Abstract
Biofilms are structured communities of microorganisms which are encased within a self-produced matrix attached to surface of abiotic or biotic. There is growing evidence that bacterial biofilms play a major lead in a range of ocular infections. The presence of biofilms has been established on most indwelling ophthalmic devices such as intraocular lenses, scleral buckles, contact lenses and suture materials. Lack of poor lens hygiene leads to infections of soft lenses that are at high risk than other types of lenses. Pseudomonas spp. is gram-negative bacteria predominant on contact lenses. Serratia spp. and Staphylococcus spp. are the next dominant microorganisms in the eye. The biofilm of these organisms led to activation of various signalling cascades which cause permanent vision loss in humans. The strategy of preventing the microbial attachment and biofilm formation by utilizing single-cell repellent surfaces is the ideal choice. Natural and man-made anti-biofilm compounds have previously been discovered to address this problem. There is a large requirement for improvement of anti-biofilm formulations to control the post-surgery eye medical devices. The organoselenium polypropylene is the one which demonstrates the capacity to decrease biofilm formation. The utilization of organoselenium copolymer assumes an indispensable job in securing against contact focal point. Nisin polypropylene material showed to stop the biofilm formation of S. epidermidis. The review emphasizes on biofilm formation on ophthalmic devices and advanced developments in the anti-biofilm materials for better vision.
All authors contributed equally
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Most of the bacterial infections involve biofilms. Cluster of microorganisms that manufacture biofilms are found to be connected with the biotic and abiotic surfaces. Biofilms are single or multilayered (Karatan and Watnick 2009) and contain either consistent or heterogeneous populations of microorganism. These stay inside the framework of extracellular polymeric substances discharged by constituent populace of biofilms. They exhibit amazingly complicated multicellular behaviours that are coordinated by cell-to-cell signalling networks. Biofilms are an expanding issue of worry that is picking up significance as time passes. Biofilms also appear on therapeutic gadget surfaces, and spread of single and grouped cells suggests a tremendous danger of microorganism scattering among the host and intensified danger of contamination. Organisms within a biofilms are problematic to kill by conventional antimicrobial medical aid and might cause indolent infections. This chapter reviews the biofilm formation on varied ophthalmic devices, their role within the disease process and prevention ways.
The primary portrayal initiated by van Leeuwenhoek on restorative microbial biofilms outlined perceptions made on dental plaque. By observant that he may solely kill tiny proportion of the microorganisms adhering to his teeth, attributable to acknowledge natural resistance of microorganism during an exposure of a biocide, ethanoic acid (Hall-Stoodley et al. 2004). In fact, it took three additional centuries for Koch to explain the scientific theory for disease. The frequency of infections caused by biofilms has been thought to be from 65% to 80%. It has taken an additional century for the restorative significance of biofilms to be perceived in spite of its measurable contribution over 80% of bacterial contamination (Health 2007, November 12). Furthermore, the ibofilm examination procedures such as microwell plate assay, Calgary Device, confocal laser scanning microscopy, Bioflux device and atomic force microscopy have become progressively common in medicinal research (Berger et al. 2018).
2 Indwelling Devices and Biofilm Infections
One of the essential clinical diseases identified with biofilm formation was therapeutic device-related contaminations. Medical device-related infections create an enormous monetary burden on care services and are related to accrued patient morbidity and mortality (Donlan 2008). Healthcare-related diseases will happen in consideration homes, clinics or in a patient’s home (van Kleef et al. 2013), with a predominance dimension of 6.4% and 1,000,000 cases detailed each year (HPA 2011). Among one million cases reported, an expected 60% of emergency clinic-related contaminations are due to biofilms that have formed on inhabiting devices (Darouiche 2004). Ophthalmic device-associated biofilm diseases in emergency clinic remain, by and large, a few days (Archibald and Gaynes 1997). Attributable to the maturing populace and the expanding assortment of implantable medical devices, contamination related to biofilms is feared to broaden. Many of the medical devices are contaminated with different types of biofilms (Marrie et al. 1982; Gristina and Costerton 1984, 1985; Webb et al. 1986). The occurrence of bacterial biofilms has been reported on several therapeutic devices such as intrauterine devices, prosthetic heart valves, urinary catheters, neurosurgical ventricular shunts, ventricular assist devices, intravascular catheters, prosthetic joint, coronary stents, cochlear implants and intraocular and contact lenses (Donlan and Costerton 2002; Bispo et al. 2015) (Fig. 11.1).
