Abstract
Multi-criteria decision making (MCR) has a rich history, employed since the early 1950s to mathematically model decision problems and identify optimal solutions from a set of alternatives. Recently, MCR has found applications in biomedical engineering and healthcare big data. The healthcare domain, characterized by a multi-stakeholder perspective involving patients, doctors, medical device manufacturers, and insurers, presents complex decision-making challenges. With diverse criteria and extensive healthcare records, it becomes challenging to make fair decisions. This paper outlines the requirements for a fair decision-making algorithm, highlighting the limitations of MCR in meeting fairness criteria. An algorithmic framework incorporating fairness criteria is presented, employing a similarity-based approach for decision-making on Electronic Health Records (EHR) to predict prospective cohort groups for a target patient.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
- Multi-criteria decision making
- biomedical engineering
- healthcare big data
- patient-centric healthcare
- fairness requirements
- fair algorithm for co-hort prediction
1 Introduction
Multi-criteria decision making (MCR) [1], also called Multi-criteria decision analysis (MCDA), is a structured method for evaluating options with conflicting criteria and selecting the best solution. Early research across various domains, including Economics, Mathematical Systems, and government policy formulation, has contributed to a rich set of methods for analysis and decision making.
The MCR problem involves alternatives, criteria, and normalized weights. Below are a few examples.
Example 1
-
1.
An individual wants to buy a car from a finite set of car models. Some criteria include price, fuel type, efficiency, safety, reliability, and size. The decision criteria are of heterogeneous types, and the respective weights assigned are 5, 3, 5, 5, 5, 4.
-
2.
A company may want to evaluate different investment opportunities. Criteria include return on investment, risk level, liquidity, and market potential for profit. The respective weights for these criteria may be 5, 3, 4, 7.
-
3.
After surgery, a patient wants to move to a senior residence. Criteria include transportation, personal care support, medication management, nursing support, social support, and technology safety. The respective weights assigned to the criteria are 4, 5, 6, 5, 4, 5.
These examples vary in complexity, requiring individual decisions to collective decisions with conflicting goals. MCR problem solving in patient-centric healthcare is more challenging, requiring fairness to both the patient and service-providing group. Recent papers [1,2,3] highlight challenges in selecting fair criteria and assigning weights in biomedical engineering and healthcare decision making. In this paper, we propose a fair algorithm to address these challenges. The paper is organized as follows. Section 2 provides a brief concise review of recent papers in MCR applied to healthcare. Section 3 explains the patient-centered health model, its emerging importance, and highlights the inadequacy of MCR in current healthcare applications. Section 4 lists fairness characteristics needed for decision-making algorithms in patient-centered care, comparing MCR with our developed algorithm and demonstrating MCR’s failure in meeting fairness criteria. Section 5 presents a skeleton of fair algorithms and semantic scoring functions used to compute similarity measures. Section 6 concludes the paper by listing problems solved using our fair algorithm and others currently under investigation.
2 A Brief Review of MCR Applied in Healthcare Domain
After reviewing the most recent publications that address the use of MCR in health- care domain, we have classified them into the following four categories.
General Survey: Papers in this category provide a broad survey of published works on MCR concepts and methods, and which of them are most commonly used for evaluation of new medicines, healthcare services, and treatment options in healthcare.
Safety-critical Aspects: Papers that focus on specific problems in healthcare domain where safety criterion is paramount. Example problems include the selection of medical devices and procedures, and deciding the best healthcare infrastructure location.
Treatment Options: Papers in this category discuss the MCR methods currently used to determine treatment options, and self-evaluate the adequacy of these methods.
Weight and Criteria Selection: Papers in this category discuss the important issue of criteria selection and weight assignment in problems that involve many stakeholders, and they in turn have very specific interests and concerns on health technology assessment should be done.
