Abstract
Tamponading agents help to keep the retina attached by keeping the neurosensory retina opposed to RPE whilst retinopexy heals. Tamponading agents could be gaseous or liquid. Commonly used gaseous agents include air, sulphur hexafluoride, and perfluoropropane. Liquid agents include silicone oil perfluorocarbon liquids and heavy silicone oil.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Tamponading agents close the retinal break and keep the neurosensory retina opposed to the RPE whilst retinopexy heals. The surface tension of the tamponading agents helps to seal the retinal break and prevents fluid from moving into the sub-retinal space till the retinopexy forms a permanent barrier. Ohm was the first to introduce air into the vitreous cavity although he did not use the word “tamponade” [1]. Rosengren was the first to use the word “tamponade” and reported successful treatment of retinal detachment with air. Tamponading agents can be divided into liquids and gases [2].
2 Physical Properties of Tamponading Agents
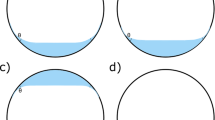
The tamponade effect of the vitreous substitutes depends on the arc of contact between the agent and the inner retinal surface, which mainly depends on four physical parameters, namely, specific gravity, buoyancy, interfacial tension, and viscosity [3].
Specific Gravity
The specific gravity of the aqueous and vitreous humour is slightly more than water. The specific gravity for any tamponading agent should be less than water to allow it to float in the vitreous cavity.
Buoyancy
Buoyancy is the force that keeps any object afloat. Archimedes principle states that any object, wholly or partially immersed in a fluid, is pushed up by a force that is equal to the weight of the fluid displaced by the object. The buoyancy of intraocular gas is more than that of silicone oil as its specific gravity is much less than water. The buoyancy is maximum at the apex of the bubble.
Interfacial Tension
When two immiscible agents are used, the interaction that occurs at the surface of the substance is called interfacial tension. A substance with higher interfacial tension tends to remain as a single large bubble with minimal dispersion. Gases have higher interfacial tension compared to liquids such as PFCL and silicone oil.
Viscosity
Viscosity of a fluid is defined as resistance to deformation. The lesser the viscosity, the lower is the energy required to deform a large bubble into small droplets. Silicone oil has high viscosity ranging from 1000Ccs to 5000cs preventing its dispersion into small bubbles.
3 Types of Tamponading Agents
Tamponading agents can be gaseous or liquid. Commonly used gaseous agents include air, sulphur hexafluoride, and perfluoropropane. Liquid agents include silicone oil which is lighter than water. Perfluorocarbon liquids and heavy silicone oil are liquid tamponading agents which are heavier than water. The gas/water interface surface tension is the greatest and therefore is the most effective in closing retinal breaks (70 erg/cm2). This is followed by silicone oil/water interface surface tension (50 erg/cm2) [4].
4 Gaseous Tamponading Agents
4.1 Kinetics of Intraocular Gases
Air
Air is colourless, inert, non-expansile, and short-acting gas. It remains in the eyes for a few days and is then replaced by aqueous humour. Air has been successfully used as a tamponading agent in the repair of primary retinal detachment with superior breaks [3]. Superior breaks are isolated from SRF due to gravity and hence retina RPE adhesions form early. Therefore, short-acting tamponade such as air is useful as it leads to early visual recovery. Inferior breaks have also been treated with air if SRF is drained completely [4].
Other Gases
Sulphur hexafluoride (SF6) and perfluoropropane (C3F8) are the commonly used gases. C2F6 is also used less commonly. These gases are heavier than air. One hundred percent SF6 doubles in volume in 2 days and is completely absorbed in 10–14 days. Hundred percent C3F8 quadruples in volume in 3 days and lasts for 30–45 days. The gas bubble goes through the phases of expansion, equilibrium, and dissolution. The expansion is due to absorption of nitrogen, oxygen, and carbon dioxide from the surrounding fluid into the bubble. In the equilibrium phase, the diffusion of nitrogen into the bubble is balanced by diffusion of gas into the surrounding fluid. During the dissolution state, gas is ultimately absorbed in the bloodstream [5]. A small volume of pure gas is used in pneumatic retinopexy. Non-expansile air gas mixtures are used as tamponade after vitrectomy. Twenty percent SF6, 14% C3F8, and 16% C2F6 are commonly used to fill the vitreous cavity after vitrectomy (Fig. 11.1).
4.2 Preparation of Gas for Injection
A millipore filter is used to maintain the sterility of the gas. A 50-mL syringe is usually used to withdraw gas from the cylinder. The gas is diluted with air to achieve the appropriate concentration of the gas. In cases of pneumatic retinopexy where pure expansile gas is required, a pressure reducing system can be attached to the gas cylinder to withdraw the gas. The gas should not be left in the syringe for long periods as the gas concentration may get altered due to diffusion of gases. For injecting gas after vitrectomy, fluid–air exchange is first performed. Air is then replaced by the desired gas. Infusion is stopped by applying a clamp to the infusion cannula. Gas syringe is then connected to the infusion line, the clamp removed and around 40 mL of gas is slowly injected to replace air.
