Abstract
Endocrine-disrupting chemicals (EDCs) exist ubiquitously in the environment. Epidemiological data suggest that the increasing prevalence of infertility may be related to the numerous chemicals. Exposure to EDCs may have significant adverse impacts on the reproductive system including fertility, ovarian reserve, and sex steroid hormone levels. This chapter covers the common exposure ways, the origins of EDCs, and their effects on ovarian function, follicular genesis, and oocyte quality. Furthermore, we will review the origin and the physiology of ovarian development, as well as explore the mechanisms in which EDCs act on the ovary from human and animal data. And then, we will focus on the bisphenol A (BPA), which has been shown to reduce fertility and ovarian reserve, as well as disrupt steroidogenesis in animal and human models. Finally, we will discuss the future direction of prevention and solution methods.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 The Common Exposure Ways, the Origins of EDCs, and their Effects on Ovarian Function, Follicular Genesis, and Oocyte Quality
Endocrine-disrupting chemicals (EDCs) are extrinsic chemicals that can interfere with the processes regulated by endogenous hormones. EDC was defined as “an exogenous chemical or mixture of chemicals that interferes with any aspect of hormone action”[1] in 2012 by the Endocrine Society. They emphasized that very low dose EDC exposures during the developmental stage might have potent and irreversible effects. The female reproductive system is regulated by hormones which means it would be the target of EDCs. Ovary is an important assurance for fertility and performs normal functions of oocyte/follicular quality, folliculogenesis, or steroidogenesis, which is also a target constitution assaulted by EDCs. As a result, EDCs exposure may disrupt folliculogenesis, oocyte quality as well as steroidogenesis.
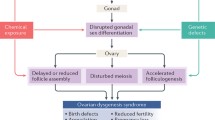
EDCs are ubiquitous in the environment, and a recent report has indicated that there are more than 800 chemicals with endocrine-disrupting properties been used in daily life [2]. People and animals tend to exposure to EDCs by various routes, such as direct contact, inhalation, ingestion, maternal-fetal transfer, or intravenous administration [3]. Generally, there are two categories of EDCs: One is naturalistic EDCs such as phytoestrogen, genistein, and coumestrol found in natural food. The other one is synthetic EDCs which can be further divided into the following groups: Dioxins, polybrominated biphenyls (PBBs), and polychlorinated biphenyls (PCBs) that are found in industrial synthetic chemicals and their by-products; Bisphenol A (BPA) and phthalate in plastics; Methoxychlor (MXC) and dichlorodiphenyltrichloroethane (DDT) in pesticides; Vinclozolin in fungicide and diethylstilbestrol (DES) in some pharmaceutical agents [4] (Fig. 3.1).
Epidemiological data have suggested that EDCs may accumulate in human body and the environment. BPA and four phthalate metabolites (mono-(2-ethylhexyl) phthalate (MEHP), monomethyl phthalate (MMP), monoisobutyl phthalate (MiBP), monoethyl phthalate (MEP)) could be detected in nearly all 1016 participants aged 70[5]. A Spanish cohort study in 2011 discovered that phthalate and phenol were commonly found in the urine of young children and pregnant women, with the urinary concentrations higher in children than in pregnant women [6]. Research in 2015 indicated that organochlorine pesticides, 13.4% of which was MXC, could be detected in follicular fluid of women from central China [7]. Besides, BPA and its derivatives can be detected in serum from second-trimester umbilical cord [8], which indicates that EDCs can be passed from mother to fetus through placenta and concentrated in fetal body. Furthermore, EDCs are difficult to be eradicated by biodegradation. For instance, MXC is persistent in soil, and its residues are present even 18 months after the soil treatment with microorganisms [9].
EDCs are prone to expose and accumulate in human body, and they can be detected in people of all ages. In addition, the existence of EDCs in follicular fluid raises a concern that EDCs may affect the reproductive system and even cause epigenetic modification of gametes. What’s more, the accumulation of EDCs in the environment is difficult to be eradicated by biodegradation, having a long-lasting impact on human health.
Researches have disclosed that EDCs adversely affect the ovary by disrupting folliculogenesis, oocyte development, and ovarian function. For instance, numerous studies have elucidated that EDCs interfered with folliculogenesis and oocyte development. Mixtures of EDCs (BPA, pesticides, phthalates, butylparaben, paracetamol, and UV-filters.) exposed to rats before puberty cause a significant reduction in primordial follicle quantities and plasma levels of prolactin [10]. Prenatal treatment of caiman latirostris with 17β-estradiol (E2), BPA, or atrazine (ATZ) can increase type III follicles, and treatment with BPA or E2 also presents higher proportioned multi-oocyte follicles [11]. Di(2-ethylhexyl) phthalate (DEHP) and MEHP can inhibit antral follicle growth via reducing estradiol production and decreasing the expression of cell cycle regulators [12]. DEHP has been proved to inhibit follicle growth and induce antral follicle atresia via dysregulation of cell cycle and apoptosis regulators [13]. Furthermore, EDCs have negative impacts on oocyte development. Female adult South African clawed toads (Xenopus laevis) that were exposed to tamoxifen (TAM) and methyldihydrotestosterone (MDHT) showed oocyte atresia in a previous study [14]. EDCs can disrupt the oocyte meiotic progression of in vitro cultured porcine oocyte cumulus complexes (OCC). BPA and 4-chloro-3-methyl phenol (CMP) exposure reduces numbers of oocytes undergoing germinal vesicle breakdown (GVBD) or reached metaphase II stage (MII) via meiotic maturation disturbance. Besides, BPA and CMP can reduce the synthesis of extracellular matrix (ECM) by altering the process of cumulus expansion [15].
Multiple studies have also consistently shown that EDCs exposure disrupted ovarian function. For example, the serum level of BPA, octylphenol (OP), and 4-nonylphenol (4-NP) is significantly elevated in precocious girls. Prepubertal exposure to EDCs including genistein, zearalenone, zeranol, and DES results in acceleration of puberty earlier onset, prolonged estrous cycle, and anovulatory period [16]. Besides, BPA and OP levels are positively correlated with the volume of the uterus and ovary [17]. Prenatal ewes exposure to mixture EDCs reduces ovarian reserve, greatly increasing the number of altered fetal ovarian genes and proteins [18]. Zama et al. [19] have suggested that transient exposure to MXC during fetal and neonatal development results in ovarian dysfunction via significant hypermethylation in the ERβ promoter regions and increase of DNMT3B. Further studies have revealed that transient exposure to MXC results in epigenetic modification in ovaries via specific signaling pathways such as IGF-1 signaling, PTEN signaling, and rapid estrogen signaling [20].
2 The Origin and the Physiology of Ovarian Development, as well as Briefly Introduce the Mechanisms in which EDCs Act on the Ovary
Ovary is a complex organ that is responsible for gametogenesis and steroidogenesis. And ovary is one of the most important target organs of endocrine disruptor chemicals. The oogonia develop from the yolk sac and then migrate to the ovary, which are proliferated by mitosis until about gestation age 28–30 weeks, and then start meiosis. The oogonia differentiate into primary oocytes, which progress into the prophase of the first meiotic division and then become dormant until puberty. The number of oocytes comes to a climax around six to seven million at gestation age 25–28 weeks, which and then starts a steady decline because of atresia. There are approximately 700,000 to two million germ cells in the neonatal period and about 300,000 to 500,000 primordial follicles at the time of puberty. For females reaching 37 years old, the numbers of primordial follicles decline to 25,000. There are about only 1000 primordial follicles reserved for peri-menopausal women (Fig. 3.2). At the period of fetus and child, the follicles hardly reach maturation. After puberty, with the stimulation of gonadotropin secreted by the pituitary gland, there is a follicle maturation every month and then about 14 days before the onset of the next menstruation cycle. In a female’s whole life, there are only 400 eggs successfully ovulated. And the rest of the follicles degenerate into atretic follicles. Follicles consist of granulosa cells surrounding an oocyte. The follicular development in a continual process of four stages, including primordial follicles, primary follicles, secondary follicles, and mature follicles, has a series of structural and physiological changes (Table 3.1).
After introducing the basic physiology of ovary, we would briefly introduce the underlying mechanisms by EDCs working on ovary as follows.
EDCs are commonly identified as compounds that can interact with androgen or estrogen receptors and thus act as antagonists or agonists of endogenous hormones. EDCs disrupt the interference with hormone by mimicking or opposing actions and the hormonal and homeostatic systems [21]. In addition, the reproductive system is vulnerable to endocrine, especially during the early stage of life. Therefore, exposure to endocrine disruptors during development may lead to disease in children or adults and even to the next generations because of epigenetic modification [21].