Biofilms on indwelling medical devices could be made out of gram-positive or gram-negative microorganisms or yeasts. Microbes usually detached from these devices include gram-positive Staphylococcus epidermidis, Enterococcus faecalis, Staphylococcus aureus and Streptococcus viridans, and the gram-negative Klebsiella pneumoniae, Escherichia coli, Proteus mirabilis and Pseudomonas aeruginosa. This biofilms arrangement might be analysed by electron microscopy when upgraded by recolouring with ruthenium red (Springer and Roth 1973).
Table 11.1 represents the most common ocular-associated infections in human.
3 Factors Influencing Biofilm Formation on Ophthalmic Devices
Biofilm formation on indwelling therapeutic devices can be determined by several variables (biotic and abiotic factors). Biofilm arrangement is a multistep procedure and adhesion to ophthalmic gadgets varies between different genera/species/strains of microscopic organisms. Microorganisms ought to adhere to the exposed surfaces of the device sufficiently long to turn out to be irreversibly snared. The rate of cell connection relies upon the sum and sorts of cells inside the fluid from which the gadget is uncovered, the progression of fluid through the gadget, and the physicochemical qualities of the surface. Segments in the fluid could adjust the surface properties and conjointly affect the rate of connection.
Once these cells irreversibly connect and fabricate extracellular polysaccharides to build up a biofilm, rate of development is affected by stream, surrounding temperature, and supplement creation of the medium and antimicrobial-medicate fixation. Common abiotic variables include pH scale, salt fixation, temperature, dampness, supplement availability, anti-microbial impacts and heavy metals (Fig. 11.2).
4 Biofilm Formation in Ophthalmological Devices
Biofilm formation on ophthalmic devices leads to various kinds of diseases like endophthalmitis, contact lens-associated keratitis and infectious crystalline keratopathy in humans. Many prosthetic device-associated ocular infections due to biofilm formation on biotic or abiotic materials fastened within the eye together with conjunctival infection and corrosion related to scleral buckles, endophthalmitis involving biofilms on intraocular lenses, keratoprosthesis and glaucoma drain implants and infectious crystalline keratopathy are reported (Zegans et al. 2005; Juarez-Verdayes et al. 2006; Ibanez et al. 2011).
5 Endophthalmitis
Plethora of reports state that clinical endophthalmitis treatment after cataract surgery is due to microorganisms intruding the site during surgery (Speaker et al. 1991; Sunderraj 1992). Staphylococcus epidermidis gram-positive bacteria conjure 76%–90% of the culture-positive cases of pseudo-endophthalmitis (Puliafito et al. 1982; Dickey et al. 1991). Improper handling of the surgical instruments can lead to rapid progression of the disease, which can cause an inflammation of the interior of the eye. Especially, cataract surgery and intraocular surgery with possible loss of vision and the eye itself are possible complications. Microorganisms adhere well to intraocular lenses due to electrostatic forces. During cataract surgery, simply wiping a lens around the wound will cause 26.7% of lenses to have viable organisms attached (Fisch et al. 1991).
Post-cataract endophthalmitis is primarily caused by gram-positive organisms from the microbiota of the eye surface. It is notable that Coagulase-negative Staphylococci (CoNS), especially epidermidis is caused by Staphylococcus (Benz et al. 2004; Schimel et al. 2013). Perhaps, there are two remedies available to manage endophthalmitis, and there is no single antibiotic treatment for all of the microbes isolated from eyes with endophthalmitis, and hence a combination of medical care is mostly counselled (Schimel et al. 2013). Hydrophobicity is consistently found to be a very important determinant of biofilm formation in different studies. Changing the surface to make it more hydrophilic may reduce early binding and robust staphylococcal biofilm development.