4.3 Contraindication
Air Travel
Reduced atmospheric pressure during air travel can lead to expansion of intraocular gas bubble and increase in intraocular pressure. This can lead to pain, decreased vision, vascular occlusion, and in extreme cases wound dehiscence and globe rupture. It is therefore advisable to avoid air travel if there is any intravitreal gas bubble.
Diving
During diving, the hyperbaric pressure causes the intraocular gas bubble to decrease in size according to Boyle’s law. During the ascent back to the water surface, atmospheric pressure decreases causing expansion of the gas bubble, which can result in vitreous, retinal, or choroidal haemorrhage [6].
Nitrous Oxide Anaesthesia
Nitrous oxide in the blood is highly water soluble. It can enter the intraocular gas bubble and lead to increased intraocular pressure. Later when the nitrous oxide returns to the bloodstream, the eye becomes hypotonous. Therefore, nitrous oxide should be discontinued at least 30 min before the injection of intraocular gas to allow its clearance from the bloodstream. Also, the use of nitrous oxide anaesthesia in gas-filled eyes must be avoided.
4.4 Complications
Increase in Intraocular Pressure
It is one of the most common complications of intraocular gas. It is usually transient due to gas expansion and can be managed by topical and systemic medications. Elevated IOP is more dangerous in eyes with pre-existing optic nerve damage. The gas bubble may expand to push the lens iris diaphragm forward which can lead to angle-closure glaucoma. Gas aspiration from the vitreous cavity may be indicated in such cases. Aphakic eyes are more prone to this complication as the iris can easily move forward.
Cataract
Oxidative stress following vitrectomy can lead to cataract. Prolonged contact of intraocular gas with the posterior surface of the lens leads to posterior subcapsular cataract. Poor compliance with post-operative positioning can lead to early development of cataracts.
Gas Migration
Gas can migrate into the subconjunctival space, anterior chamber, or sub-retinal space. Subconjunctival migration can occur due to inadequate sclerotomy closure. In most cases no treatment is required. Anterior chamber gas migration can occur even in phakic eyes without any zonular weakness. Intraoperative migration of gas in AC can lead to poor visualization of the posterior segment. Ophthalmic viscoelastic substances can be inserted into AC to remove gas. Long-term presence of gas in AC can lead to corneal decompensation. This is due to decreased endothelial nutrition due to direct contact between the gas and the endothelium. Gas is not directly endotheliotoxic [7]. Sub-retinal migration of gas can occur during fluid–air exchange if the traction on the retina is not adequately relieved. During pneumatic retinopexy, sub-retinal gas migration can occur if there is fish egging of the gas bubble.
5 Silicone Oil
Silicone oil was introduced by Cibis for use as intraocular tamponade [8]. They are particularly useful in cases that require a longer duration of tamponade.
5.1 Chemical Property
Silicone oils are hydrophobic polymers of silicone–oxygen bonds called organosiloxane with a variety of side chains. The chemical and physical properties of the silicone oil depend upon the molecular weight, the length of the linear chain, and the chemical structure of the side group. Viscosity of the silicone oil is expressed in centistokes. Increase in the polymer chain length increases the molecular weight of the oil thus increasing its viscosity. Silicone oil that is currently in use has viscosity ranging from 1000cs to 5000cs. Increase in the viscosity of silicone oil lessens the emulsification [9]. The radical side groups determine whether the silicone oil is heavier or lighter than water. The most commonly used silicone oil is polydimethylsiloxane which is lighter than water.
5.2 Physical Property
Silicone oil has a buoyant force as the specific gravity of silicone oil (around 0.97) is less than the aqueous and the vitreous humour. This upward force helps in maintaining the reattachment of the superior retina if the traction is adequately relieved. The presence of silicone oil close to the retina can also cause redirection of radial forces to tangential forces, which in turn are less effective. As the posterior retinal surface is covered by only a thin layer of aqueous, the intraocular fluid currents are inadequate to cause retinal redetachment unless the traction is significant [10]. There is always an inferior space filled with vitreous fluid as silicone oil cannot completely fill the eye. This inferior fluid with restricted movement can gradually accumulate proteins and lead to perisilicone proliferation.
The surface tension is responsible to maintain the shape of the bubble, prevent its migration through the retinal hole, and prevent any emulsification. Presence of surgical debris such as blood, viscoelastic solution, lipid, proteins etc. tend to decrease the surface tension and lead to early emulsification. Silicone oil emulsification increases the risk of PVR, retinal redetachment, keratopathy, and secondary glaucoma. Increasing the viscosity decreases the rate of emulsification. However, it has been shown that there is no difference in emulsification between 1000cs and 5000cs oil [11]. This is because apart from viscosity, other factors affect the rate of emulsification, which are content of impurities or low molecular weight siloxane, and absorption of various biological fluids such as blood, protein, lipids etc. Emulsification of silicone oil is also time dependent and most cases emulsify within 1 year [12]. Movement of silicone oil can lead to shear forces which can cause early emulsification. A more complete fill of silicone oil decreases the rate of emulsification.
