 mm/sec until failure; for bending, the central load support contacted the cranial aspect at the center of the specimen, and load was applied at 10 kN per second until failure. For torsion testing (0–2000 Nm TTM), with the longitudinal axis of the femur aligned along the axis of rotation, each bone or construct was externally rotated, so that the cranial aspect of the femur moved medially relative to the mid-shaft, at 5°/sec until failure occurred.
The novel locking plate-radius constructs under compression showed mean (±SE) stiffness of 3.59 ± 0.47 MPa, yield load of 22.65 ± 2.03 kN, and ultimate failure load of 22.65 ± 1.91kN. Under the bending test, the mean (±SE) bending moment was 514.07 ± 55.06 Nm, stiffness 0.61 ± 0.09 MPa, yield load 8.73 ± 0.95 kN, and ultimate failure load 10.82 ± 1.16 kN.
The novel locking plate-femur bone constructs showed 5.19 ± 0.15 MPa stiffness, 45.13 ± 0.76 kN yield load, and 49.31 ± 0.57 kN ultimate failure load under compression. Under bending, mean (±SE) stiffness was 0.93 ± 0.08 MPa, bending moment 620.00 ± 24.56 Nm, yield load 7.09 ± 0.50 kN, and ultimare failure load 8.51 ± 0.45 kN. Under torsion, mean (±SE) ultimate failure load was 245.64 ± 4.47 kN and ultimate failure displacement was 21.66 ± 0.48°.
The novel locking plate-tibia constructs exhibited mean (±SE) compressive stiffness of 4.0 ± 1.04 MPa, yield load of 24.07 ± 3.45 kN, and ultimate failure load of 25.85 ± 4.32 kN. The mean (±SE) bending moment was 565.37 ± 79.3 Nm, stiffness 0.58 ± 0.11 MPa, yield load 7.9 ± 1.14 kN, and ultimate failure load 9.83 ± 1.38 kN.
The novel locking plates designed and developed for fixation of different long bones of a bovine were well contoured and could fit well on the respective bone surfaces. Fixation of the bone with contoured locking plate was mechanically stronger than the standard single locking compression plate fixation and was almost as strong as double plate fixation. These contoured locking plates look promising to treat long bone diaphyseal fractures in adult cattle and buffaloes, which are otherwise difficult to treat by conventional plate fixation. However, they need to be tested in more number of cases in a variety of clinical settings.
Locking plates have certain limitations. Fracture has to be properly reduced before fixing the plate, as the bone segments cannot be manipulated once a locking screw is fixed through the plate. The cost of locking plates is also more than conventional plates, which may limit their use in routine veterinary practice.
2.2.2.6 Minimally Invasive Percutaneous Plate Osteosynthesis (MIPO)
In recent years, more focus in fracture repair has been given on minimally invasive fixation techniques. After the advancements in the development of rigid fixation systems such as LCP, a new technique of fracture fixation, i.e. less invasive stabilization system (LISS) or minimally invasive percutaneous osteosynthesis (MIPO), is gaining popularity [81,82,83,84].
In MIPO, a bone plate is fixed through two small incisions made away from the fracture site and hence referred as percutaneous plating (Fig. 2.41). As the fracture site is not directly exposed and minimally disturbed, this technique allows biological bone healing. In this technique, a bone plate is fixed in the proximal and distal bone segments in a bridging fashion across the fracture site. The bone segments are first reduced by closed or indirect methods. Two small skin incisions are made one on either end of the fractured bone, and using a blunt instrument such as artery forceps, a subcutaneous tunnel is created between the soft tissues and the periosteum connecting the two incisions. The plate is then inserted through one of the incisions along this tunnel, sliding across the fracture site on the periosteal surface of the bone, toward the opposite incision. The plate is aligned along the bone and screws are fixed at both ends of the plate through the insertion incisions, and if needed, additional stab incisions are made to fix more screws. Usually, only 2–3 screws are fixed at both ends of the plate leaving the screw holes at the center blank (bridge plating).
MIPO has the advantage of reduced operative time once familiar with the procedure. It lowers the risk for bacterial infection due to decreased duration of surgery, limited soft tissue trauma, and reduced fracture site contamination. It preserves the haematoma formed at the fracture site contributing to early callus formation and bone healing. MIPO also causes minimal damage to the periosteal vascular supply in comparison to conventional plating, which in turn may hasten fracture healing. With MIPO, the postoperative pain is relatively lesser, and the fracture healing is more rapid than traditional plating due to minimal skin incision and manipulation of bone segments. Even though MIPO has similar advantage as external skeletal fixation in terms of fracture healing, postoperative care of patient is less with MIPO.
The main disadvantage with MIPO is that the technique is difficult and challenging to learn and apply. Further, it may not be suitable for fractures requiring more rigid and stable fixation, especially in small segment fractures, and in articular fractures which require precise anatomic reduction and interfragmentary compression. With MIPO, fracture site cannot be directly visualized, and therefore, there is a need for intraoperative fluoroscopy or radiography, which may increase the risk of radiation exposure for both the patient and the surgical team.
2.2.3 Ancillary Fixation Devices
2.2.3.1 Screws
Screws have been used in many ways in orthopedic applications [7, 46, 47, 49, 54] (Fig. 2.42). Generally, screws are not used as sole fixation devices as they cannot resist bending, rotation, or axial loads. They are used as ancillary fixation devices along with primary fixation devices such intramedullary pins/nails or bone plates, where screws can stabilize the fracture and keep the bone fragments in anatomic alignment. The screw is often used to provide compression between the bone segments, so that the fractured bone can heal faster. Any screw used to bring interfragmentary compression is called as a lag screw, which not only reduces the gap between the fracture segments but also decreases the stress on the primary fixation implant. Usually, half-threaded screw is used as lag screw, wherein the near cortex is over-drilled automatically leading to compression of bone segments while tightening the screw. If fully threaded screw is used as lag screw, the near cortex must be over-drilled to achieve compression (Fig. 2.43). If the compression is achieved by the fixation device alone, it is called static compression, and if the body weight or muscle force is utilized to achieve additional compression, it is called dynamic compression.
Application of lag screw: in fully threaded cortical screw (a), the near cortex must be over-drilled to achieve interfragmentary compression, whereas in half-threaded cancellous screw (b), the near cortex is automatically over-drilled while tightening the screw which brings about compression between the fragments
Screw can be either cortex or cancellous type. Cortex screws, which are designed to anchor in the cortical bone, have fine threads (with relatively larger core diameter and smaller pitch) along their shaft. Cortex screws are commonly available in sizes varying from 1.5–5.5 mm (1.5, 2.0, 2.5, 3.5, 4.5, and 5.5 mm) in diameter with varied lengths. Most frequently used 3.5 mm cortex screw has a 6 mm head with a 3.5 mm hexagonal recess, the outer thread diameter is 3.5 mm, and the core diameter is 2.4 mm, whereas cancellous screws having coarse threads (with lesser core diameter and larger pitch) are designed to anchor in softer cancellous bone. A 3.5 mm cancellous screw has an outer thread diameter of 3.5 mm and core diameter of 1.9 mm. Cancellous screws can be fully threaded or half-threaded having a smooth unthreaded portion, which is normally used as a lag screw. Locking head screws, used along with locking plates, have core diameter larger with smaller threads than standard bone screws; the pitch of the screws is also smaller, and it matches with the pitch of the threads on the screw head. A 3.5 mm locking screw typically has thread diameter of 3.5 mm and core diameter of 2.9 mm with 1.24 mm thread pitch.
Screws can be self-tapping or non-self-tapping. Self-tapping screws are designed to directly insert into a predrilled hole in the bone, without tapping (creating threads in the bone). Self-tapping screw can allow withdrawal and reinsertion through the predrilled hole without losing its grip; but if misdirected, it can damage the previously cut threads. Hence, it is inappropriate to use self-tapping screw as a lag screw, whereas non-self-tapping screws require cutting threads in the predrilled hole in the bone using a tap having sharp threads corresponding to the profile of screw threads, before their insertion. These screws can be withdrawn and reinserted without fear of accidentally cutting a new track, as it is unable to cut threads in a dense bone. Self-drilling self-tapping screw can cut through the bony cortex and is designed for use in locking plate systems for unicortical fixation.
Generally, solid screws are used; however, cannulated screws with a hollow shaft are often used in specific applications. Cannulated bone screws are available in sizes 3.5 mm and 6.5 mm. The cannulated screw can be placed at exact location using Kirschner-wire as a guide. A small K-wire is first drilled across the fracture line, usually under C-arm fluoroscopic visualization, and the cannulated screw is then slid along the wire down into the bone using a special driver. Care should be taken not to penetrate the articular surface while placing the screw in the subchondral bone near the joint. The K-wire is then withdrawn to complete the procedure. Cannulated bone screws can be used as lag screws particularly in the metaphyseal or epiphyseal fractures of the distal humerus and distal or proximal femur.
2.2.3.2 Wires
Kirschner- or ‘K’-wires are handy orthopedic devices used in many different ways for reduction and temporary or final stabilization of fractures. They are also used as guide wires during the application of cannulated screws or nails. The difference between a pin and a wire is their diameter. Pins are between 1.5 mm and 6.5 mm in diameter, whereas Kirschner-wires are between 0.9 mm and 1.5 mm in diameter. K-wire is used to reduce comminuted bone segments before the placement of primary fixation device, to stabilize small bone segments or as a primary intramedullary device to immobilize a long bone fracture [85]. K-wires can also be used in a crossed fashion (cross pinning or cross IM pinning) to help stabilize fractures at the epiphyseal/metaphyseal region of long bones, as in cases of supracondylar femoral and humerus fractures or in proximal tibial fractures in young animals. The main advantage with a K-wire is that as it is very small, the fixation is minimally invasive and non-traumatic. Hence, it can be placed safely through an articular surface or across an open physeal (growth) plate without causing significant injury. K-wires are also widely used in external skeletal fixation systems, especially in circular fixators, which use relatively small diameter pins.
Orthopedic wire is available on a spool or in individual preformed loops (eyelet wires). It is used most widely as an adjunct to IM pinning or bone plating to provide rotational stability [7, 21]. Generally, 0.6–1.2 mm (18–24 G) thick wires are used in small animals and 1.2 to 2.0 mm (14–18 G) wires in large animal fixations. It can be used either as full-cerclage wire or hemi-cerclage wire [26, 86, 87].
The full-cerclage wire is placed around the circumference of the bone, generally to hold small fracture fragments together in a comminuted fracture or to achieve compression between long oblique/spiral fracture segments (Fig. 2.44). Spool wire is cut to the desired length and the cut ends are secured by twisting with pliers, needle holders, or special twisting instruments. While passing the wire around the bone, care should be taken not to entrap any soft tissue. A needle holder or a wire passer can help in safe passage of the wire. The wire should be firm, and even tension should be applied along the two ends during twisting to ensure proper intertwining of the two cut ends, instead of twisting one wire end around the circumference of the other (Fig. 2.45). The wire is usually cut at the third or fourth twist. It is advised to bend the twist knot down along the bone surface to prevent possible injury from the protruding wire to any surrounding neurovascular structures (Fig. 2.45b). However, one should remember that bending causes a 30% loss of wire tension. On the other hand, loop knots have been shown to produce a greater wire tension than twist knots. In this technique, the preformed (eyelet) loop wire is placed around the bone, and by taking through the eye loop, it is tightened using a special tightening instrument. After achieving the desired tension, it is bent over the loop along the bone surface and cut about 2–3 cm from the eye loop. Twist-knotted wires provide greater resistance to knot failure than single-loop knotted eyelet wires, but final wire tension (thus compression) on the bone is greater with loop-knotted wire. A double-loop knotted wire provides greater final wire tension and resistance to knot failure.
Cerclage wires should be used to stabilize only reconstructable fractures (long oblique or spiral fractures or single large butterfly fragment). Wires should not be used if the bone is not cylindrical in shape. Monofilament wire with sufficient strength should be used, and braided wire should never be used. A minimum of two cerclage wires should be applied and are placed at least 0.5 cm (or half the bone diameter) away from the fracture line and spaced approximately 1 cm (or bone diameter) apart. The wire is always placed perpendicular to the bone’s axis directly on the periosteum without interposition of the soft tissues. All wires are placed and tightened before closure. To prevent slip of wire and subsequent loosening, the wire may be passed and secured through a hole drilled in the bone cortex or secured by notching the cortex or placing a small K-wire.
Properly tightened and applied cerclage wires do not interfere with the blood supply to the underlying cortical bone. Likewise, cerclage wires can also be placed around immature bone without disrupting bone growth. However, loose wires shift back and forth along the cortical bone and disrupt the blood supply by damaging the periosteal vessels and compromising blood flow through the bony cortex and predispose to infection.
Hemi-cerclage wires are used to counter the rotational or shear forces in transverse and short oblique fractures. The orthopedic wire is passed through a hole drilled in the bone so that it only partially encircles the bone. The wire is placed before the fracture is reduced and tightened after fracture reduction. Tightening of hemi-cerclage wire should be just enough; excessive tightening may distract the fracture on the opposite cortex. If distraction is suspected, another hemi-cerclage wire can be used on the opposite side. Hemi-cerclage or full-cerclage wires can also be used to reduce the fracture and keep the bone segments in alignment during primary bone fixation with IM nail/plate and screws, especially in severely displaced/comminuted fractures of long bones such as the tibia.
Orthopedic wire can also be used for stabilization of avulsion fractures (especially of os-calcis and olecranon) to counteract tension force (Fig. 2.46). Here, two holes are drilled at the center of the bone in the proximal and distal bone segments, medio-laterally almost equidistant from the fracture line. Two wire pieces (long enough to approximate and twist the opposite ends) are then passed, one each through the proximal and distal holes. Subsequently, they are tightened uniformly on both sides in the form of figure eight wire or as a mattress suture. This type of fixation is particularly useful in fractures with small bone segments, especially in young lightweight animals. However, one should be careful not to put undue tension on the wires, which may cut through the soft bone of young animals.
Tension band wire: It is indicated for the treatment of avulsion fractures, wherein the avulsed bone segment is constantly subjected to distraction/tensile force through the attached muscle, tendon, or ligament. Tension band wires not only counteract the tensile force acting on the avulsed bone segment but also bring about compression between the fracture segments. Common fractures that are amenable to tension band wiring are that of thw olecranon, greater trochanter, patella, tibial tuberosity, and os-calcis [88, 89].
Tension band fixation consists of dual K-wires that fix the avulsed bone fragment back to the shaft and orthopedic wire that passes through a hole in the distal bone segment and behind the cut ends of K-wires twisted in a figure of ‘8’ form (Fig. 2.47). Twists are placed on each side of figure of 8 wire and loops are tightened simultaneously [90] (Fig. 2.47b). The purpose of K-wires is to maintain fracture alignment and provide rotational stability; the figure of 8 cerclage counteracts the tensile forces of the tension attachment on the avulsed bone and converts these forces into vectored forces that compress the fracture as the animal bears weight. Tension band wires should be avoided in places where it involves active growth plate as it may cause premature closure of the growth plate (if used, it should be removed within 4 weeks).
2.2.3.3 Postoperative Care and Management with Internal Fixation
Postoperatively, broad-spectrum antibiotics and non-steroidal anti-inflammatory/analgesic drugs should be given for 3–5 days. The antibiotic coverage may be extended if inflammation persists or infection develops. Prolonged use of anti-inflammatory drugs should be avoided as they may hinder bone healing.
Post-surgery, the animals should be restricted to cages/stalls, for the initial 2–3 weeks. Only minimum weight-bearing should be allowed on the operated limb, to prevent any complications. In cases of small animals, generally, the internal fixation provides rigid and stable bone fixation, and chances of implant/fixation failure are rare. Weight-bearing can be gradually increased as the fracture site consolidates. Early weight-bearing should be encouraged (as far as possible), as it will help to hasten bone healing. In large animals, special care is needed during the period of anesthetic recovery and in the immediate post-fixation period. During the period, complications such as implant failure and refracture are more common, especially in horses. However, internal fixation of fractures is associated with considerable risk both in horses and cattle. Contralateral limb laminitis is more common in horses, but in cattle, it is less common as cattle prefer to lie down more often than horses. Bending of the contralateral limb is more often seen in young animals. In cases where the animal is unable to get up or struggle while getting up, decubital ulcers may develop. Hence, soft padding should be provided at the stalls/sheds.