Category I: The paper [4] presents extensive statistics on the popularity of MCR methods across various subject areas. The engineering domain has the highest number of MCR-based publications, while agricultural and biological sciences have the fewest. Surprisingly, the healthcare domain is absent from the “Subject Areas.” The paper lists 20 different MCR methods, and among them, AHP, DEA, TOPSIS, FUZZY AHP, ELECTRE, PROMETHEE, VIKOR, and FUZZY TOPSIS are identified as the most commonly used MACDM methods in healthcare assessments. Comparisons of five methods (TOPSIS, VIKOR, PROMETHEE, MULTIMOORA, and COPRAS) on an environmental problem in a hydropower plant in Latvia lead to conclusions about their differing results and priority selections.
Category II: Four papers address the MCR approach in healthcare safety-critical scenarios. In [5], the first problem involves selecting the “infrastructure location” for health- care facilities, senior homes, and long-term therapy, integrating Analytical Hierarchy Process (AHP) and Evidential Reasoning (ER). Criteria include safety, size, total cost, accessibility, design, risks, and population profile. Decision-making for medical device manufacturers is explored in [6]. The approach, lacking an explanation for the choice of the geometric mean, determines weights through a geometric mean formula on expert weight vectors. In [7], the MCR framework selects sustainable suppliers in the health- care industry using AHP in the MARCOS method, comparing it with AHP, VIKOR, and ELECTRE.
Category III: MCR methods are increasingly applied to determine the best treatment for diseases from a set of alternatives [3, 8]. In [3], fuzzy MCR methods are proposed for cancer treatment options, including brain cancer, skin cancer, and prostate cancer, using fuzzy PROMETHEE and VIKOR methods. Challenges include the necessity of fuzzy methods, the difficulty of choosing weights even with expert input, and the need for interdisciplinary expert compromise. In [8] 72 papers on MCR methods in COVID- 19 analysis are surveyed. It reveals concerns about combining fuzzy sets with MCR, computational complexities, and result validation challenges.
Category IV: The central issue in MCR modeling is on selection of criteria and weights, and it requires humans (experts in groups). The 3-tier model [9] is a good model to start with. However its usefulness depends on (1) the number of criteria and analysis on “how complete” this list is, and (2) determining whether all attributes for each criteria have been identified to its “atomic level”. Depending on these two and the choice of weights “MCR models” differ. The paper [1] explain a group-based experimental activity for choosing the criteria and for quantifying the weights. However, they do not provide a procedure for experts in a group activity in selecting, agreeing, and quantifying the criteria and weights.
In summary, existing multi-criteria decision making methods in the field of health- care has raised many open problems. In Sect. 3 we introduce the importance of patient-centered healthcare, explain is multi-dimensional perspective by identifying the stakeholder, criteria for delivering healthcare services, and how the weights should be determined at attribute level for each criteria.
3 Shared Decision Making - Patient-Centered Healthcare
In this section we explore Patient-centered healthcare (PCH) paradigm, an active area of current research and practice [10,11,12,13,14,15], to emphasize “multi-criteria decision making” is central to the success of patient care. We review the current work on it, and propose our new model and analysis approach to solving criteria-based shared decision making.
According to the paper [11], PCH paradigm was introduced in 1988. It defined it as follows:
PCH is “care that is respectful of and responsive to individual patient preferences, needs, and values” and that ensures “that patient values guide all clinical decisions”.
This paper also emphasizes that “for some decisions there is clearly only one path, and patient preferences play little or no role”. Patient-doctor relationship should be “trust- worthy” to make patients aware where choices exist and where there is only one path. In situations where many options are available, PCH considers patient’s stand point, context, and input during the entire spectrum of decision making process [10]. It not only encourages but requires the enhancement of patient’s awareness on the treatment choices, collaborative and shared decision making between patients, families, care- givers, and healthcare providers. That is, it goes beyond just physical well-being to include emotional, social, ethical, and financial aspects during the different contexts of treatment selection and treatment delivery. Patients are given full control over sharing their clinical and treatment data with the level of privacy they choose, and in particular to bring in their choice of support group to share that information. Clinical support is set at the level of fully informing patients on their status, making them knowledgeable to understand the consequences of different options, and leaving the final decision to the patient or patient’s delegated authority. Based on the National Research Council report Crossing the quality Chasm (referred in [11], PCH rests on 8 principles listed below. 1. Respect for patient’s values, preferences, and expressed needs, 2. Coordination and integration of care, 3. Improved patient awareness, communication, and knowledge, 4. Emotional support, 5. Enhancing comfort levels (at senior homes, ICU, Long term Re- habilitation), 6. Involvement of Social Support Groups, 7. Continuation of care (Post surgery/treatment), 8. Improved Access to Service.