5.3 Indications for Using Silicone Oil
Retinal Detachment
Silicone oil is the tamponading agent of choice in cases of RD with PVR, viral retinitis, giant retinal tear, and choroidal coloboma and in chronic uveitis with hypotony [13].
RD with PVR
The silicone study group was a randomized multicentre trial to compare silicone oil with long-acting gas (SF6 or C3F8) as the tamponading agent for the management of RD with PVR [14,15,16,17,18]. It was found that silicone oil performed better than SF6 with visual acuity better than 5/200 and attached macula. However, C3F8 had similar results as that of silicone oil. Even in eyes needing relaxing retinotomy, silicone oil was found to be as effective as C3F8. Complications related to IOP and corneal abnormalities were found to be similar to oil and C3F8. Silicone oil is the tamponade of choice in cases of severe anterior PVR, difficulty in postoperative positioning, cases of redetachment, hypotony, and in one-eyed patients for early visual recovery.
Proliferative Diabetic Retinopathy
Use of silicone oil in PDR can cause regression of pre-existing iris neovascularisation and prevent post-operative rubeosis by compartmentalizing the eye and preventing the migration of the angiogenic factors anteriorly [19, 20]. Silicone oil can act as a diffusion barrier to oxygen and prevents the decrease in anterior chamber oxygen tension, hence decreases the stimulus for neovascularization [21]. Haemorrhage can lead to reproliferation behind silicone oil, which can be prevented by sealing all the bleeding points. In cases with attached retina with recurrent haemorrhage because of rubeosis iridis, silicone oil injection can lead to useful ambulatory vision. Sophisticated surgical technique combined with silicone oil has shown some success in eyes with very poor prognosis such as those with failed vitrectomy for PDR with advanced PVR [22].
Trauma
Retinal detachment following trauma can be associated with severe PVR, retinal incarceration, choroidal detachment, vitreous haemorrhage, unstable scleral wound, and hypotony due to ciliary body detachment. In such situations, silicone oil is useful for long-term tamponade.
5.4 Complications with Silicone Oil
Keratopathy
Corneal decompensation with bullous or band keratopathy can occur when silicone oil stays in contact with corneal endothelium for a long duration. This usually occurs when emulsified silicone oil migrates into the anterior chamber (Fig. 11.2). Even after oil removal, small oil droplets can migrate into anterior chamber and damage corneal endothelium. The Silicone Study report 7 disclosed an incidence of keratopathy of 27% at 2 years, equal to that of C3F8 [23].
Glaucoma
The incidence of silicone oil-induced secondary glaucoma ranges from 11 to 56% [24,25,26]. In the early postoperative period, the rise in IOP could be due to silicone oil overfill or pupillary block glaucoma. Pupillary block glaucoma is more common in aphakic eyes and is relieved by performing an inferior iridotomy. Chronic elevation of IOP occurs when emulsified oil directly blocks the aqueous outflow through the trabecular meshwork or causes inflammatory cells to impede the outflow. The treatment consists of antiglaucoma medications, topical or periocular steroids, and removal of silicone oil with the removal of oil droplets from the anterior chamber. IOP elevation may persist even after removal of oil as remaining small oil droplets or persistent inflammation may continue to obstruct the trabecular outflow or damage to the trabecular meshwork may be permanent. Glaucoma drainage devices may be used to treat such refractory glaucoma.
Silicone Oil Infiltration of Retina and Optic Nerve
Intraretinal oil droplets have been identified using OCT after macular hole surgery with internal limiting membrane (ILM) peel and silicone oil tamponade. The proposed mechanism is an iatrogenic defects in the ILM that may increase the ability of emulsified oil to penetrate retinal tissue [27]. Silicone oil infiltration of the optic nerve has been reported in another study using swept-source OCT, which showed multiple hyper-reflective spaces within the prelaminar optic nerve head and has been confirmed by adaptive optics [28]. Histopathological evidence of silicone oil invasion of the optic nerve has been shown in a patient who underwent RD repair after trauma.
Silicone Oil Adherence to Intraocular Lens (IOL)
Silicone oil most significantly adheres to silicone IOL. Small droplets may adhere to the IOL even after removal of silicone oil. This may result in visual disturbances. Simple irrigation of IOL may be partially affective in removing these droplets. Silicone oil may interact with the silicone IOL causing a permanent alteration on its surface.
5.5 Silicone Oil Removal
The optimal timing of silicone oil removal is controversial. Removal has been recommended as early as 2 months [29]. Anatomically successfully treated eyes have a likelihood of improved visual acuity after silicone oil removal [30]. The main complication associated with silicone oil removal is retinal redetachment and hypotony. The rate of retinal redetachment varies from 0 to 32% [25]. The duration of silicone oil tamponade does not affect the rate of redetachment [30]. Prophylactic 360-degree laser retinopexy and encircling reduces the incidence of redetachment after oil removal.