6 Contact Lens-Associated Keratitis
For patients, eye care practitioners and the contact lens industry, sight-threatening microbial keratitis associated with contact lens wear remains a serious concern. The use of contact lenses represents the most risk issue in developed countries for the event of microbial keratitis. Estimates of microbial keratitis in the United States suggested more than 30,000 cases annually (Pepose and Wilhelmus 1992). The incidence of contact lens-associated microbial keratitis has been shown to be impacted by the material of contact lens and conjointly by the damage schedule. Early epidemiological studies show a higher risk for the daily wear of soft contact lenses compared to the daily wear of rigid gas-permeable lenses (Cheng et al. 1999), and this risk was found higher for overnight wear soft contact lenses (Dart et al. 1991). Recently, a case-control study reported that silicone polymer hydrogel contact focal points and day-by-day expendable focal points were related with a higher rate of keratitis (Dart et al. 2008).
The increased threat of microbial keratitis in the contact lens is due to the lens that induces changes in the corneal epithelium that facilitate the movement of the organism to the ocular surface that would otherwise not be found during this niche and the limitation of natural clearance mechanisms (Fleiszig and Evans 2010; Willcox et al. 2010). There are two ways to infect the cornea and lead to keratitis with these contact lenses. One is the close interaction between the lens and the corneal epithelium that induces local changes, including hypercapnia and hypoxia, affecting the epithelium’s ability to react to damage. This could result in compromising the exchange of tear fluids between the anterior and posterior sides of the lens, neutralizing the tear fluid’s composition on the eye surface and limiting its antimicrobial properties (Fleiszig and Evans 2010; Willcox et al. 2010). However, the second approach provides a surface where microorganisms can fix and settle the surface as a biofilm, a source for microorganisms to develop into a previously damaged corneal epithelium (Willcox et al. 2010) (Fig. 11.3).
The capacity of microorganisms to stick to completely different contact lens materials has been established in vitro (Dutta et al. 2012) and is especially driven by surface hydrophobicity (Klotz et al. 1989; Bruinsma et al. 2001). P. aeruginosa, S. aureus and coagulase-negative Staphylococci (Tabbara et al. 2000) are three microorganisms predominant on contact lenses. It is a notable fact that, P. aeruginosa can easily stick to contact lenses, among any microorganisms tested so far, and this is presumably a reason that it is the most principal microbe that causes contact lens-associated keratitis (Hahn 1997). This bacterium produces many surface-associated adherence factors (adhesions) that promote epithelial cell attachment and contribute to the pathogen’s virulence.
7 Scleral Buckle-Associated Infections
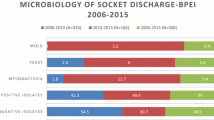
Scleral buckles are used in rhegmatogenic retinal detachments, where they are placed between the conjunctive and the sclera. Gram-positive cocci, especially coagulase-negative staphylococci, and nontuberculous mycobacterium often cause scleral buckle-associated infections (Smiddy et al. 1993; Pathengay et al. 2004). The presence of a biofilm within the explanted material was supposed to play a vital role in its pathogenesis due to the chronic evolution of this infection. From these buckle parts, more frequently gram-positive bacteria, and less frequently Mycobacterium chelonae and Proteus mirabilis, are found to grow (Holland et al. 1991). Scleral buckle infections tend to be relentless furthermore by being immune to antimicrobial treatment. Often, scleral buckle infections need exclusion of the buckling parts for resolution. Due to conjunctival erosion and infection, buckle materials are kept away from patients. The mechanism by which bacteria can persist and withstand antimicrobial treatment could also be the development of biofilms on scleral buckles. This mechanism would also describe the need to remove an infected buckle for infection resolution (Holland et al. 1991).
8 Orbital Implants and Lacrimal Intubation Devices
Lacrimal cannulation devices together with lacrimal stents and Jones tubes are normally utilized during the dacryocystorhinostomy practice to treat nasolacrimal duct obstruction (NLDO), a general cause of epiphora (Eisenbeis et al. 2011; Bispo et al. 2015). As for alternative biomaterials fixed in the eyes, Jones tube as well as lacrimal stents could offer biofilm formation with an exterior. The bacterial biofilm formation on nasolacrimal stents could lead to prosthetic failure by occluding the stent (Ibanez et al. 2011). Bacterial colonization of the outer and inner surfaces of lacrimal stents was reported in some studies (Parsa et al. 2010) (Fig. 11.4).