So, PCH models are expected to include entities who fulfill these principles and include “trustworthiness” factors that include the four components safety, security, re- liability, and availability. Although survey papers [12, 15] mention trusted relationship must be part of PCH model, no model exists to include all of the above it in the current PPC model [13]. A sufficiently complete model is necessary to suggest the services, and constraints provided by the entities in the model fulfill the 8 principles and trustworthi- ness. From such a model we can identify the criteria for shared decisions and evaluate them in determining the best service option. With this goal in mind, in Sect. 3.1 we propose a new PCH model.
3.1 Proposed PCH Model
We need a patient-centered healthcare model in which the health determinants comprehensively and collectively cover the 8 principles stated earlier. We propose such a model in Fig. 1. This model is a rich refinement of the health model proposed in [16] for mHealth (Mobile Health). We explain below the significant elements of healthcare determinants within each ring, and motive how well it covers the 8 PCC principles stated earlier.
In Fig. 1, a ring model with six layers represents various health determinants. Beginning with the innermost “Patient” layer, subsequent layers detail physical and emotional status, health goals, cultural aspects, preferences, and socioeconomic factors [16]. Expanding further, layers include social networks, family & friends, health-care facilities, environmental conditions, and infrastructure support [16]. Each layer encompasses specific determinants, such as “Health Care” for healthcare providers, with patient-defined data sharing policies. The model provides a high-level conceptual view, while detailed models, illustrated in Fig. 2 for the “Patient” [16] and Fig. 3 for a “Health Care Facility,” can be developed for each determinant, offering a comprehensive representation of the healthcare ecosystem [16].
3.2 Coverage and Comparison
The only paper that gives a conceptual PCH model is [13]. Their model is given in Fig. 2 (Page 21) of this paper. This model has essentially three levels. At the top, “Provider Characteristics” is associated with “Hospital” and “Physician, Nurse”. At the next level “Patient Centered Care” is associated with “Patient” and “Cost”. At the lowest level, the box includes “Health related quality of life/Functional status/Psychological wellbeing”. They have not given any explanation on how this diagram reflects PCC principles. In our opinion. It does not reflect any of the 8 stated principles.
As opposed to this we justify below how our conceptual model, along with a family of models for the determinants in it, add clarity and comprehensively fulfills the 8 principles of PCH.
-
1.
Principle-1: “Respect for patient’s values, preferences, and expressed needs” - Fulfilled in ring 1, ring 2 and ring 3.
-
2.
Principle-2:“Coordination and integration of care” - Fulfilled by Family & Friends (ring 4), Healthcare Facilities (ring 3), and Social Network (ring 4).
-
3.
Principle-3: “Improve patient awareness, communication, and knowledge” - Fulfilled by Healthcare (ring 3), Social Network (ring 4), Infrastructure (ring 5), Socioeconomic (ring 3).
-
4.
Principle-4: “Emotional support” - Fulfilled by Emotional Health (ring 2), Cultural, Socioeconomic (ring 3), Family, Social Network (ring 4), Infrastructure, Entertainment (ring 5)
-
5.
Principle-5: “Enhancing comfort levels” - Fulfilled by Preferences (ring 3), Health-care Facilities (ring 4), all determinants (ring 5)
-
6.
Principle-6: “Involvement Social Support Groups”-Fulfilled by all determinants (ring 4)
-
7.
Principle-7: “Continuation of care (Post surgery/treatment)” - Fulfilled by Infrastructure, Environmental Conditions (ring 5), Healthcare Facilities (ring 3: Senior Home included)
-
8.