6 Heavy Silicone Oil
Densiron® 68 and Oxane HD are the available heavy silicone oils. Densiron® 68 (Fluoron Co, Neu-Ulm, Germany) is a solution of perfluorohexyloctane (F6H8) and 5000 cSt silicone oil, characterized by an increased viscosity of F6H8 (from 2.5 to 1387 mPa) and a resulting reduction of the tendency to disperse [31]. Oxane HD is a mixture of 5700-centistoke silicone oil and RMN-3 (a partially fluorinated olefin) with a viscosity of 3300-3500 mPa [32]. The buoyancy pressure in the upper retina with conventional silicone oil was calculated at only 0.05 mmHg. In an eye filled with Densiron, the added pressure (calculation with a specific gravity of 1.06 g/cm3) is approximately 0.1 mmHg [33].
In severe PVR, especially in cases with previous multiple vitreous surgeries and tenacious RD of the inferior quadrants, there is a high chance of redetachment. Owing to the lighter-than-water density of silicone oil, an accumulation of proliferative cells and mediators, uncovered retinal breaks, and areas of unsupported retina may exist inferiorly in eyes in a slight under-filled situation, which might cause recurrent or persistent retinal detachment. Heavy silicone oil can be a therapeutic option in patients with complex inferior retinal redetachment with PVR. As the density is more than water, it is effective in tamponading the inferior retina.
6.1 Complications and Adverse Reactions
Moderate inflammatory reaction with fibrin accumulation (30–40%), epiretinal membrane formation with suspected intraretinal gliosis (30%), persistent elevated IOP, and pseudo-hypopyon due to emulsification of silicone oil are the most common adverse effects seen in one of the studies where Densiron was used. The early emulsification and pseudo hypopyon formation can be explained by the lesser viscosity of Densiron compared to the higher viscosity of the commonly used silicone oil [34]. Redetachments within the posterior staphyloma in highly myopic patients are common during Densiron endotamponade [35].
7 Perfluorocarbon Liquids
Perfluorocarbon were developed as a blood substitute for their biologically inert nature and their property of transporting oxygen. The biologic compatibility led to their use as retinal tamponade. Chang et al. were first to study the use of Perfluorocarbon Liquids (PFCLs) in humans [36]. The use of PFCL in retinal surgeries became an important landmark to handle cases that were previously deemed inoperable.
7.1 Chemical and Physical Properties
Perfluorocarbon liquids are fully fluorinated synthetic analogues of hydrocarbons containing carbon–fluorine bonds. The straight-chain compounds C5 to C9 are liquids, as are most of the cyclic compounds ranging from C5 to C17. PFCLs are colourless and odourless and possess high density (1.6–2.1 specific gravity) and low viscosity (2–3 centistokes at 25 °C). PFCLs are biologically inert and stable at temperatures up to 400 °C.
PFCLs are optically clear compounds with variable refractive indices different from saline or water. This allows for easy visibility of PFCL in saline intraoperatively. The greater the difference between refractive index, more is the visibility at the interface. Perfluoro-n-octane has a more visible surface interface (refractive index 1.27 vs. 1.33 of water).
The high specific gravity as compared to water is helpful in settling detached retinas by pushing the sub-retinal fluid anteriorly and simultaneously flattening the retina. The tamponade force is higher as compared to silicon oil.
PFCLs have low surface tension and high interfacial tension. This property decreases the likelihood of sub-retinal migration of PFCL. Due to cohesive forces amongst PFCL molecules, it tends to remain in one single bubble. Also, the low viscosity of PFCL (0.8–8.03 centistokes at 25 °C) allows for easy injection and aspiration of fluid. The boiling point of PFCL is greater than water (400–500 °C).
7.2 Indications for Use of PFCL
Retinal Detachment with Proliferative Vitreo-Retinopathy
The high specific gravity of PFCL allows anterior displacement of sub-retinal fluid and avoids the need to create a posterior drainage retinotomy. This reduces iatrogenic retinal damage. The tamponade force of PFCL stabilizes the retina during membrane peeling. PFCLs are optically clear and do not absorb radiation at wavelengths used for laser. Photocoagulation can therefore be performed in the PFCL-flattened retina.
Giant Retinal Tear
PFCL has revolutionized the way giant retinal tears with retinal detachment are treated now. Before the introduction of PFCL, patients had to be kept in a prone position and intra-ocular gas was injected to unfold the giant retinal tear. With the use of PFCL, reattachment rates are up to 90%. PFCL has advantage of gentle manipulation of the retina to unfold the tear.
Dislocated Lens and IOLs
PFCL is an ideal tool to remove a spontaneous or traumatic dislocated nucleus, a posteriorly dislocated nucleus fragment or an intraocular lens after cataract extraction. A pars plana vitrectomy is performed, where all vitreous adhesions are freed from the lens or the intraocular lens. PFCL is injected beneath the lens, lens fragment, or IOL. This helps two purposes, first is to keep the lens afloat and second to prevent any damage to the retina by dropping or sudden posterior dislocation.
Ocular Trauma
PFCL is helpful in managing cases of traumatic retinal detachments which are complicated by vitreous hemorrhage, traumatic cataract and choroidal hemorrhage. During vitrectomy in cases of ocular trauma, there are high chances of iatrogenic tears due to poor visibility, especially if it is complicated with vitreous haemorrhage. PFCL is injected once the cortical vitreous is cleared. PFCL flattens the posterior retina, dissects through the posterior hyaloid and clears the vitreous haemorrhage from the posterior pole.