The incidence of a polymicrobial biofilm was demonstrated by the evaluation of both Jones tube and silicone stent by scanning microscopy. Curiously, in the silicone stent biofilms, the authors have identified a variety of cell morphologies including fusiforms, short rod, cocci and spirochetes. Analysis of the interior surfaces of the silicone stent by confocal laser scanning microscopy unconcealed the presence of viable biofilms on the tube (Parsa et al. 2010). Biofilm formation on these polyurethane nasolacrimal stents has been connected with delayed failure of the device (Ibanez et al. 2011).
9 Conjunctival Plugs
Punctal plugs are used for the management of tear-deficient-kind dry eye. Conjunctival plugs are manufactured from hydrophobic acrylic, silicone, hydrogel and collagen. However, secondary complications might take place following implantation, including dacryocystitis, canaliculitis and acute conjunctivitis (Yokoi et al. 2000; Bourkiza and Lee 2012). Punctal plugs are usually used to treat dryness of the eye surface that does not respond to topical medication by occluding lacrimal ducts and blocking emptying of tears. It is vital that patients with punctal plugs are carefully observed. Examination of punctal aloof plugs from patients without clinical signs of infection revealed the presence of biofilms from microorganisms in 53% of the samples (Sugita et al. 2001). With regard to infection, many patients were asymptomatic, and the causal association between biofilms growing on punctal plugs and progress toward eye infection remains speculative. One case of conjunctivitis was associated with the formation of biofilm on a punctal plug (Yokoi et al. 2000). S. haemolyticus and Candida tropicalis are commonly growing biofilms on punctal plugs.
10 Outlook on Biofilm Prevention and Treatment Agents
Because biofilms are recognized for their great medical significance, efforts have been made to either stop their formation or get rid of them once they have been formed. There is a keen interest in ophthalmic materials capable of killing harmful microorganisms due to ever-increasing demand for healthy living. There are a few strategies to eradicate this biofilms on ophthalmic devices, which include preventing bacterial colonization on medical device surfaces by covalently attaching biocidal molecules and slowly releasing numerous antibiotics or modifying the external topology that may interfere with microbial adhesion.
The first two approaches would be much easier to achieve because they depend primarily on the coating of current ocular devices with obtainable biocidal molecules; the last is also more difficult because changes in the material topology could alter its optical clarity. Many medical procedures are currently used to treat device-related infections, including long-term antimicrobial strategies and antibiotic combinations and surgical revision. Unfortunately, these interventions carry the risk of re-infection and the development of antibiotic resistance, often at a higher rate. However, the application of non-adhesive and antimicrobial coatings has been researched and clinically tested as an alternative approach.
11 Investigational Strategies
There are some that have bactericidal potential and some that have adjunctive therapy potential among research strategies to control biofilms.
12 Biocidal Molecules or Inhibitors
The key to developing improved biomedical materials and devices, including infection-resistant medical implants, is effective management of biointerfacial interactions. Several of the medical devices are created from normal materials and do not seem to be antimicrobial, in order that they need modification. For example, device surfaces with modified chemicals such as polyethylene glycol and some other synthetic polymers are reported to repel (not kill) microorganisms (Ackart et al. 1975; Bridgett et al. 1992; Desai et al. 1992). These films were investigated for their resistance to bacterial adhesion. Alternatively, materials are often impregnated with antimicrobials, such as biocidal molecules, quaternary ammonium compounds, silver ions or iodine, which are slowly released into the surrounding solution over time and kill microorganisms (Fig. 11.5).