Implant removal after bone healing is not always necessary. Generally, if the fracture heals without any complications, there is no need to remove the implants. If complications arise, such as implant failure or infection, the implants should be removed. It is generally easy to remove an intramedullary pin in small animals with a small skin incision under sedation and local analgesia, whereas bone plates and screws and interlocking nails are not often removed both in small and large animals, as they require extensive surgery for removal. However, if nails and plates are kept in situ for a prolonged period, they may get trapped within the bone or bony callus and may cause stress protection resulting in refracture in later dates. If and when an internal fixation device is removed, the affected limb should be temporarily immobilized using splints and bandages for a few days to avoid chances of refracture.
2.3 External Skeletal Fixation
External skeletal fixation (ESF) indicates immobilization of a debilitating musculoskeletal injury (normally bone fractures, but often joint dislocations, tendon/ligament injuries, etc.) utilizing multiple percutaneous fixation pins (transfixation pins/transcortical pins), which are connected to make a rigid external frame or scaffold, spanning the region of instability. Parkhill devised the concept of ESF in 1897 to stabilize open fractures and malunions of the extremities. In the first half of the last century, veterinarians such as Ehmer, Leighton, Schroeder, and Stader developed various designs of external skeletal fixators. ESF has been used in both human and veterinary orthopedic applications for more than 100 years, but it has only recently (during the last 20–30 years) enjoyed resurgence of popularity among veterinarians [91,92,93,94,95,96,97,98,99]. Renewed interest in the use of ESF has occurred for several reasons: an increasing occurrence of severe bone injuries related to vehicular and firearm accidents; advances in biomechanical studies of ESF and fracture healing that have reduced the incidence of fixator related complications; and the versatility of fixators for use in treatment of a variety of conditions such as fractures, delayed and non-unions, arthrodesis and limb deformities, etc. Even though ESF has been widely used in small animals to treat various fractures, arthrodesis, and limb-lengthening procedures, it has not got widespread acceptance in large animal practice due to lack of appropriate fixation implants that can endure heavy weight of the animals that can be applied in angularly placed bones and due to postoperative management problems. The cost of treatment is also a hindering factor for use of ESF in large animals. Although open fracture repair and stabilization using pins and wires or plates and screws have remained viable treatment modalities, more attention has been given recently to minimal surgical invasion and external fracture stabilization, and ESF is being used more frequently in both pets and livestock. It has allowed repair of some fractures that are unmanageable by use of conventional techniques.
2.3.1 Indications
ESF has been recommended for the treatment of long bone fractures below the stifle or elbow joints, where cast immobilization is not suitable or provides satisfactory level of fixation (above the mid-diaphysis of the radius/ulna or tibia). Fractures with open wounds and soft tissue injuries can also be better managed using an ESF, as they cannot be suitably treated using casts, splints, or their combinations [100]. It is useful especially in open, comminuted, and infected long bone fractures, where internal fixation in not advised and also suitable for transarticular application [101] for arthrodesis or temporary immobilization during healing of the soft tissues (ligament/tendon injuries) [102] or bone fractures of the extremities (metaphyseal/epiphyseal fractures).
2.3.2 Advantages of ESF
External skeletal fixation offers several advantages, such as quick functional recovery of the injured limb with excellent mechanical properties, allowing correction of rotational or angular deformities by adjusting the external frames even after fixation of the bone; avoidance of surgical trauma to the injured or normal tissues and hence protecting the circulation at the fracture site; and avoidance of infection associated with the buried implants. It also preserves the fracture haematoma and bone stimulatory proteins released during the fracture, allowing natural or biological healing to occur with a periosteal or endosteal callus [92, 94, 103,104,105].
Diversity in design and versatility of the ESF techniques allow their application to numerous types of fractures and are useful to treat short-segment fractures also. Fixation is useful in reserving the bone length and alignment, and removal of the implant after fracture union is easy. ESF is also useful for transarticular application in cases with severe soft tissue injury or comminution of the bone at the end of long bones. It preserves the joint range of motion and allows multiple applications with reusability of components. ESF also allows providing dynamization at the fracture site to hasten bone healing [106] (Fig. 2.48). Dynamization, however, is insubstantial in large animal applications, as providing rigid and stable fixation is most important and less rigid fixation leading to fixation failure is one of the major concerns. In the treatment of fractures, the use of closed reduction and stabilization via external skeletal fixation better preserves the periosteal circulation than bone plate fixation with open method.
2.3.3 Disadvantages of ESF
Though ESF offers several advantages, it has certain limitations. Penetration of fixation pins through the soft tissues may injure the vessels, nerves, and tendons, impairing the neuromuscular functions. The open skin-pin interfaces may allow the entry of bacterial infection. Eccentric placement of the ESF connecting elements (far from the central axis of the bony column) may often put ESF devices at a mechanical disadvantage when compared to intramedullary nails and bone plates. Postoperative care and management are difficult due to the presence of fixator components exposed externally.
2.3.4 Fixator Configurations and Types
According to the shape/configuration of the external frame connecting the transfixation pins, ESF is classified as either linear fixator, circular fixator, or hybrid fixator [96, 103, 107,108,109]. Based on the number of skin surfaces penetrated by the pins, ESF can be unilateral (pins enter the skin from one surface and penetrate only till it exits the opposite cortex) or bilateral (pins enter from one surface and exit from the opposite surface). As per the number of planes involved in the fixator, an ESF can be uniplanar, biplanar, or multiplanar.
In small animal practice, unilateral or bilateral linear fixation systems are often used, and in large animals, mostly bilateral systems are used. Unilateral fixator is mostly used in an upper extremity (humerus or femur, usually along with IM nails) or mandible, etc., because the anatomical structure precludes placement of a connecting bar on the medial side, whereas bilateral fixators are commonly used in distal limb bones such as the radius, tibia, metatarsals, and metacarpals, where medial and lateral limb surfaces are easily accessible. Circular fixators are also used in both small and large animal fracture fixation. They can be used in any bone where bilateral multiplanar fixators can be applied but are particularly useful for trans-tarsal applications in the hindlimb (fractures of the tibia and proximal metatarsus, luxation of tarsal joints, etc.).
2.3.5 Biomechanics of ESF
External skeletal fixation involves fixation of fractured bone using pins transfixed through bone segments, which are then externally connected to form a rigid frame. Fracture stability is achieved by transfer of loads between the major bone segments through the fixator components spanning the fracture site. Therefore, mechanical stability of a fracture immobilized by ESF is determined by (1) the material characteristics of the bone and fracture configuration, (2) the material properties of the ESF components, and (3) the design of the ESF [95, 104, 110,111,112,113,114].
2.3.5.1 The Material Characteristic of the Bone and Fracture Configuration
The diaphysis of a long bone has more dense cortical (lamellar) bone than the metaphysis or epiphysis having less dense cancellous (spongy) bone. Further, the diaphysis is more cylindrical in shape than the metaphysis or epiphysis, which are more irregular. Therefore, implant holding power of the diaphyseal bone is more than the metaphyseal or epiphyseal bone.
Fracture configuration also influences the mechanical stability of a reconstructed bone (Fig. 2.49). When an ESF is applied for fracture stabilization, a varying proportion of load is shared by the fixator and the reconstructed bone. In a transverse fracture with compression between the bone segments, much of the ground reaction force is transmitted axially along the bone segments across the fracture line; hence, the loading of the fixator components and the pin-bone interfaces is the least (ideal load-sharing fixation). In an oblique or comminuted fracture having a large butterfly fragment that is anatomically reconstructed with full-cerclage wires or lag screws (stabilized with interfragmentary compression), the ESF takes most of the ground reaction load as compared to the reconstructed bone (a partial load-sharing fixation), whereas in a highly comminuted fracture that cannot be anatomically reconstructed, none of the ground reaction force is transmitted through the bone column; instead, all of the load is transmitted from the distal bone segment to the proximal bone segment through the pin-bone interfaces and fixator components (buttress or non-load-sharing fixation).
2.3.5.2 The Material Properties of the ESF Components
Traditionally, ESF components have been fabricated from stainless steel. The connecting bars/rings made of mild steel, aluminum, or carbon composites have also been used. Stainless steel is a sufficiently strong material than aluminum and mild steel. Mild steel is stronger than aluminum and economical. Stainless steel is also generally more rigid and stronger than carbon fiber, but it may undergo plastic deformation with progressive loss of strength at higher loads. Carbon fiber frames are stronger than aluminum frames but costlier than aluminum or stainless-steel frames. Further, carbon fiber frames can delaminate when clamps are tightened on it, which limits their use for multiple applications. As aluminum and carbon fiber are lightweight and less rigid, their frames should be thicker than that of stainless-steel frames to maintain comparable rigidity.
The methyl methacrylate used to construct a connecting bar in free-form fixation systems has certain advantages such as lightweight and more economical than standard steel connecting bars and clamps. But to achieve comparable mechanical strength, acrylic connecting bars should be about four times larger in diameter than stainless-steel connecting bars (20 mm diameter acrylic column is almost similar to 5 mm diameter stainless-steel rod). Once hardened during frame construction, acrylic connecting bars cannot be adjusted. Acrylic is also more brittle and hence can develop cracks. Further, during hardening (polymerization-exothermic reaction) of acrylic, heat is generated (>55 °C); hence, there is a possibility of thermal injury to the tissues. However, this can be minimized by wetting/rinsing the transfixation pins with cold saline during the period and also by keeping a safe gap of about 10 mm between the skin and the acrylic column. The use of epoxy putty for construction of external frame has also shown promising results in terms of mechanical strength of the fixator, which is as good as methyl methacrylate. With epoxy putty, construction of connecting bars is technically easy, and heat generation is also less (because polymerization reaction is slower in epoxy than acrylic).
2.3.5.3 The Design of the ESF
The strength and stiffness of an ESF construct are also determined to a large extent by the implant design of different ESF components.
Frame configuration: The unilateral uniplanar fixation systems are mechanically the weakest (Fig. 2.50). In unilateral fixation systems, the axial extraction force for transcortical pins is greater when the pins engage to both cortices than that engages to only one cortex. Divergent pins increase the torsional stability and yield higher resistance at the fracture site as compared to parallel pins.
Bilateral linear fixator designs provide superior biomechanical stability than that of unilateral designs, irrespective of the pin size and number. Multiplanar fixators having four connecting bars (quadrilateral) placed equidistantly from one another are mechanically superior to bilateral fixators. The number of connecting bars (more number, greater stability) and the size of the connecting bars (increased size, greater stability) used also affect the fixation stability.
Regardless of the fixator design, the clamps joining the fixation pins to the connecting bars are the weak link in the fixator assembly. If not applied properly, it may cause movement and instability at the pin-bone interfaces leading to loosening of the pin and fracture instability. Hence, in large animal applications, fixation bolts are preferred over clamps, to provide more stable fixation between the pin and connecting bar.
Circular external fixation (CEF) allows axial micromotion at the fracture site without affecting the fixation stability [113]. With CEF systems, the distribution of bending and torsional loads is more uniform across the fractured bone with transfer of greater axial load along the fracture. The CEFs are less rigid but are more resilient (load-bearing capacity) than linear fixation systems.
In CEF, relatively small diameter pins are used under tension. Tensioning of pins increases the axial stiffness. It has been seen that a properly tensioned 1.6 mm pin can be as stiff as a 4 mm non-tensioned pin. However, pin should not be tensioned more than 50% of its yield strength (i.e. 105 kg for 1.5 mm pin and 150 kg for 1.8 mm pin) to avoid deformation and breakage of pin. Further, the effect of tensioning is more in small diameter pins, and as the pin diameter increases (large animal applications), tensioning effect reduces.
The angle between the opposing (cross) pins in a ring also impacts the fixation stability; to maximize stability, this angle must be close to 90°. Eccentric position of the bone within the ring reduces the axial and torsional stiffness. The use of beaded pins (olive wires) minimizes the translation of bone segments along the axis of the pin and thus significantly enhances bending stiffness and fixation stability.
Number of pins in each bone segment: The more the number of fixation pins in each bone segment, the larger the surface area for stress distribution and, hence, the greater the fixation stiffness (Fig. 2.51). The use of two or more pins (in linear systems)/rings (in circular systems) in each bone segment significantly increases fixation stability as compared to single pin/ring fixation. However, adding more than four pins per bone segment does not increase fixation stiffness but may increase the potential for pin-tract infection.
Pin design: Smooth (non-threaded) pins have least axial extraction strength and have the tendency for premature loosening and fixation failure and hence should be avoided in linear ESF systems. Among the threaded pins, the axial extraction force is greater in positive-profile pins than negative-profile pins. Among the different pin tip styles, trocar points are better penetrable than chisel or diamond points, but they cause higher temperature along the pin tract. Experimental results have shown that the use of wire ropes (braided steel wires) instead of monofilament pins of the same diameter can provide greater stiffness with respect to transverse loads, indicating that a wire rope may be a viable alternative to a monofilament pin as the transosseous component, especially in large animal circular fixation systems; however, it has not resulted in clinical applications, may be due to technical difficulties.
Pin diameter: Pin diameter also influences the fixation rigidity both in linear and circular fixation systems, as it has a direct effect on stability at pin-bone junctions. The larger pins bend less and hence produce less movement between the pin and bone. Pin stiffness is directly proportional to its radius (fourth power); hence, larger pins provide more rigid fixation (Fig. 2.52). But pin diameter should not exceed 20–25% of the bone diameter to avoid the risks of iatrogenic fracture through the pin tract and catastrophic failure of fixation.
Pin length: The strength and stiffness of fixation are inversely proportional to pin length, which also implies to the position of the connecting bar/ring on the fixation pins. Irrespective of fixator configuration, by minimizing the distance from the bone to the connecting bar, the fixation rigidity can be increased (Fig. 2.53); doubling this distance has been shown to reduce the resistance against compressive load by about 25%. If the distance between the bone and connecting bar/ring is less, the working length of the pin will be shorter. Hence, the pin will be less flexible causing less movement at the pin-bone interfaces. Clinically, it has been recommended placing the clamps about 1–2 cm from the skin surface.
Pin placement: Proper placement of the pins relative to the bone is critical to augment the strength and stiffness of the fixator construct. The pin must be placed at the center of the medullary cavity of the bone, so as to penetrate both bone cortices, to maximize stability and prevent iatrogenic fracture. Increasing the distance between the pins increases the working length of the connecting bar bridging the fracture zone and thereby increases its deflection (and fracture gap deformation) with weight-bearing. It is also advised to distribute the pins throughout the length of the bone segments (by using more pins) to disperse the load evenly. Pins close to the fracture are placed about 1–2 cm from the fracture line.
In bilateral linear and circular ESF systems, pins are always placed parallel to each other and perpendicular to the long axis of the bone; angling of pins does not offer any significant mechanical advantage. However, in unilateral systems, divergent pins are used to increase the yield strength; pins close to the fracture are angled to shorten the working length of the connecting bar.
2.3.6 Linear External Skeletal Fixation Systems for Small Animals
External skeletal fixation (ESF) is an ever-evolving system. In the 1940s, Emerson Anton Ehmer working with the Kirschner Manufacturing Co., Washington, developed the Kirschner-Ehmer splint, popularly called as KE device. The KE device became synonymous with the external skeletal fixator for several generations of veterinarians and has been widely used in small animal applications [105]. However, due to several disadvantages of KE device, such as mechanical weakness, poor understanding of the system, and high patient morbidity, the popularity of ESF system is reduced by the early 1980s. Subsequently, better understanding of the ESF system led to improved design of fixation pins and KE clamp and a trend toward more rigid fracture fixation. Further improvements in ESF devices were directed to simplify some of the complex frame geometries with the KE device, which led to improved ESF systems such as IMEX™, SecurOS™, Innovative Animal Products™, and Synthes ESF system. These ESF devices have significant improvements in ESF design that improved technical ease of application; increased fixation rigidity, with simplified frame configurations; and decreased patient morbidity.