Intraocular foreign body may be associated with ocular trauma. Management of foreign bodies becomes easier with the use of PFCL. Foreign bodies with specific gravity less than PFCL such as wooden or plastic foreign bodies can be floated anteriorly and removed.
Sub-macular Haemorrhage
For removal of sub-retinal blood, one retinotomy is made near the edge of the bleed, which is away from fovea. PFCL is then injected on the posterior pole in one single bubble. PFCL gradually displaces the liquefied blood away from fovea, which is finally removed from the retinotomy site. A soft-tipped cannula can hasten this process.
PFCL as Tamponading Agent
Several studies have used PFCL as a short-, medium-, and long-term tamponade. The physical features of PFCLs make them excellent vitreous substitutes for dealing with inferior retinal pathology, where common tamponades with a density lower than water, like silicone oils or gases, are not so effective.
Use of PFCL as a tamponading agent for a short duration of 6–7 days does not appear to cause any toxic effects. The reattachment rate with PFCL is reported to be high, averaging between 76% and 82% with visual acuity improvement in 50–86% of cases [37,38,39,40]. The primary reattachment rates ranged between 86% and 92% with visual acuity improvement in 69% cases when PFCLs were used as a medium-term postoperative tamponade [41,42,43,44,45,46]. A typical granulomatous inflammatory reaction with precipitates was observed on the posterior lens capsule, retina, optic nerve head, or retinal blood vessels in 28% of patients. The inflammation started between 7 and 10 days after surgery and may impair posterior segment visualization. The inflammatory reaction did not correlate with final visual acuity, retinal attachment, PVR development, or persistently high intraocular pressure.
Few studies have described the use of PFCL for long-term tamponade [47, 48]. An inflammatory reaction develops as early as the third post-operative week in all cases. A white flocculent, flake-like material on various intraocular structures is found on various intraocular structures, such as the posterior lens capsule, the pars plana, the vitreous base, the optic nerve head, and the posterior retina. PFCL also disperses and migrates into the anterior chamber causing corneal endothelial damage.
Heavy silicone oil is an approved and safe tool for treating inferior pathology. Retinal toxicity of PFCL in humans has not been ruled by means of ERG or histological examination. Therefore, PFCL as a tamponading agent should be used with caution and must be removed completely as soon as possible once the retinopexy is complete. PFCL should not be used together with silicone oil as mixing can generate a new fluid known as sticky silicone oil [49].
7.3 Complications
Sub-retinal PFCL
Small bubbles of PFCL can easily migrate into the sub-retinal space through retinal breaks. To prevent the formation of small bubbles, one must inject PFCL slowly and submerge the tip of the cannula in the formed PFCL bubble to make one large bubble. If one injects PFCL rapidly without submerging the tip of the cannula in the formed PFCL bubble, numerous PFCL bubbles with a fish-egg appearance are easily formed. These bubbles should be removed before the surface of the PFCL reaches the height of the retinal tears. A large retinal break or large peripheral retinotomies are a risk factor for sub-retinal PFCL [50].
PFCL in the Anterior Chamber
Residual PFCL in the vitreous cavity may migrate into the anterior chamber post-operatively and cause visual disturbance, corneal endothelial loss, or elevation of intraocular pressure (Fig. 11.3). The effects of PFCL in the anterior chamber depends on the amount of PFCL. High volume of PFCL can cause endothelial damage by blocking its nutrition. Corneal decompensation with the replacement of endothelium with fibrotic tissue can occur 2 weeks after anterior chamber injection [51]. PFCL less than 0.25 mL appears to induce no damage to corneal endothelium but may cause changes in the trabecular meshwork [52].
Thus, if PFCL is found in the anterior chamber, it should be removed using a small-gauge needle at the slit lamp Also, surgeons should take care to remove PFCL completely from the vitreous cavity during vitrectomy.
Ocular Toxicity
PFCL cannot be left in vitreous cavity for extended period because of ocular toxicity. Extended use of PFCL as tamponade can cause both chemical and mechanical toxicity. It has been observed in animal models that high specific gravity of PFCL leads to mechanical toxicity due to compression of retina underlying it. PFCL can infiltrate the internal limiting membrane and penetrate deeper through the retinal layers involving the photoreceptor nuclear layer and the outer segment layer producing morphological changes. Atrophy and loss of outer plexiform layer and atrophy of retinal pigment epithelium have been reported. PFCL was not found beyond the Bruch’s membrane [53].
Chemical toxicity of PFCL is due to its polar impurities. These impurities cause adsorption of lipoproteins and proteins, causing fibroblastic reaction and formation of pre-retinal membranes. Some PFCLs like perfluorotributylamine have a higher tendency to give this reaction due to its amine group. Toxicity with Perfluoro-n-octane, a straight chain PFCL is the least as studied in rabbit models.
Effectiveness of Various Tamponading Agents
The silicone study was a randomized clinical trial comparing 1000 cSt silicone oil to 20% SF6 or 14% C3F8 in cases of RD with PVR. Better anatomic and visual outcomes were reported with silicone oil vs SF6 at 1 year. No significant differences in anatomic or visual outcomes were found between silicone oil and C3F8 [12, 13].