2.1 Oxidative Stress
Reactive oxygen species (ROS) such as hydrogen peroxide, superoxide, and hydroxyl radical are the by-products during natural oxygen metabolism, which can induce cellular damage and death and thus cause a wide range of diseases [22]. When ROS are excessively produced, or body clearance ability deficiency such as deficiency of antioxidants, oxidative stress will occur [23]. Oxidative stress is involved in ovarian toxicity caused by a variety of EDCs. It is well documented that ROS are involved in the initiation of apoptosis in follicular cells, poor quality of oocytes, and so on [23]. For instance, DEHP (10 μg/ml) has been proved to inhibit antral follicle growth by increasing ROS levels and reducing the expression and the activity of one of the critical antioxidant enzyme Cu/Zn superoxide dismutase (SOD) [1, 24]. MXC (1–100 μg/ml) can induce antral follicle atresia by decreasing the enzymatic activity and mRNA expression of antioxidant catalase Cu/Zn SOD1, glutathione peroxidase (GPX), and catalase [25]. In addition, neonatal exposure to EDCs (4-vinylcyclohexene diepoxide (VCD): 40–80 mg/kg/day, MXC: 50–100 mg/kg/day, and menadione: 7.5–15 mg/kg/day) can increase oocyte lipid peroxidation by ROS and thus induce permanent oocyte damage [26].
2.2 Disturbance of Steroidogenesis
Ovary is essential for the synthesis of steroid hormones. The “two-cell, two-gonadotropin” theory proposed by Armstrong et al. in 1979 demonstrates that granulosa cells express follicle-stimulating hormone (FSH) receptors, which stimulate aromatase activity, while theca cells possess luteinizing hormone (LH) receptors which stimulate androgen synthesis [27, 28]. During the process of ovarian steroidogenesis, LH stimulates the activation of 17α-hydroxylase to convert cholesterol and pregnenolone to androgens in the cal cells. Later the androgens diffuse to the granulosa cells and are transformed into estrogens under the catalysis of cytochrome P450 aromatase, which is stimulated by FSH [29, 30].
Researches have indicated that EDCs can inhibit ovarian steroidogenesis. For example, neonatal female caiman exposed to E2 or BPA presents higher estrogen serum levels [11]. DES, BP, and OP reduce estradiol and testosterone levels, and GEN causes a decline in testosterone levels and cAMP by stimulating the activity of aromatase enzyme [31]. DEHP inhibits the production of progesterone, androstenedione, testosterone, and estradiol from antral follicles, by inhibiting the expression of side-chain cleavage related enzymes such as 17α-hydroxylase-17,20-desmolase, 17β-hydroxysteroid dehydrogenase, and aromatase [13]. Cytochrome P450 aromatase is the critical steroidogenic enzyme that is responsible for the conversion of androgens to estrogens. EDCs disrupt steroidogenesis by interfering with the gene expression of cytochrome P450 aromatase. Varieties of EDCs have been proved to potentially disturb reproductive function by dysregulating the expression of CYP19 genes through differential transcriptional modulation [32, 33]. Zebrafishes exposed to an estrogenic mixture of 11 EDCs can be observed an alteration of CYP19A1 activity and Mtf-1 and tfap2c transcription factor [34]. Furthermore, Benzo[α] pyrene (B[α]P) alters the expression of CYP2N23. BPA changes CYP2P18, CYP2P19, and 4-OP and disturbs CYP2AD12 [35]. DES and tetrabromobisphenol A suppress CYP17 but not CYP19 activity, indicating different mechanisms of different EDCs acting on these cytochrome p450 aromatase [36].
EDCs not only can alter the enzymatic activity of cytochrome p450 aromatase, but also can interfere with the gonadotropin receptor signaling second messengers such as cAMP or modulate the Ca2+ associated metabolic pathway. For example, 1,1-Dichloro-2,2-bis(p-chlorophenyl)ethylene (DDE), a metabolite of DDT, suppresses progesterone synthesis through inhibiting the generation of gonadotropin receptor signaling second messengers cAMP [37], and also decreases the gene expression of P450 cholesterol side-chain cleavage (P450scc) [38]. Furthermore, Younglai et al. [39] have found elevations of [Ca(2+)](cyt) in granulosa-lutein cells, suggesting DDT can also modulate Ca2+-dependent pathways.
2.3 Nuclear Receptor Signaling
There are a variety of mechanisms in which EDCs exert harmful effects, one of which is attributed to the interaction with nuclear hormone receptors (NHRs). EDCs interfere with genomic and non-genomic estrogen receptor (ER) activity via directly binding with two ERs (ERα and ERβ), by the assistance of transcription factors like the aryl hydrocarbon receptor (AhR) or through modulation of critical enzymes during estrogen synthesis or metabolism [40]. Estrogenic signal networks are divided into the intracellular and the extracellular pathways. The intracellular pathways include the genomic pathway and the non-genomic pathway, involving in the transcription of target genes and signal transductions via binding with membrane receptors, respectively. The extracellular pathways involve other modulating factors such as other growth factors, cytokines, and hormones [40, 41]. Not only the estrogenic or androgenic receptors, multiple studies have indicated that activity of the constitutive androstane receptor (CAR), the pregnane X receptor (PXR), the thyroid hormone receptors (TRs), the retinoid X receptors (RXRs), the estrogen related receptors (ERRs), or the peroxisome proliferator-activated receptors (PPARs) could also be affected by EDCs, reviewed by Albane et al. [42].
Different kinds of EDCs exhibit different ER responsive properties. For example, kaempferol, coumestrol, daidzein, and genistein can mediate both ERα and ERβ ERE-mediated activities, while 2-2-bis(p-hydroxyphenyl)-1,1,1-trichloroethane, bisphenol AF, and BPA activate the ERα pathway. Besides, only a few kinds of EDCs activate the tethered mechanism through ERα or ERβ [43]. In addition, Sheikh et al. [44] have elucidated that BPA, MBP (4-Methyl-2, 4-bis (4-hydroxyphenyl) pent-1-ene), 4-tert-OP, and 4-NP exhibited high binding affinity with sex hormone-binding globulin (SHBG), indicating that these EDCs can potentially interfere or disrupt the steroid-binding function.
2.4 Epigenetic Modification
As we have mentioned above, the reproductive system is sensitive to EDCs, especially during the early critical development window, which may lead to subtle epigenetic alteration and thus cause permanent or even multigenerational or transgenerational changes [45,46,47,48]. The epigenetic modification of the germline includes histone modifications, DNA methylation, non-coding RNAs, or alterations in chromatin structure [49, 50]. For example, prenatal exposure to the environmental doses of phthalate mixture induced multigenerational and transgenerational effects on female reproduction [51]. Brehm et al. [52] have suggested that prenatal DEHP exposure (750 mg/kg/d) can alter estrous cyclicity, augment estradiol levels (F1 and F3), increase the presence of ovarian cysts (F1), decreased testosterone levels and folliculogenesis (F1, F2, and F3), reduce progesterone levels (F2), decrease inhibin B levels (F1 and F3), and change gonadotropin hormone levels (F1 and F3). We will discuss it further in the later section.
3 BPA Reduces Fertility Ability, Reduces the Primordial Follicle Pool Reserve, Leads to Premature Ovarian Failure, Disturbs the Estrous Cycle, and Disrupts Steroidogenesis in Different Animal and Human Models
In this section, we will focus on BPA, which is a plasticizer used commonly and widely in food and drink containers, plastic products, epoxy resins [53], and dental materials [54]. BPA can leach out from several products in the condition of high temperatures, acidic or alkaline environment, UV rays, or repeated use [55]. BPA can be detected in plasma, serum, sweat, urine, breast milk, placental tissue, umbilical cords, amniotic fluid, and fetal serum [56]. More importantly, BPA is considered a reproductive toxicant because it can be detected in various reproductive tissues [57]. Controversially, however, Teeguarden et al. [58] summarized methods of serum BPA measurement but they found that BPA serum concentrations in humans were unmeasurable, and contributed limited or no estrogenicity.
According to the World Health Organization (WHO) and Food and Agriculture Organization of the United Nations (FAO), the human exposure levels to BPA are estimated to be 0.4 ~ 1.4 mg/kg bw/d [59]. Although the safe reference dose of BPA proposed by the US Environmental Protection Agency is 50 mg/kg bw/d [60], previous studies have indicated that BPA has potentially negative impacts even at much lower doses in a non-monotonic dose-response manner [61,62,63].
A study has revealed that BPA can be measured in the urine of almost all the women undergoing IVF treatment, of which the concentrations are negatively associated with the ovarian response, including peak estradiol levels and the number of oocytes retrieved [64]. Besides, the plasma concentrations of BPA are transient with short half-lives (< 2 h) in pregnant women, while sustained in fetal plasma [65]. Furthermore, BPA concentrations in serum of women carrying fetuses with abnormal karyotypes in the early second trimester are higher than the control group [66], which raises concerns about the adverse impacts of BPA on human development.