The standard ESF systems developed for small animal applications have often tried for large animal fixations. However, the mechanical limitations of most of these ESF devices markedly limit their application in large animals. The major limitation is the inability of conventional ESF systems to sustain the heavy weight-bearing loads, leading to fixation failure, especially at the clamps used to connect the fixation pins to the connecting rods. Implant failure in large animals is mostly attributed to loosening of pin-bone interfaces. Heavy weight-bearing loads placed on transfixation pins may cause deflection of pins and thus significant strain at the pin-bone interfaces leading to bone resorption. Resorption of the bone along the pin-bone tracts can further increase pin movement, thus setting in vicious cycle of pin motion and bone resorption, resulting in reduced fixator stiffness and fixation failure. Although various ESF devices developed for humans and small animals have been used in experimental and clinical studies in large animals, the results with type II configurations were satisfactory in lightweight calves and foals weighing less than 150 kg, and type I (half-pin) designs were successful only to a limited extent.
A typical ESF device is made up of (1) fixation pins, (2) linkage devices (fixation clamps, pin grippers), and (3) connectors (connecting rods/connecting bars/sidebars). Connectors and linkage devices together form ESF frame.
2.3.6.1 Frame Configurations
ESF systems for small animal applications are available in different frame configurations: unilateral or bilateral (based on the side) and uniplanar, biplanar, or multiplanar (based on the plane) [90, 109] (Fig. 2.54). Taking both the side and plane into consideration, ESF frames can be further classified as detailed below:
-
Unilateral-uniplanar (type Ia): Fixator frame projects from only one side (mostly lateral) of the limb and occupy just one plane. The frames are constructed entirely of half-pins.
-
Unilateral-biplanar (type Ib): It is a combination of two distinct type Ia frames. Type Ib frames also protrude from only one distinct side of the limb, but the frame occupies two planes. Many modifications of the type Ib frame have been described.
-
Bilateral-uniplanar (type II): The frame projects from two sides of the limb (usually medial and lateral) but occupy only one plane. These frames are made of either entirely full-pins or a combination of full- and half-pins. Accordingly, type II frames are sub-classified as either ‘maximal’ or ‘minimal’. A maximal type II frame has full-pins in all locations, whereas a minimal type II frame has at least one full-pin each in the proximal and distal bone segments and half-pins in the remaining locations.
-
Bilateral-biplanar (type III): It is a combination of type I and type II frames. It can be constructed in many different ways.
2.3.6.2 Fixation Pins
Fixation pins are of different types. Based on their placement, pins can be called as either half-pins or full-pins. A half-pin penetrates one surface of the skin and both bone cortices. A full-pin (through and through) enters through a skin surface (near), penetrates both bone cortices, and exits through the opposite (far) skin surface.
According to their design, pins can be classified as non-threaded (smooth) or threaded. Historically, smooth pins were used in ESF systems. The placement of pins at divergent angles is recommended to increase the fixation stability, but it does not prevent pin loosening and associated morbidity. Threaded pins allow an interlock between the pin and the bone such that this pin-bone interface is much more stable when compared to use of non-threaded pins. Hence, currently most often, threaded pins are used in ESF designs.
Threaded pins can be sub-classified according to the thread profile (negative vs. positive), location of the thread (centrally threaded vs. end-threaded), or recommended use (cancellous vs. cortical).
Threaded pins manufactured by cutting threads into the core of the pin are called negative-profile pins. In partially threaded negative-profile pin, the junction of the threaded and non-threaded portion is the weak point due to the concentration of bending stress leading to cracks. In early ESF devices (such as IMEX and KE), these negative-profile pins were mostly used to provide some pin-bone interface stability when compared with smooth non-threaded pins. Modern ESF devices are designed in such a way that the positive-profile pins can be used at any position within a fixator due to improved clamp configurations such as the Secur-U™ clamp (SecurOS) and the IMEX-SK™ clamp (IMEX). Due to the improvements in these fixation systems and the advantages of positive-profile pins, the use of negative-profile pins is declining. In positive-profile pins, the threads are built above the pin core; hence, they have good holding power when implanted in the bone and are quite resistant to fatigue failure [115]. These pins are available from IMEX™, SecurOS™, and Innovative Animal Products™ in end-threaded and centrally threaded designs.
Fixation pins can also be classified based on their thread form as cortical or cancellous. Cortical pins have large number of fine threads per unit length, which is ideal for hard lamellar bone as it has greater surface area of contact through thread-bone interfaces. Cancellous pins have more coarse thread pattern with fewer threads per unit length, designed particularly for use in sites where the bone is very soft such as the metaphyses or epiphyses of long bones.
2.3.6.3 Linkage Devices (Fixation Clamps/Pin Grippers)
Connecting rods and linkage devices (clamps) are the essential frame components of an ESF. Linkage devices are specific to the manufacturers. Some of the commonly available systems are described below, but there are many other systems marketed around the world that may differ in a variety of ways but not necessarily inferior.
KE clamp: Three different sizes (small, medium, and large) of KE clamps are available. The KE single clamp has a bolt portion holding a U-shaped body. The clamp is primarily used to join the fixation pin to the connecting bar. Pin is attached through a small gripping channel present in the bolt, while a large gripping channel at one end of the U-shaped body is used to fix the connecting rod (Fig. 2.55). The clamp can also be used to make articulations in biplanar configurations and in tie-in configurations wherein an intramedullary pin is connected to an external fixation frame. The KE double clamp has two large rod-gripping channels, which is designed for attaching one connecting rod to another and is also useful for connecting an IM pin to a fixation frame. The limitation of KE clamps is that when adequately tightened to achieve firm fixation between the connecting bar and the clamp, the U-shaped body of the clamp may get deformed, which has to be restored to its original shape prior the reuse. This can be done by springing open the U-shaped body with a pin cutter applied to the open end of the ‘U’. Due to mechanical inferiority of the clamps and the technical limitations of their use, KE device is currently not commonly used as compared to more modern/advanced ESF devices.
Different types of fixator clamps: (A) KE clamp with U-shaped clamp body (a), rod-gripping channel (b) and pin-gripping channel (c); (B) Secur-U ™ clamp showing U-shaped clamp body (a), opening for connecting bar (b) and opening for fixation pin (c); and (C and D) IMEX-SK™ clamps with bolt for fixation pin (a), bolt for connecting bar (b), opening for connecting bars (c), opening for fixation pin (d), halves of clamp body (e) and slotted washer (f)
Secur-U ™ clamp: The Secur-U clamps are available in small and medium sizes. The clamp has three parts: a U-shaped body, a round head, and bolt that attaches the head to the body and tightens the clamp. The U-shaped body has an opening for the connecting bar, and the head portion has two holes each accommodating different diameter pins. The SecurOS™ fixator overcomes the problems with the KE splint, as positive-profile pins can be placed in any clamp position by using an aiming device. Tightening of the clamp may cause only slight deformation of the head portion against the connecting rod; hence, when used for the second time, the head should be rotated 180° so that there will be a different contact area. The clamp can be ideally tightened to 7.34 Nm of torque by using the precision torque wrench. Another clamp, the Augmentation Clamps™ made by SecurOS, is used to attach an augmentation plate to build a stiffer, more compact frame.
IMEX-SK™ clamp: The IMEX-SK™ fixator also overcomes many of the limitations of KE splint. SK clamps are also available in three different sizes (mini, small, and large). The clamps have three different components: a two-piece body, a long pin-gripping bolt, and another short secondary bolt. The two-piece body made of black anodized aluminum has the rod-gripping channel at the center, and the pin-gripping bolt with a slotted washer and nut goes through the bottom portion of the body and the secondary bolt through the top portion. Clamps can be fixed at the desired position along the connecting rod. The washer in the pin-gripping bolt permits effective gripping of different diameter pins. The presence of large hole in the pin-gripping bolt allows predrilling and fixation of positive-profile pins directly through the clamp. The secondary bolt which is unique to the SK clamp design helps to properly secure the connecting rod with additional grip and also allows the use of clamp as a drill guide as well as a targeting device. The secondary bolt is loosely tightened to hold the clamp in the desired location on the connecting rod and to maintain the position of the clamp while predrilling and placing a fixation pin. The connecting rods in SK splint are made from carbon fiber composite, titanium, or aluminum (instead of stainless steel), which permit the use of increased rod diameter and strength without excess weight.
2.3.6.4 General Principles of ESF Application
Many of the principles of ESF application are the same regardless of the specific device used [98, 103, 116, 117]. The use of the more modern ESF devices available today can improve the clinical outcomes because of enhanced technical simplicity of application and mechanical superiority of the devices themselves.
Anesthesia and restraint: The patient is anesthetized, the hair is clipped, and skin is prepared with scrubbing as for any orthopedic procedure. The surgical field must include a joint above and below the fracture, and it is properly draped. The animal is restrained in dorsal recumbency and the limb is suspended in a hanging limb position throughout the surgical procedure, especially for fixation of radius-ulna or tibia-fibula fractures, whereas in humerus or femur fractures (where typically unilateral fixators are used), the animal may be positioned in lateral recumbency with the affected limb facing upwards.
ESF frame construction: The planned frame configuration including pin selection should be sketched prior to surgery and placed near the radiographic viewer, which will act as a guide during fracture fixation. With the KE device, it is important to anticipate the desired number of fixation pins so that an appropriate number of clamps can be positioned on the connecting bar in the beginning since it is very difficult to add or remove clamps later during the repair, whereas SecurOS™ or IMEX-SK™ clamps can be added to the connecting rods at any point during the procedure. The distal-most and proximal-most pins are usually placed first (Fig. 2.56). These pins are then fixed to a connecting rod through the clamps to construct the frame. Fracture reduction and alignment are fine-tuned at this time prior to placing pins in the middle-clamp positions. Subsequently, predrilling and pin placement are done through the clamps (KE and IMEX-SK™ devices) or with the aid of an aiming device (SecurAim ™) to ensure placement of the pin in an appropriate position relative to the connecting bar. Pins should be positioned about 1–2 cm off the fracture line. In multiplanar frames (type Ib and type III), two uniplanar frames are interconnected. As metallic multiplanar frames tend to obstruct the radiographic visualization of the fracture, the two frames can be articulated after postoperative radiographs are made.
Pin selection: The selection of appropriate size pin depends on the bone diameter. Larger diameter pins are much stiffer; however, the penetration of the bone by excessively large pins will weaken the bone. By and large, the pin diameter should not be more than 20–25% of the bone diameter. Threaded pins are preferable to non-threaded pins because of their superior holding power in the bone. Positive-profile threaded pins offer the additional advantage of resistance to breakage. Negative-profile threaded pins may be preferred where the bone diameter is small to minimize risk of iatrogenic fracture through the pin tract. With modern ESF devices which allow the use of different pin sizes, smaller-size positive-profile threaded pins may be preferred instead of negative-profile pins. Cancellous fixation pins may be used in the metaphyseal regions of different long bones; however, placement of cancellous pins in other locations risks iatrogenic fracture through the pin tract.
Pin placement and insertion: Fixation pins are placed through ‘safe’ corridors to reduce the risks of musculotendinous or neurovascular injury. As a general rule, medio-lateral or latero-medial pin placement is safe than cranio-caudal placement. About 1–2 cm-long release incision is made (proximal to distal) in the skin at the proposed site of pin placement. A haemostat is used to bluntly dissect down and make a small ‘grid’ along the soft tissues down to the underlying bone. It is advised to make a slightly larger soft tissue corridor than the pin size because any tension of soft tissues on the fixation pin may cause irritation and inflammation. Soft tissues are retracted away from the pin during pin placement by use of a haemostat spread at the tips or use of a drill sleeve. It is always preferred to predrill the pin tract with a drill bit measuring about 10–15% smaller in diameter than the pin, before the pin placement. Ensure that the pin tract is made at the center of the bony cortex. Half-pin is then advanced through the soft tissue corridor and inserted along the predrilled hole in the bony cortex (using a power drill) so as to penetrate the far cortex. The entire trocar point should exit with 1–2 threads coming out of the far cortex to maximize stability. In case of a full-pin, it is advanced through the soft tissue corridor and both cortical surfaces to exit the far skin surface. At the exit point, a small skin incision is made, and using a haemostat, the soft tissues are retracted to create a corridor around the pin.
For drilling, a slow-speed power drill is used; a hand chuck or high-speed drill (>400 rpm) is not recommended. Hand chuck insertion creates an excessively large pin tract due to chuck wobbling, whereas high-speed drill insertion generates excessive frictional heat causing necrosis of the bone around the pin tract. Both methods risk premature pin loosening and associated pain, poor-limb use, and loss of fracture reduction.
It is also important to drill in small pulses (with 30 s between the pulses) to allow for dissipation of heat generated. If stuck, the pin should be retracted and reinserted after a while. While drilling, cold isotonic solution is dropped continuously at the pin site to minimize thermal injury to the tissues. To achieve stable fixation, at least two pins are fixed in each bone segment. The distance between the skin and connecting rod should be minimum; however, at least 1–2 cm gap should be kept between the skin and the connecting rod to allow soft tissue swelling and regular dressing of pin-skin interfaces. Except in unilateral linear fixation systems, pins are always placed parallel to each other and perpendicular to the bone axis.
ESF is often used along with intramedullary pin, as in ‘tie-in’ configuration (Fig. 2.57). In this case, the fracture is first reduced by inserting a relatively small diameter Steinmann pin into the medullary cavity. Unilateral ESF is then fixed on the lateral surface of the limb by inserting two end-threaded bicortical half-pins, one at each end. After ascertaining adequate bone reduction, additional half-pins may be reinforced as per the need. The protruding end of the IM pin is then anchored (tied-in) with proximal end of the ESF using a clamp.
Post-fixation radiographs are made to assess proper placement of fixation pins in the bone. After reviewing the radiographs, if needed, it is preferable to advance a pin that was not placed deeply enough into the bone, rather than retracting a deeply seated pin (retraction of the pin disrupts the pin-bone interface and hence increases the risk of premature pin loosening). Final adjustments are then made and all the clamps are tightened.
2.3.6.5 Postoperative Care and Management
Immediately after the surgical fixation, the external fixator components and the surgical area should be cleansed of debris and blood clots and allowed to dry. Cut ends of fixation pins are flushed, and protective caps may be applied to prevent injury to the animal as well as the handler while dressing. The skin-pin interfaces are cleaned with an antiseptic solution (0.05% chlorhexidine or 1% povidone iodine), an antibiotic ointment is applied, and then a sterile non-adherent dressing is done around the surgical area to cover the open wound or skin incision and the skin-pin interfaces. It is also advised to apply a compressive bandage on the operated limb, similar to a Robert-Jones bandage, which would help absorb exudates from the pin-skin interfaces and decrease postoperative swelling [107]. A course of broad-spectrum antibiotic is given for a period of 3–5 days, especially in open fractures to prevent bacterial infection. If bandaging is done, it should be replaced after 1–2 days. Daily cleaning and dressing of the surgical site may continue till the release incisions/wounds are healed.
The animal’s activity should be restricted in the postoperative period to prevent any complications and allow for bone healing. The patient may be confined to a cage/limited area to prevent running, jumping, or playing and allowed only leash walking. This movement restriction should continue until the radiographic confirmation of bone union. It is important to inform the animal owner about the importance of movement restriction and daily cleaning and dressing of pin-skin interfaces for successful outcome of fixation and bone healing.
The patient should be subjected to follow-up examinations at regular intervals. Although the interval of examinations may differ from case to case, it is advisable to inspect more frequently in the initial stages, especially the fixator components, and if needed, corrections (tightening the loose components) may be done. Subsequently, clinical and radiographic examinations may be carried out at 15-day intervals till radiographic bone healing. If delayed healing is suspected, staged destabilization of the fixator construct can be done (starting from sixth week) by removing certain part/s of the frame. This ‘dynamization’ reduces fixator stiffness and increases micro-movement at the fracture site leading to accelerated bone healing. The fixator is removed after the radiographic evidence of bone healing (bridging callus). For removal of fixator, the animal may be sedated and fixation pins are cut using a pin cutter, and the cut pins are pulled using a plier or hand chuck. The pin tracts are flushed with sterile saline or antiseptic solution, and the limb is temporarily bandaged for 2–3 days. The pin tracts are not sutured but allowed second intention healing to occur.