In a retrospective study comparing silicone oil vs C3F8 gas in the treatment of RD amongst highly myopic eyes with posterior staphyloma, C3F8 was associated with significantly better initial success rates and significantly better visual outcomes [54]. In another retrospective series of 56 eyes with recurrent RD associated with PVR and treated with PPV and retinectomy, silicone oil tamponade yielded significantly higher success rates than gas [55].
No significant differences in anatomical and visual success were noted between 1000 cSt and 5000 cSt silicone oil in a retrospective series of 325 eyes with complex RD [56]. Another retrospective series of 82 eyes with complex RDs reported that the use of 5000-cSt silicone oil was associated with a significantly higher rate of recurrent RD following silicone oil removal [57].
The HSO Study is an RCT comparing Densiron 68 with conventional silicone oil (either 1000 or 5000 cSt per surgeon preference) amongst patients with inferior RD associated with PVR. Forty-six patients treated with HSO were compared to 47 patients treated with standard silicone oil. The interim analysis of this study reported that, at 12 months, there were no significant differences in the anatomic success rates or visual outcomes between HSO tamponade and conventional silicone oil tamponade [58]. Neither non-inferiority nor superiority was shown with regard to final acuity.
In a case series of 12 patients, Densiron 68 was used as a primary endotamponade in patients with complex inferior retinal detachment, where standard procedures would have been unlikely to succeed. Only 4 of 12 patients (30%) showed a stable retinal re-attachment [35]. It seems that even a heavier-than-water tamponade cannot completely displace the PVR stimulating environment from the base of posterior staphyloma resulting in re-proliferation and renewing of tractional membranes.
In another case series, 49 patients affected by complex retinal re-detachment complicated with PVR were recruited. The mean follow-up was 7.6 months. The mean best-corrected visual acuity after Densiron 68 removal was 0.95 logMAR, standard error (SE: 0.068). Retinal reattachment rate was 61.2% after first surgery and 81.6% after second surgery. Nineteen cases (38.8%) had recurrences when intraocular heavy silicon oil was in situ [59].
8 Conclusion
Use of gas or silicone oil tamponade has led to favourable outcomes in patients with RD. PFCL is a good intraoperative tool for managing complicated scenarios effectively. Long-term use is restricted owing to its chemical and mechanical toxicity to the retina. HSO is best used in complex RD with PVR changes, especially inferior RD, which uses the physical property of high specific gravity of HSO.
References
Ohm J. Über die Behandlung der Netzhautablösung durch operative Entleerung der subretinalen Flüssigkeit und Einspritzung von Luft in den Glaskörper [On the treatment of retinal detachment by surgical evacuation of subretinal fluid and injection of air into the vitreous]. Albrecht Von Graefes Arch Für Ophthalmol. 1911;79(3):442–450 (in German).
Rosengren B. Results of treatment of detachment of the retina with diathermy and injection of air into the vitreous. Acta Ophthalmol. 1938;16(4):573–9.
Tan HS, Oberstein SYL, Mura M, Bijl HM. Air versus gas tamponade in retinal detachment surgery. Br J Ophthalmol. 2013;97:80–2.
Martínez-Castillo V, Verdugo A, Boixadera A, García-Arumí J, Corcóstegui B. Management of inferior breaks in pseudophakic rhegmatogenous retinal detachment with pars plana vitrectomy and air. Arch Ophthalmol. 2005;123:1078–81.
Mohamed S, Lai TY. Intraocular gas in vitreoretinal surgery. HK. J Ophthalmol. 2010;14(1):8–13.
Butler FK Jr. Diving and hyperbaric ophthalmology. Surv Ophthalmol. 1995;39:347–66.
Kanclerz P, Grzybowski A. Complications associated with the use of expandable gases in vitrectomy. J Ophthalmol. 2018;2018:8606494. https://doi.org/10.1155/2018/8606494.
Cibis PA, Becker B, Okun E, Canaan S. The use of liquid silicone in retinal detachment surgery. Arch Ophthalmol. 1962;68:590–9.
Crisp A, dejuan E Jr, Tiedeman J. Effect of silicone oil viscosity on emulsification. Arch Ophthalmol. 1987;105:546.
Saxena S, Gopal L. Fluid vitreous substitutes in vitreo retinal surgery. Curr Ophthalmol. 1996;44:191–206.
Scott IU, Flynn HW Jr, Murray TG, Smiddy WE, Davis JL, Feuer WJ. Outcomes of complex retinal detachment repair using 1000- versus 5000-centistoke silicone oil. Arch Ophthalmol. 2005;123(4):473–8.
Toklu Y, Cakmak HB, Ergun SB, Yorgun MA, Simsek S. Time course of silicone oil emulsification. Retina. 2012;32(10):2039–44.
Azen SP, Scott IU, Flynn HW Jr, et al. Silicone oil in the repair of complex retinal detachments: a prospective observational multicenter study. Ophthalmology. 1998;105(9):1587–97.