Principle-8: “Improved Access to Service” - Fulfilled by Infrastructure (ring 5), Healthcare Facilities (ring 3)
In addition to the coverage of PCC principles, we motivate below how “models of interactions” between determinants can be developed and how such models are formal enough to guide us identify the criteria and suggest mathematically sound methods for estimating weights for preferences.
3.3 Criteria, Preferences, and Decision Quality Measurement
All reviewed papers in Sect. 2 emphasize the necessity of a collaborative approach that values and respects patients’ needs and wishes for identifying criteria and weights. However, a systematic method for this purpose is lacking, and existing approaches are primarily manual, lacking standardization for decision quality assessment. The importance of measuring decision quality is discussed in [14]. While a list of evaluation measures is available on the Ottawa Hospital Research Institute website [17], many published papers do not follow it for assessing decision quality outcomes. Moreover, the available tools focus on patient evaluation, neglecting other stakeholder in Patient- Centered Healthcare (PCH).
The Delphi method [18,19,20], known for its standardized steps in collaborative decision- making, offers a potential means to enhance decision quality assessment in PCH. An innovative approach could involve adapting the evaluation list [17] for other stakeholders and combining it with the Delphi method. However, this method remains manual. While total automation of multi-criteria decision-making in patient-centered care is neither feasible nor desirable, we propose a methodology to serve as the foundation for an interactive, fair algorithm that engages all stakeholders in decision-making.
Decision Making Needs: Different decision-making scenarios, such as treatment options, post-treatment residence, medical device choices, and healthcare trends aware- ness, require distinct sets of decision-making criteria. For our discussion, we consider medical devices and senior homes as examples.
The eight principles stated in Sect. 3.2 lead us to consider Trust, Knowledge, Economics, Emotional Support, and Value as primary criteria for decision-making. Stake-holders must have mutual trust, and patients need trust in medical experts to share personal preferences. Economic factors include both patient and service provider capacity. Emotional support involves reliability from social groups, friends, family, and infrastructure. The specific features supporting mobility, safety, privacy, and physical activities in senior homes measure emotional support. Disagreements on Value between patients and doctors require moderation using Knowledge and Trust to reach a consensus in patient-centered care.
4 Fair Decision Making Principle
Fairness is defined in [21] from two perspectives. We base our work here on this definition, however we customize it with regard to patient-centered selection. So, we put patient’s input as “ideal” for the patient, and all other input from stakeholders as “avail- able options recommended by the experts”. We first discuss in Sect. 4.1 how the criteria and their weights are to be chosen from expert (domain) knowledge for patient- centric fairness. Next in Sect. 4.2 we explain how patients can introduce their desires in a semantically meaningful way to algorithmic construction. That is, “semantics from patient as additional input” is to be accepted by a fair algorithm. So, functions in the algorithm are intelligent due to expert knowledge and due to the integration of user semantics.
4.1 Expert Knowledge for Fair Decision Making
We propose the following steps to construct criteria at “atomic attribute level” and to determine the types of attributes that can lead to “units of measurements”. The selection problem is “medical and infrastructure devices” for patient care.
-
1.
Patient constructs the set of needs in the dimensions “Knowledge, Emotional Support”, gets expert opinions from trusted experts and with their help selects the set of medical devices (body-ware), and develops data sharing policies, and ethical/cultural needs. Patient lists the comfort requirements and gets the help of experts in dimensions “Economics, Value, Knowledge” in creating a list of infrastructure devices and medical devices.
-
2.
The patient gets a trusted expert to develop the criteria for selection at attribute level. That is, on behalf of the patient a finite set of trusted experts develop the list of criteria that satisfies the need of the patient.
-
3.
The experts collaborate in choosing the type for each criteria chosen, and assigning a “preference value” (weight consistent with the level of importance) for each attribute. The collaboration will discuss questions like the following:
-
What are the attributes necessary to describe the entity being examined?
-
Which attributes are required to evaluate a Purpose being examined?