Graft polymers can be established through the grafting-to technique (a), where pre-formed polymers are surface immobilized in a reaction between complementary functional groups. Grafting-from method (b) uses surface-immobilized initiators or chain transfer agents in a monomer solution that results in covalently immobilized graft polymer. Grafting-assisted materials (c)
The adhesion and colonization mechanism of bacteria on biomaterial surfaces are not fully understood; the influence of absorbable proteins was investigated. Biocidal compounds like polyethylene oxide (PEO) on the surfaces of polymeric biomaterials had shown larger protection from biofilm formation (Desai and Hubbell 1991). For instance, Desai et al. showed that incorporation of polyvinylpyrrolidone and polyethyl oxazoline on the surfaces of commonly used biomedical polymers, for example polyurethane, would provide a wide protection from various microorganisms’ adherence.
Therefore, as an example for the prevention of biocides from the exploitation of surface colonization, a hundredfold reduction in cell counts when S. aureus is undisputed in previous studies. S. aureus, E. coli and P. aeruginosa were sprayed on glass slides covered with covalently fastened poly(4-vinyl-N-alkylpyridinium bromide) or N-hexylated polymer (Tiller et al. 2001). Inhibitory effects of 2,2′-dipyridyl and 1,2,3,4,6-penta-O-galloyl-b-D-glucopyranose in the contact lens on S. aureus were evidenced (Cho et al. 2015).
Antimicrobial peptides (AMPs) are another strategy for eradicating bacteria that form biofilms. AMPs’ mechanism of action varies and involves disrupting bacterial cell membranes by creating hydrophilic channels, destabilizing the lipid bilayer and even changing membrane curvature. These mechanisms lead to penetration and death of bacterial cells. Quorum sensing (QS) is a form of chemical cell-to-cell communication used by microbes for cell-density-dependent signal transmission (Miller and Bassler 2001). Development of a peptide antagonist against fsr QS of E. faecalis derivatives would be useful to control the biofilm formation (Nakayama et al. 2013).
13 Antibiotic Molecules
When biofilms form after medical devices have been implanted, they carry the risk of device infection and may result in the patient suffering worse after treatment than before receiving medical treatment (Darouiche 2001). Bacterial colonization of the inward device may lead to both infection and failure of the device. Consistent with one study reported, surface coatings which will slowly discharge antibiotics, such as clarithromycin, rifampin and doxycycline, were capable of averting biofilm formation for up to 3 weeks (Rose et al. 2015). The intraocular lens designed to release norfloxacin was tested in rabbit model and in vitro to stop postoperative bacterial (Garty et al. 2011). Antimicrobial peptides coating on metal titanium have additionally been used fruitfully to prevent biofilm development and have the superimposed advantage that they are active against antibiotic-resistant strains (Kazemzadeh-Narbat et al. 2013). Gallium nitrate or silver also showed potential impact which will forestall the formation of biofilms. The advantages of visual exploitation systems that slowly unleash antimicrobial agents are that a number of regularly used ophthalmology antibiotics already have toxicity, penetration, and half-life. On the contrary, long exposure to these drugs could favour the selection of spontaneous resistant mutants and disturb the microbiome of the eye surface (Fig. 11.6).
14 Modifying the Exterior Topology of Ophthalmic Devices
Changes within the ophthalmic device material topology may change its optical clarity. It is always a pretty approach to change the external structure of eye devices to make it less adhesive for bacteria making an attempt to colonize. This would potentially eradicate the requirement for coating with biocide or antimicrobial agents that would be reserved for treatment and perioperative prophylaxis. Some polymers, such as dextran, polyacrylamide and polyethylene glycol, can form star-shaped, linear, and ‘bottle brush’ external nanostructures that impede the ability of the microbe to adhere to the substrate (May et al. 2014; Salwiczek et al. 2014).
In addition, nanotubes, nanopores and nanopillars made of anodized aluminium, polymethylmethacrylate and titanium dioxide were found to reduce microbial adhesion to coated surfaces (Desrousseaux et al. 2013).