2.3.7 Transfixation Pinning and Casting in Large Animals
Transfixation pinning and casting (TCP) is the most commonly used external skeletal fixation technique in large animal practice. It can be applied as a ‘hanging limb pin cast’ or as an ‘external skeletal fixator’.
2.3.7.1 Hanging Limb Pin Cast
In hanging limb pin cast, one or two transfixation pins are placed medio-laterally in the proximal bone segment of a fracture, and a full-limb cast is applied by anchoring the cast with the pin/s (Fig. 2.58). In this scenario, the load (body weight) is taken by the pin/s and transferred to the cast, sparing the fracture site. The distal part of the limb is ‘free’ and it ‘hangs’ inside the cast [13, 118].
2.3.7.1.1 Principle of Hanging Limb Pin Cast
During cast application, fracture site stability is achieved by immobilizing the joints above and below the fracture. However, inclusion of both joints in the cast is not always possible because of anatomical disposition of some bones. Fractures of the proximal tibia (and often the radius) in heavy large animals cannot be adequately stabilized using a plaster cast because the stifle or elbow joint cannot be appropriately secured in the cast. In hanging limb pin cast, the pin(s) used in the proximal bone segment helps secure the cast and prevent its downward slipping.
2.3.7.1.2 Technique
Under general anesthesia or deep sedation with regional nerve block, the animal is restrained in lateral recumbency with the injured limb positioned upwards. The area proximal to the fracture site is shaved and prepared aseptically. The proposed site of pin insertion (usually one) is marked on the skin on the outer surface (usually lateral). A small release incision is given in the skin (proximal to distal orientation) at the proposed site of pin insertion in the proximal bone segment. A hole is predrilled through the center of the bone cortex (perpendicular to the bone axis) along the proposed line of pin insertion, using an electric drill and a drill bit (about 0.5 mm smaller than the pin diameter). A proper size pin (about 6–7 mm Steinmann pin) is then inserted through the predrilled tract, so as to exit it through the far cortex and the skin on the opposite surface (standard pin insertion technique as described before is followed while passing the transfixation pin). The extra length of the pin is cut and the pin-skin interfaces (on both skin surfaces) are dressed with sterile gauze and antiseptic solution. The fracture segments are aligned by closed reduction using traction and counter-traction and held in extension using a rope tied at pastern region. The whole limb is padded using cotton, and a full-limb cast (plaster of Paris or fiberglass) is then applied in such a way that the cut ends of the pin are buried within the cast.
2.3.7.1.3 Postoperative Care and Management
Postoperatively, broad-spectrum antibiotic and analgesic-anti-inflammatory drug are administered for 3–5 days. The animal is closely observed for any soft tissue infection or necrosis around the pin exit points.
2.3.7.1.4 Limitations/Disadvantages
With handing limb pin cast, it is not possible to prevent overriding of bone segments in case of an oblique or spiral fracture, and it does not provide adequate fixation of a comminuted fracture. Placement of pin only in proximal bone segment does not prevent rotation of the distal bone/limb and hence cannot provide as stable fixation as transfixation pinning of both bone segments.
2.3.7.2 Transfixation Pinning and Casting (TCP) as an ESF
This technique includes placement of at least two fixation pins in both major bone segments (proximal and distal) and application of a full-limb cast to stabilize the fracture site [2, 13, 119, 120] (Fig. 2.59). The advantages of pin-cast ESF as compared to hanging limb pin cast is relatively more rigid fixation of fracture with limited movement of fracture segments within the pin-cast. Further, with pin-cast ESF, the cast need not span the adjacent joint (such as stifle); however, full-limb cast is always preferred, especially in heavy large animals.
2.3.7.2.1 Technique
Under general anesthesia (or deep sedation with regional nerve block), the animal is positioned in lateral recumbency. The affected leg is drawn out of the operation table and held in extended position. The whole length of the injured bone is aseptically prepared by shaving and scrubbing. The bone segments are aligned by close reduction using traction and counter-traction and held in extension using a rope tied around the pastern. The proposed sites of pin insertion are marked on the skin along the bone (upper surface). Small release incisions are made in the skin at the proposed sites of pin insertion. Subsequently, optimum size pins (smooth or threaded pins, a least two each in the proximal and distal segment) are drilled through predrilled holes in the bone cortex, so as to exit from the opposite bone cortices and the skin (through release incisions made in the skin at the pin exit points). The size of the pins is selected based on the animal’s body weight; usually, 6–7 mm pins are adequate in adult large animals.
The transfixation pins are inserted using a low-speed electric drill, following proper pin insertion principles. All the pins are passed parallel to each other and perpendicular to the bone’s axis. The pins emerging from the skin surfaces on medial and lateral surfaces are then connected using connecting bars (metal/plastic/wooden) to give greater strength to fixation. The extra length of the pins is cut, and the pin sites are protected using sterile gauze with antiseptic solution. Subsequently, a full-limb cast is applied routinely so that the cut ends of the pins are buried within the cast. Plaster of Paris or fiberglass cast can be used, but fiberglass cast has distinct advantage of lightweight and greater strength.
In open fractures, a ‘window’ is kept at the level of skin wound to allow for drainage and daily dressing. Keeping a window, however, does not give satisfactory results always, and the patient may feel discomfort due to the development of swelling at the defect site. The cast is cut and transfixation assembly is removed once the clinical union of fracture is evident, usually after 10–12 weeks in adult large animals.
2.3.7.2.2 Advantages
The biomechanical advantage of TPC includes rigid bone fixation due to the least distance between the bone and the external frame. With TPC, fixation pins can be placed at desired locations (as per the fracture configuration), and it need not dictated by the typical ESF clamp or rod position. Further, the mechanical (weight-bearing) load is distributed by sharing with the cast.
2.3.7.2.3 Disadvantages
Complications such as soft tissue infection, bone necrosis, and periosteal reaction around the transfixation pins can often occur, which are difficult to assess and treat. It is not possible to adjust the fracture reduction and alignment after the cast application. There can be difficulty in managing wounds (with open fractures) and problems in assessing the development of cast sores.
2.3.8 Linear External Skeletal Fixation Systems for Large Animals
It is a great challenge to treat long bone fractures in large animals, especially open infected fractures. As most of the bone fractures are open in nature, the fixation device should not only provide rigid fixation and well tolerated by the animal but also allow drainage and daily dressing of the open wound. Further, any fixation technique developed for large animals should also be less cumbersome to apply by practicing veterinary surgeons at field level for its wide acceptance. ESF devices developed specifically for use in large animal applications [13, 121,122,123,124,125] are not commercially available.
A full-pin type II ESF device has been developed for equines by Nunamaker and Nash in 2008 [126,127,128]. The original design comprised of partially threaded self-tapping fixation pins with core diameter of 8.6 mm at threaded portion and 9.6 mm at non-threaded portion. The connecting bars are developed from composite polyurethane reinforced with stainless-steel rods. The device was designed specifically for distal limb fractures (metacarpals and metatarsals), wherein transfixation pins placed in the proximal bone segment are connected to the opposing connecting rods that are attached to a foot plate (which is rounded and angled 15–25° from the ground surface). The foot plate in turn is fixed to a customized bar shoe. Further modification of the design included an additional tapered sleeve over the smooth pins (7.94 mm), which can be compressed against the bone cortices by tightening the nuts along the inbuilt threads on the pin ends. This improved design has greater fixator stability especially at bone-pin interfaces. The fixator construct has been found to have adequate stiffness and strength to allow immediate full weight-bearing by adult animals. The modified design can support about ten times the animal’s weight, as compared to the original version, which can support three times the body weight.
A novel bilateral external fixation device has been developed at the Indian Veterinary Research Institute, Izatnagar (UP), India, which comprises of a pair of threaded solid cylindrical connecting rods (sidebars), having a hexagonal flat inbuilt nut at the center and threads carved in opposite directions on both sides from the center (to allow distraction or compression of bone segments after bone fixation by turning the connecting rod in opposite directions) (Fig. 2.60) [13, 121,122,123]. Multiple fixation bolts help to secure the fixation pins at desired levels as per the fracture location. This fixator is unique in that it is simple and less cumbersome to apply, and fracture reduction and compression can be achieved even after bone fixation.
Different parts of novel bilateral linear fixation device: (a) connecting rod with clamps and check nuts fixed on either side of the outermost clamps; (b) ESF assembly with 6 fixation pins connected to connecting bars through clamps; and (c) fixator applied transarticularly to repair proximal metacarpal fracture in a cattle
2.3.8.1 Fixator Components
Connecting rods (side bars): The stainless-steel connecting rods measure 14 mm in diameter with different lengths (22–45 cm). The center of the connecting rod has an inbuilt hexagonal nut (2 cm wide) to facilitate turning of connecting rod with a wrench. On either side, the threads are carved in opposite directions (pitch 2 mm), ‘positive (right hand thread)’ and ‘negative (left hand thread)’.
Fixation bolt: The fixation bolts are in the form of rectangular blocks, having an eccentrically placed threaded hole to get secured along the connecting rods and on the other side an 8 mm smooth hole drilled perpendicular to the length of connecting rod to accept a 6–7 mm pin. The threads carved in the fixation bolts are either in ‘positive (right hand)’ or ‘negative (left hand)’ direction to secure along the corresponding side of the connecting rod. Variable number of fixation bolts can be fixed along the connecting rod at desired levels (to secure the pins exiting the bone segments).
Check nuts: Two small check nuts (for fixation along the threaded pins) are tightened on either side of the fixation bolts along the threaded pin to prevent loosening of the pin-bolt assembly. Two large nuts (for fixation along the connecting rods) are tightened on either side of outermost fixation bolts along the connecting rod to tightly secure the fixation bolts to prevent their rotation and thus achieve rigid fixation.
Transfixation pins: Fully threaded pins can be of negative profile or positive profile (positive-profile pins are preferred). Thread designs may be cortical or cancellous as per the location. 6–7 mm diameter pins are commonly used in adult large animals.
2.3.8.2 Indications
It is indicated for the treatment of fractures in different straight long bones such as the radius-ulna, metacarpus, metatarsus, and phalanges in cattle, buffaloes, and horses. It is particularly useful to treat open infected fractures, where cast immobilization is not indicated and internal fixation (like bone plate or nail) is not desired and also suitable for transarticular application during arthrodesis or temporary immobilization of the joint to allow healing of soft tissues (ligament/tendon injuries) or fractures of bone extremities.
2.3.8.3 Advantages
Novel bilateral ESF provides rigid fixation of fractures in straight long bones of large animals. Fractured bone segments can be reduced or compressed even after fixation of pins, by turning the hexagonal nut at the center of the connecting rods in opposite directions. The device is simple and less cumbersome to attach and assemble during bone fixation. The fixator design allows its usage in different straight long bones of varied length and in transarticular applications. Transfixation pins of different diameter can be fixed at desired locations. Wound dressing and care of the fixator assembly is easy during the convalescent period. As the device has minimal parts, the cost of manufacturing is less.
2.3.8.4 Principles and Guidelines for Application
Survey radiography: Radiographs (orthogonal views) of the fractured bone are made to determine the fracture location and configuration and to plan for fixator application (to decide the size and number of fixation pins, location of pin insertion, etc.).
Anesthesia and restraint: Using general anesthesia, the animal is restrained either in dorsal recumbency with the limb suspended or in lateral recumbency with the fractured limb extended outside the operation table (which will facilitate through and through pin insertion) and the open wound facing the surgeon (to help reduce the bone segments and keep watch on bone alignment during fixator application). While general anesthesia is always preferred in small animals and horses, deep sedation with regional or spinal analgesia can be used in small and large ruminants, especially in hindlimb applications.
Preparation of the surgical site: The hair is clipped and skin is prepared with surgical scrubbing. The preparation of surgical field must include a joint above and below the fracture, and the area is properly draped. The fracture segments are reduced and held in alignment using traction and counter-traction. In case of a compound fracture, the open wound is cleaned and dressed using cotton bandage to prevent further contamination of the wound. In stable fractures, skin sutures may be applied (to cover the fracture site) leaving sufficient gap between the sutures for drainage. The proposed sites for placement of transfixation pins are chosen (using radiographic images) and marked considering the safe corridors (generally medio-lateral/latero-medial).
Selection of pins and preparation of fixator assembly: A proper diameter pin (not exceeding 20% of the bone diameter) is selected. In medium-sized animals weighing about 300–400 kg, 6 mm fully threaded positive-profile pins may be used; in heavy animals (>400 kg), 7 mm pins are indicated. It is important to anticipate and decide the desired number of fixation pins (based on the radiographic evaluation) before surgical fixation so that appropriate number of fixation bolts can be positioned along a pair of connecting rods. Two check nuts are placed on either side of the outermost fixation bolts along the connecting rods on both ends. The length of the connecting rods is decided as per the fracture location and configuration and the number of pins needed; in mid-diaphyseal fractures, normally four pins (two in both bone segments) are fixed, but in transarticular fixations (proximal or distal metacarpal or distal radial fractures), 5–6 pins may be needed; hence, relatively long connecting rods have to be selected so as to span the carpal/fetlock joint.
Pin insertion technique: Standard pin insertion technique (as described before) is followed while inserting the transfixation pins. All the pins are inserted one by one in a single plane (medio-lateral) and parallel to each other and perpendicular to the long axis of the bone (Fig. 2.61a). It is also ensured that all the pins are inserted up to the same level to facilitate fixing of the connecting rods.
Fixation of pins with the connecting rods: Once all the pins are passed, two small nuts are inserted through both ends of the threaded pins and are brought close to the skin (Fig. 2.61b). It is ensured that the clamps in the connecting rods are spaced as per the location of transfixation pins. The pins are then fixed to the connecting rod by inserting them into the fixation bolts (through the pin holes). It is advised to insert all the pins to the corresponding clamps at a time. Similarly, the pins that exit from the opposite skin surface are also connected to another connecting rod (Fig. 2.61c, d).
Once both connecting rods are fixed, they are brought close to the skin by gentle maneuvering (if needed central hexagonal nut may be slightly hammered down) and are fixed at the desired level, so that both connecting rods lay parallel to each other (Fig. 2.61e). The distance between the bone and the connecting rods should be kept minimum; however, at least 15–20 mm gap between the skin and connecting bars is needed to allow soft tissue swelling and regular dressing of pin-skin interfaces. Subsequently, two more nuts are inserted through both ends of the threaded pins (Fig. 2.61f). The pins are cleaned from any tissue debris before inserting the nuts for smooth passage. The nuts on either side of the fixation bolts, along the threaded pins, are tightened against the bolts to achieve stable pin-bolt junctions (Fig. 2.61g). The check nuts on either side of outermost fixation bolts along the connecting rod are then tightened to rigidly secure the fixator assembly (Fig. 2.61i). The extra length of pins is cut, and the cut ends may be sealed using epoxy putty to prevent possible injury to the contralateral limb and to the handler during routine wound dressing (Fig. 2.61k, l). The surgical/open wound is approximated by placing interrupted skin sutures when possible (if not done before).
2.3.8.5 Postoperative Care and Management
Management of animals in the immediate postoperative period (48–72 h) is more critical as they may feel discomfort by the presence of the external frames. The animal may take some time to get accustomed to the fixator; hence, regular observation of the animal is required during the period. Broad-spectrum antibiotic and anti-inflammatory/analgesic drugs are given for 3–5 days. As an ESF is generally applied in an open infected fracture, prolonged antibiotic therapy may be needed. In such cases, it is always advised to change the antibiotic, as per the sensitivity test results.
Regular antiseptic dressing of the pin-skin interfaces and the skin wound (in case of open fractures) is done till the healing occurs. Pin site discharge is common with ESF; hence, prolonged dressing of the pin site is needed using an antiseptic solution like chlorhexidine or povidone iodine and an antibiotic solution. The ESF frame may be covered with a sleeve or bandage to prevent licking of the pin-skin interfaces. The movement of the animal should be avoided during the post-fixation period; however, walking should not be restricted for prolonged period, as it is an excellent form of physical therapy, which can help in early bone union.
2.3.8.6 Removal of Fixator
After the radiological union of the fracture (generally 8–12 weeks), the pins are cut using a pin cutter and the ESF frame is removed. The cut pins are pulled out of the limb with pliers. After removal of pins, the pin tract is cleaned with an antiseptic solution. The limb may be temporarily splinted and the activity of the animal restricted for another week or so.