-
Which attributes are needed for analysis?
-
Which attributes “from the examination viewpoint” are required for this analysis goal?
-
Which attributes are required to describe the examination environment?
-
Is time frame essential for this analysis issues?
-
Is there any specific geographical area specific for this analysis task?
-
Any other attributes required for analysis goal achievement?
-
-
4.
Patient shares this list with all trusted stakeholders.
-
5.
Every stakeholder will generate similar lists of their attribute choices and weights for attributes.
-
6.
This information is feeded to Algorithm P (described below) that will choose the final set of attributes (criteria) and their respective weights to be submitted to the fair Algorithm F described in Sect. 5.
Algorithm P
Let E = {E1, E2, · · · , Ek} denote the set of experts nominated by the stakeholder (patients, physicians, etc;). Because every decision must be patient centric, we let the patient assign a weight σj for expert Ej ∈ E that reflects the patient’s level of trust on the expert Ej. Let σ = σ1 + σ2 +· · · , +σk. Let CEi denote the set of criteria chosen by expert Ei, and C = Ei∈E CEi . For the sake of clarity let |C| = p. That is, there are p criteria. For each criteria ci in C a weight wi has been assigned by the expert who chose it. So, we have the set W = {wi | ci ∈ C} of weights for the criteria in set C. In the previous work [6] on medical device selection the use of “geometric mean” is suggested to calculate the weight for a criteria from the weights assigned by stakeholders. In our work we improve on this suggestion by using weighted geometric mean. That is, we use the patient-assigned trust weight σj to the expert Ej along with the expert-assigned weight wj to the criteria c of that expert’s choice in computing the weighted geometric mean in the formula below:
This weight wc is a fair weight because it satisfies the patient’s wish, and the expert’s knowledge-based input. We can prune further the set C if the number of criteria is too many by deleting those that have a low weight. This threshold has to be determined by experts. Once done, the set C and the set W = {wc | c ∈ C} are input to Algorithm F. Table 1 is an example of criteria/weight table constructed using Algorithm P for the attributes shown in the table. The number of criteria (attributes) is kept small for clarity of understanding. In principle, the set of attributes and the number of attributes are the choice of the patient and the experts.
4.2 Semantics for Patient-Centric Fairness
Patients can specify semantics for better choices in selection, introducing a “best match” concept alongside closeness to the patient’s requirements, emphasizing a “patient-centric perspective.” For attributes like “reliability, safety, and accuracy,” where higher’ implies better, and for features such as “cost and weight,” where lower’ is preferable, patient se- mantics for “lower is better” (LB) and “more is better” (MB) are integrated into scoring functions in the selection algorithm [22]. This approach allows the algorithm to prioritize options aligning with patient preferences on each attribute independently. Running the algorithm with different patient perspectives, including varied weights and attribute semantics, enables patients to consistently identify optimal choices. For instance, patients can determine the most cost-effective option among choices ensuring safety with low risk and maintenance costs [22]. In [22], ontology support is utilized to interpret the “degree of equivalence” between medical terms, enhancing the assessment of similarity between concept terms in the medical field. Semantic distance and similarity measures between sets of concepts contribute to patients’ awareness and knowledge of health- care needs, enabling informed specification of preference levels and ensuring unbiased similarity-based selection and ranking. From the algorithmic perspective a fair ranking will be “tolerant to small values”, consistent, flexible and timely. Below is a list of characteristics for an algorithmic perspective of fairness. The algorithm will produce normalized results in the interval [0, 1]. Bounded similarity measures are not produced by the widely used distance and cosine functions. The algorithm must be consistent in the sense “reversal of rank” should not happen in any environment in which the same set of inputs are used. The algorithm does not put any restriction on the number of criteria and on the number expert alternatives. For the sake of efficiency and accuracy of result, the algorithm uses only simple scoring functions (no exponential, logarithmic or fuzzy arithmetic).