Human and animal studies have illustrated that BPA exposure will reduce fertility ability by disrupting the primordial follicle pool, interfering with oogenesis, and disturbing ovary functions such as steroidogenesis and the estrous cycle. Worse still, BPA was proved to have transgenic effects that may have impacts on offspring.
Researches on infertility women have revealed that higher urinary BPA concentrations are correlated with lower antral follicle counts [67]. In animal models, scientists have obtained consistent results. In rat models, BPA exposure (2.5 and 250 mg/kg bw/d) at PND 21 can reduce the numbers of primordial, primary, preantral, and total healthy follicle numbers [55]. Atretic follicles, cysts formation, and separation of granulosa cells can be observed in rats’ ovaries after exposure to BPA orally for 4 weeks [68]. Perinatal exposure to BPA by the oral route during gestation and breastfeeding can decrease recruitment of primordial follicles, increase the number of corpora lutea, and ovulate oocytes in rats ovaries [69]. Neonatal rats subcutaneous exposed to BPA (1 mg/kg) exhibits multiple cystic follicles and decreased area of corpora lutea (CL) in the ovary [70]. In mice models, BPA can facilitate the transition from primordial to primary follicles, accelerate the dissipation of the primordial follicle pool, and inhibit meiosis I by abnormal spindle assembly [71]. BPA (10 or 100 μM) exposure to neonatal mice isolated ovaries significantly reduces germ nest breakdown and primordial follicle assembly [72]. Besides, BPA (30 M) exposure to in vitro mice oocytes during follicular development shows the reduction of granulosa cell proliferation and total estrogen production, but it still can develop and form antral-like cavities [73]. In lambs models, prenatal low dose BPA (50 μg/kg/day) exposure affects the ovarian follicular dynamics by reducing primordial follicle pool reserve and stimulating follicular recruitment and development [74]. Veiga-Lopez et al. [75] have also proved that prenatal BPA treatment causes ovarian follicular dynamics disruption on sheep. BPA exposure can shorten the time interval between the estradiol rise and the preovulatory LH surge, and disturb follicular count trajectories. Besides, BPA early exposure results in the augmentation of the number of multi-oocyte follicles (MOFs), granulosa/theca cells in antral follicles as well as antral atretic follicles, because folliculogenesis acceleration increases the incidence of atretic follicles [74]. What’s more, Gieske et al. [76] have also suggested that prenatal and postnatal exposure to BPA results in increased formation of MOFs and antral follicles in the primate model. One of the underlying mechanisms is that BPA disrupts the follicular progression. BPA induces follicular atresia via disrupting the follicular progress by interfering with the previtellogenic and vitellogenic phases. BPA exposure may stimulate follicular recruitment of the primary follicular recruitment on the primary stage and then forces the follicular transition from stage III to IV with enlarged stage IV follicles, thereby inducing atresia [77]. What’s more, BPA affects follicle numbers and constituent via interfering with the follicle development-related genes such as down-regulation of the expression of oocyte-specific histone H1 variant (H1FOO) and factor in the germline alpha (FIGLA) genes, and up-regulation of anti-Mullerian hormone (AMH) genes expression [78]. In addition, BPA may impair folliculogenesis by increasing the expression of oocytes specific genes such as Sohlh2 (spermatogenesis and oogenesis helix-loop-helix), Nobox (newborn ovary homeobox), Lhx8 (LIM homeobox 8), and FIGLA. BPA disturbs the normal process of folliculogenesis by blocking the demethylation of CpG sites of the Lhx8 gene in oocytes [72]. Furthermore, postnatal exposure to BPA can dose-dependently disturb the early ovary development by disrupting the Notch signaling pathway [79].
BPA orally exposure to young adult mice (50 μg/kg bw/day) has been shown to reduce the fertilization ability of oocytes rather than affect ovulation [80]. Acute low doses exposure of BPA (3, 5 mg/L) to zebrafish can disrupt oogenesis, displaying severe deterioration of ovarian tissue with distorted and immature oocytes, and the increased number of atretic oocytes [81]. Persistent unenclosed oocytes in the medullary region and small non-growing oocytes in secondary and antral follicles have been presented in rhesus monkeys when continuously exposed to BPA before birth [82]. Consistently, BPA exposure to human oocytes shows decreased oocyte survival, increased oocyte degeneration, and increased MLH1 (crossover marker) foci number, which indicates BPA can act as a toxic substance and affect meiotic prophase such as pairing-synapsis and recombination processes, as well as decrease oocyte survival [83]. Numerous previous studies have attempted to explain the underlying mechanisms of the impacts of BPA on oocyte development. Researches have suggested there is lipid droplet accumulation, chromatin condensation in the nuclei of granulosa cells, and autophagosomes in rats’ ovaries at 4 weeks post-exposure to BPA [68]. Exposure to BPA during early gestation age may have adverse impacts on meiosis, thus disrupts the development of the oocytes. For example, low dose BPA exposures during mid-gestation lead to oocytes displaying gross aberrations in the meiotic prophase, including enhanced levels of recombination and synaptic defects, and an increase in aneuploid eggs and embryos in rats [84]. In isolated mice ovaries model, BPA exposure (30 M) has adverse effects on the meiotic spindle, thereby hindering meiosis progression [73]. Besides, BPA exposures to rhesus monkeys during middle and gestational age can induce chromosome segregation disturbances and MOFs increase, respectively [82]. Also, BPA has been proven to have genotoxic and cytogenetic, but not mutagenic effects. BPA can interfere with the gene expressions related to meiosis. Prenatal exposure to low dose BPA may have impacts on early oogenesis by disturbing the gene expression, especially that correlated with the onset of meiosis [85]. BPA exposure to mice results in more oocytes in germ cell cyst and less primordial follicle counts through inhibiting the meiotic progression of oocytes, via down-regulated mRNA expression of specific meiotic genes, including Dmc1, Stra8, Scp3, and Rec8 [86]. BPA exposure to in vitro embryonic stem (ES) cells significantly upregulates the expression of the meiotic entry gene Stra8, accompanied by aggregated Sycp3 signal localized in nuclei and up-regulation of ovarian markers (Foxl2 and Wnt4), which can help to explain how BPA affects germ cell differentiation [87]. Furthermore, BPA can deteriorate egg quality through decreasing HDAC7 expression in mice ovary and eggs, while increasing H3K9 and H4K16 acetylation [88]. Besides, BPA exposure to ovaries induces a significant elevation in micronucleus frequency, and conventional chromosome aberrations such as breaks, gaps, and fragments increased [89]. Furthermore, BPA exposure leads to chromosome synapsis impairment and disturbance of meiotic double-strand break repair (DSBR) progression, which is essential to genomic integrity maintenance during meiosis [90]. Oocytes exposed to BPA show a significant increment of Rpa, Spo11, H2ax, and Blm genes involved in DSB generation, signaling, and repair, as well as up-regulation of Erα, Erβ, and Errγ genes related to estrogen receptor [91]. Ganesan et al. [92] have demonstrated that BPA can induce ovarian DNA damage, with significant increased DNA DSB marker cH2AX and ATM before follicle loss. Besides, they have observed ovary that may activate DNA repairment and xenobiotic biotransformation to protect oocyte from damage, or activate cell death signaling to deplete follicles.
Previous researches have indicated that BPA adversely affects ovarian functions, including disturbing estrous cycle and steroidogenesis. Neonatal period exposure to BPA causes advanced puberty onset [70] and irregular estrous cycle [70]. Prepubertal exposure to BPA in mice will present advanced puberty onset [93, 94], ovary weight reduction [78, 93, 74], disturb estrous cycle and duration [93, 94], lower E2 response during in vitro fertilization (IVF) [95], and diminish ovarian reserve [96]. Exposure to BPA during the implantation period may have potential effects on adverse pregnancy outcomes and reduction of litter size or implantation rate [97].