2.3.9 Circular External Skeletal Fixation
Circular external fixation (CEF) system was first described by a Russian scientist, Ilizarov, in the early 1960s. In CEF systems, relatively small diameter wires/pins are fixed under tension across a ring anchoring at both ends; such pins placed under tension provide good axial strength. Due to the mechanical advantage, Ilizarov model of CEF systems has been extensively used for treatment of a variety of musculoskeletal disorders like fractures, dislocations, arthrodesis, correction of angular deformities, and limb-lengthening procedures in human as well as small animal practice. Even though CEF systems were first introduced in the early 1990s for small animal applications, it has only recently attracted the attention of large animal orthopedic surgeons mostly for fracture fixation in large animals. The most commonly used CEF system in small animal applications is marketed by IMEX Veterinary Inc. However, there are many other systems available across the world. Nevertheless, CEF systems developed specifically for use in large animals are not commercially available.
2.3.9.1 Fixator Components
Apart from fixation pins, the circular fixation system comprises of three basic components: rings, connecting rods, and fixation bolts [13, 91, 95, 103, 129] (Fig. 2.62).
Circular rings (half-rings): A typical CEF system consists of four full rings or eight half-rings (two rings blocks in each major bone segment). The number of rings required in a particular case may depend on the bone involved and the location of fracture. Transarticular fixations generally require more number of rings, and often to maintain the normal joint angle and movement, ¾ rings or ½ rings are used.
Circular rings made from different materials such as stainless steel, carbon fiber, and aluminum are available for use in small animals. The rings ranging in diameter from 50 to 150 mm are available; the ring size depends on the site of application and the size of animal, but it should be large enough to maintain a gap of about 2–3 cm between the skin and ring around the limb. The thickness of the rings varies with the material used; carbon fiber and aluminum rings are thicker than stainless-steel rings.
For large animal applications, CEF rings made of stainless steel, aluminum, and mild steel have been developed. The steel rings measuring 5 mm thickness and 20 mm width having 18–28 equidistant holes (10 mm diameter) to accommodate connecting rods and fixation bolts (8 mm) are mechanically adequate in most adult large animals. Although ring diameter may vary as per the location of fracture (tibial fractures require relatively large diameter rings, while metacarpal/metatarsal fractures need only small diameter rings) and the animals’ weight, about 150–220 mm inner diameter rings are generally required for large animals. The fixation systems developed using mild steel or aluminum are sufficiently rigid and are more economical for fixation in large animals.
Fixation pins: They can be smooth or beaded (olive wire). Beaded/olive wires are specialized wires with a larger diameter bead/ball at their midpoint, preventing movement of the bone (translation) in relation to the pin. They strengthen the fixation and allow translation of bone segments when traction is applied from the opposite end. 1.0–1.8 mm (1.0, 1.2, 1.4, 1.5, 1.6, and 1.8 mm) wires/pins are generally used in small animals based on the body weight and bone fracture location (1.0 mm in cats and toy breed dogs to 1.8 mm in giant breed dogs). 2.0–2.5 mm pins may be used in young large animals, calves and foals weighing <100 kg; in animals weighing about 100–200 kg, 3 mm pins; in animals weighing about 200–300 kg, 3.5 mm pins; and in heavy adult animals weighing >300 kg, 3.5–4.5 mm pins. A pair of pins (cross pins) is fixed to each ring under tension using fixation bolts.
Fixation bolts/nuts: Bolts are slotted or cannulated to fix the transfixation pins to the rings. Cannulated bolts have better pin holding strength and are preferred especially in large animal fixation systems [129]. The hole/slot present in the bolt should be optimum to accept the fixation pins intended for use.
Connecting rods/nuts: The number of connecting rods required between each ring block may vary based on the weight of the animal and required fixation rigidity. A minimum of 2–3 connecting rods are used in small animal applications, and at least four rods are fixed in large animals, between the rings by tightening nuts on either side of the rings. The distance between the rings can be adjusted by tightening or loosening the nuts to provide tension or compression between the fracture segments. Five to six millimeter diameter connecting rods are usually used in small animal fixation systems and 8–10 mm connecting rods in large animal fixation systems.
Hybrid external skeletal fixation (HESF) is becoming popular to treat fractures with short segment. Here, the small bone segment near the joint is stabilized using small diameter pins anchored to a ring, and primary large bone segment is stabilized with linear components and pins. As the hybrid frame combines both linear and circular ESF frames, it has the advantages of both the systems and superior mechanical properties [130, 131]. In large animal fracture fixations, hybrid fixation systems are useful to treat fractures of the middle to proximal diaphysis of the tibia and radius, where it is often difficult to fix a circular ring (due to large soft tissue covering and eccentric placement of the bone) [132, 133]. Further, by using linear fixator elements, relatively smaller-size rings can be used, which in turn increases fixator stiffness.
2.3.9.2 Indications
In small animals, CEF is indicated for treatment of certain fractures which are otherwise difficult to treat (severely comminuted open fractures). Other indications are correction of angular deformities, treatment of non-unions, extremity lengthening, and arthrodeses, etc. [91, 98, 134]. In large animals, CEF is mostly used for treatment of long bone fractures, especially of the tibia, where cast application does not provide adequate level of fixation and linear fixation systems are not advised [13, 121, 129, 135,136,137,138]. As CEF is less traumatic with the use of relatively small diameter pins, it is also indicated in open fractures with severe soft tissue injuries to achieve more biological healing. CEF is also indicated in transarticular (particularly trans-tarsal) applications [139]. Fractures of extremities of long bones can also be better treated using a circular or hybrid ESF.
2.3.9.3 Application of CEF
Survey radiography: Radiographs (orthogonal views) of the fractured bone are made before planning for surgical fixation, which will help determine the fracture configuration and location and plan for fixator application (to decide the size and number of fixation pins, location of pin insertion, etc.). Radiographs of the contralateral limb often help determine the normal length of the bone.
Anesthesia and restraint: Under general anesthesia, the patient is preferably restrained in dorsal recumbency with the affected limb under suspension. In large ruminants involving hindlimb surgeries, regional/epidural analgesia can be used along with deep sedation, and the animal can be restrained in lateral recumbency with the fractured limb extended outside the operation table and the open wound facing the surgeon, to facilitate fracture reduction and fixation.
Preparation of the surgical site: The hair is clipped and skin is prepared with surgical scrubbing as for any orthopedic procedure. The preparation of the surgical field must include a joint above and below the fracture, and the whole area is properly draped. Once the surgical site is properly prepared, the proposed sites for placing the transfixation pins are chosen (using radiographic images) and marked.
Construction of fixator assembly: Proper diameter pins, connecting rods, and rings are selected (as described before). The fixator frame can be preassembled based on radiographs and then modified slightly at the time of surgery (Fig. 2.63). The frames should have a minimum of two rings in each major bone segment. The rings are spread along the entire length of each bone segment to achieve maximum mechanical advantage. In case one of the fracture segments is too small, only one ring is positioned at the level of small bone segment, and two rings are positioned at the adjoining normal bone (for transarticular fixation). The rings are interconnected using four equidistantly placed connecting rods between each ring block using nuts. Once all the rings are properly positioned along the connecting rods, the connecting rod-ring interfaces are stabilized by tightening the nuts on either side of the rings.
The fractured limb is inserted into the preassembled CEF frame and held in such a way that the fractured bone is centered within the ring block and the rings are aligned with the chosen level of pin insertion sites.
Fracture reduction: Fracture can be reduced either by closed method or by open method. Closed reduction is less traumatic and does not disturb the blood circulation at the fracture site and facilitate biological healing. Fracture healing and functional recovery are rapid with closed fracture reduction. Closed reduction can be more easily achieved in distal bones of the limb due to least soft tissue covering, especially in fresh cases. If required, semi-open method (by giving a small incision or by extending the wound margin) can be adopted to reduce the bone fragments. In cases with severe overriding of bone segments and adhesions (long-standing cases), open reduction is advised.
Pin insertion technique: Standard pin insertion technique is followed (as described before in detail). About 0.5–1.0 cm long skin incision is made (proximal to distal) at the chosen site of pin insertion, and a similar incision is made at the pin exit point in the opposite skin surface. Predrilling is generally not practiced while passing the pins during CEF fixation. The selected fixation pins are introduced along the dorsal/ventral side of the ring. If possible, one of the cross pins is positioned above the ring and another below the ring to avoid collision within the medullary cavity. The pin is carefully introduced by hand through the soft tissues up to the level of the bone cortex to gently push aside the vessels and nerves. The pin should not be inserted too close to the fracture line (at least 10 mm gap should be present between the fracture line and the pin). The pins are crossed (at 60°–90° angle to each other) from craniomedial to caudolateral and caudomedial to craniolateral direction or vice versa. As the angle between the pins decreases, the bone segment may slide (translate) from the center of the ring. This translation of bone segments can be minimized by using olive wires/beaded pins. Pins are introduced using low-speed (ideal is 150–400 rpm), high torque power drills to avoid wobbling (which could cause premature loosening) and help reduce thermal necrosis of the bone tissue. It is important to drill in small pulses (with 30 s between the pulses) to allow for dissipation of heat generated. While drilling, sterile cold solution is continuously dropped at the skin-pin interface to minimize thermal injury.
It is advisable to first pass one pin each at the level of farther rings (proximal-most and distal-most) and loosely fix the pins to the rings using fixation bolts and nuts (this will allow proper positioning of fixator assembly and fracture reduction and alignment) (Fig. 2.64). Once it is ensured that the fixator frame is properly positioned along the fractured bone/limb and bone segments are adequately aligned, fixation pins are then passed at the level of remaining rings (closer to fracture site) alternatively and fixed to the rings. Once again, the alignment of the fixator and bone segments is re-checked, and if needed, the fixator frame can be slightly manoeuvered (by repositioning the fixation bolts along the ring) to correct. The second set of pins is then passed one by one at the level of each ring (either above or below the rings) and is fixed to the rings.
Fixation of pins with the rings: The transfixation pins are fixed to the rings using slotted or cannulated bolts. Slotted bolts are technically easier to adjust, but cannulated bolts provide greater stability to the fixation. The cannulated bolts are first inserted through both ends of the transfixation pin and slid along till they are at the level of the ring and then inserted into the fixation holes. Care should be taken not to bend the pin while approximating it to the ring. When required, fissured pin-nuts or washers can be used to achieve approximation. Fixation bolt is tightened to the ring using a nut at one end of the pin (beaded end of the pin in olive wires). The fixation pin is then tensioned from the other end, before fixing it with the ring to increase the fixation rigidity. As far as possible, all the pins are equally tensioned to share and distribute load equally. Generally, 20–30 kg force is adequate for animals weighing <10 kg (1 mm pin), 30–60 kg for animals weighing 10–20 kg (1.2 mm pin), and 60–90 kg for animals weighing >20 kg (1.5/1.6 mm pin). Tension should not be more than 30 kg in partial/incomplete rings. Similarly, each pin is snugly fixed to the ring one by one by tightening the nuts along the fixation bolts. Once the pins are fixed to the rings, the extra length of the pins is cut short (using a pin cutter), and the cut end is bent toward the ring and inwardly (with a plier) to avoid any damage to the patient and the handler from the cut end of the pins.
2.3.9.4 Postoperative Care and Management
Management of animals in the immediate post-fixation period is critical (especially large animals), as they may feel discomfort by the presence of the external fixator components. The animal may take some time to get accustomed; hence, regular observation of the animal is required during this period [129]. Regular antiseptic dressing of the pin-skin interfaces and the open wound (in case of open fractures) is done until the healing occurs. Pin site discharge is common; hence, prolonged dressing of the pin-skin interfaces is needed. A broad-spectrum antibiotic is administered for 5–7 days. If prolonged therapy is needed, the antibiotic may be changed as per the sensitivity test.
The fixator frame may be covered with a sleeve or wrapped with a bandage to prevent the animal from licking the pin-skin interfaces and biting the fixator components. However, it is not always required to wrap the fixator, and only the incision site/wound is dressed as the skin surface is generally protected from direct floor contact due to the presence of rings. The exercise is restricted in the immediate post-fixation period; however, walking in a closed enclosure should be allowed as early as possible, as it is an excellent form of physical therapy to accelerate bone healing and regain functional recovery.
2.3.9.5 Removal of Fixator Assembly
After the radiological union of the fracture, the fixation pins are cut using a pin cutter. and the frame is removed. The pins are pulled out with pliers, making sure that the beaded pins are pulled from the side of the bead. After removal of pins, pin tract is cleaned with antiseptic solution, and the activity of the animal is restricted for another week. Generally, pin tracts heal quickly within a few days.
2.3.10 Acrylic- or Epoxy-Pin Fixation Systems
The connecting bars of an ESF frame can be constructed using acrylics, such as polymethyl methacrylate (PMMA) or epoxy materials, instead of steel rods to overcome some of the limitations of metallic fixator components. This type of ‘free-form’ fixation has the advantage that the pins can be passed at different directions regardless of the connecting bar/ring location, and any diameter pin can be used irrespective of the clamp size [140]. Such free-form fixation has been used since long to treat mandibular fractures in small animals and long bone fractures in birds with good success. The modified technique of epoxy-pin fixation described here is very versatile and mechanically strong [123, 141,142,143,144,145], and it can be used to treat various long bone fractures in different species of animals such as dogs, cats, sheep, goats, calves, foals, and birds [146,147,148,149,150]. Generally, all animals and birds weighing up to about 100 kg can be treated. It is economical and also easily applied by a practicing veterinarian with minimal facilities and expertise.
2.3.10.1 Fixator Components
Fixation pins: In general, pins used in free-form fixation are slightly larger than typical CEF as pins cannot be tensioned to increase their strength. Smooth pins (Kirschner wires) of different diameter ranging from 1.2 mm to 2.0 mm are generally used in dogs and cats (based on body weight, 1.2–1.5 mm wires in the metacarpal and metatarsal bones, 1.5–2.0 mm pins in the radius-ulna and tibia), 1.5–2.0 mm pins in sheep and goats, and 2.0–3.0 mm pins in calves and foals. Pins over 3 mm cannot be used as they are difficult to bend.
Acrylic/epoxy material: For acrylic-pin fixation, any commercially available medical-grade acrylic material such as self-curing dental acrylic (Pyrax Polymars), which is easily available and economical, can be used. Along with this, polyvinyl chloride (PVC) pipes of desired diameter (20 mm diameter adequate in most applications) are needed to construct the connecting bars. For epoxy-pin fixation, any commercially available industrial-grade epoxy material can be used, such as M-seal (Pidilite Ltd). They are available as regular or fast curing; fast-curing epoxy can polymerize faster, leading to quick hardening once applied. About 200 g to 1 kg epoxy material may be required to construct a fixator frame as per the species and size of the animal and location of fracture.
2.3.10.2 Indications
Indicated for fixation of long bone fractures (especially open infected fractures) below the elbow and stifle joints in dogs, cats, sheep, goats, calves, foals, and birds (weighing up to 100 kg). It is also indicated for immobilization of joints (below the elbow and stifle) by transarticular fixation (joint luxations, tendon and ligament injuries, and for arthrodesis, etc.) and correction of angular limb (antebrachial) deformities. Fractures of the mandible can also be treated effectively by epoxy-pin fixation.
2.3.10.3 Advantages
Free-form fixation provides stable fixation of fractures in lightweight animals (<100 kg). The technique is very versatile, as the epoxy-pin connecting bars can be angled at the level of the joint without compromising the fixation stability and the connecting bars/rings of different diameters can be constructed. The technique is least cumbersome, does not require fixation clamps or any special instruments/materials, and is economical too. The device is lightweight; hence, small animals and birds can tolerate well. This is very easy to design and apply in clinical situations by practicing veterinarians in any remote corner with minimal facilities and expertise.
2.3.10.4 Technique of Application
Survey radiography: Radiographs (orthogonal views) of the fractured bone help to determine the fracture type and location and plan for fixator application (to decide the size and number of fixation pins, fixator design, etc.).