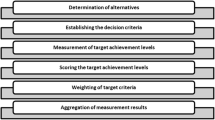
5 A Skeleton of Fair Algorithm
We assume that at every ith attribute level, there exists a sematic scoring function λi that compares two given values of the attribute and outputs a score which is a mea- sure of “best match” between the attribute values. In this paper we do not discuss their constructions, because it involves many mathematically sound details. We suggest the readers to construct their own scoring functions that satisfy the semantic criteria explained in Sect. 4.2. We also refer the reader to our recent and ongoing work [21, 22] on the rationale for the choice of scoring functions that we have constructed.
The sets C and W computed by Algorithm P are input to Algorithm F. Let A = {A1, A2, · · · , Am} denote the set of alternatives available. Assume that every Ai has all the attributes of set C (in the same order). Thus, Ais are formalized into “a vector” wherein the attributes are all in the same order, although the types of the attributes of this vector are different. This vector structure helps us to explain precisely the algorithmic steps. The patient inputs a query which consists of three parts, as shown in Table 2.
Algorithm F
The algorithm compares each component of the vector Q with the corresponding com- ponent of vector Aj. That is, it compares Qi with Aji, for i = 1, · · ·, p. It applies the scoring function λi to the pair (Qi, Aji. The value vji = λi((Qi, Aji) is a measure of “closeness”, consistent with the semantics and mode specified in the patient query structure. Next, it computes the weighted mean.
which gives the “similarity measure between the alternate Aj and the patient query Q. Having calculated the measures s1, s2, · · · , sm for all alternatives, the algorithm ranks the set of alternatives in the non-increasing order. So, the top of the ranked list is the “best match”. In case there are other considerations that may prevent this choice being adopted by the patient, the next alternative in the list can be chosen.
6 Conclusion
In our critical survey of existing multi-criteria decision-making approaches in health- care, we found a lack of specific conclusions on successful methods in the biomedical healthcare domain. The consensus among researchers is the pressing need for more efficient collaborative decision-making methods.
We examined the Patient-Centered Health (PCH) paradigm, highlighting its emerging importance, elucidating its eight fundamental principles, and identifying challenges in employing Multi-Criteria Decision Making (MCR) for shared decision-making. Subsequently, we proposed an approach based on trust, knowledge, value, economics, and social support to collaboratively select significant decision-making attributes, drawing inspiration from our previous work on semantic-centered similarity matching.
To enhance our proposed approach, deeper research is warranted, particularly in formalizing medical treatment selection problems with ontology support. Our three implementations of fair selection and ranking algorithms can be further enriched to handle complex data types of quality attributes in healthcare. Alaa Alsaig’s recent thesis introduced a user interface for gathering client requirements, and we are exploring ways to integrate healthcare ontology, making the process more interactive and iterative. This iterative loop allows stakeholders to modify their choices until a consensus is reached, with the fair algorithm serving as a vital component.
References
Schey, C., Postma, M.J., Krabbe, P.F.M., Topachevskyi, O., Volovyk, A., Connolly, M.: Assessing the preferences for criteria in multi-criteria decision analysis in treatments for rare diseases. Front. Public Health 8, 1–10 (2020)
Piniazhoko, O., Ne´meth, B.: Practical issues of determining weights for criteria to be used in an MCDA framework - based on a case study. In: ISPOR 22nd Annual International Meeting, Boston, MA, USA, p. 1 (2017)
Ozsahin, I., Ozsahin, D.U., Uzun, B., Mustapha, M.T.: Introduction - chapter 1. In: Applications of Multi-Criteria Decision-Making Theories in Healthcare and Biomedical Engineering, Elsivier - Academic Press, pp. 1–2 (2021)