15 ECM Degrading Enzymes
Synthetic biology involves engineering biological organisms through modular and generalizable victimization standard designs with the ultimate goal of developing useful solutions to real-world problems. To control the formation of biofilms on medical devices, few scientists are currently engaged in the extracellular matrix (ECM)-degrading enzymes. This can be an alternative strategy for microbial biofilm removal to stimulate microbial reversal to planktonic physiology. While the enzymes that degrade the ECM or the substratum can cost a clinical price, small signalling molecules that cause the expression of factors that stimulate biofilm dissimulation can be a viable alternative (Bispo et al. 2015). The use of phage endolysins as well as engineered phages expressing antibiofilm enzymes can also be promising choices in the site of infection for the eradication of bacterial biofilms (Lu and Collins 2007). Some cell signals, such as PQS, AI-2, C4HSL and AIP-I or their derivatives, are also of great therapeutic value (Dong et al. 2008; Kaplan 2010).
16 Conclusions and Future Directions
Since early descriptions quite three decades ago, our understanding of the formation and development of biofilms has advanced considerably. As medical interventions rely gradually on medical devices and prosthetic devices, a very important constraint is the requirement to prevent, decrease or eliminate microbial biofilms. Contact lenses and intraocular lenses have had an excellent impact on the restoration and recovery of vision within the field of eye care; however, eye infection prohibits their use. Strategies such as developing biofilm-active therapies and anti-biofilm surface coatings and improving surface topology to stop microbe adhesion are exciting avenues for future understanding to reduce the risk of visual infection associated with biofilm.
References
Ackart WB, Camp RL et al (1975) Antimicrobial polymers. J Biomed Mater Res 9(1):55–68
Archibald LK, Gaynes RP (1997) Hospital-acquired infections in the United States: the importance of inter-hospital comparisons. Infect Dis Clin North Am 11(2):245–255
Benz MS, Scott IU et al (2004) Endophthalmitis isolates and antibiotic sensitivities: a 6-year review of culture-proven cases. Am J Ophthalmol 137(1):38–42
Berger D, Rakhamimova A et al (2018) Oral biofilms: development, control, and analysis. High Throughput 7(3)
Bispo PJ, Haas W et al (2015) Biofilms in infections of the eye. Pathogens 4(1):111–136
Bourkiza R, Lee V (2012) A review of the complications of lacrimal occlusion with punctal and canalicular plugs. Orbit 31(2):86–93
Bridgett MJ, Davies MC et al (1992) Control of staphylococcal adhesion to polystyrene surfaces by polymer surface modification with surfactants. Biomaterials13(7):411–416
Bruinsma GM, van der Mei HC et al (2001) Bacterial adhesion to surface hydrophilic and hydrophobic contact lenses. Biomaterials 22(24): 3217–3224
Cheng KH, Leung SL et al (1999) Incidence of contact-lens-associated microbial keratitis and its related morbidity. Lancet 354(9174):181–185
Cho P, Shi GS et al (2015) Inhibitory effects of 2,2′-Dipyridyl and 1,2,3,4,6-Penta-O-Galloyl-b-D-Glucopyranose on biofilm formation in contact lens cases. Invest Ophthalmol Vis Sci 56(12):7053–7057
Darouiche RO (2001) Device-associated infections: a macroproblem that starts with microadherence. Clin Infect Dis 33(9):1567–1572
Darouiche RO (2004) Treatment of infections associated with surgical implants. N Engl J Med 350(14):1422–1429
Dart JK, Stapleton F et al (1991) Contact lenses and other risk factors in microbial keratitis. Lancet 338(8768):650–653
Dart JK, Radford CF et al (2008) Risk factors for microbial keratitis with contemporary contact lenses: a case-control study. Ophthalmology 115(10):1647–1654, 1654 e1–3
Desai NP, Hubbell JA (1991) Solution technique to incorporate polyethylene oxide and other water-soluble polymers into surfaces of polymeric biomaterials. Biomaterials 12(2):144–153