The Silicone Study Group. Vitrectomy with silicone oil or sulphur hexafluoride gas in eyes with severe proliferative vitreoretinopathy: results of a randomized clinical trial. Silicone study report 1. Arch Ophthalmol. 1992;110:770.
The Silicone Study Group. Vitrectomy with silicone oil or perfluoropropane gas in eyes with severe proliferative vitreoretinopathy: results of a randomized clinical trial. Silicone study report 2. Arch Ophthalmol. 1992;110:781.
The Silicone Study Group. Postoperative intraocular pressure abnormalities in the silicone study. Silicone study report 4. Ophthalmology. 1993;100:1629.
The Silicone Study Group. Relaxing retinotomy with silicone oil or long-acting gas in eyes with severe proliferative vitreoretinopathy. Silicone oil report 5. Am J Ophthalmol. 1993;116:557.
The Silicone Study Group. The incidence of corneal abnormalities in the silicone study. Arch Ophthalmol. 1995;113:764.
Brourman ND, Blumenkranz MS, Cox MS, et al. Silicone oil for treatment of severe proliferative diabetic retinopathy. Ophthalmology. 1989;96:759.
McCuen BW II, Rincoff JS. Silicone oil for progressive anterior ocular neovascularization after failed diabetic vitrectomy. Arch Ophthalmol. 1989;107:677.
De Juan E, Hardy M, Hatchell DL, et al. The effect of intraocular silicone oil on anterior chamber oxygen pressure in cats. Arch Ophthalmol. 1986;104:1063.
Rinkoff JS, de Juan E, McCuen BW II. Silicone oil for retinal detachment with advanced proliferative vitreoretinopathy following failed vitrectomy for proliferative diabetic retinopathy. Am J Ophthalmol. 1986;101:181.
Abrams GW, Azen SP, Barr CC, et al. The incidence of corneal abnormalities in the silicone study. Silicone study report 7. Arch Ophthalmol. 1995;113(6):764–9.
Al-Jazzaf AM, Netland PA, Charles S. Incidence and management of elevated intraocular pressure after silicone oil injection. J Glaucoma. 2005;14(1):40–6.
De Corral LR, Cohen SB, Peyman GA. Effect of intravitreal silicone oil on intraocular pressure. Ophthalmic Surg. 1987;18(6):446–9.
Honavar SG, Goyal M, Majji AB, et al. Glaucoma after pars plana vitrectomy and silicone oil injection for complicated retinal detachments. Ophthalmology. 1999;106(1):169–176, discussion 177.
Chung J, Spaide R. Intraretinal silicone oil vacuoles after macular hole surgery with internal limiting membrane peeling. Am J Ophthalmol. 2003;136(4):766–7.
Mrejen S, Sato T, Fisher Y, Spaide RF. Intraretinal and intra-optic nerve head silicone oil vacuoles using adaptive optics. Ophthalmic Surg Lasers Imaging Retina. 2014;45(1):71–3.
Jiang Y, Li X. The best timing of silicone oil removal. Zhonghua Yan Ke Za Zhi. 1997;33(1):39–41.
The Silicone Study Group. The effect of silicone oil removal. Silicone study report 6. Arch Ophthalmol. 1994;112:778.
Kim YK, Gunther B, Meinert H. A new, heavier-than-water silicone oil: a solution of perfluorohexyloctane in polydimethylsiloxane. Eur J Ophthalmol. 2019;15(5):627–37.
Prazeres J, Magalhães O Jr, Lucatto LF, Navarro RM, Moraes NS, Farah ME, Maia A, Maia M. Heavy silicone oil as a long-term endotamponade agent for complicated retinal detachments. Biomed Res Int. 2014;2014:136031.
Wong D, Williams R, Stappler T, Groenewald C. What pressure is exerted on the retina by heavy tamponade agents? Graefes Arch Clin Exp Ophthalmol. 2005;243(5):474–7.
Sandner D, Engelmann K. First experiences with high-density silicone oil (Densiron) as an intraocular tamponade in complex retinal detachment. Graefes Arch Clin Exp Ophthalmol. 2006;244(5):609–19.
Sandner D, Herbrig E, Engelmann K. High-density silicone oil (Densiron) as a primary intraocular tamponade: 12-month follow up. Graefes Arch Clin Exp Ophthalmol. 2007;245(8):1097–105.
Chang S, Ozmert E, Zimmerman NJ. Intraoperative perfluorocarbon liquids in the management of proliferative vitreoretinopathy. Am J Ophthalmol. 1988;106(6):668–74.
Drury B, Bourke RD. Short-term intraocular tamponade with perfluorocarbon heavy liquid. Br J Ophthalmol. 2011;95(5):694–8.
Suk KK, Flynn HW Jr. Management options for submacular perfluorocarbon liquid. Ophthalmic Surg Lasers Imaging. 2011;42(4):284–91.
Velikay M, Stolba U, Wedrich A, Li Y, Datlinger P, Binder S. The effect of chemical stability and purification of perfluorocarbon liquids in experimental extended-term vitreous substitution. Graefes Arch Clin Exp Ophthalmol. 1995;233(1):26–30.