Anesthesia and restraint: In dogs, cats, foals, and birds, general anesthesia is advised. In sheep, goats, and calves, fixation can be done with deep sedation under regional anesthesia; in hindlimb fractures, epidural analgesia can be used, and in forelimbs, nerve blocks can be used. General anesthesia may be needed in some cases, especially for forelimb fixations. The animal is positioned as for any ESF application. A cotton rope tied at the level of the digits/hoof can help to suspend the limb or may be used to pull the limb straight manually to help in fracture reduction and restraining of the animal during fixator application.
Fracture reduction and alignment: After preparing the fractured limb for aseptic surgery by hair clipping and scrubbing, the fracture segments are reduced and aligned by closed method using traction and counter-traction. Fracture reduction may be easily achieved in metacarpal and metatarsal bones in all species of animals and also in radius-ulna fractures in dogs, cats, sheep, and goats. In some cases, fracture is reduced by maneuvering through the open wound. If needed, the skin wound may be slightly extended to reduce the overriding bone segments. In most fractures of the straight bones, reduced bone segments can be maintained in apposition manually; if needed, bone-holding forceps may be used. In cases of severe overriding, especially in fractures of the tibia, hemi-cerclage wiring may be done to reduce and temporarily stabilize the bone segments. If the fracture reduction is stable, the skin wound may be sutured using simple interrupted sutures by keeping enough space between the sutures for drainage and dressing. Suturing may also be done after fixator application; however, it is slightly more difficult. It is not advised to completely close the skin wound, and in most cases, it may not be possible. Suturing the skin may help in bringing the soft tissue cover around the fracture site and also help secure the reduced bone segments in alignment until fixator application.
Fixation of pins: The proposed sites for transcortical passage of pins (based on radiographic evaluation) are marked on the skin as per the fracture type and fixator design, and small release incisions (4–5 mm) are made. In bilateral uniplanar designs, at least two pins are passed either medio-laterally or latero-medially in both proximal and distal fracture segments (Figs. 2.66, 2.67, 2.68, 2.69, 2.70, 2.71, and 2.72). In multiplanar linear and circular designs, the pins are passed in the same plane from craniomedial to caudolateral and caudomedial to craniolateral directions or vice versa; two pins are passed at one point at an angle of about 60° or more; at least two-point fixation is provided in both fracture segments. Increasing the number of pins increases the fixation rigidity, and it is desirable to use maximum number of transcortical pins spanning the whole length of the bone. When fracture is at one end of the bone (one of the fracture segments is very small), at least two pins are passed in the adjacent normal long bone, spanning the joint area (transarticular fixation). Using standard technique (as described before), the transfixation pins are inserted.
2.3.10.5 Construction of ESF Frame Using Acrylic
After all the pins are inserted, the pins in the same plane are affixed to the PVC pipes (by piercing the pipe through and through the pin ends) to prepare a temporary scaffold of connecting bars (in uniplanar design, two connecting bars, and in multiplanar design, four connecting bars) (Figs. 2.65 and 2.66). The connecting bars (PVC pipes) are aligned close to the skin leaving a gap of about 2 cm from the skin. The connecting bars on both sides can also be joined at proximal and distal ends (by using a single long PVC pipe), which will help prevent movement of pins during the post-fixation period. The acrylic powder (polymer) and liquid hardener (monomer) are mixed in a pre-cooled glass beaker with the help of a spatula, immediately before application with continuous stirring, to maintain a flowing consistency. If it becomes hard due to delay in application, it should be discarded and a fresh mix prepared. Acrylic is poured into the PVC pipes in semi-liquid (dough) state with the hollow pipes sealed at the bottom using an adhesive tape. Care should be taken to prevent any leakage of the liquid acrylic from the points of pin insertion, by reinforcing the pin insertion points with an adhesive tape. The acrylic dough is allowed to flow down the pipe making sure that the complete PVC column is filled uniformly without leaving any air pockets. The acrylic is then allowed to polymerize and harden for 10–15 min. As polymerization is an exothermic reaction releasing heat, thermal injury to the tissues may occur, which can be prevented by using cold saline and ice packs around the skin. The fumes produced during polymerization are noxious and toxic; hence, one should wear mask while mixing acrylic powder with liquid, and adequate care is taken to reduce the production of fumes by mixing acrylic part by part in a pre-cooled glass beaker.
Acrylic-pin ESF (multiplanar type III) applied for treatment of tibial and radius-ulna fractures in dogs. (a) four independent connecting bars are constructed, (b and c) connecting bars on both sides are joined at the proximal and distal ends, which provide more stable fixation by preventing bone translation
2.3.10.6 Construction of Pin Scaffold for Epoxy-Pin Fixation
Once all the transfixation pins are placed, the pins in the same plane are bent toward the fracture site (proximal pins are bent downwards; distal pins are bent upwards) using a pin bender (Figs. 2.67 and 2.68). The pins are bent as close to the bone as possible, by leaving a gap of at least 2 cm between the skin and the connecting bar to allow inflammatory swelling and dressing of the wounds. The bent pins are joined using an adhesive tape. If the fixation pins are long enough, they may connect each other after bending. If the bent pins do not connect, additional pieces of pins can be used to join them. In multiplanar design, after joining the bent fixation pins to make connecting bar scaffold, the two connecting bars on each side may be joined at the proximal and distal ends (using additional pieces of pins) to make a rectangular frame, which can strengthen the fixation stability (Figs. 2.69, 2.70, 2.71, and 2.72). If the connecting bars are very long (as in transarticular fixation), additional articulations may be fixed between the connecting bars at the center of the frame. Alternatively, all the four connecting bars may be joined using additional pieces of pins at desired locations (at least one each at proximal and distal ends) of the scaffold to construct a circular fixator frame. Variable size/length/shape connecting bars/rings can be constructed on the spot as per the case situation.
2.3.10.7 Application of Epoxy Dough Along the Pin Scaffold
After making the scaffold of interconnecting pins, the fracture fixation is checked for the alignment of bone segments again, as it is possible to correct minor defects in angulation/alignment even at this stage. After ensuring proper reduction of fracture segments, the epoxy resin and hardener are thoroughly mixed to make uniform colored dough. The epoxy dough is then applied along the pin scaffold so as to incorporate the bent pins within the mold (Figs. 2.67d, 2.69f, and 2.71e). The connecting bars and the circular rings are thus constructed keeping the fracture segments in alignment. Care is taken to maintain the continuity of the epoxy dough without any break/crack while constructing the fixator frame.
The diameter of the connecting bars/rings may vary as per the fracture situation and weight of the animal. In small animals (dogs, cats, sheep, and goats), 10–20 mm diameter connecting bars, and in calves and foals, 20–25 mm diameter connecting bars may be needed. The surface of the connecting bars/rings is smoothened using oily/waxy surface. The epoxy-pin construct is then allowed to ‘set (harden)’ for about 30–60 min. During this time, the animal should be completely restrained to prevent any inadvertent movement of the fixator frame. Once hardened, the fixator frame becomes very strong, and the animal can be allowed to bear weight on the limb.
2.3.10.8 Postoperative Care and Management
The animal should be allowed only limited weight-bearing soon after bone fixation. Weight-bearing can be gradually increased after about 1–2 weeks in stable fractures. In unstable fractures, prolonged immobilization may be needed to prevent any undue load at the fracture site. Regular antibiotic and anti-inflammatory drugs should be administered for 3–5 days, as per the case. If infection persists, prolonged antibiotic therapy is advised (as per the sensitivity test). The external fixator components are regularly watched for any change in the position and shape (bending/breakage) of fixator components. The pin-skin interfaces are regularly cleaned with antiseptic solution, so till complete healing of the open wound. Every 15 days, the animal is subjected to radiographic examination to observe for the status of fixation and bone healing.
2.3.10.9 Removal of Fixator Assembly
Once the radiographic healing (bridging callus) is evident, the fixator assembly is removed by cutting the fixation pins (between the skin and connecting bars) on both sides using a pin cutter. The cut ends of the pins are pulled out using a plier, and the pin holes are flushed using an antiseptic solution such as povidone iodine. After the removal of the fixator, the limb may be provided with external support in the form of splint and bandages for 1–2 weeks.
2.3.11 Complications of ESF
After ESF application, certain complications can develop, which may include pin-tract sepsis and drainage, pin loosening and breakage, fracture instability, and pin-tract fractures. Most of these complications can be minimized by selecting appropriate fixation device, following proper technique of fixation along with good postoperative care and management.
The pin-tract infection and drainage are the most common complications reported with the use of an ESF both in pet and domestic animals. Slight pin-tract discharge is expected in the initial period of fixation. Pin-tract discharge is directly proportional to fixation rigidity; in most cases with rigid bone fixation, pin-tract discharge is the least, whereas instability at fracture site may increase the occurrence of pin-tract infection and drainage. Pin-tract drainage is generally more in proximal limb locations, where there is more soft tissue mass. Pin-tract drainage may be prevented or minimized by adopting proper fixation technique, including pin insertion (use of release incisions), and application of compressive bandage in the early post-fixation period.
Another complication commonly observed with ESF is loosening of fixation pins. Thermal necrosis of the bone around the pin tract during pin insertion can lead to resorption of the bone leading to widening of pin tracts and pin loosening. Predrilling the pin hole, drilling with low rpm power drill, use of cold saline solution at pin-skin interfaces while drilling, and drilling in small pulses by allowing 30 s between pulses can help reduce thermal necrosis along the pin tracts. High stress exerted at pin-skin interfaces (due to pin placement very close to the fracture), inadequate stiffness of ESF frame, excessive movement of soft tissues around the fixation pins (due to inadequate release of soft tissues during pin insertion), and development of infection along the pin tracts will also increase the chances of loosening of fixation pins. Loose pins can lead to continuous pain and may predispose to osteomyelitis, delayed union or non-union, and fracture disease. It is advised to remove the loose fixation pin, especially if the pin tract is infected, and make sure to increase the stability of ESF by using additional fixation pins if needed. In case of infection, the pin tract should be debrided and flushed with antiseptic solution along with administration of systemic antibiotics after antimicrobial sensitivity testing.
Fracture through pin tracts is another complication of ESF application but rarely reported. This normally results from improper surgical technique such as the use of large diameter pins (more than one third the bone diameter), placement of pins very close to fracture site or another pin, and inadequate movement restriction postoperatively. In such cases, it is advised to remove the broken pin and replace it with another pin placed in intact major bone segment to increase the fixator stability.
Laminitis of the contralateral limb is common in large animal ESF applications. Horses are more prone to contralateral limb laminitis than cattle. Prevention and management of this condition are detailed in Chapter 8.
References
Adams, S.B., and J.F. Fessler. 1988. Fracture repair. In Textbook of large animal surgery, ed. F.W. Oehme, 2nd ed. Baltimore: Williams and Wilkins.
Anderson, D.E., and St. Jean, G. 2008. Management of fractures in field settings. The Veterinary Clinics of North America. Food Animal Practice 24: 567–582.
Charnley, J. 1963. 1963. The mechanics of conservative treatment. In The closed treatment of common fractures, ed. J. Charnley, 43–59. Philadelphia: Williams & Wilkins.
Dyce, J. 1998. Conservative management of fractures. In BSAVA manual of small animal fracture repair and management, ed. A.R. Coughlan and A. Miller. Cheltenham: British Small Animal Veterinary Association.
Harasen, G. 2012. Orthopedic therapy under wraps: the pros and cons of external coaptation. The Canadian Veterinary Journal 53: 679–680.
Leighton, R.L. 1991. Principles of conservative fracture management: splints and casts. In: fracture management. I, Boudrieau RJ (ed.). Semin Vet Med Surg Small Anim. 6: 39–51.
Nunamaker, D.M. 1985. Methods of closed fixation. In Textbook of small animal orthopaedics, ed. C.D. Newton and D.M. Nunamaker, 1st ed., 249–259. Philadelphia: JB Lippincott.
Hohn, R.B. 1975. Principles and application of plaster casts. The Veterinary Clinics of North America. Small Animal Practice 5: 291–303.
Levet, T., A. Martens, L. Devisscher, L. Duchateau, L. Bogaert, and L. Vlaminck. 2009. Distal limb cast sores in horses: risk factors and early detection using thermography. Equine Veterinary Journal 41: 18–23.
Meeson, R.L., C. Davidson, and G.I. Arthurs. 2011. Soft-tissue injuries associated with cast application for distal limb orthopedic conditions. A retrospective study of sixty dogs and cats. Veterinary and Comparative Orthopaedics and Traumatology 24: 126–131.
Tomlinson, J. 1991. Complications with fractures repaired with casts and splints. The Veterinary Clinics of North America. Small Animal Practice 21: 735–744.
Sangwan, V., G.P. Yadav, and A. Kumar. 2020. Aluminium splint incorporated fibreglass cast preserves limb function in bovines with olecranon fracture. Veterinary and Comparative Orthopaedics and Traumatology 33: 434–442.
Singh, A.P., G.R. Singh, H.P. Aithal, and P. Singh. 2020. Section D – fractures, chapter on the musculoskeletal system. In Ruminant surgery: A textbook of the surgical diseases of cattle, buffaloes, camels, sheep and goats, ed. J. Singh, S. Singh, and R.P.S. Tyagi, 2nd ed. New Delhi: CBS Publishers and Distributers.
Solanki, K.P., P.B. Patel, V.D. Dodia, J.V. Vadalia, R.J. Raval, H.M. Padheriya, and M.D. Khatariya. 2016. Comparative effectiveness of plaster of Paris and fibre glass casts in the management of long bone fractures in canines. International Journal of Environmental Science and Technology 5: 3512–3515.
Wilson, D.G., and R. Vanderby Jr. 1995. An evaluation of six synthetic casting materials. Veterinary Surgery 24: 55–59.
Wilson, D.G., and R. Vanderby Jr. 1995. An evaluation of fiberglass cast application techniques. Veterinary Surgery 24: 118–121.
Schroeder, E.F. 1933. The traction principle in treating fractures of the dog and cat. The North American Veterinarian 14: 32–36.
Adams, S.B., and J.F. Fessler. 1983. Treatment of radial, ulnar and tibial fractures in cattle, using a modified Thomas splint cast combination. Journal of the American Veterinary Medical Association 183: 430–433.
Baird, A.N., and S.B. Adams. 2014. Use of the Thomas splint and cast combination, walker splint, and spica bandage with an over the shoulder splint for the treatment of fractures of the upper limbs in cattle. The Veterinary Clinics of North America. Food Animal Practice 30: 77–90.
Ladefoged, S., S. Grulke, V. Busoni, D. Serteyn, A. Salciccia, and D. Verwilghen. 2017. Modified Thomas splint-cast combination for the management of limb fractures in small equids. Veterinary Surgery 46: 381–388.
Howard, P.E. 1991. Principles of intramedullary pin and wire fixation. In Fracture management. I, Boudrieau RJ (ed.). Semin Vet Med Surg Small Anim 6: 52–67.
Nunamaker, D.M. 1985. Methods of internal fixation. In Textbook of small animal Orthopaedics, ed. C.D. Newton and D.M. Nunamaker, 1st ed., 261–286. Philadelphia: JB Lippincott.
Rudy, R.L. 1975. Principles of intramedullary pinning. The Veterinary Clinics of North America. Small Animal Practice 5: 209–228.
Martin, R.A., J.L. Milton, P.K. Shires, et al. 1988. Closed reduction and blind pinning of selected fractures and luxations in dogs and cats. Compendium on Continuing Education for the Practicing Veterinarian 10: 784–799.
Newmann, M.E., and J.L. Milton. 1989. Closed reduction and blind pinning of 29 femoral and tibial fractures in 27 dogs and cats. Journal of the American Animal Hospital Association 25: 61–68.
De Young, D.J., and C.W. Probst. 1985. Methods of fracture fixation. In Textbook of small animal surgery, ed. D.H. Slatter, vol. 2, 1949–2014. Philadelphia: PA Saunders.
Chaffee, V.W. 1977. Multiple (stacked) intramedullary pin fixation of humeral and femoral fractures. Journal of the American Animal Hospital Association 13: 599–601.
Rush, L.V. 1959. Atlas of Rush pin technics. Berivon
Aithal, H.P., G.R. Singh, A.K. Sharma, and Amarpal. 1998. Modified technique of single pin fixation and cross intramedullary pin fixation technique for supracondylar femoral fracture in dogs: A comparative study. Indian Journal of Veterinary Surgery 19: 84–89.