Desai NP, Hossainy SF et al (1992) Surface-immobilized polyethylene oxide for bacterial repellence. Biomaterials 13(7):417–420
Desrousseaux C, Sautou V et al (2013) Modification of the surfaces of medical devices to prevent microbial adhesion and biofilm formation. J Hosp Infect 85(2):87–93
Dickey JB, Thompson KD et al (1991) Anterior chamber aspirate cultures after uncomplicated cataract surgery. Am J Ophthalmol 112(3):278–282
Dong YH, Zhang XF et al (2008) A novel two-component system BqsS-BqsR modulates quorum sensing-dependent biofilm decay in Pseudomonas aeruginosa. Commun Integr Biol 1(1):88–96
Donlan RM (2008) Biofilms on central venous catheters: is eradication possible? Curr Top Microbiol Immunol 322:133–161
Donlan RM, Costerton JW (2002) Biofilms: survival mechanisms of clinically relevant microorganisms. Clin Microbiol Rev 15(2):167–193
Dutta D, Cole N et al (2012) Factors influencing bacterial adhesion to contact lenses. Mol Vis 18:14–21
Eisenbeis C, Neppert B et al (2011) Anatomic and subjective success of structured surgical treatment strategy in the management of chronic epiphora – a postoperative analysis of contentment. Klin Monatsbl Augenheilkd 227(11):879–886
Fisch A, Salvanet A et al (1991) Epidemiology of infective endophthalmitis in France. The French collaborative study group on endophthalmitis. Lancet 338(8779):1373–1376
Fleiszig SM, Evans DJ (2010) Pathogenesis of contact lens-associated microbial keratitis. Optom Vis Sci 87(4):225–232
Garty S, Shirakawa R et al (2011) Sustained antibiotic release from an intraocular lens-hydrogel assembly for cataract surgery. Invest Ophthalmol Vis Sci 52(9):6109–6116
Gristina AG, Costerton JW (1984) Bacteria-laden biofilms: a hazard to orthopaedic prostheses. Infect Surg 67A:264–273
Gristina AG, Costerton JW (1985) Bacterial adherence to biomaterials and tissue. J Bone Joint Surg Am 67(264–73):264
Hahn HP (1997) The type-4 pilus is the major virulence-associated adhesin of Pseudomonas aeruginosa--a review. Gene 192(1):99–108
Hall-Stoodley L, Costerton JW et al (2004) Bacterial biofilms: from the natural environment to infectious diseases. Nat Rev Microbiol 2(2):95–108
Health NIO (2007, November 12). Targeted research on oral microbial biofilms (DE98-006). http://grants.nih.gov/grants/guide/rfa-files/RFA-DE-98-006.html
Holland SP, Pulido JS et al (1991) Biofilm and scleral buckle-associated infections. A mechanism for persistence. Ophthalmology 98(6):933–938
HPA (2011) English national point prevalence survey on health care associated infections and antimicrobial use. Preliminary Data. Health Protection Agency, London
Ibanez A, Trinidad A et al (2011) Biofilm colonisation in nasolacrimal stents. B-ENT 7(1):7–10
Juarez-Verdayes MA, Reyes-Lopez MA et al (2006) Isolation, vancomycin resistance and biofilm production of Staphylococcus epidermidis from patients with conjunctivitis, corneal ulcers, and endophthalmitis. Rev Latinoam Microbiol 48(3–4):238–246
Kaplan JB (2010) Biofilm dispersal: mechanisms, clinical implications, and potential therapeutic uses. J Dent Res 89(3):205–218
Karatan E, Watnick P (2009) Signals, regulatory networks, and materials that build and break bacterial biofilms. Microbiol Mol Biol 73(2):310–347
Kazemzadeh-Narbat M, Lai BF et al (2013) Multilayered coating on titanium for controlled release of antimicrobial peptides for the prevention of implant-associated infections. Biomaterials 34(24):5969–5977
Klotz SA, Butrus SI et al (1989) The contribution of bacterial surface hydrophobicity to the process of adherence of Pseudomonas aeruginosa to hydrophilic contact lenses. Curr Eye Res 8(2):195–202
Lu TK, Collins JJ (2007) Dispersing biofilms with engineered enzymatic bacteriophage. Proc Natl Acad Sci U S A 104(27):11197–11202
Marrie TJ, Nelligan J, Costerton JW (1982) A scanning and transmission electron microscopic study of an infected endocardial pacemaker lead. Circulation 66:1339–1343