In vitro experiments in isolated porcine granulosa cells have illustrated that BPA exposure can disturb steroidogenesis with the progesterone level decreased [98]. However, BPA exhibits non-monotonic dose effects on ovarian steroidogenesis, which may be attributed to different alteration properties of steroidogenic enzymes. For instance, steroidogenic gene expressions are promoted by BPA at lower concentrations (5 and 15 μg/L) while inhibited at higher concentrations (50 μg/L) [99]. The basal progesterone level elevates when BPA is at 10−8 M to 10−5 M, and FSH-stimulated progesterone level is promoted when BPA is at 10−7 M and 10−6 M. In comparison, BPA at 10−4 M inhibits the basal and gonadotropin-stimulated progesterone production [100]. Besides, BPA increases progesterone levels and elevates mRNA expression of steroidogenic acute regulatory protein (StAR) and P450scc at 10−7 to 10−5 M. In contrast, progesterone levels and P450scc expression are decreased, and StAR expression is increased at 10−4 M. BPA exposure at the concentrations of 10−6 to 10−4 M inhibits estradiol levels and P450 aromatase expression in a dose-dependent manner [101]. BPA exposure (10−7 to 10−4 M) shows enhancive testosterone synthesis, augmentation of mRNA expression of cholesterol side-chain cleavage enzyme (P450scc), 17- hydroxylase (P450c17), and StAR in rat ovarian theca-interstitial cells. BPA (20 mg/ml) disturbs progesterone and estradiol synthesis via down-regulated gene expression of 3b-hydroxysteroid dehydrogenase (3b-HSD), cytochrome P450 side-chain cleavage (CYP11A1) and CYP19A1 related to encode steroidogenesis enzymes [102]. In the studies of isolated human luteinized granulosa cells, BPA exposure (10, 100 μg/mL) lessens the expression of steroidogenic enzyme Cyp11A1 and StAR in mice antral follicles in vitro, causing a reduction of steroidogenesis including progesterone, androstenedione, testosterone, and estradiol. However, these effects can be reversed by the removal of BPA in acute exposure [103]. Perinatal rats exposed to BPA (0.5, 50 μg/kg day) exhibit higher levels of mRNA expression of 3β-hydroxysteroid dehydrogenase and serum progesterone, and lower levels of androgen receptor (AR) [69]. Banerjee et al. have elucidated that catalase mediated reproductive damage to granulosa cells in rats after BPA exposure. BPA exposure results in the elevation of nitric oxide, lipid peroxidation, pro-inflammatory cytokine, serum FSH and LH levels, as well as reduction of the catalase expression and estrogen or progesterone levels, of which the effects can be augmented by pretreatment with catalase blocker [104]. Zhang et al. have also revealed that BPA action may involve epigenetic regulation, as well as ER and AR signaling, nuclear receptor subfamily 5, group A, number 1 (Nr5a1) pathway [99].
We have reviewed that BPA exposure has effects on follicular formation, oocyte development, and steroidogenesis based on human and animal studies. Various studies have also observed that BPA has transgenerational effects on steroidogenesis and folliculogenesis. In utero low doses of BPA exposure will affect early ovarian development and reduce the fecundity of females in the subsequent generations.
BPA exposure (20 μg/L) to zebrafish can diminish female adult fertility up to F2 [105]. A further study [106] has shown that in utero BPA exposure not only affects F1 but also reduces fecundity on the subsequent three generations. Wang et al. [107] have indicated that F1 female mice exposed to low doses of BPA exhibit various fertility problems, significantly increased dead pups and estrus cycle disturbance. In vivo [107] and in vitro [108] studies have reached a consistent result that BPA exposure may inhibit germ cell nest breakdown via altering the expression of critical ovarian apoptotic genes, such as decreasing expression of pro-apoptotic factors and increasing expression of anti-apoptotic factors. Shi et al. [94] also have found transgenerational effects of BPA on the earlier onset of puberty, estrous cyclicity disturbance, fertility problem, serum testosterone elevation, and primary and secondary follicle counts reduction. Early BPA exposure to F1 might reduce the relative ovary weight in F2. However, they did not observe that BPA exposure affected germ cell nest breakdown, primordial, primary, or secondary follicles in F3 ovaries on PND 4, whereas exposure to BP tended to increase germ cells in nests. Likewise, Berger et al. [109] have shown no transgenerational effects on germ cell nest breakdown and gene expression on PND 4. Collectively, these data have suggested that BPA directly targets the ovary to inhibit germ cell nest breakdown in the F1 generation, but not the subsequent generations.
One of the reasons to explain BPA exposure affecting female germ cells is that BPA may change the gene expression pattern. Liu et al. [110] have elucidated that BPA exposure to zebrafish can result in the global DNA demethylation in the ovary via altering transcripts of DNA methylation/demethylation-associated genes: glycine N-methyltransferase (GNMT), DNA methyltransferase (DNMTs), and ten-eleven translocation. The global DNA methylation level is significantly elevated in the ovary, which can be affected by DNMTs expression alteration [111]. BPA exposure can affect the DNA methylation of imprinting genes by decreasing gene expressions of Igf2r, Peg3, and H19, and curtailing mRNA expressions of specific meiotic genes, as well as increasing Nobox mRNA expression in fetal mouse germ cells [112]. Chao et al. [71] have illustrated that BPA exposure to CD-1 mice results in reduced imprinting gene expressions of Igf2r and Peg3 via the ER signaling pathway during oogenesis. A study conducted on zebrafish has demonstrated that exposure to 5 μg/L BPA may promote apoptosis in mature follicles and downregulate oocyte maturation-promoting signals, probably via alterations in the chromatin structure mediated by histone modifications [113]. Collectively, these data have indicated that the detrimental impacts of BPA on the female reproductive system may be due to the deregulation of epigenetic mechanisms.
In addition to the transgenic effects on germ cell development, BPA can also affect the sex hormone production on subsequent generations. In utero, BPA exposure will reduce cytochrome P450 aromatase mRNA levels, estradiol levels, and preantral follicle numbers in the F1 generation. On the other hand, it may decrease testosterone levels and alter mRNA expression of cytochrome P450 cholesterol side-chain cleavage, cytochrome P450 aromatase, 3β-hydroxysteroid dehydrogenase 1, and steroidogenic acute regulatory protein in the F2 generation [114]. Moustafa et al. [115] have illustrated that exposure to BPA (50 and 200 mg/kg), especially at 200 mg/kg, results in a clear marked DNA fragmentation and an increase in ER expression in the ovary, as well as serum estrogen elevation of both dam and F1 female rats. The methylation level of ovarian cytochrome P450 aromatase gene (CYP19A1A) is drastically reduced and increased, respectively, by 7- and 35-day BPA exposure. CYP19A1A mRNA expression in the ovary is reversely correlated to methylation levels of the four CpGs at the 5-flanking region [111]. These results suggest that the alteration of CYP19A1A expression can be related to the modification of DNA methylation status.
Although we have presented the human and animal data of the pernicious effects of BPA, the experiment doses of BPA are higher than the environmental doses. One study [116] has illustrated that there was no significant alteration in transcriptome and ovarian morphology in sheep ovaries when in vitro exposure to BPA at environmental doses (10–7 M and 10–8 M). Therefore, we are not sure about the exact doses of BPA which can exert its harmful effects. Further studies to prove different dose effects of BPA are needed.
4 The Future Direction of Prevention and Solution Methods
Due to the adverse health impacts caused by BPA exposure, BPA has begun to be eliminated from various consumer products or be replaced by substitutes such as bisphenol S (BPS), which is structurally similar to BPA. However, the structural similarity implicates that BPS may have analogical adverse effects. For instance, neonatal exposure to BPS (5 and 50 mg/kg) causes BPA like endocrine and structural changes in female rats [117]. Prenatal BPS exposure alters the expression of estrogen-responsive genes in both the uterus and ovary, displaying heightened responses in the uterus and diminished responses in the ovary, respectively [118]. Besides, BPS exposure can accelerate ovarian follicular development in prepubertal female mice. BPS causes significant germline apoptosis and embryonic lethality in the genetic model system Caenorhabditis elegans [119]. BPS administration in low or high doses can lead to female reproductive toxicities and oxidative stress in mice [120]. In consequence, these findings urge more researches and safe novel alternatives to BPA.
In addition to looking for new alternatives, studies also attempt to discover new therapies that can reverse the harmful effects of BPA. For example, Tualang honey has a protective effect on minimizing BPA-induced ovarian toxicity by modifying the estrous cycle and reducing numbers of atretic follicles [121]. Further study suggests that Tualang honey can change the ERα, ERβ, and C3 expressions and distribution in BPA-treated rats [122]. High doses of BPA (100 mg/kg/day) were pernicious to ovaries, and vitamins may have protective effects [123]. Vitamin C can be a potential antidote in a condition of ovarian toxification by BPA exposure [124]. 1,25-dihydroxyvitamin D3 (1,25D3) may reverse the detrimental effect of BPA by increasing mtDNA content, attenuating mtDNA deletion, inhibiting reduction in E2 secretion and COXI expression. Besides, 1,25D3 can increase mitochondrial biogenesis-related proteins by PI3K-Akt signaling and elevate cellular oxygen consumption rate and ATP production [125]. What’s more, Ficus deltoidea may protect against BPA-induced toxicity of the pituitary-ovarian axis in prepubertal female rats. It can restore normal estrous cycle, normalize FSH and progesterone levels, as well as reduce the number of atretic follicles [126].