Taherdoost, H., Madanchian, M.: Multi-criteria decision making (MCDM) methods and concepts. Encyclopedia 2023, 77–87 (2023)
Dehe, B., Bamford, D.: Development, test and comparison of two multiple criteria decision analysis (MACDA) models: a case of healthcare infrastructure location. Expert Syst. Appl. 2015, 1–11 (2021)
Barkaoui, H., Rejeb, H. B., Barkaoui, A., Tavares, J.M.R.: Multi-criteria decision making for medical device development. Eng. Manag. J. 35, 1–18 (2022)
Stevi´c´, Z., Pamuc˘ar, D., Pus˘ka, A., Chatterjee, P.: Sustainable supplier selection in health-care industries using a new MCDM method: measurement of alternatives and ranking according to compromise solution (MARCOS). Comput. Ind. Eng. 140, 106231 (2020)
Anvari, A.S.: The application of MCDM methods in covid-19 pandemic: a state of the art review. Appl. Soft Comput.Comput. 126, 1–40 (2022)
Angelis, A., Kanavos, P.: Multiple criteria decision analysis (MCDA) for evaluating new medicines in health technology assessment and beyond: the advance value framework. Soc Sci Medoc. Sci. Med. 188, 137–156 (2017)
Zhao, J., Gao, S., Wang, J., Liu, X., Hao, Y.: Differentiation between two healthcare concepts: person-centered and patient-centered care. Int. J. Nurs. Sci. 3, 398–402 (2016)
Barry, M.J., Edgman-Levitan, S.: Shared decision making - the pinnacle of patient-centered care. N. Engl. J. Med. 366(9), 78–781 (2012)
Constand, M.K., Macdermid, J.C., Bello-Has, V.D., Law, M.: Scoping review of patient- centered care approaches in healthcare. BMC Health Serv. Res. 14(271), 1–9 (2014)
Jayadevappa, R., Chhatre, S.: Patient centered care - a conceptual model and review of the state of the art. Open Health Serv. Policy J. 4, 15–25 (2011)
Kaltoft, M., Cunich, M., Salkeld, G., Dowie, J.: Assessing decision quality in patient- centered care requires a preference-sensitive measure. J. Health Serv. Res. Policy 19(2), 110–117 (2014)
Ogden, K., Barr, J., Greenfield, D.: Determining requirements for patient-centered care: a participatory concept making study. BMC Health Serv. Res. 17(780), 1–11 (2017)
Wan, K., Alagar, V.: Context-aware, knowledge-intensive, and patient-centric mobile health care model. In: 12th International Conference on Natural Computation, Fuzzy Systems and Knowledge Discovery (ICNC-FSKD), Zhangjiajie, China, pp. 2253–2260 (2015)
Ottawa Hospital Research Institute, Patient decision aids (2022)
Hsu, C.C., Sandford, B.A.: The delphi technique: making sense of consensus. Pract. Assess. Res. Eval. Assess. Res. Eval. 12(1), 1–10 (2007)
Okoli, C., Pawlowski, S.D.: The delphi method as a research tool: an example, design considerations and applications. Inf. Manag. 42(1), 15–29 (2004)
Strozyna, M., Elden, G., Filipiak, W.A.D., Malyszko, J., Wecel, K.: A framework for the quality-based selection and retrieval of open data - a use case from the maritime domain. Electr. Markets 28, 219–233 (2018)
Alsaig, A., Alagar, V., Mohammad, M., Alhalabi, W.: A user-centric semantic-based algorithm for ranking services: design and analysis. Serv. Oriented Comput. Appli. 11(1), 101–120 (2017)
Liu, Y.: A family of algorithms for patient similarity based on electronic health records, Master’s thesis, Concordia University, Montreal, Canada (2022). http://spectrum.library.concordia.ca
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2024 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this paper
Cite this paper
Alsaig, A., Alsaig, A., Alagar, V. (2024). A Critical Review of Multi Criteria Decision Analysis Method for Decision Making and Prediction in Big Data Healthcare Applications. In: Huang, DS., Premaratne, P., Yuan, C. (eds) Applied Intelligence. ICAI 2023. Communications in Computer and Information Science, vol 2015. Springer, Singapore. https://doi.org/10.1007/978-981-97-0827-7_8
Download citation
DOI: https://doi.org/10.1007/978-981-97-0827-7_8
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-97-0826-0
Online ISBN: 978-981-97-0827-7
eBook Packages: Computer ScienceComputer Science (R0)