Whitney, W.O., and S.C. Schrader. 1987. Dynamic intramedullary crosspinning technique for repair of distal femoral fractures in dogs and cats: 71 cases (1981-1985). Journal of the American Veterinary Medical Association 191: 1133–1138.
Jenny, J. 1950. Kuntscher’s medullary mailing in femur fractures of the dog. Journal of the American Veterinary Medical Association 117: 381–387.
Déjardin, L.M., K.L. Perry, D.J.F. von Pfeil, and L.P. Guiot. 2020. Interlocking nails and minimally invasive osteosynthesis. The Veterinary Clinics of North America. Small Animal Practice 50 (1): 67–100.
Dueland, R.T., K.A. Johnson, S.C. Roe, M.H. Engen, and A.S. Lesser. 1999. Interlocking nail treatment of diaphyseal long-bone fractures in dogs. Journal of the American Veterinary Medical Association 214 (1): 59–66.
Durall, I., and M.C. Diaz. 1996. Early experience with the use of an interlocking nail for the repair of canine femoral shaft fractures. Veterinary Surgery 25: 397–406.
Larin, A., C.S. Eich, R.B. Parker, and W.P. Stubbs. 2001. Repair of diaphyseal fractures in cats using interlocking intramedullary nails: 12 cases (1996-2000). Journal of the American Veterinary Medical Association 219 (8): 1098–1104.
Raghunath, M., and S.S. Singh. 2003. Use of static intramedullary interlocking nail for repair of comminuted/segmental femoral diaphyseal fractures in four dogs. Indian Journal of Veterinary Surgery 24: 89–91.
Wheeler, J.L., W.P. Stubbs, D.D. Lewis, and A.R. Cross. 2004. Intramedullary interlocking nail fixation in dogs and cats: biomechanics instrumentation. Compendium on Continuing Education for the Practising Veterinarian -North American 26 (7): 519–529.
Bellon, J., and P.-Y. Mulon. 2011. Use of a novel intramedullary nail for femoral fracture repair in calves: 25 cases (2008-2009). Journal of the American Veterinary Medical Association 238: 1490–1496.
Bhat, S.A., H.P. Aithal, P. Kinjavdekar, Amarpal, M.M.S. Zama, P.C. Gope, A.M. Pawde, R.A. Ahmad, and M.B. Gugjoo. 2014. An in vitro biomechanical investigation of an intramedullary interlocking nail system developed for buffalo tibia. Veterinary and Comparative Orthopaedics and Traumatology 27: 36–44.
Dilipkumar, D., M. Patil, B.V. Shivaprakash, Bhagavantappa B.N. Venkatgiri, D. Jahangir, A. Mahesh, and S. Arunkumar. 2019. Intramedullary interlocking nail fixation for repair of long bone fractures in cattle. Indian Journal of Veterinary Surgery 40: 48–51.
Madhu, D.N. 2015. Development and evaluation of interlocking nail and tubular locking plate for management of femur fracture in large ruminants. PhD thesis submitted to Deemed University, Indian Veterinary Research Institute, Izatnagar- 243 122 (UP), India.
Marturello, D.M., K.M. Gazzola, and L.M. Déjardin. 2019. Tibial fracture repair with angle-stable interlocking nailing in 2 calves. Veterinary Surgery 48: 597–606.
Nuss, K. 2014. Plates, pins and interlocking nails. The Veterinary Clinics of North America. Food Animal Practice 30: 91–126.
McClure, S.R., J.P. Watkins, and R.B. Ashman. 1998. An in vivo evaluation of intramedullary interlocking nail fixation of transverse femoral osteotomies in foals. Veterinary Surgery 27: 29–36.
Watkins, J.P., and R.B. Ashman. 1990. Intramedullary interlocking nail fixation in foals: effects on normal growth and development of the humerus. Veterinary Surgery 19: 80.
Boudrieau, R.J. 1991. Principles of screw and plate fixation. Seminars in Veterinary Medicine and Surgery (Small Animal) 6 (1): 75–89.
Brinker, W.O., R.B. Hohn, and W.D. Prieur. 1984. Manual of internal fixation in small animals. New York: Springer.
Igna, C., and L. Schuszler. 2010. Current concepts of internal plate fixation of fractures. Bulletin of University of Agricultural Sciences and Veterinary Medicine 67 (2): 118–124.
Muller, M.E., M. Allgower, R. Schneider, and H. Willenegger. 1979. Manual of internal fixation. 2nd ed. New York: Springer-Verlag.
Allgower, M., R. Ehrsahm, and R. Ganz. 1969. Clinical experience with a new compression plate “DCP”. Acta Orthopaedica Scandinavica. Supplementum 125: 46–61.
Allgower, M., S.M. Perren, and P. Matter. 1970. A new plate for internal fixation-the dynamic compression (DCP). Injury 2: 40–47.
Ayyappan, S. 2013. AO techniques of dynamic compression plate (DCP) and limited contact dynamic compression plate (LC-DCP) application for fracture management in dogs. Advances in Animal and Veterinary Sciences 1 (2S): 33–36.
Perren, S.M., M. Russenberger, S. Steinemann, M.E. Muller, and M. Allgower. 1969. A dynamic compression plate. Acta Orthopaedica Scandinavica. Supplementum 125: 31–41.
Schatzer, J. 1991. Screws and plates and their applications. In Manual of internal fixation techniques recommended by the AO-ASIF group, ed. M. Allgower, 3rd ed., 179–199. Cham: Springer.
Uhthoff, H.K., P. Poitras, and D.S. Backman. 2006. Internal plate fixation of fractures: short history and recent developments. Journal of Orthopaedic Science 11 (2): 118–126.
Perren, S.M., K. Klaue, O. Pohler, M. Predieri, S. Steinemann, and E. Gautier. 1990. The limited contact dynamic compression plate (LC-DCP). Archives of Orthopaedic and Trauma Surgery 109: 304–310.
Nunamaker, D.M., K.F. Bowman, D.W. Richardson, and M. Herring. 1986. Plate luting: a preliminary report of its use in horses. Veterinary Surgery 15 (4): 289–293.
Nunamaker, D.M., D.W. Richardson, and D.M. Butterweck. 1991. Mechanical and biological effects of plate luting. Journal of Orthopaedic Trauma 5 (2): 138–145.
Bruese, S., J. Dee, and W.D. Prieur. 1989. Internal fixation with a veterinary cuttable plate in small animals. Veterinary and Comparative Orthopaedics and Traumatology 1: 40–46.
Theoret, M.C., and N.M.M. Moens. 2007. The use of veterinary cuttable plates for carpal and tarsal arthrodesis in small dogs and cats. The Canadian Veterinary Journal 48 (2): 165–168.
Lewis, D.D., R.T. van Ee, M.G. Oakes, and A.D. Elkins. 1993. Use of reconstruction plates for stabilization of fractures and osteotomies involving the supracondylar region of the femur. Journal of the American Animal Hospital Association 29: 171–178.
Anson, L.W., D.J. De Young, D.C. Richardson, and C.W. Betts. 1988. Clinical evaluation of canine acetabular fractures stabilized with an acetabular plate. Veterinary Surgery 17: 220–225.
Braden, T.D., and W.D. Trieur. 1986. New plate for acetabular fractures: technique of application and long-term follow-up evaluation. Journal of the American Veterinary Medical Association 188: 1183–1186.
Brinker, W.O., R.B. Hohn, and W.D. Prieur. 1998. Manual of internal fixation in small animals. Berlin: Springer.
Barnhart, M.D., and K.C. Maritato. 2018. Locking plates in veterinary orthopaedics. ACVS Foundation, Wiley Blackwell. Onlinelibrary.wiley.com/doi/book/10.1002/9781119380139
Frigg, R. 2001. Locking compression plate (LCP). An osteosynthesis plate based on the dynamic compression plate and the point contact fixator (PC-fix). Injury 32: 63–66.
Frigg, R. 2003. Development of locking compression plate. Injury 34: S-B6-10.
Gautier, E., and C. Sommer. 2003. Guidelines for the clinical application of the LCP. Injury 34: S-B63-76.
Kowaleski, M. 2009. Locking plate systems: LCP. In: Proceedings spring scientific meeting, British veterinary Orthopaedic association, Moores A (ed.), 1st April 2009, Austin Court, Birmingham. p 1–3.
Kowaleski, M. 2009. Locking plate systems: SOP and ALPS. In: proceedings spring scientific meeting, British veterinary Orthopaedic association. Moores A (ed.), 1st April 2009, Austin Court, Birmingham. pp. 4–9.
Wagner, M. 2003. General principles for the clinical use of the LCP. Injury 34: S-B31-B42.
Wagner, M., and R. Frigg. 2006. AO manual of fracture management, internal fixators: concepts and cases using LCP and LISS, 1–57. Clavadelerstrasse: AO Publishing.
Aguila, A.Z., J.M. Manos, A.S. Orlansky, R.J. Todhunter, E.J. Trotter, and M.C.H. Van der Meulen. 2005. In vitro biomechanical comparison of limited contact dynamic compression plate and locking compression plate. Veterinary and Comparative Orthopaedics and Traumatology 18: 220–226.
Egol, K.A., E.N. Kubiask, E. Fulkerson, F.J. Kummer, and K.J. Koval. 2004. Biomechanics of locked plates and screws. Journal of Orthopaedic Trauma 18 (8): 488–493.
Keller, M., and K. Voss. 2002. AO vet news. UniLock: applications in small animals. AO Dialogue 15: 20–21.
Gamper, S., A. Steiner, K. Nuss, S. Ohlerth, A. Fürst, J.G. Ferguson, J.A. Auer, and C. Lischer. 2006. Clinical evaluation of the CRIF 4.5/5.5 system for long-bone fracture repair in cattle. Veterinary Surgery 35: 361–368.
Reems, M.R., B.S. Beale, and D.A. Hulse. 2003. Use of a clamp-rod construct and principles of biological osteosynthesis for repair of diaphyseal fractures in dogs and cats: 47 cases (1994-2001). Journal of the American Veterinary Medical Association 223: 330–335.
Zahn, K., and U. Matis. 2004. The clamp rod internal fixator- application and results in 120 small animal fracture patients. Veterinary and Comparative Orthopaedics and Traumatology 17: 110–120.
Ahmad, R.A. 2013. Development and evaluation of designer locking plates for fixation of tibial and radial fractures in large ruminants. PhD thesis submitted to Deemed University, Indian Veterinary Research Institute, Izatnagar- 243 122 (UP), India.
Ahmad, R.A., H.P. Aithal, Amarpal, P. Kinjavdekar, P.C. Gope, and D.N. Madhu. 2021. Biomechanical properties of a novel locking compression plate to stabilize oblique tibial osteotomies in buffaloes. Veterinary Surgery 50: 444–454.
Hudson, C.C., A. Pozzi, and D.D. Lewis. 2009. Minimally invasive plate osteosynthesis: applications and techniques in dogs and cats. Veterinary and Comparative Orthopaedics and Traumatology 3: 175–182.
Krettek, C., M. Muller, and T. Miclau. 2001. Evolution of minimally invasive plate osteosynthesis (MIPO) in the femur. Injury 32 (Suppl 3): C14–C23.
Schmokel, H.G., S. Stein, H. Radke, K. Hurter, and P. Schawalder. 2007. Treatment of tibial fractures with plates using minimally invasive percutaneous osteosynthesis in dogs and cats. The Journal of Small Animal Practice 48: 157–160.
Tong, G., and S. Bavonratanvech. 2007. AO manual of fracture management: minimally invasive plate osteosynthesis (MIPO), 3–7. Clavadelerstrasse: AO Publishing.
Morshead, D. 1982. Fracture fixation with Kirschner wires. Compendium on Continuing Education for the Practicing Veterinarian 4: 491–501.
Gambardella, P.C. 1980. Full cerclage wires for fixation of long bone fractures. Compendium on Continuing Education for the Practicing Veterinarian 2: 665–671.
Withrow, S.J. 1978. Use and misuse of full cerclage wires in fracture repair. The Veterinary Clinics of North America. Small Animal Practice 8: 201–212.
Birchard, S.J., and R.M. Bright. 1981. The tension band wire for fracture repair in the dog. Compendium on Continuing Education for the Practising Veterinarian 3: 37–41.
Petit, G.B., and D.H.J.S. Slatter. 1973. Tension band wiring for fixation of avulsed canine tibial tuberosity. Journal of the American Veterinary Medical Association 163: 242–244.
Corr, S.A. 2005. Practical guide to linear external skeletal fixation in small animals. In Practice 27 (2): 76–85.
Bilgili, H. 2004. Circular external fixation system of Ilizarov: part V. fracture treatment by the Ilizarov technique. Veteriner Cerrahi Dergisi 10 (1–2): 75–89.
Carnmichael, S. 1991. The external fixator in small animal orthopaedics. The Journal of Small Animal Practice 32: 486–493.
Egger, E.L. 1998. External skeletal fixation. In Current techniques in small animal surgery, Bojrab, ed. M.J., 4th ed., 941–950. Philadelphia.
Harari, J., T. Bebchuk, B. Segun, and J. Lincoln. 1996. Closed repair of tibial and radial fractures with external skeletal fixator. Compendium on Continuing Education for the Practising Veterinarian 18: 651–657.
Ilizarov, G.A. 1992. The apparatus: components and biomechanical principles of application. In Transosseous Osteosynthesis, ed. S.A. Green, 63–136. Berlin: Springer-Verlag.
Johnson, A.L., and C.E. DeCamo. 1992. External skeletal fixation- linear fixation. The Veterinary Clinics of North America. Small Animal Practice 29: 1135–1143.
Lewis, D.D., A.R. Cross, S. Carmichael, and M.A. Anderson. 2001. Recent advances in external skeletal fixation. The Journal of Small Animal Practice 42: 103–112.
Marcellin-Little, D.J. 1999. Fracture treatment with circular external fixation. The Veterinary Clinics of North America. Small Animal Practice 29: 1153–1170.
Ozsoy, S., and K. Altunatmaz. 2003. Treatment of extremity fractures in dogs using external fixators with closed reduction and limited open approach. Veterinary Medicine Czech 48: 133–140.
Aron, D.N., J.P. Toombs, and S.C. Hollingworth. 1986. Primary treatment of severe fractures by external skeletal fixation: threaded pins compared with smooth pins. Journal of the American Animal Hospital Association 22: 659–670.
Toombs, J.P. 1992. Trans articular application of external skeletal fixation. The Veterinary Clinics of North America. Small Animal Practice 22: 181–194.
Morshead, D., and E.B. Leeds. 1984. Kirschner-Ehmer apparatus immobilization following Achilles tendon repair in six dogs. Veterinary Surgery 13: 11–14.
Bilgili, H., and B. Olcay. 1998. Circular external fixation system of Ilizarov: part I. history, components, indications and principles of system. Turkish Journal of Veterinary Surgery 4: 62–67.
Johnson, A.L., J.A.C. Eurel, J.M. Losonsky, and E.L. Egger. 1998. Biomechanics and biology of fracture healing with external skeletal fixation. Compendium on Continuing Education for the Practising Veterinarian 20: 487–500.
Toombs, J.P. 1991. Principles of external skeletal fixation using the Kirschner-Ehmer splint. Seminars in Veterinary Medicine and Surgery (Small Animal) 6 (1): 68–74.
Egger, E.L., D.G. Lewallen, and R.W. Norrdin, et al. 1988. Effect of destabilizing rigid external fixation on healing of unstable canine osteotomies. Transactions of the 34th Annual Meeting of Orthopedic Research Society 13: 302.
Aron, D.N., and J.P. Toombs. 1984. Updated principles of external skeletal fixation. Compendium on Continuing Education for the Practicing Veterinarian 6: 845–858.
Green, S.A. 1991. The Ilizarov method. Rancho technique. The Orthopedic Clinics of North America 22: 677–688.
Hierholzer, G., R. Kleining, G. Horster, and P. Zemenides. 1978. External fixation- classification and indications. Archives of Orthopaedic and Trauma Surgery 92: 175–182.
Egger, E.L. 1990. Biomechanics and fracture healing with external fixation. In Proceedings 18th annual veterinary surgical forum, Chicago, IL. p 321–323.