Because humans are exposed to low doses and mixtures of various kinds of EDCs at different life stages, exploration of the exact effects of EDCs on human life turns to be complicated. This means that rather than the investigation of single-exposure, dose-response effects of pure chemical, we need new strategies to conduct a risk assessment on mixtures of daily EDCs such as the safe exposure threshold of mixtures rather than single pure compounds. Besides, EDCs are ubiquitous in the environment hence humans in different life stages from embryo, fetus, infant, child to adolescence, adulthood, and aging are vulnerable to EDCs. Therefore, researches on EDCs should not only focus on the dose effects, but also the timing effects. In conclusion, EDCs have been proven to be of significant adverse effects on human life. In order to diminish even reverse the harmful impacts of EDCs, we still need further researches.
References
Zoeller RT, Brown TR, Doan LL, Gore AC, Skakkebaek N, Soto A, Woodruff T, Vom Saal F. Endocrine-disrupting chemicals and public health protection: a statement of principles from the Endocrine Society. Endocrinology. 2012;153(9):4097–110.
Bergman Å, Heindel JJ, Jobling S, Kidd K, Zoeller TR, Organization WH. State of the science of endocrine disrupting chemicals 2012. Geneva, Switzerland: World Health Organization; 2013.
Gore AC, Crews D, Doan LL, La Merrill M, Patisaul H, Zota A. Introduction to endocrine disrupting chemicals (EDCs). A guide for public interest organizations and policy-makers. Washington, DC: Endocrine Society; 2014.
Diamanti-Kandarakis E, Bourguignon J-P, Giudice LC, Hauser R, Prins GS, Soto AM, Zoeller RT, Gore AC. Endocrine-disrupting chemicals: an Endocrine Society scientific statement. Endocr Rev. 2009;30(4):293–342.
Olsén L, Lampa E, Birkholz DA, Lind L, Lind PM. Circulating levels of bisphenol A (BPA) and phthalates in an elderly population in Sweden, based on the prospective investigation of the vasculature in Uppsala seniors (PIVUS). Ecotoxicol Environ Saf. 2012;75:242–8.
Casas L, Fernández MF, Llop S, Guxens M, Ballester F, Olea N, Irurzun MB, Rodríguez LSM, Riaño I, Tardón A. Urinary concentrations of phthalates and phenols in a population of Spanish pregnant women and children. Environ Int. 2011;37(5):858–66.
Zhu Y, Huang B, Li QX, Wang J. Organochlorine pesticides in follicular fluid of women undergoing assisted reproductive technologies from Central China. Environ Pollut. 2015;207:266–72.
Gerona RR, Woodruff TJ, Dickenson CA, Pan J, Schwartz JM, Sen S, Friesen MW, Fujimoto VY, Hunt PA. Bisphenol-A (BPA), BPA glucuronide, and BPA sulfate in midgestation umbilical cord serum in a northern and Central California population. Environ Sci Technol. 2013;47(21):12477–85.
Golovleva L, Polyakova A, Pertsova R, Finkelshtein Z. The fate of methoxychlor in soils and transformation by soil microorganisms. J Environ Sci Health Part B. 1984;19(6):523–38.
Johansson HKL, Jacobsen PR, Hass U, Svingen T, Vinggaard AM, Isling LK, Axelstad M, Christiansen S, Boberg J. Perinatal exposure to mixtures of endocrine disrupting chemicals reduces female rat follicle reserves and accelerates reproductive aging. Reprod Toxicol. 2016;61:186–94. https://doi.org/10.1016/j.reprotox.2016.03.045.
Stoker C, Beldoménico PM, Bosquiazzo VL, Zayas MA, Rey F, Rodríguez H, Muñoz-de-Toro M, Luque EH. Developmental exposure to endocrine disruptor chemicals alters follicular dynamics and steroid levels in Caiman latirostris. Gen Comp Endocrinol. 2008;156(3):603–12. https://doi.org/10.1016/j.ygcen.2008.02.011.
Gupta RK, Singh JM, Leslie TC, Meachum S, Flaws JA, Yao HHC. Di-(2-ethylhexyl) phthalate and mono-(2-ethylhexyl) phthalate inhibit growth and reduce estradiol levels of antral follicles in vitro. Toxicol Appl Pharmacol. 2010;242(2):224–30. https://doi.org/10.1016/j.taap.2009.10.011.
Hannon PR, Brannick KE, Wang W, Gupta RK, Flaws JA. Di(2-ethylhexyl) phthalate inhibits antral follicle growth, induces atresia, and inhibits steroid hormone production in cultured mouse antral follicles. Toxicol Appl Pharmacol. 2015;284(1):42–53. https://doi.org/10.1016/j.taap.2015.02.010.
Cevasco A, Urbatzka R, Bottero S, Massari A, Pedemonte F, Kloas W, Mandich A. Endocrine disrupting chemicals (EDC) with (anti)estrogenic and (anti)androgenic modes of action affecting reproductive biology of Xenopus laevis: II. Effects on gonad histomorphology. Comp Biochem Physiol Part C: Toxicol Pharmacol. 2008;147(2):241–51. https://doi.org/10.1016/j.cbpc.2007.10.001.
Mlynarčíková A, Nagyová E, Ficková M, Scsuková S. Effects of selected endocrine disruptors on meiotic maturation, cumulus expansion, synthesis of hyaluronan and progesterone by porcine oocyte–cumulus complexes. Toxicol In Vitro. 2009;23(3):371–7.
Nikaido Y, Danbara N, Tsujita-Kyutoku M, Yuri T, Uehara N, Tsubura A. Effects of Prepubertal exposure to Xenoestrogen on development of estrogen target organs in female CD-1 mice. In Vivo. 2005;19(3):487–94.
Qiao L, Zheng L-X, Cai D. Study on the levels of the bisphenol A, octylphenol, 4-nonylphenol in serum of precocious girls. J Hygiene Res. 2010;39(1):9–12.
Lea RG, Amezaga MR, Loup B, Mandon-Pépin B, Stefansdottir A, Filis P, Kyle C, Zhang Z, Allen C, Purdie L, Jouneau L, Cotinot C, Rhind SM, Sinclair KD, Fowler PA. The fetal ovary exhibits temporal sensitivity to a ‘real-life’ mixture of environmental chemicals. Sci Rep. 2016;6:22279. https://doi.org/10.1038/srep22279.
Zama AM, Uzumcu M. Fetal and neonatal exposure to the endocrine disruptor Methoxychlor causes epigenetic alterations in adult ovarian genes. Endocrinology. 2009;150(10):4681–91. https://doi.org/10.1210/en.2009-0499.
Zama AM, Uzumcu M. Targeted genome-wide methylation and gene expression analyses reveal signaling pathways involved in ovarian dysfunction after developmental EDC exposure in Rats1. Biol Reprod. 2013;88(2):1–13. https://doi.org/10.1095/biolreprod.112.104802.
Heindel JJ, Balbus J, Birnbaum L, Brune-Drisse MN, Grandjean P, Gray K, Landrigan PJ, Sly PD, Suk W, Slechta DC. Developmental origins of health and disease: integrating environmental influences. Endocrinology. 2015;156(10):3416–21.
Saeidnia S, Abdollahi M. Toxicological and pharmacological concerns on oxidative stress and related diseases. Toxicol Appl Pharmacol. 2013;273(3):442–55. https://doi.org/10.1016/j.taap.2013.09.031.
Luderer U. Chapter four - ovarian toxicity from reactive oxygen species. In: Litwack G, editor. Vitamins & hormones, vol. 94. Cambridge, MA: Academic Press; 2014. p. 99–127. https://doi.org/10.1016/B978-0-12-800095-3.00004-3.
Wang W, Craig ZR, Basavarajappa MS, Gupta RK, Flaws JA. Di (2-ethylhexyl) phthalate inhibits growth of mouse ovarian antral follicles through an oxidative stress pathway. Toxicol Appl Pharmacol. 2012;258(2):288–95. https://doi.org/10.1016/j.taap.2011.11.008.
Gupta RK, Miller KP, Babus JK, Flaws JA. Methoxychlor inhibits growth and induces atresia of Antral follicles through an oxidative stress pathway. Toxicol Sci. 2006;93(2):382–9. https://doi.org/10.1093/toxsci/kfl052.
Sobinoff AP, Pye V, Nixon B, Roman SD, McLaughlin EA. Adding insult to injury: effects of xenobiotic-induced Preantral Ovotoxicity on ovarian development and oocyte fusibility. Toxicol Sci. 2010;118(2):653–66. https://doi.org/10.1093/toxsci/kfq272.
Armstrong D, Goff A, Dorrington J. Ovarian follicular development and function. New York: Raven Press; 1979. p. 169–82.