Sirimaharaj M, Balachandran C, Chan WC, et al. Vitrectomy with short term postoperative tamponade using perfluorocarbon liquid for giant retinal tears. Br J Ophthalmol. 2005;89(9):1176–9.
Sigler EJ, Randolph JC, Calzada JI, Charles S. 25-gauge pars plana vitrectomy with medium-term postoperative perfluorotamponade for inferior retinal detachment. Ophthalmic Surg Lasers Imaging Retina. 2013;44:34–40.
Sigler EJ, Randolph JC, Calzada JI, Charles S. Pars plana vitrectomy with medium-term postoperative perfluoro-n-octane for recurrent inferior retinal detachment complicated with advanced proliferative vitreoretinopathy. Retina. 2013;33:791–7.
Sigler EJ, Randolph JC, Charles S. Foreign body response within postoperative perfluoro-n-octane for retinal detachment repair. Retina. 2014;34(2):237–46.
Rofail M, Lee LR. Perfluoro-n-octane as a postoperative vitreoretinal tamponade in the management of giant retinal tears. Retina. 2005;25(7):897–901.
Rush R, Sheth S, Surka S, Ho I, Gregory-Roberts J. Postoperative perfluoro-n-octane tamponade for primary retinal detachment repair. Retina. 2012;32:1114–20.
Singh J, Ramaesh K, Wharton SB, Cormack G, Chawla HB. Perfluorodecalin-induced intravitreal inflammation. Retina. 2001;21(3):247–51.
Kirchhof B, Wong D, van Meurs J, et al. Use of perfluorohexyloctane as a long-term internal tamponade agent in complicated retinal detachment surgery. Am J Ophthalmol. 2002;133(1):95–101.
Kertes PJ, Wafapoor H, Peyman GA, Calixto N Jr, Thompson H. The management of giant retinal tears using perfluoroperhydrophenanthrene. A multicenter case series. Vitreon collaborative study group. Ophthalmology. 1997;104(7):1159–65.
Romano MR, Vallejo-Garcia JL, Parmeggiani F, Vito R, Vinciguerra P. Interaction between perfluorcarbon liquid and heavy silicone oil: risk factor for “sticky oil” formation. Curr Eye Res. 2014;32(2):212.
Garcia-Valenzuela E, Ito Y, Abrams GW. Risk factors for retention of subretinal perfluorocarbon liquid in vitreoretinal surgery. Retina. 2004;24(5):746–52.
Stolba U, Krepler K, Velikay M, Binder S. Anterior segment changes in rabbits after experimental aqueous replacement with various amounts of different perfluorocarbon liquids. Graefes Arch Clin Exp Ophthalmol. 1999;237(6):501–7.
Moreira H, de Queiroz JM Jr, Liggett PE, McDonnell PJ. Corneal toxicity study of two perfluorocarbon liquids in rabbit eyes. Cornea. 1992;11(5):376–9.
Figueroa MS, Casas DR. Inflammation induced by perfluorocarbon liquid: intra- and postoperative use. Biomed Res Int. 2014;2014:907816. https://doi.org/10.1155/2014/907816.
Mancino R, Ciuffoletti E, Martucci A, et al. Anatomical and functional results of macular hole retinal detachment surgery in patients with high myopia and posterior staphyloma treated with perfluoropropane gas or silicone oil. Retina. 2013;33:586–92.
Quiram PA, Gonzales CR, Hu W, et al. Outcomes of vitrectomy with inferior retinectomy in patients with recurrent rhegmatogenous retinal detachments and proliferative vitreoretinopathy. Ophthalmology. 2006;113:2041–7.
Scott IU, Flynn HW Jr, Murray TG, Smiddy WE, Davis JL, Feuer WJ. Outcomes of complex retinal detachment repair using 1000- vs 5000-centistoke silicone oil. Arch Ophthalmol. 2005;123:473–8.
Soheilian M, Mazareei M, Mohammadpour M, Rahmani B. Comparison of silicon oil removal with various viscosities after complex retinal detachment surgery. BMC Ophthalmol. 2006;6:21.
Joussen AM, Rizzo S, Kirchhof B, Schrage N, Li X, Lente C, et al. Heavy silicone oil versus standard silicone oil in as vitreous tamponade in inferior PVR (HSO Study): interim analysis. Acta Ophthalmol. 2011;89(6):e483–9.
Caporossi T, Franco F, Finocchio L, Barca F, Giansanti F, Tartaro R, et al. Densiron 68 heavy silicone oil in the management of inferior retinal detachment recurrence: analysis on functional and anatomical outcomes and complications. Int J Ophthalmol. 2019;12(4):615–20.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Jain, A., MB, T., Singh, J. (2021). Tamponading Agents in Vitreoretinal Surgery. In: Jain, A., Natarajan, S., Saxena, S. (eds) Cutting-edge Vitreoretinal Surgery. Springer, Singapore. https://doi.org/10.1007/978-981-33-4168-5_11
Download citation
DOI: https://doi.org/10.1007/978-981-33-4168-5_11
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-33-4167-8
Online ISBN: 978-981-33-4168-5
eBook Packages: MedicineMedicine (R0)