Kummer, F.J. 1992. Biomechanics of the Ilizarov external fixator. Clinical Orthopaedics 280: 11–14.
Kürüm, B., H. Bilgili, and C. Yardımcı. 2002. Circular external fixation system of Ilizarov. Part IV: biomechanical properties of the system. Turkish Journal of Veterinary and Animal Sciences 8: 107–115.
Lewis, D.D., D.G. Bronson, M.L. Samchukov, R.D. Welch, and J.T. Stallings. 1998. Biomechanics of circular external skeletal fixation. Veterinary Surgery 27: 454–464.
Paley, D. 1991. Biomechanics of the Ilizarov external fixator. In Operative principles of Ilizarov, ed. A. Bianchi-Maiocchi and J. Aronson, 33–41. Milan: Medi Surgical Video.
Kraus, K.H., H.M. Wotton, R.J. Boudrieau, L. Schwarz, D. Diamond, and A. Minihan. 1998. Type-II external fixation, using new clamps and positive-profile threaded pins, for treatment of fractures of the radius and tibia in dogs. Journal of the American Veterinary Medical Association 212: 1267–1270.
Aron, D.N., and C.W. Dewey. 1992. Application and postoperative management of external skeletal fixators. The Veterinary Clinics of North America. Small Animal Practice 22 (1): 69–98.
Egger, E.L. 1990. Principles of fracture management- the use of external skeletal fixation. In Canine orthopedics, ed. W.G. Whittick, 2nd ed., 248–264. Philadelphia: Lea & Febiger.
Ramakumar, V., M. Manohar, and R.P.S. Tyagi. 1973. Hanging pin cast for oblique fracture of tibia in a cow-A disadvantage. The Indian Veterinary Journal 50: 714–716.
Lescun, T.B., S.R. McClure, M.P. Ward, C. Downs, D.A. Wilson, S.B. Adams, J.F. Hawkins, and E.L. Reinertson. 2007. Evaluation of transfixation casting for treatment of third metacarpal, third metatarsal, and phalangeal fractures in horses: 37 cases (1994-2004). Journal of the American Veterinary Medical Association 230: 1340–1349.
Lozier, J.W., A.J. Niehaus, A. Muir, and J. Lakritz. 2018. Short- and long-term success of transfixation pin casts used to stabilize long bone fractures in ruminants. The Canadian Veterinary Journal 59: 635–641.
Aithal, H.P. 2015. Management of fractures. In A handbook on field veterinary surgery, ed. M.M.S. Zama, H.P. Aithal, and A.M. Pawde, 145–154. New Delhi: Published by Astral.
Aithal, H.P., Amarpal, P. Kinjavdekar, A.M. Pawde, K. Pratap, P. Kumar, D.K. Sinha, and H.C Setia. 2009. A novel bilateral linear external skeletal fixation device for treatment of long bone fractures in large animals: A report of 12 clinical cases. 33rd Congress of ISVS held at Veterinary college, GADVASU, Ludhiana (Punjab), 11–13 Nov. 2009, Abst: OR-1.
Dubey, P., H.P. Aithal, P. Kinjavdekar, Amarpal, P.C. Gope, D.N. Madhu, Rohit Kumar, T.B. Sivanarayanan, A.M. Pawde, and M.M.S. Zama. 2021. A comparative in vitro biomechanical investigation of a novel bilateral linear fixator vs. circular and multiplanar epoxy-pin external fixation systems using a fracture model in buffalo metacarpal bone. World Journal of Surgery and Surgical Research 4: 1331.
Singh, G.R., H.P. Aithal, Amarpal, P. Kinjavdekar, S.K. Maiti, M. Hoque, A.M. Pawde, and H.C. Joshi. 2007. Evaluation of two dynamic axial fixators for large ruminants. Veterinary Surgery 36: 88–97.
Singh, G.R., H.P. Aithal, R.K. Saxena, P. Kinjavdekar, Amarpal, M. Hoque, S.K. Maiti, A.M. Pawde, and H.C. Joshi. 2007. In-vitro biomechanical properties of linear, circular and hybrid external skeletal fixation devices developed for use in large ruminants. Veterinary Surgery 36: 80–87.
Nash, R.A., D.M. Nunamaker, and R. Boston. 2001. Evaluation of a tapered-sleeve transcortical pin to reduce stress at the bone-pin interface in metacarpal bones obtained from horses. American Journal of Veterinary Research 62: 955–960.
Nunamaker, D.M., and R.A. Nash. 2008. A tapered sleeve transcortical pin external skeletal fixation device for use in horses: development, application, and experience. Veterinary Surgery 37: 725–732.
Nunamaker, D.M., D.W. Richardson, D.M. Butterweck, M.T. Provost, and R. Sigafoos. 1986. A new external skeletal fixation device that allows immediate full weight bearing: application in the horse. Veterinary Surgery 15: 345–355.
Aithal, H.P., G.R. Singh, M. Hoque, S.K. Maiti, P. Kinjavdekar, Amarpal, A.M. Pawde, and H.C. Setia. 2004. The use of circular external skeletal fixation device for the management of long bone osteotomies in large ruminants: an experimental study. Journal of Veterinary Medicine A51: 284–293.
Farese, J.P., D.D. Lewis, A.R. Cross, K.E. Collins, G.M. Anderson, and K.B. Halling. 2002. Use of IMEX SK-circular external fixator hybrid constructs for fracture stabilization in dogs and cats. Journal of the American Animal Hospital Association 38: 279–289.
Rao, J.R., V.G. Kumar, T.M. Rao, D.P. Kumar, K.C.S. Reddy, and K.B.P. Raghavender. 2016. Use of hybrid external fixation technique in the repair of long bone fractures in dogs. International Journal of Current Microbiology and Applied Sciences 5 (11): 579–586.
Aithal, H.P., G.R. Singh, P. Kinjavdekar, Amarpal, M. Hoque, S.K. Maiti, A.M. Pawed, and H.C. Setia. 2007. Hybrid construct of linear and circular external skeletal fixation devices for fixation of long bone osteotomies in large ruminants. The Indian Journal of Animal Sciences 77: 1083–1090.
Shah, M.A., Rohit Kumar, P. Kinjavdekar, Amarpal, H.P. Aithal, Mohammad Arif Basha, and Asif Majid. 2022. The use of circular and hybrid external skeletal fixation systems to repair open tibial fractures in large ruminants: a report of six clinical cases. Veterinary Research Communications 46: 563–575.
Marcellin-Little, D.J., A. Ferretti, S.C. Roe, and D.J. Deyoung. 1998. Hinged Ilizarov external fixation for correction of antebrachial deformities. Veterinary Surgery 27: 231–245.
Aithal, H.P., Amarpal, P. Kinjavdekar, A.M. Pawde, G.R. Singh, and H.C. Setia. 2010. Management of tibial fractures using a circular external fixator in two calves. Veterinary Surgery 39: 621–626.
Bilgili, H., B. Kurum, and O. Captug. 2008. Use of a circular external skeletal fixator to treat comminuted metacarpal and tibial fractures in six calves. The Veterinary Record 163: 683–687.
Gulaydin, A., and M. Sarierler. 2018. Treatment of long bone fractures in calves with Ilizarov external fixator. Veterinary and Comparative Orthopaedics and Traumatology 31 (5): 364–372.
Olcay, B., H. Bilgili, and B. Kürüm. 1999. Treatment of communitive diaphyseal metacarpal fracture in a calf using the Ilizarov circular external fixation system. Israel Journal of Veterinary Medicine 54: 122–127.
Aithal, H.P., Amarpal, P. Kinjavdekar, A.M. Pawde, G.R. Singh, M. Hoque, S.K. Maiti, and H.C. Setia. 2007. Management of fractures near carpal joint of two calves by transarticular fixation with a circular external fixator. The Veterinary Record 161: 193–198.
Roe, S.C., and T. Keo. 1997. Epoxy putty for free-form external skeletal fixators. Veterinary Surgery 26 (6): 472–477.
Tyagi, S.K., H.P. Aithal, P. Kinjavdekar, Amarpal, A.M. Pawde, and J. Singh. 2014. Comparative biomechanical evaluation of acrylic- and epoxy- pin external skeletal fixation systems with two- and three- point fixation per segment under compressive loading. Advances in Animal and Veterinary Sciences 2: 212–217.
Tyagi, S.K., H.P. Aithal, P. Kinjavdekar, Amarpal, A.M. Pawde, and I.P. Sarode. 2014. Physical characters and economics of acrylic and epoxy polymers as frame components of external skeletal fixator. The Indian Journal of Animal Sciences 84: 1261–1264.
Tyagi, S.K., H.P. Aithal, P. Kinjavdekar, Amarpal, A.M. Pawde, T. Srivastava, K.P. Tyagi, and S.W. Monsang. 2014. Comparative evaluation of in vitro mechanical properties of different designs of epoxy-pin external skeletal fixation systems. Veterinary Surgery 43: 355–360.
Tyagi, S.K., H.P. Aithal, P. Kinjavdekar, Amarpal, A.M. Pawde, T. Srivastava, J. Singh, and D.N. Madhu. 2015. In vitro biomechanical testing of different configurations of acrylic external skeletal fixator constructs. Veterinary and Comparative Orthopaedics and Traumatology 28: 227–233.
Willer, R.L., E.L. Egger, and M.B. Histand. 1991. Comparison of stainless steel versus acrylic for the connecting bar of external fixators. Journal of the American Animal Hospital Association 27: 541–548.
Aithal, H.P., P. Kinjavdekar, Amarpal, A.M. Pawde, Rohit Kumar, Rekha Pathak, P. Kumar, S.K. Tyagi, P. Dubey, and D.N. Madhu. 2019. Treatment of open bone fractures using epoxy-pin fixation in small ruminants: a review of 26 cases. Rum Science 8: 103–114.
Aithal, H.P., P. Kinjavdekar, Amarpal, A.M. Pawde, M.M.S. Zama, Prasoon Dubey, Rohit Kumar, S.K. Tyagi, and D.N. Madhu. 2019. Epoxy-pin external skeletal fixation for management of open bone fractures in calves and foals: a review of 32 cases. Veterinary and Comparative Orthopaedics and Traumatology 32: 257–268.
Bennet, R.A., and A.B. Kuzma. 1992. Fracture management in birds. Journal of Zoo and Wildlife Medicine 22: 5–38.
Kumar, P., H.P. Aithal, P. Kinjavdekar, Amarpal, A.M. Pawde, K. Pratap, Surbhi, and D.K. Sinha. 2012. Epoxy-pin external skeletal fixation for treatment of open fractures or dislocations in 36 dogs. Indian Journal of Veterinary Surgery 33: 128–132.
Tyagi, S.K., H.P. Aithal, P. Kinjavdekar, Amarpal, A.M. Pawde, and Abhishek Kumar Saxena. 2021. Acrylic and epoxy-pin external skeletal fixation systems for fracture management in dogs. Indian Journal of Animal Research. https://doi.org/10.18805/IJAR.B-4265.
Author information
Authors and Affiliations
Chapter 2: Sample Questions
Chapter 2: Sample Questions
Q. No. 1: Mark the most appropriate answer.
-
1.
Intramedullary pinning is most resistant against
(a) bending, (b) rotation, (c) tension, (d) torsion
-
2.
Bone plating should be done at the following surface of a long bone.
(a) compression side (b) tension side (c) lateral side (d) medial side
-
3.
Technique of fracture fixation wherein multiple percutaneous, transcortical pins are passed in the proximal and distal bone segment and are connected to a rigid external frame is known as
(a) external fixation (b) internal fixation (c) external skeletal fixation (d) none of the above
-
4.
Which of the following is not true with respect to an ESF?
(a) strength increases as complexity of design increases (b) increasing the number of pins increases fixator strength (c) the larger the pin diameter, the greater is the fixation stability (d) the more the distance from the bone to side bars increases, the more the fixation stiffness
-
5.
Avulsion fracture of the olecranon can be better treated by
(a) screw fixation (b) IM pinning (c) tension band wiring (d) cross pinning
-
6.
Transfixation pinning and casting are a type of
(a) external fixation (b) internal fixation (c) external skeletal fixation (d) none of these
-
7.
The technique of choice for the fixation of a supracondylar femoral fracture is
(a) retrograde technique of single pinning, (b) stack pinning, (c) cross intramedullary pinning, (d) K-nailing
Q. No. 2: State true or false.
-
1.
A plaster cast applied straight can neutralize bending and rotational forces but generally unable to resist compressive, shear, and tensile forces.
-
2.
Creating an opening (window) in the cast will reduce its strength considerably and make the window site prone for breakage.
-
3.
Modified Thomas splint is indicated in proximal femoral and humeral fractures.
-
4.
IM nailing in a long bone fracture is contraindicated if periosteal system is already damaged.
-
5.
In fractures with smaller bone segment, retrograde pinning is preferred due to accurate placement and better purchase of pin.
-
6.
K-nails are not indicated if there are longitudinal cortical cracks in the fractured bone.
-
7.
Plaster cast can be used for effective immobilization of fractures at the distal end of the femur.
-
8.
Close pinning can only be used for recent stable fractures.
-
9.
Internal fixation should be avoided in the presence of infection.
-
10.
Periosteal stripping is preferred during plate fixation.
-
11.
Cross IM pinning using small diameter pins can provide stable fixation of small fracture segments near the joint with minimal damage to the growth plate.
-
12.
Interlocking nail is biomechanically superior to bone plate.
-
13.
Limited contact DCPs with undercut can reduce the contact between the plate and the bone surface and in turn reduce the stress protection and vascular compromise.
-
14.
Fully threaded cortical screw can be used as ‘lag screw’ by over-drilling the far cortex to achieve interfragmentary compression.
-
15.
Positive-profile threaded pins are stronger than negative-profile threaded pins of similar size.
-
16.
During ESF application, pins are introduced using high-speed, low torque power drills to avoid wobbling and reduce thermal necrosis of the bone.
-
17.
A properly tensioned 1.6 mm K-wire provides stiffness equivalent to a 4 mm fixator pin.
Q. No. 3: Fill in the blanks.
-
1.
________________________ sling is used to hold the shoulder joint in flexion, while ________________________ sling is indicated to hold the hip joint in flexed position.
-
2.
Introduction of the pin for IM pinning through one end of the bone is called as _________________________ technique, and when it is introduced through the fracture site, it is termed as ________________________ technique.
-
3.
The diameter of the intramedullary pin should be about ______________________ of medullary cavity diameter, to achieve adequate stability.
-
4.
Interlocking nailing with fixation of either proximal or distal transfixation bolts is called as _____________________________, whereas fixation of both proximal and distal bolts is termed as ______________________________.
-
5.
____________________________________ plates with threaded screw holes typically have combi holes to allow placement of either __________________________ or ____________________________ screws.
-
6.
Minimally invasive plate osteosynthesis is _______________ (less/more) traumatic, ___________________ (less/more) biological, and __________ (less/more) rigid than standard plate fixation.
-
7.
An orthopedic wire placed around the circumference of the bone is called as _________________________________, and a wire passed through a hole drilled in the bone to partially encircle the bone is ______________________________.
-
8.
The methods used to reduce thermal necrosis of tissues during ESF application include __________________________, _______________________________, and ____________________________________.
-
9.
Free-form fixation has the advantage of ________________________________________________________, but the disadvantage is _________________________________________.
Q. No. 4: Write short note on the following.
-
1.
Principles of locking compression plate
-
2.
Advantages of interlocking nailing
-
3.
Minimally invasive plate osteosynthesis
-
4.
Principles of external skeletal fixation
-
5.
Plaster cast vs. fiberglass cast
-
6.
Rush pinning vs. cross IM pinning
-
7.
Dynamic self-compression plate vs. locking plate
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Aithal, H.P., Pal, A., Kinjavdekar, P., Pawde, A.M. (2023). Principles of Fracture Fixation Techniques. In: Textbook of Veterinary Orthopaedic Surgery. Springer, Singapore. https://doi.org/10.1007/978-981-99-2575-9_2
Download citation
DOI: https://doi.org/10.1007/978-981-99-2575-9_2
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-99-2574-2
Online ISBN: 978-981-99-2575-9
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)