May RM, Hoffman MG et al (2014) Micro-patterned surfaces reduce bacterial colonization and biofilm formation in vitro: potential for enhancing endotracheal tube designs. Clin Transl Med 3:8
Miller MB, Bassler BL (2001) Quorum sensing in bacteria. Annu Rev Microbiol 55:165–199
Nakayama J, Yokohata R et al (2013) Development of a peptide antagonist against fsr quorum sensing of Enterococcus faecalis. ACS Chem Biol 8(4):804–811
Parsa K, Schaudinn C et al (2010) Demonstration of bacterial biofilms in culture-negative silicone stent and jones tube. Ophthal Plast Reconstr Surg 26(6):426–430
Pathengay A, Karosekar S et al (2004) Microbiologic spectrum and susceptibility of isolates in scleral buckle infection in India. Am J Ophthalmol 138(4):663–664
Pepose JS, Wilhelmus KR (1992) Divergent approaches to the management of corneal ulcers. Am J Ophthalmol 114(5):630–632
Puliafito CA, Baker AS et al (1982) Infectious endophthalmitis. Review of 36 cases. Ophthalmology 89(8):921–929
Rose WE, Otto DP et al (2015) Prevention of biofilm formation by methacrylate-based copolymer films loaded with rifampin, clarithromycin, doxycycline alone or in combination. Pharm Res 32(1):61–73
Salwiczek M, Qu Y et al (2014) Emerging rules for effective antimicrobial coatings. Trends Biotechnol 32(2):82–90
Schimel AM, Miller D et al (2013) Endophthalmitis isolates and antibiotic susceptibilities: a 10-year review of culture-proven cases. Am J Ophthalmol 156(1):50–52. e1
Smiddy WE, Miller D et al (1993) Scleral buckle removal following retinal reattachment surgery: clinical and microbiologic aspects. Ophthalmic Surg 24(7):440–445
Speaker MG, Milch FA et al (1991) Role of external bacterial flora in the pathogenesis of acute postoperative endophthalmitis. Ophthalmology 98(5):639–649; discussion 650
Springer EL, Roth IL (1973) The ultrastructure of the capsules of Diplococcus pneumoniae and Klebsiella pneumoniae stained with ruthenium red. J Gen Microbiol 74(1):21–31
Sugita J, Yokoi N et al (2001) The detection of bacteria and bacterial biofilms in punctal plug holes. Cornea 20(4):362–365
Sunderraj, P. (1992). "Anterior chamber aspirate cultures after uncomplicated cataract surgery." Am J Ophthalmol 113(2): 221–2
Tabbara KF, El-Sheikh HF et al (2000) Extended wear contact lens related bacterial keratitis. Br J Ophthalmol 84(3):327–328
Tiller JC, Liao CJ et al (2001) Designing surfaces that kill bacteria on contact. Proc Natl Acad Sci U S A 98(11):5981–5985
van Kleef E, Robotham JV et al (2013) Modelling the transmission of healthcare associated infections: a systematic review. BMC Infect Dis 13:294
Webb LX, Meyers RT, Cordell AR, Hobgood AR, Costerton JW, Gristina AG (1986) Inhibition of bacterial adhesion by antibacterial surface pretreatment of vascular prostheses. J Vasc Surg 4:16–21
Willcox MD, Carnt N et al (2010) Contact lens case contamination during daily wear of silicone hydrogels. Optom Vis Sci 87(7):456–464
Yokoi N, Okada K et al (2000) Acute conjunctivitis associated with biofilm formation on a punctal plug. Jpn J Ophthalmol 44(5):559–560
Zegans ME, Shanks RM et al (2005) Bacterial biofilms and ocular infections. Ocul Surf 3(2):73–80
Acknowledgments
Dr Kishore and Dr Bramhachari are grateful to thier academic institutions for the support extended.
Conflict of Interest
The authors declares that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Godisela, K.K., Bramhachari, P.V. (2019). Biofilm Formation on Ophthalmic Device-Related Infections: Insights on Clinical Implications. In: Bramhachari, P. (eds) Implication of Quorum Sensing and Biofilm Formation in Medicine, Agriculture and Food Industry . Springer, Singapore. https://doi.org/10.1007/978-981-32-9409-7_11
Download citation
DOI: https://doi.org/10.1007/978-981-32-9409-7_11
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-32-9408-0
Online ISBN: 978-981-32-9409-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)