Hillier SG, Whitelaw PF, Smyth CD. Follicular oestrogen synthesis: the ‘two-cell, two-gonadotrophin’ model revisited. Mol Cell Endocrinol. 1994;100(1-2):51–4.
Erickson GF, Magoffin DA, Dyer CA, Hofeditz C. The ovarian androgen producing cells: a review of structure/function relationships. Endocr Rev. 1985;6(3):371–99.
Richards JS. Hormonal control of gene expression in the ovary. Endocr Rev. 1994;15(6):725–51.
Myllymäki S, Haavisto T, Vainio M, Toppari J, Paranko J. In vitro effects of diethylstilbestrol, genistein, 4-tert-butylphenol, and 4-tert-octylphenol on steroidogenic activity of isolated immature rat ovarian follicles. Toxicol Appl Pharmacol. 2005;204(1):69–80.
Kazeto Y, Place AR, Trant JM. Effects of endocrine disrupting chemicals on the expression of CYP19 genes in zebrafish (Danio rerio) juveniles. Aquat Toxicol. 2004;69(1):25–34. https://doi.org/10.1016/j.aquatox.2004.04.008.
Wang J, Liu X, Wang H, Wu T, Hu X, Qin F, Wang Z. Expression of two cytochrome P450 aromatase genes is regulated by endocrine disrupting chemicals in rare minnow Gobiocypris rarus juveniles. Comp Biochem Physiol Part C: Toxicol Pharmacol. 2010;152(3):313–20.
Urbatzka R, Rocha E, Reis B, Cruzeiro C, Monteiro RAF, Rocha MJ. Effects of ethinylestradiol and of an environmentally relevant mixture of xenoestrogens on steroidogenic gene expression and specific transcription factors in zebrafish. Environ Pollut. 2012;164:28–35. https://doi.org/10.1016/j.envpol.2012.01.018.
Puthumana J, Kim B-M, Jeong C-B, Kim D-H, Kang H-M, Jung J-H, Kim I-C, Hwang U-K, Lee J-S. Nine co-localized cytochrome P450 genes of the CYP2N, CYP2AD, and CYP2P gene families in the mangrove killifish Kryptolebias marmoratus genome: identification and expression in response to B [α] P, BPA, OP, and NP. Aquat Toxicol. 2017;187:132–40.
Roelofs MJE, Piersma AH, van den Berg M, van Duursen MBM. The relevance of chemical interactions with CYP17 enzyme activity: assessment using a novel in vitro assay. Toxicol Appl Pharmacol. 2013;268(3):309–17. https://doi.org/10.1016/j.taap.2013.01.033.
Jorge Chedrese P, Feyles F. The diverse mechanism of action of dichlorodiphenyldichloroethylene (DDE) and methoxychlor in ovarian cells in vitro. Reprod Toxicol. 2001;15(6):693–8. https://doi.org/10.1016/S0890-6238(01)00172-1.
Crellin N, Kang H, Swan C, Chedrese P. Inhibition of basal and stimulated progesterone synthesis by dichlorodiphenyldichloroethylene and methoxychlor in a stable pig granulosa cell line. Reproduction. 2001;121(3):485–92.
Younglai E, Kwan T, Kwan C-Y, Lobb D, Foster W. Dichlorodiphenylchloroethylene elevates cytosolic calcium concentrations and oscillations in primary cultures of human granulosa-lutein cells. Biol Reprod. 2004;70(6):1693–700.
Shanle EK, Xu W. Endocrine disrupting chemicals targeting estrogen receptor signaling: identification and mechanisms of action. Chem Res Toxicol. 2011;24(1):6–19. https://doi.org/10.1021/tx100231n.
Kiyama R, Wada-Kiyama Y. Estrogenic endocrine disruptors: molecular mechanisms of action. Environ Int. 2015;83:11–40. https://doi.org/10.1016/j.envint.2015.05.012.
le Maire A, Bourguet W, Balaguer P. A structural view of nuclear hormone receptor: endocrine disruptor interactions. Cell Mol Life Sci. 2010;67(8):1219–37. https://doi.org/10.1007/s00018-009-0249-2.
Li Y, Luh CJ, Burns KA, Arao Y, Jiang Z, Teng CT, Tice RR, Korach KS. Endocrine-disrupting chemicals (EDCs): in vitro mechanism of estrogenic activation and differential effects on ER target genes. Environ Health Perspect. 2013;121(4):459–66. https://doi.org/10.1289/ehp.1205951.
Sheikh IA, Tayubi IA, Ahmad E, Ganaie MA, Bajouh OS, AlBasri SF, Abdulkarim IMJ, Beg MA. Computational insights into the molecular interactions of environmental xenoestrogens 4-tert-octylphenol, 4-nonylphenol, bisphenol A (BPA), and BPA metabolite, 4-methyl-2, 4-bis (4-hydroxyphenyl) pent-1-ene (MBP) with human sex hormone-binding globulin. Ecotoxicol Environ Saf. 2017;135:284–91. https://doi.org/10.1016/j.ecoenv.2016.10.005.
Heindel JJ, Vandenberg LN. Developmental origins of health and disease: a paradigm for understanding disease cause and prevention. Curr Opin Pediatr. 2015;27(2):248–53. https://doi.org/10.1097/MOP.0000000000000191.
Rosenfeld CS. The epigenome and developmental origins of health and disease. Cambridge, MA: Academic Press; 2015.
Hoffman DJ, Reynolds RM, Hardy DB. Developmental origins of health and disease: current knowledge and potential mechanisms. Nutr Rev. 2017;75(12):951–70.
Rattan S, Flaws JA. The epigenetic impacts of endocrine disruptors on female reproduction across generations. Biol Reprod. 2019;101(3):635–44.
Xin F, Susiarjo M, Bartolomei MS. Multigenerational and transgenerational effects of endocrine disrupting chemicals: a role for altered epigenetic regulation? Semin Cell Dev Biol. 2015;43:66–75. https://doi.org/10.1016/j.semcdb.2015.05.008.
Skinner MK. Endocrine disruptors in 2015: epigenetic transgenerational inheritance. Nat Rev Endocrinol. 2016;12(2):68–70. https://doi.org/10.1038/nrendo.2015.206.
Zhou C, Gao L, Flaws JA. Exposure to an environmentally relevant phthalate mixture causes Transgenerational effects on female reproduction in mice. Endocrinology. 2017;158(6):1739–54. https://doi.org/10.1210/en.2017-00100.
Brehm E, Rattan S, Gao L, Flaws JA. Prenatal exposure to Di(2-Ethylhexyl) phthalate causes long-term Transgenerational effects on female reproduction in mice. Endocrinology. 2018;159(2):795–809. https://doi.org/10.1210/en.2017-03004.
Vandenberg LN, Hauser R, Marcus M, Olea N, Welshons WV. Human exposure to bisphenol A (BPA). Reprod Toxicol. 2007;24(2):139–77.
Fleisch AF, Sheffield PE, Chinn C, Edelstein BL, Landrigan PJ. Bisphenol A and related compounds in dental materials. Pediatrics. 2010;126(4):760–8. https://doi.org/10.1542/peds.2009-2693.
Patel S, Brehm E, Gao L, Rattan S, Ziv-Gal A, Flaws JA. Bisphenol A exposure, ovarian follicle numbers, and female sex steroid hormone levels: results from a CLARITY-BPA study. Endocrinology. 2017;158(6):1727–38.
Patel S, Zhou C, Rattan S, Flaws JA. Effects of endocrine-disrupting chemicals on the ovary. Biol Reprod. 2015;93(1):21–9.
Ziv-Gal A, Flaws JA. Evidence for bisphenol A-induced female infertility: a review (2007–2016). Fertil Steril. 2016;106(4):827–56.
Teeguarden J, Hanson-Drury S, Fisher JW, Doerge DR. Are typical human serum BPA concentrations measurable and sufficient to be estrogenic in the general population? Food Chem Toxicol. 2013;62:949–63.
Organization WH (2011) Joint FAO/WHO expert meeting to review toxicological and health aspects of bisphenol A: final report, including report of stakeholder meeting on bisphenol A, Nov. 1–5, 2010, Ottawa, Canada.
Program NT. Carcinogenesis bioassay of Bisphenol A (CAS no. 80-05-7) in F344 rats and B6C3F1 mice (feed study). Natl Toxicol Program Tech Rep Ser. 1982;215:1–116.
Birnbaum LS. Environmental chemicals: evaluating low-dose effects. Research Triangle, NC: National Institute of Environmental Health Sciences; 2012.
Vandenberg LN. Low-dose effects of hormones and endocrine disruptors. In: Vitamins & hormones, vol. 94. Amsterdam: Elsevier; 2014. p. 129–65.
Vandenberg LN, Colborn T, Hayes TB, Heindel JJ, Jacobs DR Jr, Lee D-H, Shioda T, Soto AM, Vom Saal FS, Welshons WV. Hormones and endocrine-disrupting chemicals: low-dose effects and nonmonotonic dose responses. Endocr Rev. 2012;33(3):378–455.
Mok-Lin E, Ehrlich S, Williams PL, Petrozza J, Wright DL, Calafat AM, Ye X, Hauser R. Urinary bisphenol A concentrations and ovarian response among women undergoing IVF. Int J Androl. 2010;33(2):385–93. https://doi.org/10.1111/j.1365-2605.2009.01014.x.
Martínez M, Rovira J, Sharma RP, Nadal M, Schuhmacher M, Kumar V. Prenatal exposure estimation of BPA and DEHP using integrated external and internal dosimetry: a case study. Environ Res. 2017;158:566–75.
Yamada H, Furuta I, Kato EH, Kataoka S, Usuki Y, Kobashi G, Sata F, Kishi R, Fujimoto S. Maternal serum and amniotic fluid bisphenol A concentrations in the early second trimester. Reprod Toxicol. 2002;16(6):735–9.
Souter I, Smith KW, Dimitriadis I, Ehrlich S, Williams PL, Calafat AM, Hauser R. The association of bisphenol-A urinary concentrations with antral follicle counts and other measures of ovarian reserve in women undergoing infertility treatments. Reprod Toxicol. 2013;42:224–31.
Saddick SY. Light and transmission Electron microscopic studies on subacute toxicity of Bisphenol A on the rat ovary. Anal Quant Cytopathol Histopathol. 2015;37(4):227–34.
Santamaría C, Durando M, de Toro MM, Luque EH, Rodriguez HA. Ovarian dysfunctions in adult female rat offspring born to mothers perinatally exposed to low doses of bisphenol A. J Steroid Biochem Mol Biol. 2016;158:220–30.
Kato H, Ota T, Furuhashi T, Ohta Y, Iguchi T. Changes in reproductive organs of female rats treated with bisphenol A during the neonatal period. Reprod Toxicol. 2003;17(3):283–8. https://doi.org/10.1016/S0890-6238(03)00002-9.
Chao H-H, Zhang X-F, Chen B, Pan B, Zhang L-J, Li L, Sun X-F, Shi Q-H, Shen W. Bisphenol A exposure modifies methylation of imprinted genes in mouse oocytes via the estrogen receptor signaling pathway. Histochem Cell Biol. 2012;137(2):249–59.
Zhang T, Li L, Qin XS, Zhou Y, Zhang XF, Wang LQ, De Felici M, Chen H, Qin GQ, Shen W. Di-(2-ethylhexyl) phthalate and bisphenol A exposure impairs mouse primordial follicle assembly in vitro. Environ Mol Mutagen. 2014;55(4):343–53.
Lenie S, Cortvrindt R, Eichenlaub-Ritter U, Smitz J. Continuous exposure to bisphenol A during in vitro follicular development induces meiotic abnormalities. Mutat Res Genet Toxicol Environ Mutagen. 2008;651(1):71–81. https://doi.org/10.1016/j.mrgentox.2007.10.017.
Rivera OE, Varayoud J, Rodríguez HA, Muñoz-de-Toro M, Luque EH. Neonatal exposure to bisphenol A or diethylstilbestrol alters the ovarian follicular dynamics in the lamb. Reprod Toxicol. 2011;32(3):304–12.
Veiga-Lopez A, Beckett E, Salloum BA, Ye W, Padmanabhan V. Developmental programming: prenatal BPA treatment disrupts timing of LH surge and ovarian follicular wave dynamics in adult sheep. Toxicol Appl Pharmacol. 2014;279(2):119–28.
Gieske MC, Lawson C, Smith H, Murdoch B, Vande Voort C, Hunt PA. Fetal exposure to Bisphenol A causes meiotic defects and abnormal follicle formation in a primate model. Oxford, UK: Oxford University Press; 2011.
Migliaccio M, Chioccarelli T, Ambrosino C, Suglia A, Manfrevola F, Carnevali O, Fasano S, Pierantoni R, Cobellis G. Characterization of follicular atresia responsive to BPA in Zebrafish by morphometric analysis of follicular stage progression. Int J Endocrinol. 2018;2018:4298195.
Li Y, Zhang W, Liu J, Wang W, Li H, Zhu J, Weng S, Xiao S, Wu T. Prepubertal bisphenol A exposure interferes with ovarian follicle development and its relevant gene expression. Reprod Toxicol. 2014;44:33–40.
Altunbas K, Celik S, Yagci A, Akkaya OO. The effect of bisphenol A on Notch signaling pathway in the follicular development of neonatal rat ovary. In: World Congress of Reproductive Biology 2014. Bristol, UK: BioScientifica; 2014.
Moore-Ambriz TR, Acuña-Hernández DG, Ramos-Robles B, Sánchez-Gutiérrez M, Santacruz-Márquez R, Sierra-Santoyo A, Piña-Guzmán B, Shibayama M, Hernández-Ochoa I. Exposure to bisphenol A in young adult mice does not alter ovulation but does alter the fertilization ability of oocytes. Toxicol Appl Pharmacol. 2015;289(3):507–14.
Yön ND, Akbulut C. Histological changes in zebrafish (Danio rerio) ovaries following administration of bisphenol A. Pak J Zool. 2014;46(4):1153–9.
Hunt PA, Lawson C, Gieske M, Murdoch B, Smith H, Marre A, Hassold T, Vande Voort CA. Bisphenol A alters early oogenesis and follicle formation in the fetal ovary of the rhesus monkey. Proc Natl Acad Sci. 2012;109(43):17525–30.
Brieno-Enriquez M, Robles P, Camats-Tarruella N, Garcia-Cruz R, Roig I, Cabero L, Martinez F, Caldés MG. Human meiotic progression and recombination are affected by Bisphenol A exposure during in vitro human oocyte development. Hum Reprod. 2011;26(10):2807–18.
Susiarjo M, Hassold TJ, Freeman E, Hunt PA. Bisphenol A exposure in utero disrupts early oogenesis in the mouse. PLoS Genet. 2007;3(1):e5.
Lawson C, Gieske M, Murdoch B, Ye P, Li Y, Hassold T, Hunt PA. Gene expression in the fetal mouse ovary is altered by exposure to low doses of bisphenol A. Biol Reprod. 2011;84(1):79–86.
Zhang H-Q, Zhang X-F, Zhang L-J, Chao H-H, Pan B, Feng Y-M, Li L, Sun X-F, Shen W. Fetal exposure to bisphenol A affects the primordial follicle formation by inhibiting the meiotic progression of oocytes. Mol Biol Rep. 2012;39(5):5651–7.
Aoki T, Takada T. Bisphenol a modulates germ cell differentiation and retinoic acid signaling in mouse ES cells. Reprod Toxicol. 2012;34(3):463–70. https://doi.org/10.1016/j.reprotox.2012.06.001.
Liu B, Zhou S, Yang C, Chen P, Chen P, Xi D, Zhu H, Gao Y. Bisphenol a deteriorates egg quality through HDAC7 suppression. Oncotarget. 2017;8(54):92359.
Xin L, Lin Y, Wang A, Zhu W, Liang Y, Su X, Hong C, Wan J, Wang Y, Tian H. Cytogenetic evaluation for the genotoxicity of bisphenol-a in Chinese hamster ovary cells. Environ Toxicol Pharmacol. 2015;40(2):524–9.
Allard P, Colaiácovo MP. Bisphenol a impairs the double-strand break repair machinery in the germline and causes chromosome abnormalities. Proc Natl Acad Sci. 2010;107(47):20405–10.
Brieno-Enriquez M, Reig-Viader R, Cabero L, Toran N, Martinez F, Roig I, Garcia Caldes M. Gene expression is altered after bisphenol a exposure in human fetal oocytes in vitro. Mol Hum Reprod. 2011;18(4):171–83.
Ganesan S, Keating AF. Bisphenol A-induced ovotoxicity involves DNA damage induction to which the ovary mounts a protective response indicated by increased expression of proteins involved in DNA repair and xenobiotic biotransformation. Toxicol Sci. 2016;152(1):169–80.
Nah WH, Park MJ, Gye MC. Effects of early prepubertal exposure to bisphenol a on the onset of puberty, ovarian weights, and estrous cycle in female mice. Clin Exp Reprod Med. 2011;38(2):75–81.
Shi M, Sekulovski N, Mac Lean JA, Whorton A, Hayashi K. Prenatal exposure to Bisphenol a analogues on female reproductive functions in mice. Toxicol Sci. 2019;168(2):561–71.
Bloom MS, Kim D, Vom Saal FS, Taylor JA, Cheng G, Lamb JD, Fujimoto VY. Bisphenol A exposure reduces the estradiol response to gonadotropin stimulation during in vitro fertilization. Fertil Steril. 2011;96(3):672–7.
Cao Y, Qu X, Ming Z, Yao Y, Zhang Y. The correlation between exposure to BPA and the decrease of the ovarian reserve. Int J Clin Exp Pathol. 2018;11(7):3375–82.
Berger RG, Hancock T, DeCatanzaro D. Influence of oral and subcutaneous bisphenol-a on intrauterine implantation of fertilized ova in inseminated female mice. Reprod Toxicol. 2007;23(2):138–44.
Grasselli F, Baratta L, Baioni L, Bussolati S, Ramoni R, Grolli S, Basini G. Bisphenol A disrupts granulosa cell function. Domest Anim Endocrinol. 2010;39(1):34–9.
Zhang Y, Gao J, Xu P, Yuan C, Qin F, Liu S, Zheng Y, Yang Y, Wang Z. Low-dose bisphenol a disrupts gonad development and steroidogenic genes expression in adult female rare minnow Gobiocypris rarus. Chemosphere. 2014;112:435–42.
Mlynarčíková A, Kolena J, Ficková M, Scsuková S. Alterations in steroid hormone production by porcine ovarian granulosa cells caused by bisphenol A and bisphenol A dimethacrylate. Mol Cell Endocrinol. 2005;244(1):57–62. https://doi.org/10.1016/j.mce.2005.02.009.
Zhou W, Liu J, Liao L, Han S, Liu J. Effect of bisphenol a on steroid hormone production in rat ovarian theca-interstitial and granulosa cells. Mol Cell Endocrinol. 2008;283(1):12–8. https://doi.org/10.1016/j.mce.2007.10.010.
Mansur A, Adir M, Yerushalmi G, Hourvitz A, Gitman H, Yung Y, Orvieto R, Machtinger R. Does BPA alter steroid hormone synthesis in human granulosa cells in vitro? Hum Reprod. 2016;31(7):1562–9.
Peretz J, Flaws JA. Bisphenol a down-regulates rate-limiting Cyp11a1 to acutely inhibit steroidogenesis in cultured mouse antral follicles. Toxicol Appl Pharmacol. 2013;271(2):249–56.
Banerjee O, Singh S, Prasad SK, Bhattacharjee A, Banerjee A, Banerjee A, Saha A, Maji BK, Mukherjee S. Inhibition of catalase activity with 3-amino-1, 2, 4-triazole intensifies bisphenol a (BPA)-induced toxicity in granulosa cells of female albino rats. Toxicol Ind Health. 2018;34(11):787–97.
Santangeli S, Consales C, Pacchierotti F, Habibi H, Carnevali O. Transgenerational effects of BPA on female reproduction. Sci Total Environ. 2019;
Ziv-Gal A, Wang W, Zhou C, Flaws JA. The effects of in utero bisphenol a exposure on reproductive capacity in several generations of mice. Toxicol Appl Pharmacol. 2015;284(3):354–62.
Wang W, Hafner KS, Flaws JA. In utero bisphenol a exposure disrupts germ cell nest breakdown and reduces fertility with age in the mouse. Toxicol Appl Pharmacol. 2014;276(2):157–64.
Zhou C, Wang W, Peretz J, Flaws JA. Bisphenol a exposure inhibits germ cell nest breakdown by reducing apoptosis in cultured neonatal mouse ovaries. Reprod Toxicol. 2015;57:87–99.
Berger A, Ziv-Gal A, Cudiamat J, Wang W, Zhou C, Flaws JA. The effects of in utero bisphenol a exposure on the ovaries in multiple generations of mice. Reprod Toxicol. 2016;60:39–52.
Liu Y, Zhang Y, Tao S, Guan Y, Zhang T, Wang Z. Global DNA methylation in gonads of adult zebrafish Danio rerio under bisphenol a exposure. Ecotoxicol Environ Saf. 2016;130:124–32.
Liu Y, Yuan C, Chen S, Zheng Y, Zhang Y, Gao J, Wang Z. Global and cyp19a1a gene specific DNA methylation in gonads of adult rare minnow Gobiocypris rarus under bisphenol a exposure. Aquat Toxicol. 2014;156:10–6.
Zhang X-F, Zhang L-J, Feng Y-N, Chen B, Feng Y-M, Liang G-J, Li L, Shen W. Bisphenol a exposure modifies DNA methylation of imprint genes in mouse fetal germ cells. Mol Biol Rep. 2012;39(9):8621–8.
Santangeli S, Maradonna F, Gioacchini G, Cobellis G, Piccinetti CC, Dalla Valle L, Carnevali O. BPA-induced deregulation of epigenetic patterns: effects on female zebrafish reproduction. Sci Rep. 2016;6:21982.
Mahalingam S, Ther L, Gao L, Wang W, Ziv-Gal A, Flaws JA. The effects of in utero bisphenol a exposure on ovarian follicle numbers and steroidogenesis in the F1 and F2 generations of mice. Reprod Toxicol. 2017;74:150–7.
Moustafa GG, Ahmed AA. Impact of prenatal and postnatal exposure to bisphenol a on female rats in a two generational study: Genotoxic and immunohistochemical implications. Toxicol Rep. 2016;3:685–95.
Cotinot C, Mandon-Pepin B, Loup B, Amezaga MR, Lea RG, Sinclair KD, Rhind SM, Fowler PA In vitro exposre to environmental doses of BPA, MEHP and PCBs results in few transcriptions alterations in the fetal sheep ovary. In: Biology of Reproduction, 2013.
Ahsan N, Ullah H, Ullah W, Jahan S. Comparative effects of Bisphenol S and Bisphenol A on the development of female reproductive system in rats; a neonatal exposure study. Chemosphere. 2018;197:336–43.
Hill CE, Sapouckey SA, Suvorov A, Vandenberg LN. Developmental exposures to bisphenol S, a BPA replacement, alter estrogen-responsiveness of the female reproductive tract: a pilot study. Cogent Med. 2017;4(1):1317690.
Chen Y, Shu L, Qiu Z, Lee DY, Settle SJ, Hee SQ, Telesca D, Yang X, Allard P. Exposure to the BPA-substitute bisphenol S causes unique alterations of germline function. PLoS Genet. 2016;12(7):e1006223.
Nourian A, Soleimanzadeh A, Jalali AS, Najafi G. Effects of bisphenol-S low concentrations on oxidative stress status and in vitro fertilization potential in mature female mice. In: Veterinary research forum. Urmia, Iran: Urmia University; 2017. p. 341.
Zaid SSM, Othman S, Kassim NM. Potential protective effect of Tualang honey on BPA-induced ovarian toxicity in prepubertal rat. BMC Complement Altern Med. 2014;14(1):509.
Mohamad Zaid SS, Kassim NM, Othman S. Tualang honey protects against bpa-induced morphological abnormalities and disruption of ERα, ERβ, and C3 mRNA and protein expressions in the uterus of rats. Evid Based Complement Alternat Med. 2015;2015:202874. https://doi.org/10.1155/2015/202874. Epub 2015 Dec 14. PMID: 26788107; PMCID: PMC4691614
Bilgi A, Abalı R, Bilgi PT, Şahin M, Tunçdemir M, Boran AB. The apoptotic effects of bisphenol a exposure on the rat ovary: an experimental study. Environ Sci Pollut Res. 2019;26(10):1–6.
Mehranjani MS, Mansoori T. Stereological study on the effect of vitamin C in preventing the adverse effects of bisphenol a on rat ovary. Int J Reprod Biomed. 2016;14(6):403.
Lee C-T, Wang J-Y, Chou K-Y, Hsu M-I. 1, 25-Dihydroxyvitamin D3 modulates the effects of sublethal BPA on mitochondrial function via activating PI3K-Akt pathway and 17β-estradiol secretion in rat granulosa cells. J Steroid Biochem Mol Biol. 2019;185:200–11.
Zaid SSM, Kassim NM, Othman S. Tualang honey protects against BPA-Induced morphological abnormalities and disruption of ERα, ERβ, and C3 mRNA and protein expressions in the uterus of rats. Evid Based Complement Alternat Med. 2015;202874. https://doi.org/10.1155/2015/202874.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Huang, J., Zeng, H. (2021). The Influence of Environmental Factors on Ovarian Function, Follicular Genesis, and Oocyte Quality. In: Zhang, H., Yan, J. (eds) Environment and Female Reproductive Health. Advances in Experimental Medicine and Biology, vol 1300. Springer, Singapore. https://doi.org/10.1007/978-981-33-4187-6_3
Download citation
DOI: https://doi.org/10.1007/978-981-33-4187-6_3
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-33-4186-9
Online ISBN: 978-981-33-4187-6
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)